Abstract
Background.
Cannabis use and cannabis use disorder are more prevalent in U.S. states with medical marijuana laws (MMLs), as well as among individuals with elevated psychological distress. We investigated whether adults with moderate and serious psychological distress experienced greater levels of cannabis use and/or disorder in states with MMLs compared to states without MMLs.
Methods.
National Survey of Drug Use and Health data (2013-2017) were used to compare past-month cannabis use, daily cannabis use, and cannabis use disorder prevalence among adults with moderate and serious psychological distress in states with versus without MMLs. We executed pooled multivariable logistic regression analyses to test main effects of distress, MMLs and their interaction, after adjustment.
Results.
Compared to states without MMLs, states with MMLs had higher adjusted prevalence of past-month use (11.1% vs. 6.8%), daily use (4.0% vs. 2.2%), and disorder (1.7% vs. 1.2%). Adults with moderate and serious psychological distress had greater adjusted odds of any use (AORs of 1.72 and 2.22, respectively) and of disorder (AORs of 2.17 and 2.94, respectively), compared to those with no/mild distress. We did not find evidence of an interaction between MMLs and distress category for any outcome.
Conclusions.
Associations between elevated distress and cannabis use patterns are no greater in states with MML. However, cannabis use is more prevalent in MML states. Thus, higher base rates of cannabis use and disorder among adults with elevated distress are proportionally magnified in these states.
Keywords: cannabis, CUD, marijuana legalization laws, psychological distress, mental health, policy analysis
1. INTRODUCTION
Over the past decade in the United States, cannabis use has steadily risen. Today, approximately 1 in 8 U.S. adults have used cannabis in the past year, and 8 million individuals report using cannabis daily or nearly every day (Compton et al., 2016; Hasin et al., 2015). This growth tracks with marijuana legalization laws (Harper et al., 2012): since 1996, over 30 states have passed laws allowing for medical consumption (NCSL, 2019), including 20 states in the past 10 years. Eleven states and Washington DC—representing a fifth of the U.S. population—have also legalized recreational use (Policy Surveillance, 2015).
The extent to which cannabis dependence and cannabis use disorder (CUD) have increased over this same period is a subject of continued inquiry. For instance, Azofeifa and colleagues (2016) examined trends from the National Survey on Drug Use and Health (NSDUH) from 2002-2014, and reported an 11% decrease in prevalence of cannabis dependence among past-year cannabis users aged ≥ 12 years over this time period (Azofeifa, 2016). Meanwhile, Compton and colleagues (2016) examined NSDUH data over the same interval and found stable prevalence of CUD at the population level—inclusive of users and non-users.(Compton et al., 2016) This result has been confirmed elsewhere (Grucza et al., 2016). By contrast, analyses using the National Epidemiologic Survey of Alcohol and Related Conditions have suggested an increase in CUD over time (Hasin et al., 2015). While there are discrepancies across data sources (Grucza et al., 2007; Hasin and Grant, 2016), a preponderance of correlational evidence indicates that CUD rates have been relatively stable for the past decade (Compton et al., 2016, 2019; Grucza et al., 2016), suggesting that they may not have risen in parallel with changes in marijuana laws.
However, more direct evidence from survey data links trends in cannabis use with medical marijuana laws (MMLs) by indicating an uptick in prevalence following MML passage (Cerdá et al., 2012; Hasin et al., 2017; Williams et al., 2017). Evidence likewise indicates that MMLs are predictive of increased CUD when examined with 1- and 2-year time lags,(Martins et al., 2016; Wen et al., 2015) a finding observed across multiple data sets (Hasin, 2017; Hasin et al., 2018), though there has been at least one exceptional finding (Mauro et al., 2019). A similar pattern has been observed in the context of recreational marijuana legalization, though studies are still ongoing. Cerdá and colleagues (2019) examined change in cannabis use and CUD from 2008-2016 as a function of recreational marijuana laws, and found differential increases in both outcomes among those residing in states with recreational laws over this period (Cerdá et al., 2019).
One important line of inquiry is the degree to which marijuana legalization laws — and associated growth in cannabis use—impact vulnerable populations such as those with mental illness and elevated psychological distress. Although the population-level effects of marijuana legalization laws may be diffuse, studies have found that individuals with mental health conditions are more susceptible to adverse effects of cannabis use (National Academies of Sciences, Engineering, and Medicine et al., 2017). Adults with clinically significant psychological distress are more likely to consume cannabis (Kessler et al., 2003), including on a daily basis (Weinberger et al., 2019). One underlying theory is that individuals with heightened psychological distress are more likely to self-medicate in order to decrease anxiety and increase a sense of wellbeing (Lee et al., 2009; Patrick et al., 2016). Elevated cannabis consumption, in turn, has been associated with later development of mental health conditions (Di Forti et al., 2014; Haney and Evins, 2016; Large et al., 2011), as well as cannabis dependence and CUD more directly (National Academies of Sciences, Engineering, and Medicine et al., 2017). Against this backdrop, it is possible that removal of legal barriers to cannabis use may result in a greater relative difference in cannabis use and CUD prevalence among those with moderate and serious distress, compared to those with little or none. This may be particularly likely as MMLs shift norms of cannabis use (Carliner et al., 2017; Roditis et al., 2016), potentially reducing stigma associated with consumption among those with elevated distress.
Based on the relationship between elevated psychological distress and cannabis consumption, there remains an important question as to whether MMLs have resulted in larger negative effects within this population. To explore this question, we examined the relationship between elevated psychological distress and prevalence of cannabis use and CUD in states with MMLs versus those without MMLs. We hypothesized that individuals with moderate and severe psychological distress would observe differentially greater levels of cannabis consumption in states with MMLs versus states without MMLs, and that these differences would translate into higher rates of CUD.
