Abstract
Purpose
Congenital penile curvature (CPC) is a rare condition with surgical correction being the standard therapy. In the current study, we report long-term results analyzing the surgical and functional outcomes using a modified Nesbit technique.
Materials and Methods
Patients with CPC were included. After penile degloving and mobilization of the neurovascular bundle an artificial erection was performed. An ellipsoid part of the tunica albuginea was excised at the point of maximum curvature on the convex side of deviation. The tunical defect was then closed by interrupted absorbable sutures with inverted knots. Results of correction were documented intra- and postoperatively by artificial erection. Pre- and postoperative evaluation included measurement of penile length and curvature after pharmacological erection. Erectile function, alteration in glans sensation, palpable suture as well as short- and long-term complication were also recorded using validated questionnaires and objective examinations.
Results
Fifty-five patients with mean age 26.93 years (14–66 years) and mean curvature 69.81° (25°–90°) were included in the study. Ventral or ventrolateral curvature was observed in 83.6%. Mean operative time was 106.8 minutes (55–169 minutes). Totally straightness of the penis was achieved in 51/55 patients (92.8%). After a mean long-term follow-up of 36.68 months (4–87 months), erectile function worsened in 3.6% of patients. Median penile length loss associated with this technique was 1.7 cm (0–3.0 cm).
Conclusions
Surgical therapy of CPC using our modified Nesbit technique is feasible, safe and provides reliable long-term outcomes, representing an alternative for surgical correction of CPC.
Keywords: Congenital, Erectile dysfunction, Operative surgical procedures, Penile diseases, Penile induration, Reconstructive surgical procedures
INTRODUCTION
Congenital penile curvature (CPC) is a relatively uncommon condition, that differs from Peyronie's disease [1]. It can be mistakenly considered similar to Peyronie's disease because of the similar physical manifestations, but the aetiology and pathophysiology are different [2]. CPC is considered to be a result of abnormal development of the tunica albuginea of the corpora cavernosa with increased elasticity of the tunica on the convex side of the curvature [3]. Although CPC can be rarely associated with urethral plate malformation, such as hypospadias, epispadias or shortened urethral plate, the typical clinical manifestation is an isolated penile deviation, which usually occurs ventrally, with an orthotopic meatus [4]. CPC tends to present in late adolescent or early adult life, when the patients may be concerned with the aesthetic or functional aspects of their penis [1]. However, the severity and direction of the curvature can vary and can even make sexual intercourse practically impossible. Many studies reported that patients with a curvature of more than 30° will eventually seek treatment [3].
Surgical correction of CPC is the gold standard treatment in affected patients. Various surgical techniques have been reported for the treatment of penile curvature [5]. Most surgical corrective procedures start with complete penile degloving and artificial erection, but there are authors reporting satisfactory results performing small incisions at the site of maximum curvature [3]. The first reported technique for CPC was described by Nesbit [6], consisting of excision of horizontal ellipse(s) of the tunica albuginea on the convex side of the curvature and close with non-absorbable sutures. Many authors have described modifications of the Nesbit technique, trying to reduce penile shortening, the mobilisation of the neurovascular bundle, and postoperative palpable sutures or suture granulomas [7,8]. In 1985, Essed and Schroeder [9] as well as Ebbehøj and Metz [10] separately proposed an incisionless plication technique of the tunica albuginea, minimizing the risk of injury to neurovascular bundle as well as decreasing the complexity and time of the procedure. The length-preserving grafting techniques, usually used in Peyronie's disease, are not commonly used in the treatment of CPC, since CPC patients with isolated penile curvature tend to have above average penile length [11].
Most of the studies regarding the treatment of CPC are small retrospective cohorts (<30 patients) with short terms results and inconsistent or incomplete reporting of outcomes and/or complication without using standardized tools. Furthermore, some of the studies included a variety of performed surgical techniques performed by many surgeons [12]. We present the long-term results, analysing the outcomes (surgical and functional) and complications after the surgical repair of CPC by a single surgeon using a modified Nesbit technique.
MATERIALS AND METHODS
1. Ethics statement
From February 2008 to January 2018, we retrospectively included patients with CPC of >25° and indication for surgical repair of the curvature. We prospectively reached the patients for a follow-up visit. In lieu of a formal ethics committee, the principles of the Helsinki Declaration were followed during the present study. Informed consent was submitted by all subjects when they were enrolled. All patients were informed about the surgical procedure in detail and realistic expectations were pointed out. Moreover, risks, complications and potential outcomes of surgery were discussed preoperatively.
