Abstract
Background
The current coronavirus disease 2019 pandemic has had an unprecedented impact on all physicians and has resulted in dramatic changes to clinical and research operations. No study has yet looked at the impact of coronavirus disease 2019 on the surgical research community. In this study, we sought to understand the impact of the pandemic and its associated restrictions on academic surgeons.
Methods
We surveyed members of the Association for Academic Surgery and the Society of University Surgeons. Survey questions included demographics, current challenges to basic and clinical research activities, attitudes toward remote work and productivity maintenance, and the solutions implemented to maintain productivity.
Results
Of 301 respondents, 70% cited a negative impact on research productivity due to mandatory building shutdowns, minimized personnel as a result of social distancing, and suspensions of animal work and clinical trials, with senior faculty and division chiefs and chairs more likely to report a negative impact (P = .001). Only 11% of respondents are documenting their financial losses, and only 19% indicated they received appropriate guidance regarding why and how to monitor the financial impact of the pandemic. Researchers have attempted to maintain research productivity through a focus on remote work, including manuscript writing, grant writing, and data analysis. Some participants have found silver linings, including more time to dedicate to research and family as a result of fewer clinical duties.
Conclusion
Productivity strategies developed during the pandemic, including writing, remote work and meetings, and structured scheduling, are lessons that will allow the surgical research community to be resilient in the face of future disruptions.
Introduction
The novel coronavirus disease 2019 (COVID-19) pandemic is an unprecedented crisis with far-reaching impact. It has put a heavy burden on frontline personnel, including surgeons, and has caused incredible public health and economic disruptions. Surgeons are accustomed to responding to crises in the operating room and, during the current pandemic, are being called to apply their crisis management tools in new ways to combat the effects of the pandemic on their clinical programs, including the introduction of new screening protocols, a rapid shift toward telemedicine, and the suspension of elective procedures in many institutions.1 For academic surgeons, the crisis has placed a unique and unprecedented strain on a less recognized but important facet of work–research.
Despite these significant changes in the clinic, it is unclear how surgical research has been affected by the COVID-19 pandemic or how academic surgeons are responding to the crisis. Although recent studies have assessed the implications of the pandemic on pediatric and oncologic research efforts, as well as the broader research community, there has been no large study to identify the effects specifically in the surgical community.2, 3, 4 We sought to understand the impact of the COVID-19 pandemic on surgical research endeavors and identify solutions and potential opportunities to optimize research under the current challenges so that academic surgeons can more adequately plan for future disruptions to their research activity.
Methods
A questionnaire was developed to ascertain demographic data, assess the current challenges that surgeon-scientists are facing during the COVID-19 pandemic, and identify potential solutions to maintain productivity. Survey topics included the financial impacts of the pandemic, the impact of governmental and institutional regulations on access to the laboratory and research productivity, and strategies for maintaining productivity while under stay-at-home orders. The survey was validated for content and clarity by the Basic and Translational Science Committee of the Association for Academic Surgery (AAS) and the Research Committee of the Society of University Surgeons (SUS). The questionnaire was circulated via email distribution to the membership of the AAS and the SUS. Data were collected from April 6 to 10, 2020. We elected to have a short distribution period to minimize time as a confounding variable, given the rapidly evolving situation during the COVID-19 pandemic; accordingly, the expected response rate was anticipated to be lower than that of prior surveys disseminated through the AAS and SUS networks. All personal or identifiable information was removed before analysis to ensure anonymity. Respondents were stratified by academic rank, defined as trainee (medical student, resident, fellow), junior faculty (<5 years post-training), senior faculty (>5 years post-training), or division chair or section chief. Raw data were exported to Microsoft Excel (Microsoft Corporation, Redmond, WA), and χ2 tests were performed where appropriate, with significance defined as P < .05.
