Abstract
Rapid responses in the early stage of a new epidemic are crucial in outbreak control. Public holidays for outbreak control could provide a critical time window for a rapid rollout of social distancing and other control measures at a large population scale. The objective of our study was to explore the impact of the timing and duration of outbreak-control holidays on the coronavirus disease 2019 (COVID-19) epidemic spread during the early stage in China. We developed a compartment model to simulate the dynamic transmission of COVID-19 in China starting from January 2020. We projected and compared epidemic trajectories with and without an outbreak-control holiday that started during the Chinese Lunar New Year. We considered multiple scenarios of the outbreak-control holiday with different durations and starting times, and under different assumptions about viral transmission rates. We estimated the delays in days to reach certain thresholds of infections under different scenarios. Our results show that the outbreak-control holiday in China likely stalled the spread of COVID-19 for several days. The base case outbreak-control holiday (21 d for Hubei Province and 10 d for all other provinces) delayed the time to reach 100 000 confirmed infections by 7.54 d. A longer outbreak-control holiday would have had stronger effects. A nationwide outbreak-control holiday of 21 d would have delayed the time to 100 000 confirmed infections by nearly 10 d. Furthermore, we find that outbreak-control holidays that start earlier in the course of a new epidemic are more effective in stalling epidemic spread than later holidays and that additional control measures during the holidays can boost the holiday effect. In conclusion, an outbreak-control holiday can likely effectively delay the transmission of epidemics that spread through social contacts. The temporary delay in the epidemic trajectory buys time, which scientists can use to discover transmission routes and identify effective public health interventions and which governments can use to build physical infrastructure, organize medical supplies, and deploy human resources for long-term epidemic mitigation and control efforts.
Keywords: COVID-19, Model, Lunar New Year holiday, Extension, Social distancing
1. Introduction
The coronavirus disease 2019 (COVID-19) pandemic is spreading rapidly [1]. Studies have estimated that the basic reproductive number of COVID-19 is higher than that of severe acute respiratory syndrome (SARS) coronavirus [2]. COVID-19 has posed major challenges for epidemic control because its routes of transmission are not fully understood, and prevention and screening, diagnosis, and treatment approaches still need to be developed and tested. Public health authorities initially lacked evidence-based approaches and protocols to contain the epidemic, and the rapid spread of the virus required new physical infrastructure, medical supplies, and human resources for an effective epidemic response.
In the initial response to the epidemic of a new virus, social policies to change people’s behaviors are potentially powerful in reducing and slowing down the spread of the disease. During the early stage of the COVID-19 outbreak in China, the holiday during the Chinese Lunar New Year, was a public holiday for outbreak control, which began during the same time period as the Chinese Lunar New Year, was utilized as a social policy that enabled fast responses at national scale [1], [3]. During this time period, the Chinese government initiated emergency responses to the epidemic, and enacted a series of non-pharmaceutical interventions such as travel restrictions, social distancing, active contact tracing, isolation, and quarantine, as well as public information and education campaigns [1]. For example, the Chinese government encouraged people to stay at home, discouraged mass gatherings, and closed schools, government offices, factories, libraries, and museums [4], [5], [6], [7], [8], [9], [10].
A public holiday for outbreak control—hereinafter referred to as an outbreak-control holiday—has been used as a public health policy in the past. For example, Mexico launched an outbreak-control holiday to contain the spread of H1N1 in 2009, during which schools and workplaces were closed and people were encouraged to stay at home [11]. During such an outbreak-control holiday people do not go to work and tend to stay at home, limiting social contacts to family members and close friends. As a result, these holidays can slow down the spread of epidemics that are transmitted via social contacts [12], [13], [14], [15], [16]. As an epidemic response strategy, an outbreak-control holiday can interrupt a wide variety of transmission routes, including direct and indirect physical contact, droplet contact, and airborne transmission. Outbreak-holidays can thus be particularly useful when a new pathogen’s precise transmission routes are not yet known [17], [18], [19], [20], [21].
While several studies have investigated the effectiveness of travel restrictions and social distancing measures in preventing the spread of COVID-19 in China, it is still generally unclear how the trend of an epidemic changes according to different characteristics of an outbreak-control holiday [22], [23]. Taking China’s outbreak-control holiday as an example, this paper aims to contribute to future policy decisions by answering the following questions: What was the likely impact of the outbreak-control holiday in China on the early COVID-19 epidemic? How would this impact have varied if the following parameters of the outbreak-control holiday had been different: the duration, implementation timing, and the effectiveness of accompanying policies? Our results provide important insights for policy makers charged with designing public health interventions to control the present COVID-19 pandemic, as well as epidemics that will emerge in the future.