2. Study design
Inclusion criteria for surgical treatment were the diagnosis of CPC, penile curvature leading to difficulty or inability for sexual intercourse but erection hardness score (EHS) ≥3 after artificial erection. Exclusion criteria were erectile dysfunction refractory to phosphodiesterase type 5 inhibitors or intracavernous injections, patients with psychological or psychiatric conditions, the presence of hypospadias or other congenital anomalies of the penis, as well as penile curvature less than 25°.
Pre- and postoperative evaluation consisted of detailed medical history, physical examination including sonography and artificial erection of the penis using intracavernosal Alprostadil (Caverject®; Pfizer, New York, NY, USA), in order to objectively assess the penile curvature or straightening and EHS. For complex curvatures the degrees of the curvature were measured separately for the primary and secondary curvature. Erectile function was, moreover, assessed by the international index of erectile function questionnaire-erectile function (IIEF-EF) domain and sexual encounter profile questions (SEP1-SEP5). Further questionnaires to assess the overall physical and mental wellbeing were given to the patients at follow-up: international prostate symptom score (IPSS), Center for Epidemiologic Studies Depression (CES-D) Scale, aging male symptom score (AMS) and 12-Item Short Form Health Survey (SF-12). Patients displaying an EHS of 3 or 4 were included in the study. On all the patients was performed the same modified Nesbit technique.
The postoperative outcome was considered successful when complete straightness of the penis was achieved without major long-term complications. Complete straightness at the time of follow-up was defined as no evidence of curvature or residual curvature of less than 15°. Erect penile length and curvature was measured pre- and postoperatively during artificial erection. Length's measurement was done from the pubic bone to the tip of the glans [13]. As adequate length measurement in case of severe curvature is difficult, the concave side of curvature was measured in these cases (from point of maximum curvature to pubic bone and to tip of glans). In order to record systematically possible early and long-term postoperative complication at follow-up a standardised check-list accompanied by the above-mentioned questionnaires were used.
3. Surgical technique
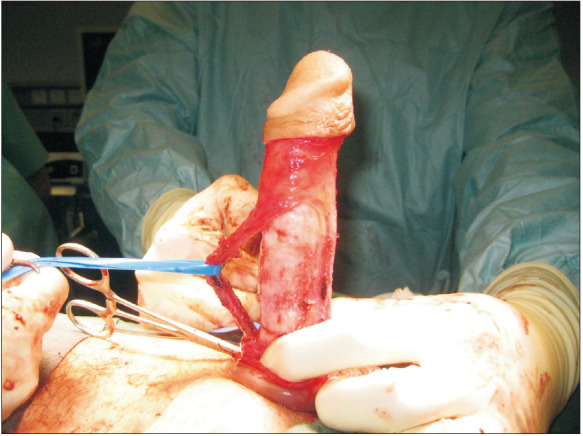
Surgery was performed in general anaesthesia. First, a circumcising skin incision followed by penile degloving was performed. After lateral dissection and mobilization of the neurovascular bundle or the urethra, which allows maximum exposure of the corpora cavernosa, an artificial erection was performed to assess the degree of deformity and the point of maximum curvature (Fig. 1, 2). Depending on the curvature, one or more ellipsoid part(s) of the tunica albuginea were excised at the point of maximum curvature on the convex side of curvature (Fig. 3, 4). The tunical defect was then closed by interrupted absorbable PDS 2-0 sutures with inverted/buried knots (Fig. 5). Penile straightening was documented intraoperatively by artificial erection (Fig. 6). In the next step, the neurovascular bundle was reapproximated and Buck's fascia was closed. Then the penile skin is closed, usually performing a circumcision. Loosely dressing is put around the penis at the end of surgery. A transurethral catheter is placed during surgery and left for 3 days.
Fig. 1. Intraoperative photo showing the basic steps in our modified Nesbit technique in a typical congenital penile curvature patient with 70° curvature: intraoperative artificial erection after penile degloving and lateral mobilization of the neurovascular bundle marking the point of maximum curvature in the convex side of the curvature.
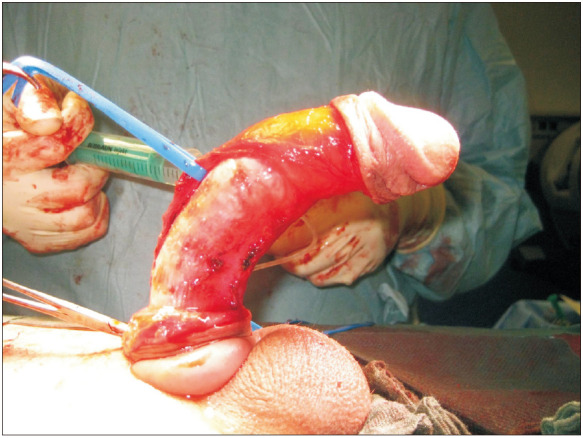
Fig. 2. Intraoperative photo showing the basic steps in our modified Nesbit technique in a typical congenital penile curvature patient with 70° curvature: the complete mobilization of the neurovascular bundle.
