Abstract
Background
Kounis syndrome is the occurrence of acute coronary syndrome precipitated by an allergic reaction in the presence or absence of underlying coronary artery disease. The syndrome is explained by the effect of released inflammatory mediators on the coronary arteries and platelets.
Case summary
We report an uncommon case of Kounis syndrome Type II in a 65-year-old man 24 h after being bitten by a hymenoptera. Clinical context, electrocardiogram, coronary angiography, and enhanced cardiac magnetic resonance imaging (MRI) imaging modality are presented.
Discussion
Awareness and understanding of this syndrome is essential for starting early and appropriate therapy, thereby preventing life-threatening events. Accordingly, we highlight the importance of enhanced cardiac MRI to complete the assessment of this entity.
Keywords: Kounis syndrome, Acute coronary syndrome, Cardiac MRI, Allergic reaction, Myocardial infarction, Case report
Learning points
Improve physician awareness of a potential Kounis syndrome among allergic patients presenting with acute coronary syndrome.
Highlight on the appropriate tricky unstandardized management of Kounis syndrome.
Importance of enhanced cardiac magnetic resonance imaging to complete the assessment of Kounis syndrome.
Introduction
‘Kounis syndrome’ also known as ‘allergic angina’ or ‘allergic myocardial infarction’ was first described in 1991 as the occurrence of acute coronary syndrome (ACS) triggered by hypersensitivity, allergic, or anaphylactic reaction.1 The lack of international guidelines makes the optimal management decision difficult, considering that treatment of one of the two involved entities may worsen the other. Since Kounis syndrome is rare and a limited number of clinicians will encounter it through their career; we report this case in order to highlight the additive utility of contrast enhanced cardiac magnetic resonance imaging (MRI) for diagnostic and prognostic purposes, emphasizing the importance of putting this syndrome, as a potential differential diagnosis, among patients presenting with an acute typical cardiac chest pain.
Timeline
| Day 0 (admission date) | A 65-year-old male patient presents with an anaphylactic cardiovascular collapse, successfully treated by IV corticosteroids, anti-histamines and fluids. |
| Day 1 | He develops a severe epigastric pain attributed to ST-segment elevation myocardial infarction in the inferior electrocardiogram leads. |
| Within 4 h | Transfer to specialized cardiac catheterization centre. Coronary angiography shows a significant stenosis of hypoplastic right coronary artery and an uncertain culprit distal occlusion on the left posterior descending artery. Ventriculogram reveals an akinesia of the infero-median wall. |