Results
Demographic data
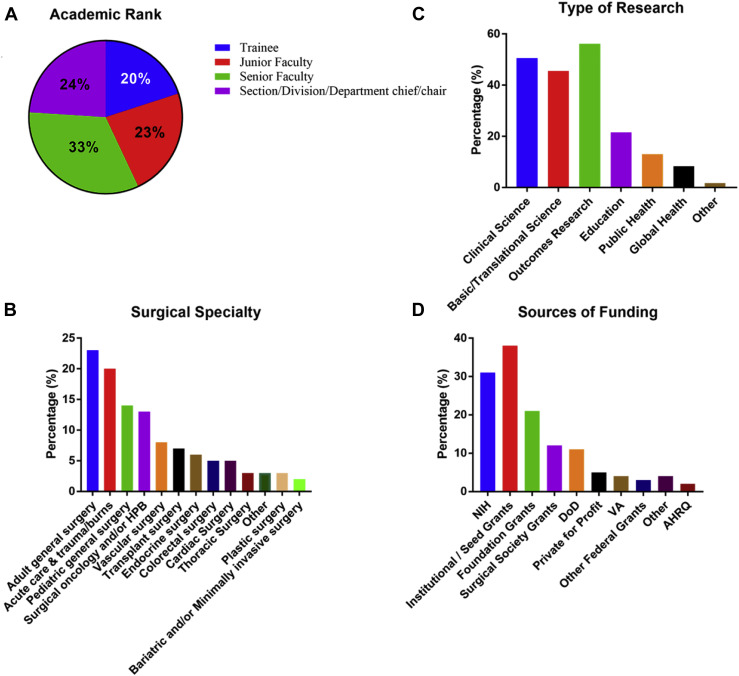
The survey was sent out to 2,504 members of the SUS and AAS memberships, and 301 responded to the survey (12%). Of those, 61 (20%) were trainees, 68 (23%) junior faculty, 100 (33%) senior faculty, and 72 (24%) division chairs or section chiefs. The most common surgical specialties were general (23%), acute care and trauma (20%), pediatric (14%), oncology (13%), vascular (8%), and transplant (7%). All participants indicated that they perform research of some kind, including 137 (45.6%) who perform basic science research, 152 (50.5%) clinical research, and 169 (56.2%) outcomes-based research. The majority of participants (73.1%) were funded, with the majority of their funding derived from institutional or seed grants (37.9%), the National Institutes of Health (31.2%), and foundation grants (21.3%) (Fig 1 ).
Fig 1.
Demographic characteristics of participants. (A) Academic rank was defined as trainee (medical student or resident), junior faculty (5 years or less out of training), senior faculty, or department/division chairs. Respondents were also classified by (B) surgical specialty and (C) type of research performed. Of the 73% of participants who are funded, sources of funding are indicated (D).
Current challenges during the COVID-19 pandemic
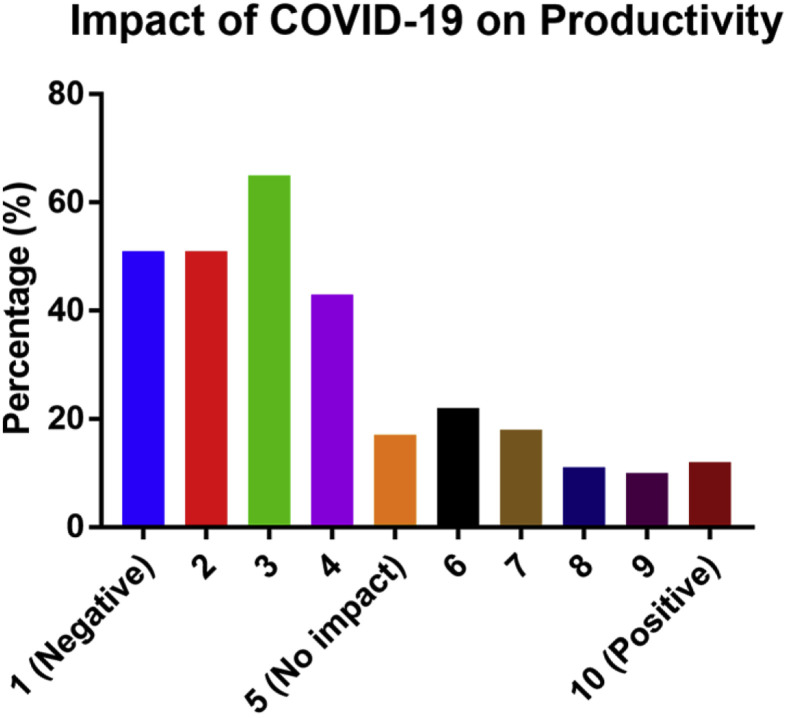
Most researchers (70%) surveyed have been negatively impacted by overall restrictions and changes (Fig 2 ). When stratified by rank, senior faculty and division chairs/chiefs were more likely to perceive a negative impact than trainees (P = .001). Negative impacts commonly derived from city, state, and federal restrictions, as well as institutional building shutdowns. Interestingly, 24% indicated a positive impact of the pandemic on research. Responses from these participants cited fewer clinical duties and more time to dedicate to research, including writing manuscripts and grants.