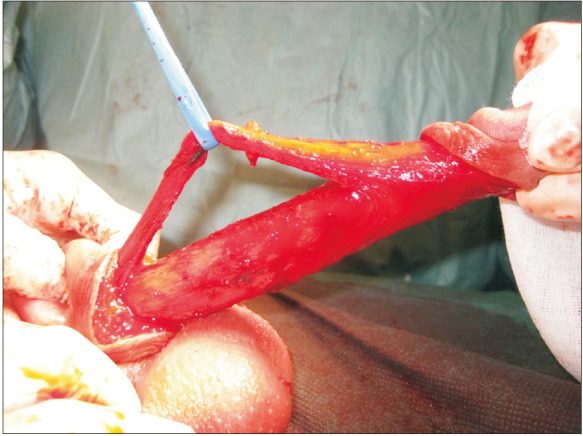
Fig. 3. Intraoperative photo showing the basic steps in our modified Nesbit technique in a typical congenital penile curvature patient with 70° curvature: excision of an ellipsoid part of the tunica albuginea at the convex side of the curvature.
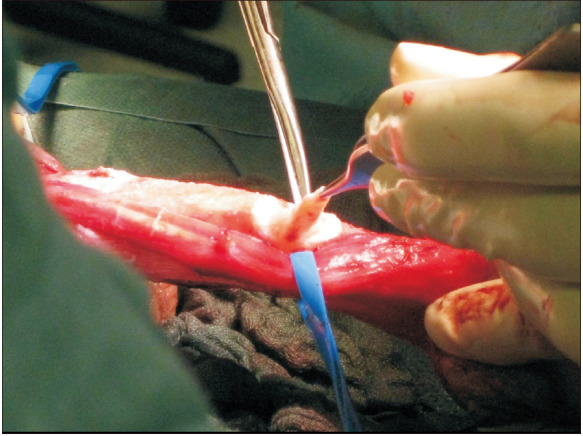
Fig. 4. Intraoperative photo showing the basic steps in our modified Nesbit technique in a typical congenital penile curvature patient with 70° curvature: showing the intact erectile tissue after excision of the tunica.
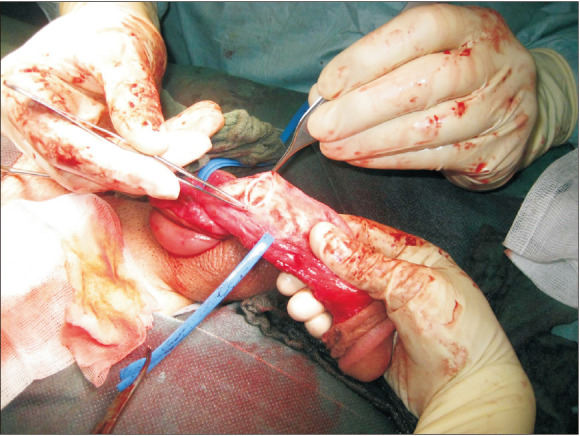
Fig. 5. Intraoperative photo showing the basic steps in our modified Nesbit technique in a typical congenital penile curvature patient with 70° curvature: closing the defect in the tunica with absorbable PDS 2-0 and inverted/buried knots.
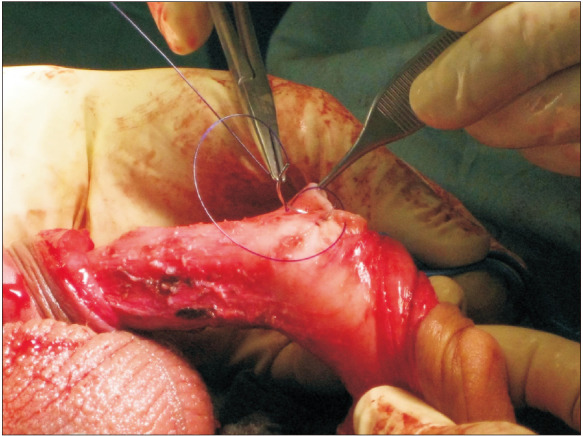
Fig. 6. Intraoperative photo showing the basic steps in our modified Nesbit technique in a typical congenital penile curvature patient with 70° curvature: artificial erection after closing the tunical defect showing a complete straightening of the penis.