| Day 2 | Enhanced cardiac magnetic resonance imaging shows an acute transmural myocardial necrosis on the infero-median segment and an acute sub-endocardial necrosis on the infero-septo-basal segment. Diagnosis of Type II Kounis syndrome treated with dual antiplatelets, statins, amlodipine, and avoiding beta-blockers. |
| 3 months after hospital discharge | Asymptomatic patient with good clinical performance for daily activities. |
Case presentation
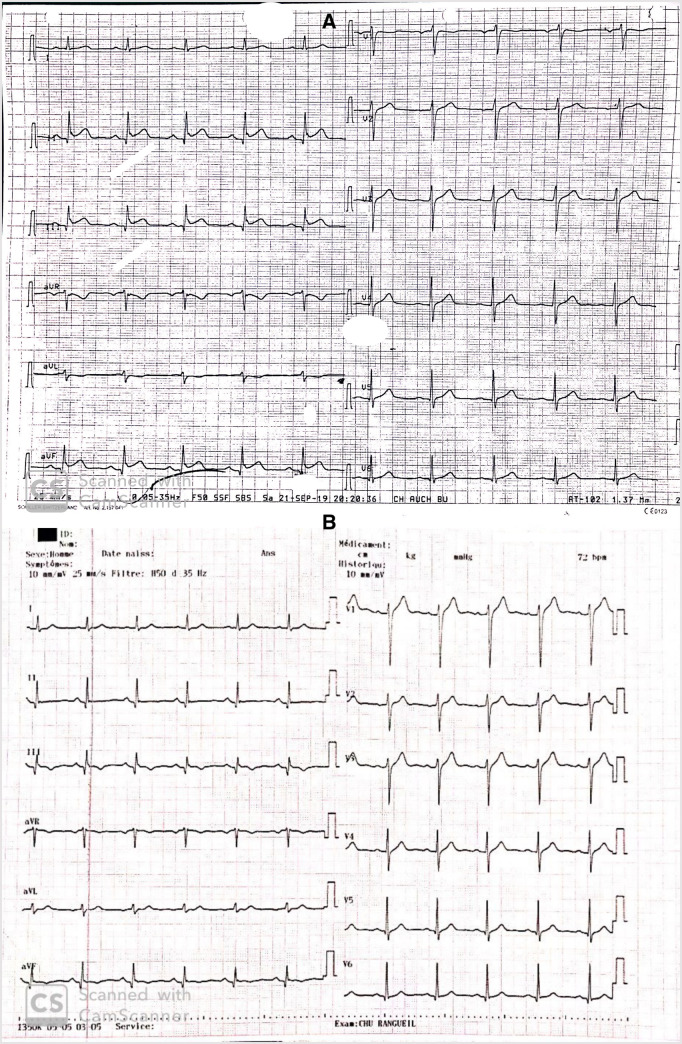
A 65-year-old man presented to a peripheral hospital with anaphylactic cardiovascular collapse after a hymenoptera bite. He was known to have hypertension, dyslipidaemia, and allergic reactions. The patient was successfully treated with intravenous fluids, oxygen support, corticosteroid, and antihistamines. Twenty-four hours later, he developed a severe epigastric pain with 1-mm ST-segment elevation in the inferior leads on the electrocardiogram (ECG) which required a transfer to our specialized cardiac catheterization centre (Figure 1A).
Figure 1.
Electrocardiogram. (A) Electrocardiogram showing ST-elevation in inferior leads and (B) Electrocardiogram showing Q waves in inferior leads.
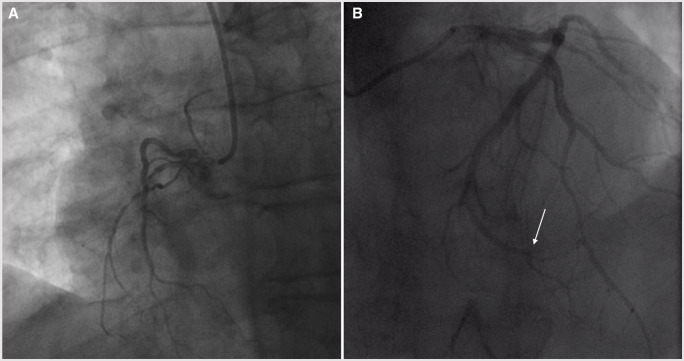
On admission, he was haemodynamically stable. Physical exam was unremarkable for cardiopulmonary findings. Laboratory studies showed: WBC count of 11.4 g/l (4–10 g/L normal range), eosinophils count of 0.3 g/L (2.3%) (0.04–0.5 g/L normal range), haemoglobin 13.9 g/dL (13–17.5 g/dL normal range), creatinine clearance 64 mL/min, positive sensitive troponin 228 ng/L which raised to 425 ng/L (<14 ng/L normal value), and mild elevated IgE level (0.14 kUa/L) (<0.1 KUa/L normal value). Electrocardiogram revealed a regular sinus rhythm with Q waves on inferior leads and a regression of ST-segment elevation (Figure 1B). Transthoracic echocardiography was normal, left ventricle ejection fraction was 60% without other relevant findings (Supplementary material online, Videos S1 and S2). Coronary angiography, within 4 h following anginal symptoms, showed a significant stenosis of a hypoplastic right coronary artery (Supplementary material online, Video S3, Figure 2A) and a probable culprit distal occlusion on the left posterior descending (LPD) artery rising from the left circumflex artery (Supplementary material online, Video S4, Figure 2B). We could not perform intracoronary imaging due to distality of the lesion. Ventriculography revealed an akinesia of the infero-lateral wall (Supplementary material online, Video S5).
Figure 2.
Coronary angiogram. (A) Significant stenosis on the hypoplastic right coronary artery. (B) Probable culprit distal occlusion on the left posterior descending artery rising from the left circumflex artery.
