Abstract
Background
Atrial fibrillation can contribute to heart failure. Frequently, rhythm control is unachievable. Atrioventricular (AV) junction ablation and pacemaker implantation remain to be a therapeutic option for rate control in atrial fibrillation. Interventricular asynchrony is a potential downside of right ventricular pacing. However, cardiac resynchronization therapy and His pacing restore physiological activation sequences of the ventricles.
Case summary
The reported patient had undergone several interventions to cure atrial fibrillation without sufficient rhythm control and experienced deleterious effects of recurrent arrhythmias. Finally, we decided to ablate the AV junction simultaneously with the implantation of a His bundle pacemaker. Atrioventricular junction ablation had to be repeated following conduction recurrence. A left-sided transaortic approach was required to create a permanent effect and to avoid distal lesions. His pacing was not affected by the AV junction ablation at all. The pre-existing widened QRS was normalized by His pacing, the patient became free of any complaints with full restoration of exertion capability.
Discussion
His pacing has the potential to contribute to a revival of the ‘ablate-and-pace’ concept for incurable atrial fibrillation by restoring physiological ventricular activation, thereby overcoming the particular drawbacks of continuous ventricular pacing. Atrioventricular junction ablation simultaneously with the pacemaker implantation procedure is safe and feasible. His pacing is at least an alternative for cardiac resynchronization therapy. The implantation procedure is sometimes challenging.
Keywords: Case report, Atrial fibrillation, AV junction ablation, His pacing, Ablate-and-pace
Learning points
Atrial fibrillation contributes to heart failure. If curative treatment options fail, atrioventricular (AV) junction ablation is able to provide rate control and symptom relief.
His bundle pacing resembles the physiological activation sequence of the ventricles, thus overcoming the downsides of right ventricular pacing.
Ablation of the AV junction simultaneously with the implantation of a His pacemaker is safe and feasible. Distal His ablation lesions can be avoided by a left-sided ablation approach.
Introduction
Atrial fibrillation can contribute to heart failure although the mechanism is not completely understood. Part of the mechanism is tachycardia-induced cardiomyopathy. A curative intervention of atrial fibrillation might not be indicated due to comorbidities, age, or previous unsuccessful attempts. Rate control and regularization can also be achieved by ablating the atrioventricular (AV) junction. This procedure is bound to the implantation of a pacemaker.1 The complete interruption of the AV conduction results in almost 100% ventricular stimulation by a pacemaker system.
The idea to stimulate the heart at the His bundle and the beneficial haemodynamic effects were described 50 years ago.2 His bundle pacing might overcome some of the downsides of AV junction ablation, which is not curative for atrial fibrillation and burdened by pacing-induced ventricular asynchrony.
Timeline
| 2011 | Atrial fibrillation detected |
| 2014–2019 | Antiarrhythmic drug treatment with betablockers, dronedarone, amiodarone |
| February 2017 | First pulmonary vein isolation (PVI) |
| October 2017 | Second PVI, re-isolation of all four veins, left atrial roof-line |
| February 2018 | Third PVI, box lesion of left atrial posterior wall, septal mitral line, tricuspid line |
| June 2018 | Fourth procedure, ablation of complex fractionated atrial electrograms |
| June 2019 | His pacemaker implantation, simultaneous atrioventricular (AV) junction ablation |
| July 2019 | Re-ablation of AV junction via transaortic approach |
| April 2020 | Absence of any atrial arrhythmias proven by stored electrograms and arrhythmia plot of the implanted pacemaker (recent follow-up visit) |
Case presentation
We report a 72-year-old male patient referred for heart rate control by AV junction ablation with simultaneous implantation of a His bundle pacemaker. Atrial fibrillation was first diagnosed in 2011. Antiarrhythmic drug therapy with betablockers and dronedarone did not lead to sufficient rhythm control; amiodarone had to be discontinued due to visual impairment. Despite anticoagulation with apixaban, ischaemic events occurred. The electrocardiogram showed sinus bradycardia, first-degree AV block, and intraventricular conduction delay (QRS width 172 ms with right precordial positivity).