4. Statistical analysis
The continuous values of the patients' data are presented as mean values±standard deviations, along with the respected range (minimum–maximum value). All the analyses were performed using IBM SPSS ver. 20.0 software (IBM Corp., Armonk, NY, USA). For comparisons between the quantitative variables the Student's pair t-test was used, where there was a regular distribution of data or the Wilcoxon signed-rank test, where the data followed a non-parametric distribution. For the comparison of categorical variables (proportions and rates), the chi-square test or Fisher's exact test was used depending on the number of categories of each variable.
RESULTS
From February 2008 to January 2018, 55 patients with CPC underwent a modified Nesbit (excisional corporoplasty) technique for curvature correction. The mean age at the time of surgery was 26.93±9.52 years ranging from 14–66 years. The direction of the curvature varied with the majority of the patients (83.6%) having a ventral or ventrolateral curvature. The mean primary curvature was 69.81°±16.76° (range: 25°–90°). Six patients (10.9%) had undergone previous surgical treatment for CPC. Mean operative time was 106.8±28.1 minutes (range: 55–169 minutes). The clinical characteristics of the patients are analytically shown in Table 1. Intraoperatively, penile curvature was corrected completely in all the patients, except for 4 patients (7.2%) who showed a dorsal hypercorrection of 10° to 15° at the end of surgery.
Table 1. Clinical characteristics of patients.
| Characteristic | Value |
|---|---|
| No. of patient | 55 |
| Age (y) at time of surgery | 26.93±9.52 (14–66) |
| BMI (kg/m2) | 23.61±3.09 (18–32) |
| Follow-up (mo) | 36.68±27.70 (4–87) |
| Direction congenital penile curvature at presentation (total=55) | |
| Ventral | 35 (63.6) |
| Lateral left | 6 (10.9) |
| Dorsal | 1 (1.8) |
| Ventrolateral | 11 (20.0) |
| Dorsolateral | 2 (3.6) |
| Direction of primary curvature at presentation (total=55) | |
| Ventral | 46 (83.6) |
| Lateral left | 8 (14.5) |
| Dorsal | 1 (1.8) |
| Angle of primary curvature at presentation (°) | 69.81±16.76 (25–90) |
| Ventral (n=46) | 72.4±14.9 (25–90) |
| Lateral left (n=8) | 53.1±18.3 (25–75) |
| Dorsal (n=1) | 85a |
| Direction of secondary curvature at presentation (total=13) | |
| Lateral left | 9 (69.2) |
| Lateral reight | 2 (15.4) |
| Dorsal | 2 (15.4) |
| Angle of secondary curvature at presentation (°) | 20.42±11.76 (10–50) |
| Lateral left (n=9) | 21.2±13.5 (25–90) |
| Lateral reight (n=2) | 17.5±3.5 (25–75) |
| Dorsal (n=2) | 20.0±14.4 (10–30) |
| Previous surgical treatment for CPC (total=55) | 6 (10.9) |
| No. of tunical excision | 2.36±0.91 (1–5) |
| Operative time (min) | 106.8±28.1 (55–169) |
| Hospitalization (d) | 5.3±1.7 (3–11) |
Values are presented as number only, mean±standard deviation (range), or number (%) unless other indicated. The sum of the percentages does not equal 100% because of rounding.
BMI: body mass index, CPC: congenital penile curvature.
aMean value.
After a mean follow-up of 36.68±27.70 months (4–87 months), only two patients reported a partial recurrence of curvature of less than 40°, which did not interfere with sexual intercourse and did not require additional treatment. The remaining patients showed a complete straight penis at follow-up. All patients were able to perform satisfying sexual intercourse. According to the IIEF-EF score, erectile function slightly improved or remained unchanged in the majority of patients and worsened in 3.6% of the cohort. The EHS score was 3 or 4 in all the patients at the time of follow-up. Postoperative scores (IIEF-EF, EHS, SEP) regarding sexual function improved, without reaching statistical significance, except from SEP5 question which was significant improved (p=0.034). Mean erect penile length before surgery and at follow-up was 16.8±1.3 cm and 14.2±1.6 cm, respectively (p=0.011), with a median penile length loss associated with this technique of 1.7 cm (range: 0–3.0 cm). Patient satisfaction rate was as high as 90.9%, while overall success rate reached 92.8%. Transient decreased sensation at glans penis occurred in 16.4% of patients. Palpable suture knots were observed in 23.6% of the patients, but bothersome were reported only from 7.3% of the patients. Outcomes and complications of this study are shown in detail in Table 2 and 3.