2. Methods
2.1. Model description
We used a compartment model (Fig. S1 in Appendix A)—a commonly used modeling approach to estimate the impact of interventions on infectious disease transmission [24], [25]—to simulate COVID-19 spread in China. Our model divided the population into subgroups according to the status of COVID-19 infection, including susceptible, latent infection, active infection, confirmed diagnosis, followed by treatment and recovery. In order to capture how the Pdisease spread across provinces, we further separated the population into two regions: Hubei Province, which was the center of the epidemic, and the rest of China. To capture the transmission due to travel across Hubei’s borders, our model allowed transition of the susceptible and latent infected population between Hubei and the rest of China. The infection force was proportional to the prevalence of untreated infections, including people in both latent and symptomatic infection stages. We made the following assumptions: First, we assumed that the population under treatment, although still infected, did not cause more infections because they were receiving treatment in isolated settings. Second, we did not consider reinfection among the recovered population, due to likely immunity and the relatively small size of this group. Model development and statistical analysis were performed in R (verson 3.6.3, Austria).
Our model accounted for several events that could potentially affect transmission dynamics. The model simulated the disease transmission since 10 January 2020, when the diagnosis of COVID-19 was formally established. We assumed that there were 100 000 persons traveling through Hubei Province based on the past-year daily travel volume during the Chinese Lunar New Year travel season, or chunyun. Since many cities in Hubei were locked down since 23 January 2020 [9], we assumed no transitions between Hubei and other provinces since that time. We calibrated transmission rates before and during the outbreak-control holiday to estimate its impact on epidemic dynamics. We assumed that the disease transmission rate after the outbreak-control holiday returned to the level before the holiday (see Section S1 in Appendix A for further model details).
2.2. Data sources, parameter estimation, and calibration
Our primary data sources were the daily updates of the COVID-19 epidemic published by China’s national and provincial Health Commissions, including the cumulative number of confirmed cases, deaths, and recoveries, for both China as a whole and Hubei Province [26], [27]. We used the average incubation period for the duration of the latent infection period in our model [28]. We estimated the values of other model parameters and the initial epidemic conditions using model calibration [29], [30]. Calibration targets included daily increments of confirmed cases, cumulative number of deaths, and cumulative number of recoveries from 20 January 2020 to 31 January 2020, separately for Hubei Province and the combined total of the other provinces in China. We used a direct search algorithm [29] to identify the model parameter values that resulted in the closest match between the projected outcomes and the calibration targets. To account for uncertainties in the model parameters, we repeated the calibration process for 1000 replications and collected the set of calibrated parameters with a total calibration error no larger than 20% above the minimum error. Further details of the model parameter description can be found in Section S2 in Appendix A. Our calibrated model performed well in capturing the overall trend of the reported numbers of confirmed cases, deaths, and recoveries during the calibration period (Fig. S2 in Appendix A). The calibration results suggest that the transmission rate during the outbreak-control holiday was 55% of the rate before the holiday in Hubei Province and 45% of the rate before the holiday in all other provinces of China.
2.3. Projection scenarios
2.3.1. Epidemic impact of public holidays for outbreak control with different durations
We estimated the cumulative numbers of confirmed infections and all infections for the following outbreak-control holiday scenarios: ① base case: an outbreak-control holiday for 21 d in Hubei Province and 10 d in all other provinces of China, both starting on 24 January 2020 [5], [31]; ② no outbreak-control holiday; ③ 7-day holiday: an outbreak-control holiday for 7 d starting on 24 January 2020, with the same length as the Chinese Lunar New Year holiday; ④ 10-day holiday: an outbreak-control holiday for 10 d starting on 24 January 2020; and ⑤ 21-day holiday: an outbreak-control holiday for 21 d starting on 24 January 2020.
2.3.2. Epidemic impact of public holidays for outbreak control with different starting times
In addition, we estimated the cumulative numbers of confirmed infections and all infections for variations in starting time for the base case outbreak-control holiday: ① a 5-day earlier start and ② a 5-day later start.
2.3.3. Epidemic impact of public holidays for outbreak control when other policies are implemented that further reduce transmission rate
We also estimated the cumulative numbers of confirmed infections and all infections for variations in the effectiveness of other epidemic control policies during the outbreak-control holiday: ① a further 50% reduction of the transmission rate during the outbreak-control holiday compared with the base case scenario; and ② a further 90% reduction of the transmission rate.
2.4. “Buying time”: By how many days did the outbreak-control holiday delay epidemic spread?
We further estimated the number of days until specific levels of COVID-19 epidemic spread were reached under the different policy scenarios: ① the number of days until 10 000, 50 000, and 100 000 confirmed infections were reached; and ② the number of days until 50 000 and 100 000 cases of all infections (including confirmed/diagnosed, undiagnosed, and latent infections) were reached. We compared these numbers under the different outbreak-control holiday scenarios against the comparator scenario of “no outbreak-control holiday” to quantify the reductions in epidemic spread caused by the base case outbreak holiday and its variants.
2.5. Role of the funding source
The funders of the study had no role in the study design, data collection, data analysis, data interpretation, or writing of this report.