2. MATERIALS & METHODS
2.1. Study Population
We utilized data from the National Survey of Drug Use and Health (NSDUH) public use data files for the years 2013-2017 (SAMHSA and RTI International, 2019) in order to conduct a pooled cross-sectional analysis. Using five years of data increased sample sizes/accuracy of estimates for smaller subgroups and may reduce the influence of confounding historical events on associations. 2013 was the first year for which NSDUH included indicator variables on state-level legality and de-criminalization of cannabis consumption. NSDUH is supported by the Substance Abuse and Mental Health Services Administration (SAMHSA), and provides annualized estimates pertaining to tobacco, alcohol and drug use, as well as mental health status and service utilization in the previous 12 months (SAMHSA and RTI International, 2019). The sample is representative at the state level, using an independent multi-state area probability design; however, public use datafiles do not provide state identifiers. We restrict analyses to those aged 18 and older at the time of survey administration, in part because we wished to focus on adults, but also because the measure of psychological distress—the Kessler Psychological Distress Scale (K6)—is only administered to those aged 18 and older.
The combined sample over the five-year period contained 207,835 observations. We computed survey weights for the NSDUH at the unit-level and individual level. As analyses were based on publicly-available, deidentified data from SAMHSA, this study was determined to be exempt from review by RAND’s Institutional Review Board.
2.2. Measures
2.2.1. Past-month cannabis use
We created a dichotomous indicator of any cannabis in the past month based on a nonzero response to the NSDUH question: “What is your best estimate of the number of days you used marijuana or hashish during the past 30 days?” A second dichotomous indicator categorized respondents as near daily/daily users based on a response of 25 or more days out of the past 30 days (Budney et al., 2003).
2.2.2. Cannabis use disorder
Individuals were identified as having cannabis use disorder (CUD) in the year prior to survey administration based on an indicator provided by NSDUH. NSDUH determines the presence of specific substance use disorders (e.g. cannabis, cocaine, opioid) based on responses to questions about dependence and/or abuse of substances, following DSM-IV diagnostic criteria (APA, 1994). To be identified as having CUD, individuals must meet criteria for dependence by endorsing three or more of six dependence symptoms or for abuse by endorsing one or more of four abuse symptoms. A full overview of the methodology can be found on SAMHSA’s website (Pacek et al., 2015; SAMHSA, 2019; Whitlow et al., 2004).
2.2.3. State medical marijuana legalization (MML) status
While NSDUH public use data files do not include U.S. state indicators, beginning in 2013 NSDUH incorporated an indicator variable (i.e. MEDMJST2) to identify whether individuals were residing in a state with a law allowing cannabis use for medical reasons. Specifically, NSDUH organizes respondents according to the state in which they reside at time of interview into two categories: those states for which a law is already in effect, and those without such a law in place. In cases where a law is going into effect during the survey year, a respondent’s classification is based on the survey date relative to date of law passage. NSDUH public use data files do not provide an indicator of state recreational marijuana use laws, nor do they include questions in which respondents are asked to distinguish their consumption patterns according to recreational versus medical use.
2.2.4. Psychological distress
Individuals’ psychological distress status was assessed using the well-validated Kessler Psychological Distress Scale (K6) screening tool, a 6-item instrument that evaluates level of psychological distress based on reported frequency of nervousness, hopelessness, restlessness, depressed or sad mood, feeling that everything is an effort, and feeling down, no good, or worthless during the month in the prior year during which these symptoms were most prevalent (Kessler et al., 2010, 2003). Response options are on a five-point Likert scale from 0 (none of the time) to 4 (all the time), and are summated across items (possible range: 0-24). We applied a commonly used set of cut-points to categorize respondents into three groups: a score of 0-7 indicates no/mild psychological distress, 8-12 indicates moderate psychological distress, and 13 or higher indicates serious psychological distress (Kessler et al., 2003, 2006, 2008; Wang et al., 2007).
2.2.5. Covariates
We included five demographic characteristics as covariates in analyses: sex (female, male), age (18-25, 26-34, 35-49, 50-64, 65+) race/ethnicity and language (Hispanic interviewed in English, Hispanic interviewed in Spanish, non-Hispanic White, non-Hispanic Black, non-Hispanic Asian, non-Hispanic Other), educational attainment (less than high school graduate, high school graduate, partial college, 4-year college graduate or above) and total family income (<$20,000, $20,000-$49,999, $50,000-$74,999, $75,000+).
2.3. Statistical analyses
Data were weighted according to NSDUH survey weights, and analyzed using survey procedures in SAS/STAT v.9 for Linux (SAS, 2016). First, we examined descriptive characteristics of the sample, cross-tabulating prevalence of past month cannabis use, as well as daily use and cannabis use disorder among users, according to state MML status (legal, not legal) and psychological distress level (no/mild distress, moderate distress, serious distress). In addition to reporting estimates at the population level, we also reported daily use and CUD as conditional on any use: specifically, daily cannabis use in the past month conditional on any use in the past month, and CUD in the past year conditional on any use in the past year. We also examined these outcomes according to demographic characteristics to inspect balance across MML and non-MML states.
Next, we conducted multivariable logistic regression analyses to examine the cross-sectional associations among state MML status, psychological distress status, and outcomes of interest, adjusting for covariates. Specifically, we tested for the hypothesized interaction between MML status (legal, not legal) and psychological distress level (no/mild distress, moderate distress, serious distress) on likelihood of any cannabis use in the past month, likelihood of daily use, and likelihood of cannabis use disorder (CUD). The latter two outcomes were examined with (i) the sample restricted just to those individuals who reported any marijuana use, given the strong positive skew of daily use and CUD, as well as (ii) unrestricted, in order to derive population-level estimates. All analyses used a pooled sample across survey years (2013-2017).