Fig 2.
Impact of restrictions due to the current pandemic on research productivity. The question was framed as, “How has the current COVID-19 pandemic affected your scientific research productivity?” Three hundred out of 301 participants answered this question, and of those, 70% indicated a negative impact. Interestingly, 24% indicated a positive impact.
The majority of basic scientists whose work depends on animal colonies have had to halt experiments and/or wean their animal colonies. The majority of participants (86.5%) have had to wean their colonies by at least 50%. This has also carried over to researchers who work with primary cells, cell lines, or tissue culture, as 75% of respondents have been negatively affected by COVID-19 restrictions. For those who had been affected, building closures and inability to access the lab space contributed to the halting of their research. Of those investigators conducting clinical trials, 88.4% have had to stop their work, citing their patients’ inability to access the hospital, lack of personnel as a result of stay-at-home orders, shifting of clinical duties toward COVID-19 care, and the cessation of nonessential research per institutional mandate (Fig 2). In terms of overall time dedicated to research weekly, the results were split, with 47.3% indicating increased time for research and 52.7% having decreased time, with no differences noted when stratified by rank or number of lab employees.
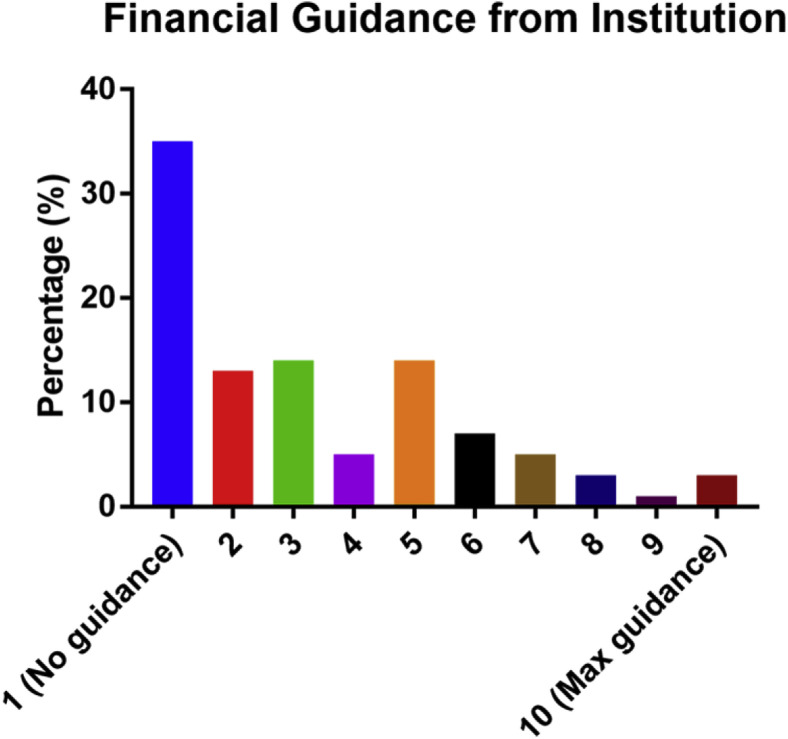
COVID-19 closures have affected the financial situation of many individuals and institutions. However, only 19% of participants felt that they had received enough guidance (indicating 6 to 10 in the survey) to prepare for the financial implications of COVID-19, and the remaining 81% felt that they had little to no guidance, indicating between 1 and 5 (Fig 3 ). Perhaps because of this lack of information, only 10.8% of participants are documenting their research financial losses accrued due to COVID-19. Fortunately, 63.4% of investigators have not had to lay off or furlough any team members. Despite a lack of financial guidance, 74.9% of investigators felt that they have received moderate to complete support from their parent institution in navigating the crisis.