3. Results
3.1. Epidemic impact of public holidays for outbreak control with different durations
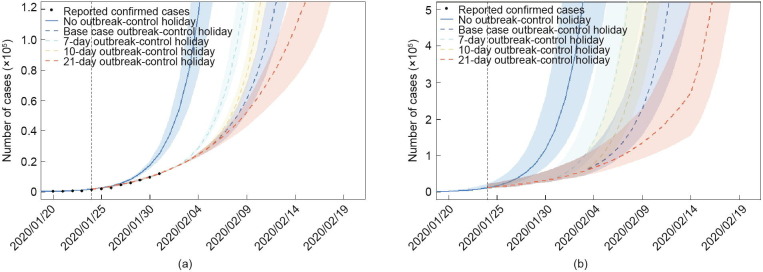
Fig. 1 shows the epidemic impact of the outbreak-control holiday with different durations for the mainland of China. The vertical dashed lines indicate the starting time of the outbreak-control holiday in the base case scenario—that is, 24 January 2020. The dots represent daily cumulative confirmed infections [27]. The outbreak-control holiday significantly reduced infections in comparison with the “no outbreak-control holiday” scenario. The impact of the outbreak-control holiday increased with increasing duration of the holiday. The outbreak-control holiday did not immediately reduce the confirmed infections following the start of the holiday (as shown in Fig. 1(a)) because the COVID-19 incubation period is relatively long and because the holiday started during the early stage of epidemic control. The outbreak-control holiday immediately reduced all infections (as shown in Fig. 1(b)) and delayed epidemic spread in the long run. In Section S3 (in Appendix A), we show the impact of the outbreak-control holiday separately for Hubei Province; in Section S3, we show the impact of the outbreak-control holiday for all other provinces in China.
Fig. 1.
Epidemic impact of an outbreak-control holiday with different durations. (a) Cumulative number of confirmed infections, (b) cumulative number of all infections (including latent and active infection). The solid line represents the model projection for the no outbreak-control holiday scenario, and dashed lines represent the outbreak-control holiday scenarios with varying lengths. The shaded bands represent 95% uncertainty intervals of model outputs.
Compared with the “no outbreak-control holiday” scenario, the base case outbreak-control holiday delayed the time to 50 000 confirmed infections by 6.19 d and the time to 100 000 confirmed cases by 7.54 d. The delay in the time to reach 100 000 total infections was of similar magnitude (Table 1 ). The delay in the time to specific epidemic spread levels increased with the duration of the holiday. For example, a nationwide outbreak-control holiday with a 7-day duration would have increased the time to 100 000 confirmed infections by 4.36 d, while a nationwide outbreak-control holiday with a 21-day duration would have delayed the same number of infections by nearly 10 d.
Table 1.
Impact of outbreak-control holidays on the numbers of days to reach different levels of COVID-19 epidemic spread.
| Scenarios | Effect of outbreak-control holidays on the number of days to reacha |
||||
|---|---|---|---|---|---|
| Confirmed infections |
All infectionsb |
||||
| 10 000 cases | 50 000 cases | 100 000 cases | 50 000 cases | 100 000 cases | |
| Duration | |||||
| No outbreak-control holiday (reference) | ─ | ─ | ─ | ─ | ─ |
| Base case outbreak-control holidayc | 1.48 (1.18, 1.80) | 6.19 (5.00, 7.45) | 7.54 (6.22, 9.06) | 5.09 (3.07, 6.73) | 6.92 (5.65, 8.3) |
| 7-day outbreak-control holiday | 1.48 (1.18, 1.80) | 4.09 (3.44, 4.73) | 4.36 (3.65, 5.04) | 4.00 (3.04, 4.69) | 4.34 (3.66, 5.02) |
| 10-day outbreak-control holiday | 1.48 (1.18, 1.80) | 5.53 (4.58, 6.54) | 6.10 (5.09, 7.11) | 5.08 (3.07, 6.47) | 6.08 (5.06, 7.10) |
| 21-day outbreak-control holiday | 1.48 (1.18, 1.80) | 6.89 (5.42, 8.96) | 9.95 (7.66, 13.26) | 5.11 (3.07, 7.01) | 8.21 (5.85, 11.59) |
| Starting time | |||||
| Base case outbreak-control holiday (reference) | ─ | ─ | ─ | ─ | ─ |
| Base case outbreak-control holiday, 5 d earlier | 5.14 (3.87, 6.48) | 2.46 (1.80, 3.05) | 1.47 (1.02, 1.85) | 3.26 (2.35, 5.20) | 1.96 (1.28, 2.63) |
| Base case outbreak-control holiday, 5 d later | −1.48 (−1.80, −1.18) | −5.19 (−6.53, −3.87) | −4.90 (−6.71, −3.58) | −5.09 (−6.73, −3.07) | −5.99 (−8.04, −4.22) |
| Transmission rate reduction | |||||
| Base case outbreak-control holiday (reference) | ─ | ─ | ─ | ─ | ─ |
| Base case outbreak-control holiday, +50% transmission rate reduction | 1.69 (0.89, 2.21) | 5.57 (3.81, 7.28) | 4.98 (3.45, 6.80) | 6.33 (5.01, 7.72) | 5.46 (3.89, 7.21) |
| Base case outbreak-control holiday, +90% transmission rate reduction | 6.00 (1.96, 8.54) | 9.12 (6.65, 11.88) | 8.19 (5.96, 11.02) | 10.14 (8.06, 12.53) | 8.76 (6.63, 11.47) |
The values in the cells represent the differences in days to reach the specified epidemic levels between a policy scenario and the comparator.