3. RESULTS
3.1. Population characteristics – according to state MML status
Consistent with other U.S. population estimates, 8.7% of adults reported any cannabis use in the past month, with roughly a third (34.2%) of past-month users (3.0% overall) reporting daily use. Prevalence of cannabis use disorder among users was 10.2% among those reporting any use in the past year, and 1.4% at the population level. Overall prevalence of no/mild psychological distress was 76.6%, compared to 12.6% for moderate psychological distress and 10.8% for severe psychological distress.
Table 1 provides descriptive comparisons of individuals residing in states with versus without MMLs. As established in prior studies, individuals in states with MMLs were more likely to report cannabis use in the past month: 10.5% of adults, compared to 7.1% in non-legalized states (p<0.001). We also found higher prevalence of daily cannabis use in MML states (3.7% vs. 2.3%; p<0.001) as well as prevalence of CUD (1.6% vs. 1.4%; p<0.001). Conditional on any cannabis use in the past month, we observed a higher prevalence of daily cannabis use among users in MML states compared with non-MML states (35.1% vs. 33.0%, p=0.03), but did not find evidence of a difference in the prevalence of CUD between users in MML states versus non-MML states (p=0.30). Individuals in states with MMLs did not differ significantly from those in states without MMLs in terms of average levels of psychological distress: in both settings, just over three-quarters of individuals reported no/mild psychological distress, with the remainder fairly evenly distributed across moderate and severe distress categories. Those in MML states were, however, higher income, more educated, and had a different racial/ethnic profile (p<0.05).
Table 1.
Demographic Comparison of Those Living in MML States versus Non-MML States
| Characteristic | States with MML | States without MML | Difference (MML – non-MML) |
|||
|---|---|---|---|---|---|---|
| Percent | Sample N | Percent | Sample N | Percent/ Days |
Chi-Square P-value |
|
| Sex | ||||||
| Female | 51.6 | 29,499 | 51.9 | 33,283 | −0.3 | 0.28 |
| Male | 48.4 | 27,653 | 48.1 | 30,789 | 0.3 | |
| Age | ||||||
| 18-25 Years | 14.2 | 8,099 | 14.4 | 9,251 | −0.2 | |
| 26-34 Years | 16 | 9,159 | 15.7 | 10,034 | 0.3 | |
| 35-49 Years | 24.9 | 14,247 | 25.1 | 16,081 | −0.2 | 0.59 |
| 50-64 Years | 25.5 | 14,590 | 25.6 | 16,429 | −0.1 | |
| 65+ Years | 19.3 | 11,056 | 19.2 | 12,277 | 0.1 | |
| Race/Ethnicity | ||||||
| Hispanic, Spanish Speaking | 5.9 | 3,376 | 3.8 | 2,421 | 2.1 | |
| Hispanic, English Speaking | 13.1 | 7,510 | 8.7 | 5,566 | 4.4 | |
| Non-Hispanic Black | 8.9 | 5,079 | 14.4 | 9,209 | −5.5 | <0.001 |
| Non-Hispanic White | 61.1 | 34,892 | 68.1 | 43,636 | −7.0 | |
| Non-Hispanic Asian | 8.0 | 4,559 | 3.1 | 1,963 | 4.9 | |
| Non-Hispanic Other | 3.0 | 1,736 | 2.0 | 1,277 | 1.0 | |
| Income | ||||||
| Less than $20,000 | 15.9 | 9,105 | 18.9 | 12,112 | −3.0 | |
| $20,000-$49,999 | 28.3 | 16,185 | 32.2 | 20,642 | −3.9 | <0.001 |
| $50,000-$74,9999 | 16.1 | 9,177 | 16.8 | 10,775 | −0.7 | |
| $75,000+ | 39.7 | 22,686 | 32.1 | 20,542 | 7.6 | |
| Educational Attainment | ||||||
| Less than High School | 12.4 | 7,061 | 13.9 | 8,910 | −1.5 | |
| High School Graduate | 24 | 13,742 | 29 | 18,603 | −5.0 | <0.001 |
| Some College | 29.5 | 16,859 | 29.3 | 18,767 | 0.2 | |
| College Graduate | 34.1 | 19,490 | 27.8 | 17,791 | 6.3 | |
| Psychological Distress Status | ||||||
| No/Mild Psych. Distress | 76.7 | 43,850 | 76.5 | 49,030 | 0.2 | |
| Moderate Psych. Distress | 12.6 | 7,183 | 12.6 | 8,098 | 0.0 | 0.75 |
| Severe Psych. Distress | 10.7 | 6,120 | 10.8 | 6,944 | −0.1 | |
| Cannabis-Related Measures | ||||||
| Past-year Cannabis Use | 16.1 | 9,184 | 11.8 | 7,550 | 4.3 | <0.001 |
| Past-month Cannabis Use | 10.5 | 6,016 | 7.1 | 4,546 | 3.4 | <0.001 |
| Daily Cannabis Use* | 35.1 | 2,115 | 33.0 | 1,499 | 2.1 | 0.03 |
| Cannabis Use Disorder** | 10.0 | 922 | 10.5 | 791 | −0.5 | 0.30 |
Footnotes. CUD = Cannabis Use Disorder.
Daily use, conditional on use in the past month. Cannabis use disorder, conditional on any use in the past year.
3.2. Past-month cannabis use—according to psychological distress status and state MML status
In multivariable regression models adjusted for demographic characteristics (see Table 2), we found that elevated psychological distress status was associated with greater odds of any cannabis use: an odds ratio of 1.72 among moderately distressed individuals and 2.22 among severely distressed individuals, compared to individuals with no/mild distress (p<0.001). Additionally, we found that residing in a state with legalized medical marijuana status was associated with 1.85 greater odds of any cannabis consumption, compared to those residing in a state without legalized status (p<0.001). However, interactions between state legalization status and psychological distress were non-significant, both for moderate distress by state legalization status and serious distress by state legalization status.