Fig 3.
Participants indicated the amount of guidance they feel they have received from their parent institution regarding the financial impact of COVID-19. The question was framed as, “Do you feel that you have received guidance regarding the financial implication of the shutdown of labs and funding?” Out of 301 respondents, 294 individuals answered this question. Of those, only 19% felt that they had received adequate guidance, indicating a 6 or above on this question.
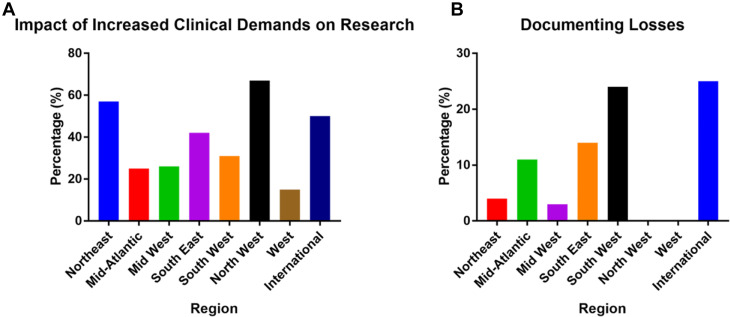
Although all states have been affected by COVID-19, not all have been affected equally. Participants in the northeast and northwest indicated that increased clinical demands were significantly affecting their ability to pursue research (P = .04). However, documenting financial losses also differed by region, with participants located in the southwest region documenting more often (P = .004) (Fig 4 ).
Fig 4.
Participants indicated whether increased clinical demands have impacted their ability to perform research (A) and whether they are documenting their losses (B) (stratified by region). Those in the northeast and northwest were more likely to be affected by increased clinical demands (P = .04). In terms of documenting losses, those in the southwest region were documenting losses more (P = .004).
Developing solutions
As institutions and buildings shut down, most nonessential researchers have shifted to remote work. To understand the effect on productivity, we surveyed participants to ask what solutions they have implemented to optimize this work arrangement. Although most (54.2%) have not increased the frequency of lab meetings, a larger proportion of labs with >10 members have increased the frequency of group meetings (13% for <5 members, 21% for labs between 6 and 10 in size, 27% for 11 to 15 members, and 47% for labs larger than 15 members, P < .001). In addition to lab meetings, 41.1% of participants have scheduled one-on-one meetings with their team members. Many have shifted their focus from wet lab techniques to data analysis, manuscript writing, and grant writing (59.8%), whereas others have increased their collaborations with other labs (17.0%). More than half (61.8%) of participants have positively changed their perspective on telecommuting and video conferencing, especially larger labs (>11 members). Platforms used for video conferencing included Zoom (84.2%), WebEx (34.8%), Skype (18.6%), and Microsoft Teams (16.2%). Attitudes reflected through the comments were largely positive, including comments that online meetings were more effective and convenient and that it would likely be a lasting tool for communication moving forward. Participants also stated that online meetings are a good option for maintaining face-to-face interactions and increase their ability to communicate with distant collaborators. After the current crisis ends, 53.0% would encourage their team members to work from home more often. Interestingly, trainees and junior faculty were more likely than senior faculty and division chairs/chiefs to encourage telecommuting once the COVID-19 pandemic is over (P < .001). On the other hand, there were also many respondents who felt that online meetings were inefficient and take longer than in-person meetings and that working from home was more difficult than in the office. Many also commented on the value of human interactions to produce and cultivate ideas, which was not felt to be reproducible through virtual means.