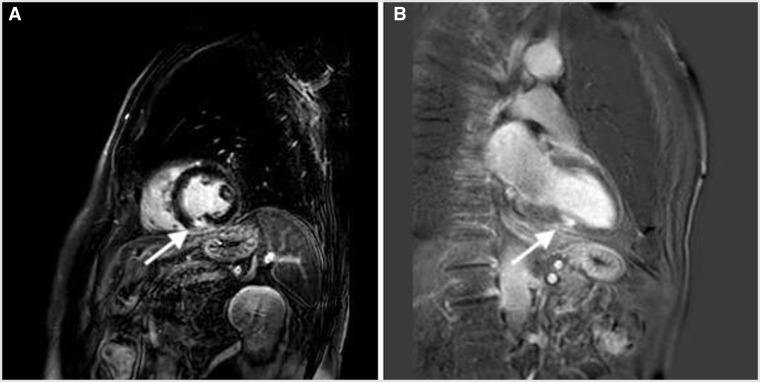
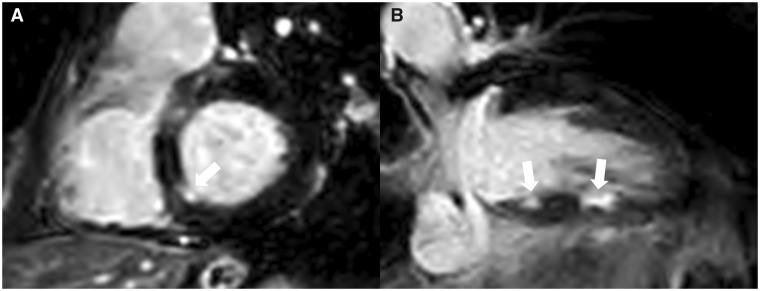
In the absence of a significant lesion explaining the clinical findings and the possibility of an unidentified distal occlusion of the LPD artery, we decided to complete our workup with contrast enhanced cardiac MRI. FAT-SAT T2-weighted sequence showed an oedema (hypersignal) in the infero-septo-basal segment correlating with sub-endocardial myocardial infarction. Contrast enhancement showed acute transmural myocardial necrosis on the infero-median segment (Figure 3A and B, Supplementary material online, Video S6), acute sub-endocardial necrosis on the infero-septo-basal segment (Figure 4A and B, Supplementary material online, Video S6), and a normal left ventricular ejection fraction at 59% (Supplementary material online, Video S7). Diagnosis of Kounis syndrome Type II was made based on the clinical context, coronary angiography, and cardiac MRI. The patient was discharged home with dual antiplatelets therapy (Aspirin and ticagrelor), statins, amlodipine, and subcutaneous adrenaline injection kit. A good clinical outcome was noted at 3 months of follow-up.
Figure 3.
Cardiac magnetic resonance imaging. (A) Short-axis enhanced cardiac magnetic resonance imaging showing an acute transmural myocardial necrosis on the infero-median segment. (B) Long-axis enhanced cardiac magnetic resonance imaging showing an acute transmural myocardial necrosis on the infero-median segment.
Figure 4.
Cardiac magnetic resonance imaging. (A) Short-axis late gadolinium enhanced cardiac magnetic resonance imaging showing an acute sub-endocardial necrosis on the infero-septo-basal segment. (B) Long-axis late gadolinium enhanced cardiac magnetic resonance imaging showing an acute sub-endocardial necrosis on the infero-septo-basal segment and the transmural infero-median necrosis.
Discussion
Several types of Kounis syndrome are described in literature based on coronary angiography characteristics. Type 1 is observed in patients with patent coronary arteries, Type 2 occurs in patients with pre-existing atheromatous coronaries, and Type 3 is associated with stent thrombosis. Overall, Kounis syndrome is characterized by the simultaneous occurrence of ACS in the event of allergic reaction. The pathophysiological mechanism of this phenomenon is not well-understood. It is hypothesized that secreted leucotrienes, histamines, and other pro-inflammatory mediators in the peripheral circulation during the acute hypersensitivity phase has an effect on the smooth muscle of the coronary vessels that results in coronary vasospasm. In addition to an activation of platelets, causing plaque erosion, or rupture and activating the coagulation cascade which induces thrombosis. Certain studies suggest that these mediators constitute a common pathway for both allergic and non-allergic ACS.2
Unfortunately, there are no clear guidelines or specific recommendations to follow regarding the management of Kounis syndrome.3 The therapeutic approach involves establishing an early myocardial perfusion and managing the anaphylactic reaction. It is essential to know that such beneficial strategies for either of the two combined entities may adversely affect the other.4 For this reason, corticosteroids and anti-histamines are preferred over epinephrine that would worsen the ischaemic event by worsening coronary vasoconstriction. In our case, corticosteroids and anti-histamines were administered before the occurrence of angina and ACS diagnosis. On the other hand, the use of aspirin which is the cornerstone for ACS treatment must be closely monitored due to the ability of aspirin on itself to induce or worsen the anaphylactic reaction.5 Percutaneous coronary intervention was avoided giving the hypoplastic feature of the right coronary artery, and the distally located culprit LPD lesion. Medical treatment based on dual antiplatelet therapy, amlodipine, and statins was provided with close allergology follow-up. It is worth noting that the use of beta-blockers in Kounis syndrome is harmful unlike in non-allergic angina where a beneficial effect has been established. Blocking beta receptors may lead to an unopposed activity of α-adrenergic receptors which would aggravate the coronary spasm and may inhibit some of the beneficial effects of epinephrine.