Table 2.
Odds of Past-Month Cannabis Use, by MML Status and Distress Level
| Odds Ratio | 95% CI | P-Value | |
|---|---|---|---|
| Medical Marijuana Legalization | |||
| Medical Marijuana Law (MML) | 1.85 | 1.75, 1.95 | < 0.001 |
| No MML Law | --- | --- | --- |
| Psychological Distress Status | |||
| Serious Distress (K6>12) | 2.22 | 2.07, 2.38 | < 0.001 |
| Moderate Distress (K6: 8-12) | 1.72 | 1.57, 1.88 | < 0.001 |
| No/Mild Distress (K6<8) | --- | --- | --- |
| Interaction: MML by Distress Status | |||
| MML*Moderate Distress | 0.95 | 0.85, 1.07 | 0.41 |
| MML*Serious Distress | 0.97 | 0.87, 1.09 | 0.63 |
Footnotes: Logistic regression model adjusted for sociodemographic characteristics including sex, age, race/ethnicity, income and educational attainment.
3.3. Daily cannabis use and CUD — according to psychological distress status and state MML status
In terms of daily cannabis use, we found that—among individuals who reported any cannabis use—those with moderate and serious psychological distress did not have greater likelihood of daily consumption, compared to those with no/mild distress (see Table 3). However, individuals residing in MML states were more likely to consume cannabis on a daily basis, compared to those residing in a state without legalized status (p=0.01). As with past month use, hypothesized interactions between state legalization status and psychological distress status were non-significant (p>0.05).
Table 3.
Adjusted Odds of Daily Cannabis Use and CUD, by MML Status and Distress Level
| Daily Cannabis Use | Cannabis Use Disorder | |||||
|---|---|---|---|---|---|---|
| Medical Marijuana Legalization | Odds Ratio | 95% CI | P-Value | Odds Ratio | 95% CI | P-Value |
| Medical Marijuana Law (MML) | 1.18 | 1.04, 1.34 | 0.01 | 1.05 | 0.87, 1.28 | 0.58 |
| No MML Law | --- | --- | --- | --- | --- | --- |
| Psychological Distress Status | ||||||
| Serious Distress (K6>12) | 1.11 | 0.95, 1.29 | 0.18 | 2.94 | 2.49, 3.47 | < 0.001 |
| Moderate Distress (K6: 8-12) | 1.07 | 0.90-1.27 | 0.44 | 2.17 | 1.85, 2.54 | < 0.001 |
| No/Mild Distress (K6<8) | --- | --- | --- | --- | --- | --- |
| Interaction: MML*Distress Status | ||||||
| MML*Moderate Distress | 0.93 | 0.74, 1.18 | 0.54 | 0.88 | 0.69, 1.12 | 0.29 |
| MML*Serious Distress | 1.10 | 0.90, 1.34 | 0.35 | 1.10 | 0.84, 1.44 | 0.47 |
Footnotes: Logistic regression models adjusted for sociodemographic characteristics including sex, age, race/ethnicity, income and educational attainment.
Lastly, we found that—among individuals who used cannabis in the past year—those with moderate and serious psychological distress had increased odds of cannabis use disorder, compared to individuals with no/mild distress (p<0.001) (see Table 3). However, we did not find evidence of greater odds of having cannabis use disorder in states with legalized medical marijuana status compared to non-legalized status (p>0.05). Likewise, interactions between state legalization status and psychological distress status were non-significant (p>0.05).
3.4. Adjusted population-level estimates of cannabis-related outcomes
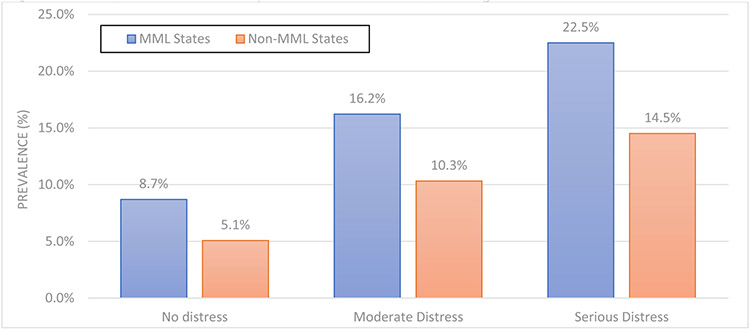
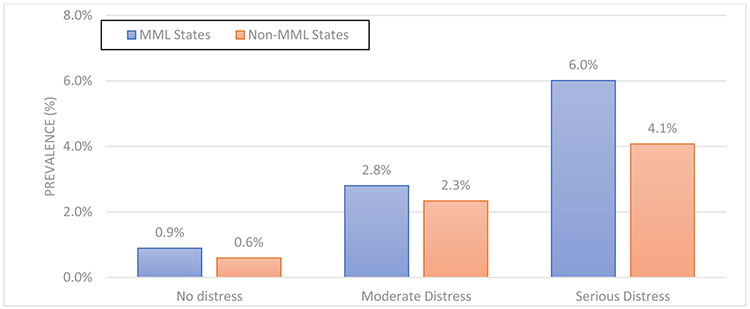
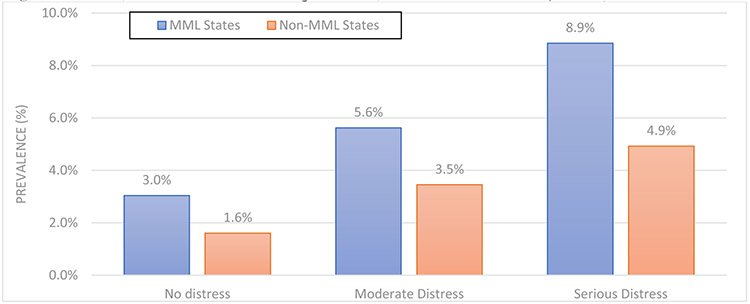
To produce adjusted population-level estimates of past-month cannabis use prevalence, daily use prevalence and CUD prevalence by MML status and psychological distress level, we generated predictive marginal values from regression models. These estimates, reflected in Figures 1A-1C, represent the expected prevalence of cannabis-related outcomes after adjusting for state differences in sociodemographic characteristics.