Maintaining research productivity
In the face of all these obstacles, we asked researchers to share advice on how they are able to maintain research productivity. Overwhelmingly, participants indicated that writing is the best way to maintain productivity, whether through grants, manuscripts, institutional review board protocols, or taking another look at unfinished projects. Remote data collection and clinical projects have also been a focus. The general takeaway was to identify projects that can be done from home and reduce efforts on other projects. In response to the challenge of remote work, many respondents recommended setting up a strict schedule and minimizing distractions during work hours. Perhaps most importantly, participants indicated that a flexible attitude is essential. Many unexpected silver linings were also reported, including more time at home with family or pets and better work–life balance. Trainees especially indicated more time in all categories than those of higher academic rank (P < .001) (Fig 5 ).
Fig 5.
Silver linings that COVID-19 has brought despite the current challenges, stratified by rank. Trainees indicated more silver linings than other career stages (P < .001).
Discussion
Overall effects of COVID-19 on research
Survey responses show the substantial impact of the COVID-19 crisis on research, with most surgeons reporting significant restrictions on research activities. Understandably, surgical departments and laboratories are subject to policies and restrictions outside their control, and thus may not be able to respond independently of these agencies. Restrictions included stay-at-home orders, reallocation of duties to clinical care, and physical closure of laboratories and research buildings.
Institutional bans on clinical research cited concerns over worker and patient safety due to unnecessary exposures. Unfortunately, this has hampered ongoing clinical research efforts and may have long-lasting effects for both patients and researchers.5 However, it is important to note that although the majority (>75%) of respondents stated that their research was negatively affected, almost a quarter of respondents (24%) indicated a positive impact. Before COVID-19, surgeons often faced challenges in balancing clinical practice, research, and personal time.6 Now, in parts of the country that were not as severely affected, the actual workload for some surgeons decreased due to cancellations of elective surgery, which may have led to an increased opportunity to engage more fully in research efforts.
Financial challenges and the future of research funding
This crisis has brought about major financial challenges for hospitals, which have reported significant losses due to the COVID-19 pandemic.7 , 8 These losses will especially strain surgical research at institutions where research was not as well supported, likely leading to further budget restrictions. In this study, over 60% of participants felt like they had little or no guidance from their institutions to prepare them for the financial implications of COVID-19. This was readily apparent in that only 10% of respondents were documenting research financial losses accrued due to COVID-19. Although there has been some guidance from the National Institutes of Health (NIH) about allowances because of COVID-19, there has been no guidance as to whether further funds may become available because of COVID-19 losses.9 However, given the extent of current congressionally approved stimulus funds, it would seem prudent to document losses in real time so that the accuracy of the net loss is improved if funds do become available, either through funding agencies, institutions, or the government. The long-term effects of COVID-19 may also be detrimental to research funding agencies’ ability to support new awards. In the United States, the extent of cuts has not yet been become apparent. The NIH and National Science Foundation have redirected funds to COVID-19 research, and the current funding cycle is being moved to a virtual study section to minimize disruption to the process.10 It may be too early to understand the full financial ramifications of COVID-19 on national research funding and pay lines. Lastly, it may be beneficial for investigators to develop a plan for advancing projects and prepare to submit new grants to counteract any potential budget reductions.
Solutions to address research challenges during COVID-19
The survey inquired about potential solutions to challenges posed by COVID-19. Like many other researchers, surgeons have developed innovative solutions to cope with the COVID-19 pandemic. As a result of social distancing, many laboratories and research efforts have gone to virtual platforms, and those with larger laboratories have increased the frequency of meetings, helping to give lab members a sense of schedule and accountability. As an upside to this pandemic, many researchers report having the time to complete unfinished projects, such as grants and manuscripts. This may also be an opportune time for surgical researchers to consider writing more retrospective clinical papers and review manuscripts. In terms of digital communication, most participants (62%) found value in remote meetings, although some maintained that in-person meetings have the benefit of sparking collaborations and innovative ideas that cannot be replicated by digital meetings. Even more unexpected silver linings included more time at home with family and a better work-life balance, which may result in durable changes to working arrangements after the pandemic.
Guidance on re-opening and preparing for future disasters
As the COVID-19 pandemic begins to subside and gives rise to a new normal, it is beneficial for research communities to develop a cohesive strategy for reopening. This strategy has 4 main considerations: financial, research activity and diversity, laboratory space and infrastructure, and personal health.