Table 2. Postoperative outcomes.
| Variable | At baseline | Postoperative | p-value |
|---|---|---|---|
| Penile deviation (total=55) | |||
| Yes | 55 (100) | 8 (14.5) | <0.0001* |
| No | 0 (0) | 47 (85.5) | |
| Angle of deviation (°) | 69.81±16.76 (25–90) | 2.45±7.5 (0–40) | <0.0001* |
| Penile length (cm) | 16.8±1.3 | 14.2±1.6 | 0.011* |
| EHS | 3.6±0.7 | 3.8±0.4 | 0.419 |
| IIEF-EF domain | 26.16±4.8 | 28.53±2.7 | 0.079 |
| SEP1 (% of yes) | 95.5 | 100 | 0.784 |
| SEP2 (% of yes) | 63.6 | 77.3 | 0.493 |
| SEP3 (% of yes) | 73.7 | 72.7 | 0.667 |
| SEP4 (% of yes) | 81.0 | 95.2 | 0.317 |
| SEP5 (% of yes) | 52.4 | 80.0 | 0.034* |
| IPSS | 2.18±2.8 | 3.7±4.0 | 0.051 |
Values are presented as number (%), mean±standard deviation (range), percent only.
EHS: erection hardness score, IIEF-EF: international index of erectile function questionnaire-erectile function, SEP: sexual encounter profile question, IPSS: international prostate symptom score.
*Asterisk indicates a statistically significant (p<0.05).
Table 3. Early and long-term complications.
| Complication | Value |
|---|---|
| Hematoma (total=55) | 8 (14.5) |
| Wound Infection/abscess (total=55) | 3 (5.5) |
| Recurrence of curvature (total=55) | 2 (3.6) |
| Revision surgery | 5 (9.1) |
| Aetiology for revision (total=5) | |
| Hematoma | 3 (60.0) |
| Abscess | 2 (40.0) |
| Recurrence of curvature | 0 (0) |
| Palpable suture knot (total=55) | 34 (61.8) |
| Subjective bothersome from palpable suture (total=55) | 9 (16.4) |
| Decreased sensation at glans penis (total=55) | 9 (16.4) |
| Loss of distal rigidity of penis (total=55) | 0 (0) |
| Subjective loss of penile length (total=55) | 21 (38.2) |
| Loss of penile length affected QoL (total=55) | 5 (9.1) |
| Worsening of erectile function (total=55) | 2 (3.6) |
Values are presented as number (%).
QoL: quality of life.
At follow-up we further assessed the overall physical and mental wellbeing of the patients. The IPSS score remained low (as expected due to the young age of the patients) both pre- and postoperatively (2.18±2.8 vs. 3.7±4.0, p=0.051). The mean AMS score were 24.6±8.8, which remained below 26, meaning that our cohort did not show significant symptoms consistent with a low testosterone level after surgery. The overall physical health measured by SF-12 physical sub-score was 52.3±6.6, showing an above average physical health. Mental health was assessed with SF-12 mental subscore as well as CES-D score, 51.2±9.0 and 10.1±8.8, respectively, showing an overall good mental health after surgery in our cohort.
DISCUSSION
CPC is a relatively uncommon condition. Surgical correction of CPC is the gold standard treatment in affected patients [3]. CPC tends to present in late adolescent or early adult life, when the patients may be concerned with the aesthetic or functional aspects of their penis [1]. Various surgical techniques have been reported for the treatment of penile curvature, mostly consisting from plication techniques (excisional or incisional corporoplasty, or incisionless plication), while grafting techniques are rarely reported [3,14]. The majority of studies until now are small retrospective cohorts, without standardized measurement and/or recording of postoperative outcomes and complications. This resulted in data of low level of evidence regarding CPC when compared to Peyronie's disease. Our study is one of the few studies with standardized documentation of the postoperative outcomes.
A number of retrospective studies compared the outcomes of excisional/incisional corporoplasty procedures to incisionless plication techniques which showed that while there is decreased risk of complications, there is an increased risk of recurrence associated with incisionless plication [15,16,17]. Two of them reported overall better outcomes in patients treated with the Nesbit or modified Nesbit techniques [16,17]. We also used a modified Nesbit technique, performing an excisional corporoplasty at the convex side of the curvature after lateral dissection and mobilization of the neurovascular bundle or the urethra. The penile straightening rate or success rate of older excisional corporoplasty studies ranged from 83% to almost 100% [3,18,19], which is comparable to our penile straightening rate of 92.8%. On the other hand, there are incisional corporoplasty and incisionless plication studies that reported success rates as low as 77% and 73%, respectively [20,21]. In this regard it should be mentioned that a less than 15° residual curvature was defined as complete straight, which is a common practise compared to the literature [1,5]. Two patients showed a residual curvature of 25° and 40°, respectively, at the time of follow-up, which did not interfere with sexual intercourse. It is important to mention that these patients showed a severe ventral curvature before surgery. Considering this, a mild residual curvature at follow-up can be regarded as a successful outcome in these cases. This is reflected by the fact that sexual intercourse at follow-up was also possible in these cases. Adequate preoperative counselling of patients is of utmost importance, and realistic expectations have to be discussed, particularly in such severe cases.