All infections include confirmed/diagnosed, undiagnosed, and latent infections.
3.2. Epidemic impact of public holidays for outbreak control with different starting times
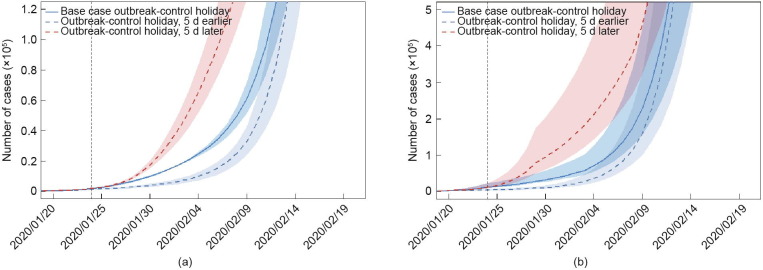
Fig. 2 shows the epidemic impact of the outbreak-control holiday with different starting times. The policy impact increases with earlier starting times. This impact, however, diminishes as the epidemic progresses. If the base case outbreak-control holiday had been implemented 5 d earlier, the time to 10 000 confirmed infections would have been delayed by an additional 5.14 d. However, the earlier implementation would only have caused an additional 1.47-day delay in the time to reach 100 000 confirmed infections. If the base case outbreak-control holiday had been implemented 5 d later than in reality, the impact of the outbreak-control holiday would have been substantially weakened (Fig. 2).
Fig. 2.
Epidemic impact of an outbreak-control holiday with different starting times. (a) Cumulative number of confirmed infections, (b) cumulative number of all infections (including latent and active infection). The solid line represents the base case outbreak-control holiday scenario (with 21 d in Hubei Province and 10 d in all other provinces of China, both starting on 24 January, 2020), and dashed lines represent the outbreak-control holiday scenarios with starting time 5 d earlier and later, respectively. The shaded bands represent 95% uncertainty intervals of model outputs.
3.3. Epidemic impact of public holidays for outbreak control during which the transmission rate is further reduced
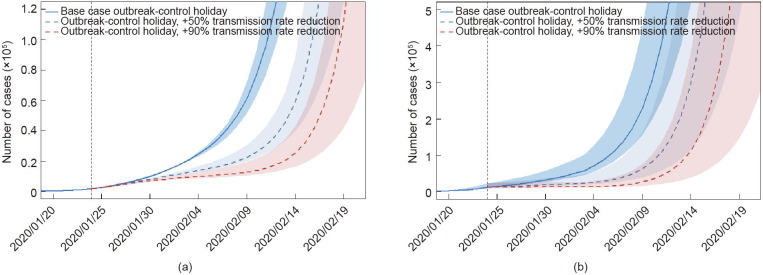
Fig. 3 shows the epidemic impact of the base case outbreak-control holiday in the presence of additional interventions with further effects on the transmission rate. Such interventions could substantially boost the impact of the policy. Compared with the base case outbreak-control holiday with the current calibrated reduction in the transmission rate, reducing the transmission rate by 50% or 90% results in an additional 1.69 and 6.00 d, respectively, to reach 100 000 confirmed infections.
Fig. 3.
Epidemic impact of an outbreak-control holiday with different transmission rates during the holiday. (a) Cumulative number of confirmed infections, (b) cumulative number of all infections (including latent and active infection). The solid line represents the base case outbreak-control holiday scenario (with 21 d in Hubei Province and 10 d in all other provinces of China, both starting on 24 January, 2020), and dashed lines represent the outbreak-control holiday scenarios with transmission rates further reduced by 50% and 90%, respectively, during the holiday period. The shaded bands represent 95% uncertainty intervals of model outputs.
4. Discussion
China’s outbreak-control holiday in the early stages of the COVID-19 epidemic bought a substantial amount of time to prepare for an effective epidemic response. Our model shows that the epidemic spread was substantially dampened by the Chinese Lunar New Year holiday and its subsequent extension by 3 d. The outbreak-control holiday rapidly and significantly reduced the COVID-19 transmission rate—according to our calibration results, to 55% of the pre-holiday rate in Hubei Province and to 45% of the pre-holiday rate in all other provinces of China. The core strategy of the outbreak-control holiday was to substantially reduce social contacts in the population and thus prevent COVID-19 transmission from patients in pre-symptomatic phases. In contrast, without an outbreak-control strategy social contacts may actually intensify during a holiday, because people often meet during holidays and engage in social activities together, potentially exacerbating the spread of an epidemic. During the outbreak-control holiday, the Chinese government people to stay at home and limit social contacts—both directly (e.g., through public information and education campaigns) and indirectly (e.g., by closing public buildings and transport systems) [1]. The outbreak-control holiday further delayed the mass movement of people across China and reduced the contacts that people from Hubei Province had with community members in their Lunar New Year holiday destinations in other provinces of China.