Financially, as mentioned earlier, it would be prudent for researchers to document losses as the pandemic unfolds. Although there has been no official statement from the NIH regarding future funding cycles, it may be appropriate to reach out to individual program officers and institutions to review budgets and options for intramural and extramural funding.
In resuming bench research or clinical trials, making the most of web-based tools to promote productivity will continue to be a critical strategy. Most respondents in this study indicated that they felt positively about the technology and believe that it will likely remain an important tool for communication moving forward owing to its ease of use in face-to-face conferencing and convenience in choosing a location. Telemedicine is now part of the clinical reality and will likely remain so in the future. It has the potential to improve clinical research and be integrated into clinical research protocols. Similarly, diversifying research portfolios to include remote work will also benefit research productivity. Engaging in opportunities to perform different types of activities both in and away from the physical laboratory or clinic space will help to minimize future interruptions. This can also be facilitated by developing new collaborations locally and nationally. As stay-at-home orders begin to relax, this will slowly allow personnel to resume benchtop research and clinical trials. For the basic scientist who conducts animal research, reconstituting mouse colonies when animal facilities reopen is an important first step, as animal colonies take longer to recover.
Reviewing the lab space and infrastructure will be important to maintain social distancing and ensure adequate ventilation, as well as stocking adequate personal protective equipment (PPE) and appropriate disinfectants. Implementing distancing rules for common spaces such as break rooms or tissue culture rooms will also have to be addressed. Both clinical and basic science research programs are likely to have to implement new protocols to document revised operating procedures that account for increased attention to distancing and hygiene. Additionally, laboratories may need to devise new approaches for onboarding and training of new personnel in the setting of distancing rules.
Above all, the personal health of all researchers should be paramount. Labs may adopt measures to decrease personnel exposures, including minimizing the number of individuals present at any given time either by alternating days, opening weekends, or allowing evening work opportunities, as appropriate. At the same time, implementing social distancing, having an appropriate masking policy, and reviewing safety protocols is essential. It is important to recognize that the COVID-19 pandemic has not just had a physical toll, but an emotional toll as well. The psychological safety of laboratory personnel must be considered with open communication, flexibility for individual concerns (eg, childcare and personal health), and guidance on institutional resources for wellbeing (Table I ).
Table I.
Summary of strategies for maintaining productivity and wellness during a crisis, and how to ramp up once that is allowed
| Financial | Review research budgets with leadership Reach out to grant funding agencies Document all lab losses as they occur Aggressive plan for submitting new grants |
| Research | Optimize web-based tools to promote productivity Diversify your research portfolio Pursue collaborations Allow personnel to start new in vitro experiments Postpone experiments that will use PPE Reconstitute mouse colonies |
| Lab space | Physical modification of the lab space including modification of ventilation (if necessary), availability of PPE, and accessibility of hand sanitizer and disinfectants Implement physical distancing rules for commons spaces, lunchroom, tissue culture rooms, etc |
| Personal health | Minimize the number of individuals who are present at any given time in a given space, by implementing shifts, alternating days, or including weekend opportunities Be mindful of childcare constraints and at-risk personnel, as these individuals might need additional flexibility and remote work plans Implement safety measures (6-foot distancing, masking policy, handwashing, additional safety protocols) |
PPE, personal protective equipment.
Limitations
This study has many inherent limitations due to the nature of a survey. As the time for dissemination was short, the response rate achieved was low (12%), potentially leading to responder bias. Also, as this study relies on self-reported data, there may be variability and inconsistency in the responses. Still, this study reflects opinions from academic surgeons across many different specialties and career stages regarding the current challenges they are facing, and their experiences and solutions can serve to inform other surgeon-scientists in similar situations.