Recurrent atrial arrhythmia with 2:1 conduction (Figure 1) led to clinical signs of heart failure and reduced exercise capacity. Left ventricular (LV) ejection fraction decreased to 39% together with marked interventricular and intraventricular dyssynchrony.
Figure 1.
Twelve-lead electrocardiogram; atrial flutter with 2:1 atrioventricular conduction, heart rate 120/min, and QRS widening with right precordial positivity. Calibrating rectangle: 200 ms, 1 mV (50 mm/s. sweep).
A total of four curative ablation procedures were performed. After two pulmonary vein isolation procedures in 2017, regularized atrial flutter resulted. In February 2018, left atrial substrate modification was added with box isolation of the left atrial posterior wall, as well as linear lesions along the septal mitral and tricuspid isthmus. In June 2018, conduction block was confirmed within a fourth intervention and augmented by ablation of complex fractionated atrial electrograms. Nevertheless, the patient experienced relapse of atrial macro-reentry. Short-term rate control following electrical cardioversion was marked by immediate freedom from complaints.
Because the patient refused a fifth curative attempt, we decided to achieve rate control by ablating the AV junction. Given the clinical signs of heart failure and the depressed LV function, physiological pacing was sought for prevention of deterioration of cardiac function due to permanent right ventricular stimulation, and His pacing was preferred to biventricular pacing by the patient.
In June 2019, we implanted a triple chamber pacemaker (Solara™, Medtronic Inc., Minneapolis, MN, USA). After placement of a right ventricular and a right atrial lead the His bundle was identified and a pacing electrode screwed in. The QRS complex narrowed from 172 to 112 ms by non-selective His bundle capture (Figure 2).
Figure 2.
Twelve-lead electrocardiogram; sinus rhythm, narrow QRS complex with non-selective His bundle pacing. Calibrating rectangle: 200 ms, 1 mV (50 mm/s. sweep).
Ablation of AV junctional conduction was performed immediately thereafter without affecting pacemaker function and stimulated QRS morphology (Figure 3).
Figure 3.
Fluoroscopy of atrioventricular junction ablation with right atrial (A), right ventricular (V), and His electrode (H) in place. C, ablation catheter tip.
Unfortunately, AV conduction and atrial flutter reoccurred with loss of the initial clinical improvement. Atrioventricular junction ablation was repeated 4 weeks later. In order to avoid distal AV junctional lesions that might affect His pacing, AV conduction was interrupted by a single left-sided lesion via a transaortic approach.
Ten months after, the patient is free of complaints with full restoration of exertion capacity. Left ventricular function has normalized. All stimulation thresholds are <1.0 Volt at 0.5 ms pulse width. Surprisingly, sinus rhythm persists during the entire follow-up period. Echocardiography revealed resynchronization of regional wall movement, ejection fraction is 59% (Figure 4).
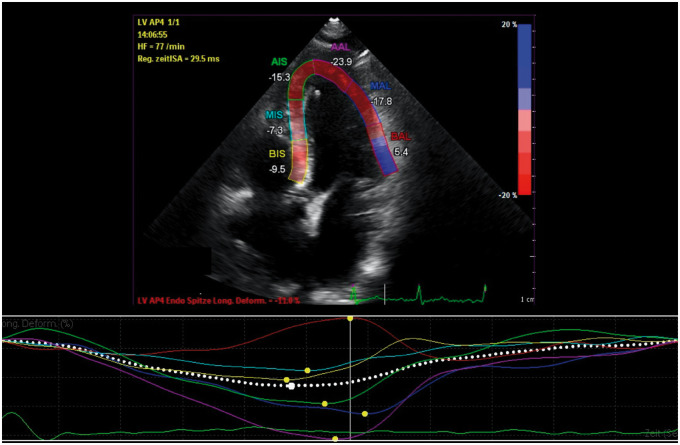
Figure 4.