Except penile straightening, there are 3 other major postoperative concerns regarding the surgical correction of CPC, irrespectively of the technique used. These are the postoperative penile shortening, the postoperative decreased sensation at glans penis (usually transient) and the palpable sutures or granulomas [22]. Penile shortening is more a sequela of every plication technique rather than a complication. Shortening of the penis is dependent on direction and degree of curvature, as well as the length of the phallus [23]. Since the ventral direction of the curvature is also associated with the most loss in penile length [23], patients with CPC are in increased risk of postoperative significant penile shortening. In our study, the median penile length loss of 1.7 cm is similar to other studies especially if we take into account the fact that we had a rather difficult to treat cohort of patients with ventral curvature in 83% of them and with a mean angle of 69.8°.
The mobilisation of the neurovascular bundle is considered responsible for the transient postoperative decreased sensation at glans penis. Glans hypaesthesia may lead to diminished sensations during sexual activity. However, even if present, this usually does not interfere with sexual intercourse [24]. Many surgeons modified the Nesbit technique in order to avoid the mobilisation of the neurovascular bundle [19,25]. The incidence of decrease glans sensation in these studies ranged from 0% to 1.6%, but was underreported in the majority of the studies [3]. Leonardo et al [15] studied outcomes of 31 patients with CPC with a mean follow up of 39 months comparing the Nesbit technique (excisional corporoplasty) with incisionless plication. 75% of patients undergoing the Nesbit procedure reported paraesthesia of the glans as compared to 37% in plication group. In our study, it was observed in 12% of the patients postoperatively and was only transient in all of them lasting from a few days and up to 3 months.
Another relative bothersome sequala of all plication techniques is the postoperative palpable suture at the site of plication. Although almost all patients feel a suture at the site, it is usually not bothersome. In studies comparing Nesbit with incisionless plication, patients' discomfort and ability to feel the sutures during erection was more prominent in the incisionless plication group, making patients most likely to complain of palpable sutures (around 21%) [15,16,17]. In our study, the tunical defect was closed with interrupted absorbable PDS 2-0 sutures with inverted/buried knots. This technique allows to minimize the incidence of bothersome palpable knots, showing a palpable suture in only 61% of the patients with subjective bother during erection in less than one third of them (16.4%). The rate of postoperative palpable sutures was objectively assessed through physical examination in the follow-up visit. Therefore, the demonstrated rate of palpable knots could be higher than the subjective report of the patients, commonly used in other studies [14]. Furthermore, the tunical tissue have a high rate of inflammatory reaction to foreign bodies, which results into the development of granulomas in the site of the sutures [26]. Therefore, even if we use an absorbable suture, postoperative palpable knots could emerge. In cases of excisional or incisional plication corporoplasty of the tunica, retrospective studies have showed that the use of absorbable sutures does not increase the recurrence rate of the curvature. On the other hand, the suture seems to play an important role in incisionless plication techniques, with higher recurrence rates when using an absorbable suture [14].
Another important aspect is erectile function after surgery, as, according to the literature, this is slightly more common with excisional/incisional corporoplasty compared to incisionless plication [15,16,17]. Thus, patient selection is key to success. Patients should have adequate erectile function preoperatively. Mean IIEF-EF score in the present study was 26.16±4.8 points before surgery and raised up to 28.53±2.7 afterwards without reaching statistical significance (p=0.079). Moreover, all patients showed an EHS of 3 or 4 during artificial erection test, pre- and postoperatively. In this regard it should be highlighted that the IIEF questionnaire for assessment of erectile function is not validated for patients with Peyronie's disease. It is hard to think that erectile function is improved after excisional corporoplasty in patients with CPC. In the best case, erectile function will be unchanged compared to the preoperative status. The reason why the IIEF-EF score is improved after surgery is the fact that many patients were unable to engage in sexual intercourse before surgery. However, after surgery when the penis is straight, sexual intercourse is possible which leads to increased IIEF-EF scores. The EHS provides a more objective and adequate way of assessing erectile function, especially during intracavernosal injection test, and should be preferred in this regard. Furthermore, through the SEP questions we observed an overall improvement in sexual function and sexual satisfaction in our study.
The incidence of postoperative haematoma and infection remained low but slightly higher that other studies in the literature (Table 3). This could be explained by the fact that our study was performed with standardized documentation of all outcomes and complication, when compared to previous studies in the literature [3]. This reduces the recall bias meaning that the reported incidence of postoperative haematoma and infection could be underreported in previous studies. Furthermore, our study's cohort consisted of rather difficult to treat patients with mean curvature of 69.81° (clearly larger than other studies in the literature) and with 10.9% of the patients having recurrence of the curvature after surgical treatment in other centres. The observed complications were treated successfully in all the patients and did not affect the outcomes and success rates.