The COVID-19 pandemic is an unprecedented disaster, and the research community, like most other organizations, was not prepared for this crisis. However, it is imperative that the community learn from this pandemic and turn it into an opportunity to develop strategies to help prepare for the next disaster, especially as many cities are facing an increasing number of COVID-19 cases and the risk of a new round of closures. For the surgical research community, this may include examining many of the current effects of the COVID-19 on research, as elucidated in this survey. For example, web-based integration of clinical research protocols, follow-up appointments using telehealth, and medications by mail or in-hospital appropriate facilities may allow for future protocols to be less affected, especially those for critically ill patients or with rare diseases. For individual labs, this pandemic has shown the value of having a diversified research portfolio that has multiple avenues of research with diverse infrastructure requirements, such as integrated use of web tools for clinical trials or bench work that can be analyzed remotely. In order for researchers to remain productive in the event of a future disaster or disruption, contingency plans need to be in place to account for disruptions in supply chain or resource allocation. Applying the lessons learned in the pandemic to create a plan of action will ensure a more durable and effective research enterprise.
In conclusion, the COVID-19 pandemic is an unprecedented disaster and has generated significant challenges for surgeons conducting research. These challenges have centered on workforce issues, laboratory infrastructure, financial implications, and the actual conduct of both clinical and basic research. Surgeons have persevered and developed many innovative solutions to continue their research endeavors. We can learn from the lessons of the COVID-19 pandemic to prepare and plan for other pandemics and disasters to help guide surgical research in the future.
Conflict of interest/Disclosure
None.
Funding/Support
None.
Acknowledgments
The authors acknowledge the editorial support of Monica Fahrenholtz, with the Office of Surgical Research Administration at Texas Children’s Hospital. We also acknowledge JJ Jackman and Catherine Hunter with the Association for Academic Surgery and Yumi Hori with the Society of University Surgeons with help in developing and distributing the survey.
References
- 1.Diaz A., Sarac B.A., Schoenbrunner A.R., Janis J.E., Pawlik T.M. Elective surgery in the time of COVID-19. Am J Surg. 2020;219:900–902. doi: 10.1016/j.amjsurg.2020.04.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Weiner D.L., Balasubramaniam V., Shah S.I., Javier J.R. the Pediatric Policy Council. COVID-19 impact on research, lessons learned from COVID-19 research, implications for pediatric research. Pediatr Res. 2020;88:148–150. doi: 10.1038/s41390-020-1006-3. [DOI] [PubMed] [Google Scholar]
- 3.Auletta J.J., Adamson P.C., Agin J.E. Pediatric cancer research: Surviving COVID-19. Pediatr Blood Cancer. 2020;67 doi: 10.1002/pbc.28435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bailey C., Black J.R.M., Swanton C. Cancer research: The lessons to learn from COVID-19. Cancer Discov. 2020;10:1263–1266. doi: 10.1158/2159-8290.CD-20-0823. [DOI] [PubMed] [Google Scholar]
- 5.Lupkin S. Coronavirus pandemic brings hundreds of US clinical trials to a halt; 2020. https://www.npr.org/sections/health-shots/2020/04/11/832210606/coronovirus-pandemic-brings-hundreds-of-u-s-clinical-trials-to-a-halt Accessed April 21, 2020.
- 6.Keswani S.G., Moles C.M., Morowitz M., and the Basic Science Committee of the Society of University Surgeons The future of basic science in academic surgery: Identifying barriers to success for surgeon-scientists. Ann Surg. 2017;265:1053–1059. doi: 10.1097/SLA.0000000000002009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.American Hospital Association Hospitals and health systems face unprecedented financial pressures due to COVID-19; 2020. https://www.aha.org/guidesreports/2020-05-05-hospitals-and-health-systems-face-unprecedented-financial-pressures-due Accessed April 21, 2020.
- 8.KaufmanHall Kaufman Hall perspective; 2020. https://flashreports.kaufmanhall.com/kha-perspective-april-2020 Accessed May 1, 2020.
- 9.National Institutes of Health (NIH) Flexibilities available to AHRQ recipients and applicants directly impacted by the novel coronavirus (COVID-19) due to loss of operations; 2020. https://grants.nih.gov/grants/guide/notice-files/NOT-HS-20-010.html Accessed April 21, 2020.
- 10.Webster P. How is biomedical research funding faring during the COVID-19 lockdown? Nat Med. 2020 doi: 10.1038/d41591-020-00010-4. Epub ahead of print. [DOI] [PubMed] [Google Scholar]