Echocardiographic strain rate imaging of left ventricular regional wall movement demonstrates resynchronization with His bundle pacing.
Discussion
Ablation of the AV junction results in rate control and is associated with symptomatic and prognostic benefit. In 1611 patients, pacing with junctional ablation reduced heart failure hospitalizations by 69%.3 However, pacing-induced cardiomyopathy is reported in up to 12% of patients within 4 years.4 Biventricular pacing is haemodynamically favourable compared to right ventricular stimulation (especially in patients with depressed LV function), but it also does not restore physiologic activation.5 In contrast, stimulation of the His bundle results in completely physiologic ventricular activation.6,7 However, the implantation procedure for His bundle stimulation is technically challenging.8,9
Usually, AV junction ablation is performed in a separate procedure after the pacemaker implantation. The AV junction is in close spatial proximity to the His lead, mechanical alteration is a concern. Therefore, we performed pacemaker implantation and the ablation in a single procedure, so that immediate lead revision would have been possible if the ablation compromised the His bundle pacing lead.
Growth of the ablation lesion size also might affect the His threshold in a way not exactly to predict. Loss of stimulation in a pacemaker-dependent patient is a life-threatening event. Therefore, we recommend an additional right ventricular electrode to guarantee stimulation at any time. Ablation of the AV junction is a technically reliable procedure with high success rates. A repeat procedure has to be performed in 2.9%, in 6.9% add-on lesions via transaortic approach, as required in the reported case.10
Finally, the patient has become free of any atrial arrhythmia without additional interventions. Perhaps reduction in left atrium (LA) wall tension by heart rate control and resynchronization plays a role in prohibiting arrhythmia recurrence.
The beneficial effects of rate control by AV junction ablation, as well as the usefulness of physiological pacing by biventricular or His bundle stimulation, have found their way into the guidelines. The European guidelines give AV junction ablation and resynchronization therapy for intractable tachycardias a IIa indication (evidence B),11 and a Class I indication (evidence C) for tachycardia-related cardiomyopathy.12 ACC/AHA/HRS guidelines recommend AV junction ablation and physiological stimulation techniques for patients with impaired LV function, AV block and expected pacing rates >40% (Class IIa indication, evidence B).13
His bundle stimulation is evolving field and an alternative strategy to biventricular stimulation, as well as a therapeutic option for non-responders of cardiac resynchronization therapy.5,14 The procedure requires special skills of the implanter. If attempts to stimulate the His bundle fail, biventricular pacing by introducing a coronary venous LV electrode is an alternative to achieve cardiac resynchronization, vice versa.
Lead author biography

Dirk Grosse Meininghaus is Head of the Department of Cardiology at Carl-Thiem-Hospital in Cottbus, Germany. He finished Medical school in Giessen, Germany in 1993, and received his cardiology and electrophysiology training in Hamburg and Bremen, Germany. His special interests are catheter ablation of arrhythmias, atrial fibrillation, oral anticoagulation, and cardiac resynchronization therapy.
Supplementary material
Supplementary material is available at European Heart Journal - Case Reports online.
Slide sets: A fully edited slide set detailing this case and suitable for local presentation is available online as Supplementary data.
Consent: The author/s confirm that written consent for submission and publication of this case report including image(s) and associated text has been obtained from the patient in line with COPE guidance.
Conflict of interest: none declared.