Despite the encouraging results of our study, there are some limitations that have to be considered. This study included only 55 patients who underwent our modified excisional corporoplasty technique. However, given the fact that CPC represents a relatively uncommon condition, that differs from Peyronie's disease, this number represents an adequate population. Our study's cohort consisted of rather difficult to treat patients with mean curvature of 69.81° and 10.9% previously treated. These difficult-to-treat cases are uncommon outside reference centres. Langer multicentre prospective studies as well as randomized clinical trials comparing the available techniques are needed to enlighten the treatment modalities in patients with CPC.
CONCLUSIONS
In conclusion, patients with CPC can expect excellent outcomes and minimal side effects with the described modified Nesbit technique, providing reliable long-term outcomes and representing an alternative for surgical correction of CPC. The advantages and disadvantages of each method as well as the possible associated complications vary and should be discussed with the patient pre-operatively in order to ensure appropriate patient expectations and increase satisfaction rates. The surgeon's personal experience with a specific technique seems to play an important role in the selection of the treatment as well as the postoperative results.
Footnotes
Conflict of Interest: The authors have nothing to disclose.
- Conceptualization: GH, IS.
- Data curation: PS, IM.
- Formal analysis: IS, PS.
- Investigation: PS, GH.
- Methodology: IS, IM, GH.
- Resources: JG, SL, HK.
- Software: JG, HK.
- Supervision: SL, JG, GH.
- Validation: HK, GH.
- Visualization: GH.
- Writing—original draft: IS, PS, IM.
- Writing—review & editing: HK, JG, SL, GH.
Data Sharing Statement
The data analyzed for this study have been deposited in HARVARD Dataverse and are available at https://doi.org/10.7910/DVN/ILQF81.
References
- 1.Yachia D, Beyar M, Aridogan IA, Dascalu S. The incidence of congenital penile curvature. J Urol. 1993;150:1478–1479. doi: 10.1016/s0022-5347(17)35816-0. [DOI] [PubMed] [Google Scholar]
- 2.Baskin LS, Duckett JW, Lue TF. Penile curvature. Urology. 1996;48:347–356. doi: 10.1016/S0090-4295(96)00213-0. [DOI] [PubMed] [Google Scholar]
- 3.Makovey I, Higuchi TT, Montague DK, Angermeier KW, Wood HM. Congenital penile curvature: update and management. Curr Urol Rep. 2012;13:290–297. doi: 10.1007/s11934-012-0257-x. [DOI] [PubMed] [Google Scholar]
- 4.Donnahoo KK, Cain MP, Pope JC, Casale AJ, Keating MA, Adams MC, et al. Etiology, management and surgical complications of congenital chordee without hypospadias. J Urol. 1998;160:1120–1122. doi: 10.1097/00005392-199809020-00041. [DOI] [PubMed] [Google Scholar]
- 5.Hatzichristodoulou G. Advances in the surgical treatment of Peyronie's disease. Current Sex Health Rep. 2016;8:186–192. [Google Scholar]
- 6.Nesbit RM. Congenital curvature of the phallus: report of three cases with description of corrective operation. J Urol. 1965;93:230–232. doi: 10.1016/S0022-5347(17)63751-0. [DOI] [PubMed] [Google Scholar]
- 7.Yachia D. Modified corporoplasty for the treatment of penile curvature. J Urol. 1990;143:80–82. doi: 10.1016/s0022-5347(17)39871-3. [DOI] [PubMed] [Google Scholar]
- 8.Baskin LS, Lue TF. The correction of congenital penile curvature in young men. Br J Urol. 1998;81:895–899. doi: 10.1046/j.1464-410x.1998.00645.x. [DOI] [PubMed] [Google Scholar]
- 9.Essed E, Schroeder FH. New surgical treatment for Peyronie disease. Urology. 1985;25:582–587. doi: 10.1016/0090-4295(85)90285-7. [DOI] [PubMed] [Google Scholar]
- 10.Ebbehøj J, Metz P. New operation for “krummerik” (penile curvature) Urology. 1985;26:76–78. doi: 10.1016/0090-4295(85)90264-x. [DOI] [PubMed] [Google Scholar]
- 11.Hatzichristodoulou G, Osmonov D, Kübler H, Hellstrom WJG, Yafi FA. Contemporary review of grafting techniques for the surgical treatment of Peyronie's disease. Sex Med Rev. 2017;5:544–552. doi: 10.1016/j.sxmr.2017.01.006. [DOI] [PubMed] [Google Scholar]