In most reported cases of Kounis syndrome, the diagnosis was made by using traditional tools such as ECG, cardiac enzymes, and coronary angiography. We reflect on our case the additive diagnostic information such as contrast enhancement patterns, location of myocardial injury, and necrosis provided by the enhanced cardiac MRI. Furthermore, cardiac MRI is also beneficial to evaluate myocardial viability in the affected areas following revascularization. Recently, cardiac MRI has become the widespread standard of care to differentiate between ischaemic and non-ischaemic cardiac diseases.6 In addition, it plays an essential role in the diagnosis of Kounis syndrome by assessing variant valuable parameters such as myocardial perfusion defects, patterns of myocardial contrast enhancement, dyskinesis in dynamic MR, and localization of defects (transmural, epicardial, or subendocardial).7
Conclusion
Several cases of Kounis syndrome encountered in clinical practice might be misdiagnosed. Early recognition is vital in order to start an early and appropriate management to avoid clinical deterioration, and progressing to life-threatening situation. As such, physicians, should be aware of this rare syndrome which must be excluded in patients presenting with ACS by a thorough history taking for a potential allergen exposure. Lastly, we emphasize on the importance of cardiac MRI as a useful tool to perform in order to complete the assessment of this syndrome.
Lead author biography

Jerome Roncalli, MD, PhD, completed his medical research training at Northwestern University in Chicago, under Professor Douglas Losordo. He is a Professor of Cardiology at the Purpan School of Medicine in Toulouse, France. Prof. Roncalli serves as the Assistant Director of the Cardiac Catheterization Laboratory since 2008. He also serves as Director of the Heart Failure, Transplantations and Assist Devices Unit at the University Hospital of Toulouse. Prof. Roncalli is a member of the French and the European Society of Cardiology. Prof. Roncalli is currently coordinator of the CARDIOMET Institute and the IMPACT FHU.
Supplementary material
Supplementary material is available at European Heart Journal - Case Reports online.
Slide sets: A fully edited slide set detailing this case and suitable for local presentation is available online as Supplementary data.
Consent: The author/s confirm that written consent for submission and publication of this case report including image(s) and associated text has been obtained from the patient in line with COPE guidance.
Conflict of interest: none declared.
Supplementary Material
References
- 1. Kounis NG, Zavras GM.. Histamine-induced coronary artery spasm: the concept of allergic angina. Br J Clin Pract 1991;45:121–128. [PubMed] [Google Scholar]
- 2. Kounis NG. Kounis syndrome (allergic angina and allergic myocardial infarction): a natural paradigm? Int J Cardiol 2006;110:7–14. [DOI] [PubMed] [Google Scholar]
- 3. Cevik C, Nugent K, Shome GP, Kounis NG.. Review treatment of kounis syndrom. Int J Cardiol 2010;143:233–236. [DOI] [PubMed] [Google Scholar]
- 4. Omri M, Kraiem H, Mejri O, Naija M, Chebili N.. Management of Kounis syndrome: two case reports. J Med Case Rep 2017;11:145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Fassio F, Losappio L, Antolin-Amerigo D, Peveri S, Pala G, Preziosi D, Massaro I, Giuliani G, Gasperini C, Caminati M, Heffler E.. Kounis syndrome: a concise review with focus on management. Eur J Intern Med 2016;30:e7–e10. [DOI] [PubMed] [Google Scholar]
- 6. Baritussio A, Scatteia A, Bucciarelli-Ducci C.. Role of cardiovascular magnetic resonance in acute and chronic ischemic heart disease. Int J Cardiovasc Imaging 2018;34:67–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Okur A, Kantarci M, Karaca L, Ogul H, Aköz A, Kızrak Y, Aslan S, Pirimoglu B, Aksakal E, Emet M.. The utility of cardiac magnetic resonance imaging in Kounis syndrome. Postepy Kardiol Interwencyjnej 2015;3:218–223. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.