The base case scenario in our analysis was the outbreak-control holiday issued by China’s State Council during the early stage of the epidemic—a 21-day holiday for Hubei province and a 10-day holiday for all other provinces in China. In addition, we separately quantified several important components of this overall impact: the nationwide Lunar New Year holiday, which lasted 7 d; the nationwide extension of the Lunar New Year holiday by 3 days; and the additional 11-day holiday extension in Hubei Province, which brought the total holiday duration in Hubei Province to 21 d. The Lunar New Year holiday induced about half the impact of the overall outbreak-control holiday; the additional extension of the outbreak-control holiday in Hubei Province induced about one fifth of the overall policy impact. As such, the Lunar New Year holiday, whose start incidentally coincided with the emergence of the COVID-19 epidemic, was a major driver of the overall outbreak-control holiday impact. We included the Lunar New Year holiday in the estimate of overall policy impact, because it is likely that the Chinese government would have adopted an outbreak-control holiday around a similar time as the start of the Lunar New Year holiday, if this traditional holiday had not coincided with the early phase of the epidemic. Moreover, the Chinese government already started encouraging people to stay at home and limit social contacts during the traditional holiday [1], effectively changing it into an outbreak-control holiday. Finally, future epidemic outbreaks—which outbreak-control holidays could help contain—are unlikely to coincide again with national public holidays. The overall impact of the entire holiday time, including the Lunar New Year holiday, is thus the most policy-relevant estimate.
Our second key finding is that an outbreak-control holiday is more efficient in delaying epidemic spread the earlier it is implemented and the longer it lasts. While the traditional Lunar New Year holiday coincided with the early stage of the COVID-19 epidemic, the Chinese government acted quickly in using and extending it for outbreak control. It also extended it for a longer time in Hubei Province, the original epicenter of the epidemic. Our findings here should motivate governments facing future epidemics to consider adopting extended outbreak-control holidays in the earliest stages of an emerging epidemic.
In considering such decisions, governments need to weigh the epidemic impact of outbreak-control holidays against other social outcomes, which were not measured in this study. For instance, outbreak-control holidays—even those that are expected—can reduce economic growth [32]. Future research should extend our work to include multiple outcomes of outbreak-control holidays, and to quantify the differential impacts of policy variants, such as implementing outbreak-control holidays at different times in different places.
Our third key finding is that the impact of outbreak-control holidays in delaying epidemic spread will be substantially enhanced if other interventions further reduce transmission rates during the holidays. Such interventions could include contact tracing, community-based management of close contacts of infected people, and environmental disinfection and ventilation.
The goal of our study was not to replicate the entire epidemic trajectory and the control efforts during the COVID-19 epidemic in China, but rather to explore the impact of an outbreak-control holiday that primarily focused on social distancing during the early period of the epidemic and to understand how its duration and starting time would affect the pace of disease transmission in general. Governments can start outbreak-control holidays nearly immediately, because this policy does not require new infrastructures or systems: Governments merely need to announce and publicize the holiday.
In contrast, other outbreak-control policies and approaches take longer to plan and implement, because they require new infrastructures or systems. We used the epidemiological data from the early stage of the epidemic (i.e., during the normal Chinese Lunar New Year holiday before 31 January) to calibrate our model of the COVID-19 transmission dynamic. This selection allows us to isolate the impact of the outbreak-control holiday from the policies and approaches that were implemented later. Such later policies and approaches included the “leave no patient unattended or untreated” strategy, which comprised of mass testing for COVID-19 and facility-based isolation and treatment of patients with both severe and mild COVID-19 [33]. This strategy required new infrastructure. For instance, in February 2020 the Chinese government opened new hospitals for treatment and isolation of COVID-19 patients in Wuhan, Hubei Province, (the Huoshenshan and Leishenshan Hospitals) and implemented facility isolation for patients with mild-to-moderate COVID-19 in so-called Fangcang shelter hospitals [33]. This strategy also required time to build broad social support for mass testing and facility-based isolation [34]. The combined impact of the early outbreak-control holiday and the later policies was that by March 2020 the COVID-19 epidemic was brought under control in the city of Wuhan and in the rest of China [23].
Our results show that if no other measures had been implemented after the outbreak-control holiday, as we assumed in this study, the epidemic spread after the holiday could have returned to the trajectories of nearly exponential growth that were observed before the holiday. That is, an outbreak-control holiday, which mainly enhances social distancing for a finite period of time, should not be expected to be sufficient for epidemic control. Rather, it can merely serve to slow down transmission for some time. This finding indicates that, once an outbreak-control holiday ends and the economy reopens, second-waves are likely—unless people continue preventive measures, such as working from home and maintaining physical distance and wearing masks when outside the home [35].