- 12.Paez A, Mejias J, Vallejo J, Romero I, De Castro M, Gimeno F Grupo Urologico del Suroeste Madrileno (GUSOM) Long-term patient satisfaction after surgical correction of penile curvature via tunical plication. Int Braz J Urol. 2007;33:502–507. doi: 10.1590/s1677-55382007000400007. [DOI] [PubMed] [Google Scholar]
- 13.Habous M, Muir G, Soliman T, Farag M, Williamson B, Binsaleh S, et al. Outcomes of variation in technique and variation in accuracy of measurement in penile length measurement. Int J Impot Res. 2018;30:21–26. doi: 10.1038/s41443-017-0013-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sokolakis I, Hatzichristodoulou G. Current trends in the surgical treatment of congenital penile curvature. Int J Impot Res. 2019 doi: 10.1038/s41443-019-0177-0. [Epub] [DOI] [PubMed] [Google Scholar]
- 15.Leonardo C, De Nunzio C, Michetti P, Tartaglia N, Tubaro A, De Dominicis C, et al. Plication corporoplasty versus Nesbit operation for the correction of congenital penile curvature. A long-term follow-up. Int Urol Nephrol. 2012;44:55–60. doi: 10.1007/s11255-011-9976-z. [DOI] [PubMed] [Google Scholar]
- 16.Nyirády P, Kelemen Z, Bánfi G, Rusz A, Majoros A, Romics I. Management of congenital penile curvature. J Urol. 2008;179:1495–1498. doi: 10.1016/j.juro.2007.11.059. [DOI] [PubMed] [Google Scholar]
- 17.Poulsen J, Kirkeby HJ. Treatment of penile curvature--a retrospective study of 175 patients operated with plication of the tunica albuginea or with the Nesbit procedure. Br J Urol. 1995;75:370–374. doi: 10.1111/j.1464-410x.1995.tb07351.x. [DOI] [PubMed] [Google Scholar]
- 18.Colpi G, Piediferro G, Castiglioni F, Contalbi G, Carmignani L. Penile septoplasty for congenital ventral penile curvature: results in 51 patients. J Urol. 2009;182:1489–1494. doi: 10.1016/j.juro.2009.06.059. [DOI] [PubMed] [Google Scholar]
- 19.Perdzyński W, Adamek M. Three anatomical levels: possibilities to decrease invasiveness of reconstructive surgery for congenital penile curvature. Cent European J Urol. 2017;70:280–288. doi: 10.5173/ceju.2017.1509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mayer M, Rey Valzacchi G, Silva Garretón A, Layus O, Gueglio G. Patient satisfaction with correction of congenital penile curvature. Actas Urol Esp. 2018;42:414–419. doi: 10.1016/j.acuro.2017.11.002. [DOI] [PubMed] [Google Scholar]
- 21.Hsieh JT, Liu SP, Chen Y, Chang HC, Yu HJ, Chen CH. Correction of congenital penile curvature using modified tunical plication with absorbable sutures: the long-term outcome and patient satisfaction. Eur Urol. 2007;52:261–266. doi: 10.1016/j.eururo.2006.12.033. [DOI] [PubMed] [Google Scholar]
- 22.Hatzichristodoulou G, Lahme S. Peyronie's disease. In: Merseburger AS, Kuczyk MA, Moul JW, editors. Urology at a glance. Berlin-Heidelberg: Springer-Verlag Berlin Heidelberg; 2014. pp. 225–236. [Google Scholar]
- 23.Greenfield JM, Lucas S, Levine LA. Factors affecting the loss of length associated with tunica albuginea plication for correction of penile curvature. J Urol. 2006;175:238–241. doi: 10.1016/S0022-5347(05)00063-7. [DOI] [PubMed] [Google Scholar]
- 24.Hatzichristodoulou G. Introducing the ventral sealing technique using collagen fleece for surgical therapy of patients with ventral Peyronie's curvature: initial experience. Int J Impot Res. 2018;30:306–311. doi: 10.1038/s41443-018-0044-4. [DOI] [PubMed] [Google Scholar]
- 25.Akbulut F, Akman T, Salabas E, Dincer M, Ortac M, Kadioglu A. Neurovascular bundle dissection for Nesbit procedure in congenital penile curvature patients: medial or lateral? Asian J Androl. 2014;16:442–445. doi: 10.4103/1008-682X.123667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Tuken M, Altinay S, Temiz MZ, Cakir OO, Aykan S, Semercioz A, et al. The effects of four different suture materials on penile tissue of rats. Int J Impot Res. 2016;28:50–53. doi: 10.1038/ijir.2015.32. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data analyzed for this study have been deposited in HARVARD Dataverse and are available at https://doi.org/10.7910/DVN/ILQF81.