Figure 1A.
Any Cannabis Use, by MML Status and Psychological Distress Status
Figure 1C.
CUD Among Users, by MML Status and Psychological Distress Status
Across all three cannabis-related measures, we found that population-level prevalence differed according to MML status (p<0.001)—with a larger percentage of individuals residing in MML states expected to use cannabis in the past month, use cannabis daily, and have CUD in the past year, compared to the percentage in non-MML states. Likewise, across all three cannabis-related measures, we found that population-level prevalence differed according to psychological distress status (p<0.001)—with a larger percentage of individuals with moderate/serious psychological distress expected to use cannabis in the past month, use cannabis daily, and have CUD in the past year, compared to the percentage of individuals with no/mild psychological distress.
Proportional differences between MML states and non-MML states were similar across psychological distress categories, though in absolute terms these differences were largest among those in the serious psychological distress category. For example, the expected prevalence of CUD among those with no/mild distress was 3.0% in MML states, versus 1.6% in non-MML states—an absolute difference of 1.4%. By contrast, the expected prevalence of CUD among those with serious distress was 8.9% in MML states, versus 4.9% in non-MML states—an absolute difference of 4.0%.
4. DISCUSSION
To our knowledge, this is the first study to examine whether state medical marijuana laws are associated with differential use of cannabis and prevalence of CUD among individuals with elevated psychological distress. We do not find evidence that MML status was associated with disproportionately higher cannabis use or CUD in this population. Rather, we observe a consistent pattern of main effects, with higher levels of cannabis use and CUD in MML states compared to non-MML states, and higher levels of cannabis use and CUD among those with elevated psychological distress compared to those with no/mild distress. However, at the population level, this proportional relationship implies that the absolute magnitude of differences between MML states and non-MML states—including for prevalence of CUD—is largest among those with serious psychological distress.
Similar to prior studies, we find that elevated psychological distress is associated with greater likelihood of cannabis use and greater likelihood of CUD. For instance, Weinberger and colleagues (2019) reviewed NSDUH from 2008-2016 and concluded that persons with serious psychological distress reported higher rates of daily cannabis use.(Weinberger et al., 2019) Additional studies have found that perceived stress and mental health status are positively associated with prevalence of CUD (Moitra et al., 2015) and heavy cannabis use (Degenhardt et al., 2003). Our findings extend this evidence base, indicating elevated likelihood of any cannabis use, daily use, and CUD among those with both moderate and serious psychological distress, compared to those with no/mild distress. The magnitudes of these effects were large: for example, individuals with moderate psychological distress were more than twice as likely to experience CUD in the past year compared to those with no/mild distress, while those with serious psychological distress were almost three times as likely.
The results also extend past evidence indicating that state legalization of medical marijuana is associated with higher frequency of cannabis use-related outcomes (Martins et al., 2016; Wen et al., 2015). For example, we observed elevated cannabis use in MML states—both in terms of any use and daily use. We also confirm past findings that—at the population-level—MML states have elevated levels of CUD, compared to non-MML states (Martins et al., 2016; Wen et al., 2015). Our results further suggest that individuals with CUD may reside in MML states merely as a function of a greater number of individuals reporting any use, rather than as a result of differential behavior patterns in MML states compared to non-MML states. Specifically, we observed that the odds of CUD, conditional on any use, were similar between MML and non-MML states; however, a higher prevalence of cannabis use in MML states translated to a higher prevalence of CUD.
We did not find evidence indicating a differential effect of MML status on cannabis use-related outcomes among those with elevated distress, compared to no/mild distress. There are a couple potential explanations. One is that MMLs may have made cannabis use for any purpose more socially acceptable, resulting in broadly distributed effects at the population level (Azofeifa, 2016; Carliner et al., 2017; Schmidt et al., 2019; Wen et al., 2019). Past studies have shown that, while MMLs are intended for medical purposes, they may have a more expansive effect that includes non-medical use (Pacula and Smart, 2017; Williams et al., 2017). Relatedly, to the extent that MMLs have uniquely impacted populations seeking cannabis for medical use, these effects may also be broadly distributed across the psychological distress levels we evaluated: those with psychological distress comprise only one class of individuals who may be seeking medical marijuana. Other indications include, for example, cancer, glaucoma, epilepsy, chronic pain and multiple sclerosis (Boehnke et al., 2019a). In fact, only a handful of states list mental health conditions—apart from post-traumatic stress disorder—as qualifying conditions.
The impact of overall higher use among distressed individuals residing in MML states is unclear. It is possible, for example, that MMLs could lead to adverse, cannabis-related outcomes such as dependence among some individuals with psychological distress, while also serving a medicinal function that improves outcomes for others. In fact, past studies have independently observed both patterns of findings in different settings (Hayatbakhsh et al., 2007; Kedzior and Laeber, 2014; Moitra et al., 2015; Walsh et al., 2017). It is likewise possible that this elevated cannabis use reflects substitutionary behavior for prescription medicines such as analgesics and anxiolytics, as documented elsewhere in the literature (Boehnke et al., 2019b, 2016; Bradford and Bradford, 2017, 2016). In the context of this study, evidence indicates that MMLs have not resulted in disproportionately greater rates of cannabis use and CUD among those with elevated distress. Future research at the individual level could differentiate these trends by identifying predictors of class membership in cannabis use trajectories that lead to CUD versus those that generate therapeutic benefits.