The main benefit of a public holiday for outbreak control in and of itself is thus that it buys time to develop effective responses that are not immediately available. First, a country can use the time of halted epidemic spread during an outbreak-control holiday to build critical infrastructure for further epidemic control measures, such as emergency field hospitals. Second, the time allows a country to organize medical supplies for the screening, diagnosis, and treatment of COVID-19 patients and to train and deploy specialized human resources for the long-term epidemic response, including hospitalists and infection-control specialists. Finally, the time can be used for scientific discovery and knowledge gain, which is important for designing the most effective and efficient epidemic response for the longer term [36], [37], [38], [39], [40], [41]. During the outbreak-control holiday in China, substantial progress was made toward the characterization and identification of COVID-19 [42], [43], the origin and transmission routes of the virus [17], [18], [41], the epidemiological pattern of the epidemic [28], [44], [45], and potential treatment approaches [46], [47], [48]. At the same time, however, our knowledge of COVID-19 transmission routes remains imperfect, and specific antiviral treatment and vaccines are not yet available [46], [49].
Our study has several limitations. First, we modeled the impact of the outbreak-control holiday policy in China, which included not only time off work but also particular measures to encourage social distancing, such information and education campaigns and the closing of public buildings, spaces, and transport systems. Replication of the impact a public holiday for outbreak control, which we estimated, will thus depend on the precise policy design, even for a very similar future epidemic. Future empirical research should identify the individual impacts of each of the key components of the outbreak-control holiday policy used in China. Second, we did not explicitly capture changing capacity for COVID-19 testing and diagnosis in our model. For the simplicity of model structure, we instead assumed an overall delay in diagnosis after the infected individuals showed symptoms, which was calibrated to the reported confirmed cases. Future modeling work should explore how the impact of outbreak-control holidays changes with growing capacity to test and diagnose COVID-19 and similar diseases as an epidemic progresses. Third, we only estimated the epidemic impact of the outbreak-control holiday, and did not quantify the impact on social and economic outcomes. Future research should identify the impact of the outbreak-control holiday on a range of outcomes and weigh them against each other in a principled way, such as through a cost-benefit analysis.
Taking China as an example, we show that an outbreak-control holiday can substantially dampen COVID-19 epidemic spread. Yet, if the epidemic is not fully contained during the outbreak-control holiday (i.e., there are still undetected cases in the community), cases will surge and eventually return to the trajectories observed before the holiday. Our findings thus emphasize that long-term preventive strategies are needed, which are effective even as people return to work after the holiday. The major benefit of an outbreak-control holiday thus does not lie in long-term epidemic control but in a short-term delay of epidemic spread. This delay can buy time for governments to build infrastructure for prevention and treatment and prepare processes for public health interventions. It can also buy time for scientists to generate the knowledge that can guide policy to increasingly higher levels of impact in controlling COVID-19 and similar epidemics.
Acknowledgments
Acknowledgements
This research was supported by the Bill & Melinda Gates Foundation (INV-006261): “COVID-19: public health governance & service delivery systems in China”, 2020–2022. It was also supported by the Alexander von Humboldt Foundation, through the Alexander von Humboldt Professor award, funded by the Federal Ministry of Education and Research, Germany.
Compliance with ethics guidelines
Simiao Chen, Qiushi Chen, Weizhong Yang, Lan Xue, Yuanli Liu, Juntao Yang, Chen Wang and Till Bärnighausen declare that they have no conflict of interest or financial conflicts to disclose.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.eng.2020.07.018.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
References
- 1.Chen S., Yang J., Yang W., Wang C., Bärnighausen T. COVID-19 control in China during mass population movements at New Year. Lancet. 2020;395(10226):764–766. doi: 10.1016/S0140-6736(20)30421-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Liu Y., Gayle A.A., Wilder-Smith A., Rocklöv J. The reproductive number of COVID-19 is higher compared to SARS coronavirus. J Travel Med. 2020;27(2):1–4. doi: 10.1093/jtm/taaa021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Yin D. China indefinitely shuts schools, extends holiday in effort to control outbreak [Internet]. Beijing: Caixin Global Limited; c2019 [updated 2020 Jan 27; cited 2020 Jan 28]. Available from: https://www.caixinglobal.com/2020-01-27/china-indefinitely-shuts-schools-extends-holiday-in-effort-to-control-outbreak-101508893.html.
- 4.The State Council of the People’s Republic of China. The state council’s announcement on the arrangement of public holidays in 2020 [Internet]. Beijing: The State Council of the People’s Republic of China; 2019 Nov 21 [cited 2020 Feb 3]. Available from: http://www.gov.cn/zhengce/content/2019-11/21/content_5454164.htm. Chinese.
- 5.The State Council of the People’s Republic of China. The state council’s announcement on extending the New Year holiday in 2020 [Internet]. Beijing: The State Council of the People’s Republic of China; 2020 Jan 27 [cited 2020 Jan 31]. Available from: http://www.gov.cn/zhengce/content/2020-01/27/content_5472352.htm. Chinese.
- 6.National Health Commission of the People’s Republic of China. Transcript of the press conference on Jan 26, 2020 [Internet]. Beijing: National Health Commission of the People’s Republic of China; 2020 Jan 26 [cited 2020 Jan 31]. Available from: http://www.nhc.gov.cn/xcs/fkdt/202001/12ec9062d5d041f38e210e8b69b6d7ef.shtml. Chinese.