Supplementary Material
References
- 1. Chatterjee NA, Upadhyay GA, Ellenbogen KA, McAlister FA, Choudhry NK, Singh JP.. Atrioventricular nodal ablation in atrial fibrillation: a meta-analysis and systematic review. Circ Arrhythm Electrophysiol 2012;5:68–76. [DOI] [PubMed] [Google Scholar]
- 2. Narula OS, Scherlag BJ, Samet P.. Pervenous pacing of the specialized conducting system in man. His bundle and A-V nodal stimulation. Circulation 1970;41:77–87. [DOI] [PubMed] [Google Scholar]
- 3. Mittal S, Musat DL, Hoskins MH, Prillinger JB, Roberts GJ, Nabutovsky Y. et al. Clinical outcomes after ablation of the AV junction in patients with atrial fibrillation: impact of cardiac resynchronization therapy. J Am Heart Assoc 2017;6:e007270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Kiehl EL, Makki T, Kumar R, Gumber D, Kwon DH, Rickard JW. et al. Incidence and predictors of right ventricular pacing-induced cardiomyopathy in patients with complete atrioventricular block and preserved left ventricular systolic function. Heart Rhythm 2016;13:2272–2278. [DOI] [PubMed] [Google Scholar]
- 5. Loring Z, Sun AY.. Should His bundle pacing be preferred over cardiac resynchronization therapy following atrioventricular junction ablation? Cardiol Clin 2019;37:231–240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Beer D, Sharma PS, Subzposh FA, Naperkowski A, Pietrasik GM, Durr B. et al. Clinical outcomes of selective versus nonselective His bundle pacing. JACC Clin Electrophysiol 2019;5:766–774. [DOI] [PubMed] [Google Scholar]
- 7. Upadhyay GA, Tung R.. Selective versus non-selective his bundle pacing for cardiac resynchronization therapy. J Electrocardiol 2017;50:191–194. [DOI] [PubMed] [Google Scholar]
- 8. Abdelrahman M, Subzposh FA, Beer D, Durr B, Naperkowski A, Sun H. et al. Clinical outcomes of his bundle pacing compared to right ventricular pacing. J Am Coll Cardiol 2018;71:2319–2330. [DOI] [PubMed] [Google Scholar]
- 9. Vijayaraman P, Dandamudi G, Zanon F, Sharma PS, Tung R, Huang W. et al. Permanent His bundle pacing: recommendations from a Multicenter His Bundle Pacing Collaborative Working Group for standardization of definitions, implant measurements, and follow-up. Heart Rhythm 2018;15:460–468. [DOI] [PubMed] [Google Scholar]
- 10. Kay GN, Ellenbogen KA, Giudici M, Redfield MM, Jenkins LS, Mianulli M. et al. The Ablate and Pace trial: a prospective study of catheter ablation of the AV conduction system and permanent pacemaker implantation for treatment of atrial fibrillation. APT Investigators. J Interv Card Electrophysiol 1998;2:121–135. [DOI] [PubMed] [Google Scholar]
- 11. Brignole M, Auricchio A, Baron-Esquivias G, Bordachar P, Boriani G, Breithardt OA. et al. 2013 ESC Guidelines on cardiac pacing and cardiac resynchronization therapy: the Task Force on cardiac pacing and resynchronization therapy of the European Society of Cardiology (ESC). Developed in collaboration with the European Heart Rhythm Association (EHRA). Eur Heart J 2013;34:2281–2329. [DOI] [PubMed] [Google Scholar]
- 12. Brugada J, Katritsis DG, Arbelo E, Arribas F, Bax JJ, Blomstrom-Lundqvist C. et al. 2019 ESC Guidelines for the management of patients with supraventricular tachycardia. The Task Force for the management of patients with supraventricular tachycardia of the European Society of Cardiology (ESC). Eur Heart J 2020;41:655–720. [DOI] [PubMed] [Google Scholar]
- 13. Kusumoto FM, Schoenfeld MH, Barrett C, Edgerton JR, Ellenbogen KA, Gold MR. et al. 2018 ACC/AHA/HRS Guideline on the evaluation and management of patients with bradycardia and cardiac conduction delay: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society. J Am Coll Cardiol 2019;74:e51–e156. [DOI] [PubMed] [Google Scholar]
- 14. Sharma PS, Dandamudi G, Herweg B, Wilson D, Singh R, Naperkowski A. et al. Permanent His-bundle pacing as an alternative to biventricular pacing for cardiac resynchronization therapy: a multicenter experience. Heart Rhythm 2018;15:413–420. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.