A distinction should be made in our analysis between proportional and absolute effects. We observed non-significant differences in proportional terms when comparing those with elevated and no/mild psychological distress in MML and non-MML states. However, given the higher base rate of cannabis use and CUD among individuals with moderate and severe distress, this implies that the magnitude of the difference in absolute terms is considerably larger. For example, adjusted prevalence of CUD among individuals with no/mild distress was 0.9% in MML states versus 0.6% in non-MML states—a proportional difference of 50%, but an absolute difference of 0.3%. By contrast, adjusted prevalence of CUD among individuals with serious distress was 6.1% in MML states versus 4.0% in non-MML states—a proportional difference of (again) roughly 50%, but an absolute difference of 2.1%. In other words, the absolute difference in prevalence of CUD—when contrasting MML versus non-MML states—is seven times larger among those with serious psychological distress compared to those with no/mild distress (2.1% versus 0.3%). In practical terms, this means that, to the extent that individuals with psychological distress are at greater risk of adverse cannabis-related outcomes such as CUD, this risk is proportionally magnified in states with MMLs.
Several study limitations should be noted. First, our analytic sample comprised U.S. adults from repeated cross-sectional panels of the NSDUH. Future research might explore other populations such as adolescents, or more specific populations such as those with particular mental health conditions. We focused on those with elevated psychological distress to capture individuals with and without a diagnosis experiencing symptoms that might motivate selfmedication. Second, the absence of state level indicator variables in the public use data files precluded us from tracking trends over time within states, requiring us to conduct a pooled analysis for the 2013-2017 period. Restricted NSDUH datasets would have allowed us to examine longitudinal trends in medical and recreational marijuana laws at the state level, as past research has indicated differences in use patterns based on recreational versus medical use (Lin et al., 2016; Sznitman, 2017; Wall et al., 2019). Likewise, state-level data would have allowed us to distinguish between states that were early implementers of MMLs and later implementers of MMLs (Hasin et al., 2017). The present analysis presents descriptive differences in cannabis use and CUD in states with MMLs versus without MMLs, and should not be taken as indicative of any causal relationships. Lastly, all data from NSDUH are selfreported, raising the possibility of introducing biases in estimates, including effects from social desirability bias (Johnson, 2014). Indeed, social desirability bias may be amplified in states without MMLs, where cannabis use is a criminal offense and respondents may therefore be less willing to endorse items asking about their consumption.
4.1. Conclusions
Consistent with prior research, we find that adults with elevated psychological distress are more likely to use cannabis, use it daily, and have greater likelihood of cannabis use disorder. Similarly, adults residing in states with MMLs have high rates of cannabis use and daily use. It does not appear that individuals with elevated psychological distress are uniquely impacted by MMLs. However, in absolute terms, outcomes such as daily cannabis use and CUD are magnified among those with elevated psychological distress who reside in MML states. Further research is required to understand the relationship between cannabis use, state laws and therapeutic versus adverse outcomes in this vulnerable population, as well as to identify subgroups at different levels of cannabis-related risk such as those with concomitant use of other substances and medications.
Figure 1B.
Daily Cannabis Use Among Users, by MML Status and Psychological Distress Status
Highlights.
Adults with elevated psychological distress are more likely to use cannabis
Cannabis use and cannabis use disorder are more common in legalized states
Cannabis use and risk of cannabis use disorder are proportionally magnified among those with elevated psychological distress residing in legalized states
Acknowledgments
Role of Funding Source
Funding for this study was provided by the National Institute of Mental Health (R01MH104381). NIMH played no additional roles in study design, collection, analysis or interpretation of data, writing of the report, or design to submit this paper for publication.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflicts of Interest
The authors declare no conflicts of interest.
REFERENCES
- APA, 1994. Diagnostic and Statistical Manual of Mental Disorders (4th edition). American Psychiatric Association, Washington DC. [Google Scholar]
- Azofeifa A, 2016. National Estimates of Marijuana Use and Related Indicators — National Survey on Drug Use and Health, United States, 2002-2014. MMWR Surveill. Summ 65. [DOI] [PubMed] [Google Scholar]
- Boehnke KF, Gangopadhyay S, Clauw DJ, Haffajee RL, 2019a. Qualifying Conditions Of Medical Cannabis License Holders In The United States. Health Aff. (Millwood) 38, 295–302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boehnke KF, Litinas E, Clauw DJ, 2016. Medical Cannabis Use Is Associated With Decreased Opiate Medication Use in a Retrospective Cross-Sectional Survey of Patients With Chronic Pain. J. Pain Off. J. Am. Pain Soc 17, 739–744. [DOI] [PubMed] [Google Scholar]
- Boehnke KF, Scott JR, Litinas E, Sisley S, Williams DA, Clauw DJ, 2019b. Pills to Pot: Observational Analyses of Cannabis Substitution Among Medical Cannabis Users With Chronic Pain. J. Pain Off. J. Am. Pain Soc 20, 830–841. [DOI] [PubMed] [Google Scholar]