- 7.Liu W., Yue X.G., Tchounwou P.B. Response to the COVID-19 epidemic: the Chinese experience and implications for other countries. Int J Environ Res Public Health. 2020;17(7):2304–2309. doi: 10.3390/ijerph17072304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Viner R.M., Russell S.J., Croker H., Packer J., Ward J., Stansfield C. School closure and management practices during coronavirus outbreaks including COVID-19: a rapid systematic review. Lancet Child Adolesc Health. 2020;4(5):397–404. doi: 10.1016/S2352-4642(20)30095-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wuhan’s Headquarter on the Novel Coronavirus Prevention and Control. The announcement from Wuhan’s headquarter on the novel coronavirus prevention and control [Internet]. Wuhan: General Office of Hubei Provincial People's Government; 2020 Jan 23 [cited 2020 Jan 31]. Available from: http://www.hubei.gov.cn/zhuanti/2020/gzxxgzbd/zxtb/202001/t20200123_2014402.shtml. Chinese.
- 10.Zhang J., Litvinova M., Liang Y., Wang Y., Wang W., Zhao S. Changes in contact patterns shape the dynamics of the COVID-19 outbreak in China. Science. 2020;368(6498):1481–1486. doi: 10.1126/science.abb8001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Stern A.M., Markel H. What Mexico taught the world about pandemic influenza preparedness and community mitigation strategies. JAMA. 2009;302(11):1221–1222. doi: 10.1001/jama.2009.1367. [DOI] [PubMed] [Google Scholar]
- 12.Poletti P., Caprile B., Ajelli M., Pugliese A., Merler S. Spontaneous behavioural changes in response to epidemics. J Theor Biol. 2009;260(1):31–40. doi: 10.1016/j.jtbi.2009.04.029. [DOI] [PubMed] [Google Scholar]
- 13.Hatchett R.J., Mecher C.E., Lipsitch M. Public health interventions and epidemic intensity during the 1918 influenza pandemic. PNAS. 2007;104(18):7582–7587. doi: 10.1073/pnas.0610941104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ahmed F., Zviedrite N., Uzicanin A. Effectiveness of workplace social distancing measures in reducing influenza transmission: a systematic review. BMC Public Health. 2018;18(1):518. doi: 10.1186/s12889-018-5446-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ferguson N.M., Cummings D.A.T., Cauchemez S., Fraser C., Riley S., Meeyai A. Strategies for containing an emerging influenza pandemic in Southeast Asia. Nature. 2005;437(7056):209–214. doi: 10.1038/nature04017. [DOI] [PubMed] [Google Scholar]
- 16.Glass R., Glass L., Beyeler W., Min H. Targeted social distancing designs for pandemic influenza. Emerg Infect Dis. 2006;12(11):1671–1681. doi: 10.3201/eid1211.060255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Phan L.T., Nguyen T.V., Luong Q.C., Nguyen T.V., Nguyen H.T., Le H.Q. Importation and human-to-human transmission of a novel coronavirus in Vietnam. N Engl J Med. 2020;382(9):872–874. doi: 10.1056/NEJMc2001272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chan J.W., Yuan S., Kok K.-H., To K.-W., Chu H., Yang J. A familial cluster of pneumonia associated with the 2019 novel coronavirus indicating person-to-person transmission: a study of a family cluster. Lancet. 2020;395(10223):514–523. doi: 10.1016/S0140-6736(20)30154-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wang C., Horby P.W., Hayden F.G., Gao G.F. A novel coronavirus outbreak of global health concern. Lancet. 2020;395(10223):470–473. doi: 10.1016/S0140-6736(20)30185-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.United Nations. Coronavirus emergency: here’s what we know so far [Internet]. New York: United Nations; 2020 Feb 3 [cited 2020 Feb 4]. Available from: https://news.un.org/en/story/2020/02/1056562.
- 21.Burki T.K. Coronavirus in China. Lancet Respir Med. 2020;8(3):238. doi: 10.1016/S2213-2600(20)30056-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Tian H., Liu Y., Li Y., Wu C.-H., Chen B., Kraemer M.U.G. An investigation of transmission control measures during the first 50 days of the COVID-19 epidemic in China. Science. 2020;368(6491):638–642. doi: 10.1126/science.abb6105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Pan A.n., Liu L.i., Wang C., Guo H., Hao X., Wang Q.i. Association of public health interventions with the epidemiology of the COVID-19 outbreak in Wuhan, China. JAMA. 2020;323(19):1915–1923. doi: 10.1001/jama.2020.6130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Brauer F., van den Driessche P., Wu J. Springer; Berlin: 2008. Mathematical epidemiology. [Google Scholar]
- 25.Martcheva M. Springer; Berlin: 2015. An introduction to mathematical epidemiology. [Google Scholar]
- 26.Updates on the epidemic [Internet]. Wuhan: Health Commission of Hubei Province; [cited 2020 Jan 31]. Available from: http://wjw.hubei.gov.cn/fbjd/tzgg/. Chinese.