- Bradford AC, Bradford WD, 2017. Medical Marijuana Laws May Be Associated With A Decline In The Number Of Prescriptions For Medicaid Enrollees. Health Affairs. 36, 945–951. [DOI] [PubMed] [Google Scholar]
- Bradford AC, Bradford WD, 2016. Medical Marijuana Laws Reduce Prescription Medication Use In Medicare Part D. Health Affairs. 35, 1230–1236. [DOI] [PubMed] [Google Scholar]
- Budney AJ, Moore BA, Vandrey RG, Hughes JR, 2003. The time course and significance of cannabis withdrawal. J. Abnorm. Psychol 112, 393–402. [DOI] [PubMed] [Google Scholar]
- Carliner H, Brown QL, Sarvet AL, Hasin DS, 2017. Cannabis use, attitudes, and legal status in the U.S.: A review. Prev. Med., Special issue: Behavior change, health, and health disparities 2017 104, 13–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cerdá M, Mauro C, Hamilton A, Levy NS, Santaella-Tenorio J, Hasin D, Wall MM, Keyes KM, Martins SS, 2019. Association Between Recreational Marijuana Legalization in the United States and Changes in Marijuana Use and Cannabis Use Disorder From 2008 to 2016. JAMA Psychiatry 77, 165–171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cerdá M, Wall M, Keyes KM, Galea S, Hasin D, 2012. Medical marijuana laws in 50 states: Investigating the relationship between state legalization of medical marijuana and marijuana use, abuse and dependence. Drug Alcohol Depend. 120, 22–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Compton WM, Han B, Jones CM, Blanco C, 2019. Cannabis use disorders among adults in the United States during a time of increasing use of cannabis. Drug Alcohol Depend. 204,107468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Compton WM, Han B, Jones CM, Blanco C, Hughes A, 2016. Marijuana use and use disorders in adults in the USA, 2002-14: analysis of annual cross-sectional surveys. Lancet Psychiatry 3, 954–964. [DOI] [PubMed] [Google Scholar]
- Degenhardt L, Hall W, Lynskey M, 2003. Exploring the association between cannabis use and depression. Addiction 98, 1493–1504. [DOI] [PubMed] [Google Scholar]
- Di Forti M, Sallis H, Allegri F, Trotta A, Ferraro L, Stilo SA, Marconi A, La Cascia C, Reis Marques T, Pariante C, Dazzan P, Mondelli V, Paparelli A, Kolliakou A, Prata D, Gaughran F, David AS, Morgan C, Stahl D, Khondoker M, MacCabe JH, Murray RM, 2014. Daily use, especially of high-potency cannabis, drives the earlier onset of psychosis in cannabis users. Schizophr. Bull 40, 1509–1517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grucza RA, Abbacchi AM, Przybeck TR, Gfroerer JC, 2007. Discrepancies in Estimates of Prevalence and Correlates of Substance Use and Disorders Between Two National Surveys. Addict. 102, 623–629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grucza RA, Agrawal A, Krauss MJ, Cavazos-Rehg PA, Bierut LJ, 2016. Recent Trends in the Prevalence of Marijuana Use and Associated Disorders in the United States. JAMA Psychiatry 73, 300–301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haney M, Evins AE, 2016. Does Cannabis Cause, Exacerbate or Ameliorate Psychiatric Disorders? An Oversimplified Debate Discussed. Neuropsychopharmacol. Off. Publ. Am. Coll. Neuropsychopharmacol 41, 393–401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harper S, Strumpf EC, Kaufman JS, 2012. Do medical marijuana laws increase marijuana use? Replication study and extension. Ann. Epidemiol 22, 207–212. [DOI] [PubMed] [Google Scholar]
- Hasin DS, 2018. US Epidemiology of Cannabis Use and Associated Problems. Neuropsychopharmacology 43, 195–212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hasin DS, Grant B, 2016. NESARC Findings on Increased Prevalence of Marijuana Use Disorders—Consistent With Other Sources of Information. JAMA Psychiatry 73, 532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hasin DS, Saha TD, Kerridge BT, Goldstein RB, Chou SP, Zhang H, Jung J, Pickering RP, Ruan WJ, Smith SM, Huang B, Grant BF, 2015. Prevalence of Marijuana Use Disorders in the United States Between 2001-2002 and 2012-2013. JAMA Psychiatry 72, 1235–1242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hasin DS, Sarvet AL, Cerdá M, Keyes KM, Stohl M, Galea S, Wall MM, 2017. US Adult Illicit Cannabis Use, Cannabis Use Disorder, and Medical Marijuana Laws: 1991-1992 to 2012-2013. JAMA Psychiatry 74, 579–588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayatbakhsh MR, Najman JM, Jamrozik K, Mamun AA, Alati R, Bor W, 2007. Cannabis and Anxiety and Depression in Young Adults: A Large Prospective Study. J. Am. Acad. Child Adolesc. Psychiatry 46, 408–417. [DOI] [PubMed] [Google Scholar]
- Johnson TP, 2014. Sources of Error in Substance Use Prevalence Surveys. Int. Sch. Res. Not 2014, 923290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kedzior KK, Laeber LT, 2014. A positive association between anxiety disorders and cannabis use or cannabis use disorders in the general population- a meta-analysis of 31 studies. BMC Psychiatry 14, 136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Barker PR, Colpe LJ, Epstein JF, Gfroerer JC, Hiripi E, Howes MJ, Normand S-LT, Manderscheid RW, Walters EE, Zaslavsky AM, 2003. Screening for serious mental illness in the general population. Arch. Gen. Psychiatry 60, 184–189. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Galea S, Jones RT, Parker HA, 2006. Mental illness and suicidality after Hurricane Katrina. Bull. World Health Organ 84, 930–939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Green JG, Gruber MJ, Sampson NA, Bromet E, Cuitan M, Furukawa TA, Gureje O, Hinkov H, Hu C-Y, Lara C, Lee S, Mneimneh Z, Myer L, Oakley- Browne M, Posada-Villa J, Sagar R, Viana MC, Zaslavsky AM, 2010. Screening for serious mental illness in the general population with the K6 screening scale: results from the WHO World Mental Health (WMH) survey initiative. Int. J. Methods Psychiatr. Res 19 Suppl 1, 4–22. h [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Keane TM, Ursano RJ, Mokdad A, Zaslavsky AM, 2008. Sample and design considerations in post-disaster mental health needs assessment tracking surveys. Int. J. Methods Psychiatr. Res 17 Suppl 2, S6–S20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Large M, Sharma S, Compton MT, Slade T, Nielssen O, 2011. Cannabis use and earlier onset of psychosis: a systematic meta-analysis. Arch. Gen. Psychiatry 68, 555–561. [DOI] [PubMed] [Google Scholar]