- 27.Updates on the epidemic [Internet]. Beijing: National Health Commission of the People’s Republic of China; [cited 2020 Feb 22]. Available from: http://www.nhc.gov.cn/xcs/yqtb/list_gzbd.shtml. Chinese.
- 28.Li Q., Guan X., Wu P., Wang X., Zhou L., Tong Y. Early transmission dynamics in Wuhan, China, of novel coronavirus-infected pneumonia. N Engl J Med. 2020;382(13):1199–1207. doi: 10.1056/NEJMoa2001316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Stout N.K., Knudsen A.B., Kong C.Y., McMahon P.M., Gazelle G.S. Calibration methods used in cancer simulation models and suggested reporting guidelines. PharmacoEconomics. 2009;27(7):533–545. doi: 10.2165/11314830-000000000-00000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kong C.Y., McMahon P.M., Gazelle G.S. Calibration of disease simulation model using an engineering approach. Value Health. 2009;12(4):521–529. doi: 10.1111/j.1524-4733.2008.00484.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hubei announced to extend Lunar New Year holiday until Feb 13 [Internet]. Beijing: Xinhua Net; [cited 2020 Aug 10]. Available from: http://www.xinhuanet.com/local/2020-02/01/c_1125520350.htm.
- 32.Lin J.L., Liu T.S. Modeling lunar calendar holiday effects in Taiwan. Taiwan Econ Forecast Policy. 2002;33(2):1–37. [Google Scholar]
- 33.Chen S., Zhang Z., Yang J., Wang J., Zhai X., Bärnighausen T. Fangcang shelter hospitals: a novel concept for responding to public health emergencies. Lancet. 2020;395(10232):1305–1314. doi: 10.1016/S0140-6736(20)30744-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Li Z., Chen Q., Feng L., Rodewald L., Xia Y., Yu H. Active case finding with case management: the key to tackling the COVID-19 pandemic. Lancet. 2020;396(10243):63–70. doi: 10.1016/S0140-6736(20)31278-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Maxouris C, Levenson E, Waldrop T. Some US states return to previous restrictions to slow surge of coronavirus cases [Internet]. Atlanta: Cable News Network; c2020 [updated 2020 June 30; cited 2020 Jul 1]. Available from: https://edition.cnn.com/2020/06/29/health/us-coronavirus-monday/index.html.
- 36.Horton R. Offline: 2019-nCoV outbreak—early lessons. Lancet. 2020;395(10221):322. doi: 10.1016/S0140-6736(20)30212-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Heymann D.L. Data sharing and outbreaks: best practice exemplified. Lancet. 2020;395(10223):469–470. doi: 10.1016/S0140-6736(20)30184-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.The Lancet Emerging understandings of 2019-nCoV. Lancet. 2020;395(10221):311. doi: 10.1016/S0140-6736(20)30186-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Huang C., Wang Y., Li X., Ren L., Zhao J., Hu Y.i. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395(10223):497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Chen N., Zhou M., Dong X., Qu J., Gong F., Han Y. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020;395(10223):507–513. doi: 10.1016/S0140-6736(20)30211-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Lu R., Zhao X., Li J., Niu P., Yang B.o., Wu H. Genomic characterisation and epidemiology of 2019 novel coronavirus: implications for virus origins and receptor binding. Lancet. 2020;395(10224):565–574. doi: 10.1016/S0140-6736(20)30251-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Zhu N., Zhang D., Wang W., Li X., Yang B., Song J. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020;382(8):727–733. doi: 10.1056/NEJMoa2001017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Zhou P., Yang X.L., Wang X.G., Hu B., Zhang L., Zhang W. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature. 2020;579(7798):270–273. doi: 10.1038/s41586-020-2012-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Epidemiology Working Group for NCIP Epidemic Response of the Chinese Center for Disease Control and Prevention. The epidemiological characteristics of an outbreak of 2019 novel coronavirus diseases (COVID-19) in China. Chin J Epidemiol 2020;41(2):145–51. Chinese.
- 45.Guan W., Ni Z., Hu Y., Liang W., Ou C., He J. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382:1708–1720. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Richardson P., Griffin I., Tucker C., Smitha D., Oechslea O., Phelan A. Baricitinib as potential treatment for 2019-nCoV acute respiratory disease. Lancet. 2020;395(10223):e30–e31. doi: 10.1016/S0140-6736(20)30304-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Cao B., Wang Y., Wen D., Liu W., Wang J., Fan G. A trial of lopinavir–ritonavir in adults hospitalized with severe COVID-19. N Engl J Med. 2020;382:1787–1799. doi: 10.1056/NEJMoa2001282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Wang Y., Zhang D., Du G., Du R., Zhao J., Jin Y. Remdesivir in adults with severe COVID-19: a randomised, double-blind, placebo-controlled, multicentre trial. Lancet. 2020;395(10236):1569–1578. doi: 10.1016/S0140-6736(20)31022-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Wang F.S., Zhang C. What to do next to control the 2019-nCoV epidemic? Lancet. 2020;395(10222):391–393. doi: 10.1016/S0140-6736(20)30300-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.