- Lee CM, Neighbors C, Hendershot CS, Grossbard JR, 2009. Development and Preliminary Validation of a Comprehensive Marijuana Motives Questionnaire. J. Stud. Alcohol Drugs 70, 279–287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin LA, Ilgen MA, Jannausch M, Bohnert KM, 2016. Comparing adults who use cannabis medically with those who use recreationally: Results from a national sample. Addict. Behav 61, 99–103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martins SS, Mauro CM, Santaella-Tenorio J, Kim JH, Cerda M, Keyes KM, Hasin DS, Galea S, Wall M, 2016. State-level medical marijuana laws, marijuana use and perceived availability of marijuana among the general U.S. population. Drug Alcohol Depend. 169, 26–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mauro CM, Newswanger P, Santaella-Tenorio J, Mauro PM, Carliner H, Martins SS, 2019. Impact of Medical Marijuana Laws on State-Level Marijuana Use by Age and Gender, 2004-2013. Prev. Sci. Off. J. Soc. Prev. Res 20, 205–214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moitra E, Christopher PP, Anderson BJ, Stein MD, 2015. Coping-motivated marijuana use correlates with DSM-5 cannabis use disorder and psychological distress among emerging adults. Psychol. Addict. Behav. J. Soc. Psychol. Addict. Behav 29, 627–632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Academies of Sciences, Engineering, and Medicine, 2017. The Health Effects of Cannabis and Cannabinoids: The Current State of Evidence and Recommendations for Research, The National Academies Collection: Reports funded by National Institutes of Health. National Academies Press (US), Washington (DC) Accessed on Jan 8, 2020. [PubMed] [Google Scholar]
- NCSL, 2019. State Medical Marijuana Laws. National Conference of State Legislatures, Denver, CO: Accessed on Jan 8, 2020. [Google Scholar]
- Pacek LR, Mauro PM, Martins SS, 2015. Perceived risk of regular cannabis use in the United States from 2002 to 2012: differences by sex, age, and race/ethnicity. Drug Alcohol Depend. 149, 232–244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pacula RL, Smart R, 2017. Medical Marijuana and Marijuana Legalization. Annu. Rev. Clin. Psychol 13, 397–419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patrick ME, Bray BC, Berglund PA, 2016. Reasons for Marijuana Use Among Young Adults and Long-Term Associations With Marijuana Use and Problems. J. Stud. Alcohol Drugs 77, 881–888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Policy Surveillance, 2015. Recreational Marijuana Laws LawAtlas, Philadelphia, PA: Accessed on Jan 8, 2020. [Google Scholar]
- Roditis ML, Delucchi K, Chang A, Halpern-Felsher B, 2016. Perceptions of social norms and exposure to pro-marijuana messages are associated with adolescent marijuana use. Prev. Med. 93, 171–176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- SAMHSA, 2019. 2018 Methodological Summary and Definitions. Accessed on Jan 8, 2020. [Google Scholar]
- SAMHSA, RTI International, 2019. National Survey on Drug Use and Health. SAS Institute Inc, Cary, NC: Accessed on Jan 8, 2020. [Google Scholar]
- Schmidt LA, Jacobs LM, Vlahov D, Spetz J, 2019. Impacts of Medical Marijuana Laws on Young Americans Across the Developmental Spectrum. Matern. Child Health J. 23, 486–495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sznitman SR, 2017. Do recreational cannabis users, unlicensed and licensed medical cannabis users form distinct groups? Int. J. Drug Policy 42, 15–21. [DOI] [PubMed] [Google Scholar]
- Wall MM, Liu J, Hasin DS, Blanco C, Olfson M, 2019. Use of marijuana exclusively for medical purposes. Drug Alcohol Depend. 195, 13–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walsh Z, Gonzalez R, Crosby K, S. Thiessen M, Carroll C, Bonn-Miller MO, 2017. Medical cannabis and mental health: A guided systematic review. Clin. Psychol. Rev 51, 15–29. [DOI] [PubMed] [Google Scholar]
- Wang PS, Gruber MJ, Powers RE, Schoenbaum M, Speier AH, Wells KB, Kessler RC, 2007. Mental Health Service Use Among Hurricane Katrina Survivors in the Eight Months After the Disaster. Psychiatr. Serv. Wash. DC 58, 1403–1411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weinberger AH, Pacek LR, Sheffer CE, Budney AJ, Lee J, Goodwin RD, 2019. Serious psychological distress and daily cannabis use, 2008 to 2016: Potential implications for mental health? Drug Alcohol Depend. 197, 134–140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wen H, Hockenberry JM, Cummings JR, 2015. The effect of medical marijuana laws on adolescent and adult use of marijuana, alcohol, and other substances. J. Health Econ 42, 64–80. [DOI] [PubMed] [Google Scholar]
- Wen H, Hockenberry JM, Druss BG, 2019. The Effect of Medical Marijuana Laws on Marijuana-Related Attitude and Perception Among US Adolescents and Young Adults. Prev. Sci. Off. J. Soc. Prev. Res 20, 215–223. [DOI] [PubMed] [Google Scholar]
- Whitlow CT, Liguori A, Livengood LB, Hart SL, Mussat-Whitlow BJ, Lamborn CM, Laurienti PJ, Porrino LJ, 2004. Long-term heavy marijuana users make costly decisions on a gambling task. Drug Alcohol Depend. 76, 107–111. [DOI] [PubMed] [Google Scholar]
- Williams AR, Santaella-Tenorio J, Mauro CM, Levin FR, Martins SS, 2017. Loose regulation of medical marijuana programs associated with higher rates of adult marijuana use but not cannabis use disorder. Addict. 112, 1985–1991. [DOI] [PMC free article] [PubMed] [Google Scholar]