Abstract
Background
It is unclear whether a connection exists between femoral head size, offset, neck length, and cup abduction angles, and rate of revision in metal-on-metal (MoM) total hip arthroplasty (THA) implant systems.
Methods
A retrospective review of MoM THA completed by a single surgeon with a single implant between 2003 and 2008 was conducted. Patient demographics, implant data, radiographs, and revision details were collected at follow-up. Incidence rates for revision and osteolysis were calculated in regard to the femoral head size, stem offset, neck length, and cup abduction angles.
Results
Six hundred and ninety two THAs were identified, with 79% of patients returning for a median follow-up of 10.3 years (interquartile range = 6.0-12.3). The median time to revision was 7.5 years (interquartile range = 5.3-9.9) among 27 total revision surgeries. The overall incidence rate of revision was 5.4 revisions per 1000 person-years, 3.0 revisions per 1000 person-years for adverse local tissue reaction. Hips with a cup abduction angle of ≤40° had revisions at nearly twice the rate of those with an angle of 41°-50° (incidence rate ratio = 1.98, 95% confidence interval: 0.92, 4.29). Hips with a 9 mm neck length had an increased rate of revision (incidence rate ratio = 5.94, 95% confidence interval: 1.33, 26.55) relative to those with a neck length of 0 mm. Rates of osteolysis were similar between implants of different head sizes, neck lengths and cup abduction angles.
Conclusions
MoM implant systems with longer necks and smaller cup abduction angles may lead to increased need for revision. Results from this study suggest a need for closer long-term follow-up of MoM THA systems.
Keywords: Metal-on-metal, Total hip arthroplasty, Revision, Osteolysis
Introduction
Metal-on-metal (MoM) total hip arthroplasty (THA) had been widely used since the 1960s for treatment of hip osteoarthritis [1,2]. Durability was the initial advantage of MoM articulations, as they originally surpassed their metal-on-polyethylene competitors. Metal-on-polyethylene THA had trouble accommodating larger femoral head sizes and was known to have a finite life because of polyethylene wear [3,4]. MoM was appealing for younger, more physically active patients because of less wear and for all patients because of increased stability with greater head-to-neck ratios [5]. However, over time, MoM hip systems have experienced the phenomenon now known as metallosis because of the components releasing metal debris [6]. This phenomenon, eventually termed ‘adverse local tissue reaction’ (ALTR), is the destruction of the surrounding bone and soft tissue. In the early 2000s, there became an increased awareness of ALTR, which has become a prominent reason for THA revision [[7], [8], [9], [10]]. The implantation of MoM hips was drastically reduced once this evidence became widespread. However, a large number of patients still retain these implants and continue to follow up. Management of this population can be challenging for surgeons. There are no clear guidelines to help surgeons decide when to revise these patients and no clear data on the natural course of these implants when left in place.
Radiographic and laboratory studies have been used to track the status of MoM implants that have been left in place. Laboratory analyses of chromium and cobalt levels in the serum have been correlated with increased MoM wear [2,8,[11], [12], [13]]. Inflammatory markers may be useful in monitoring the severity of the metal debris and ALTR [14]. Radiographs and magnetic resonance imaging (MRI) can help determine the presence and extent of tissue destruction. Larger cup abduction angles (acetabular inclination) have been previously associated with increased risk of failure [[15], [16], [17]]. It is also surmised that the actual source of metal debris in these MoM THA may be from the trunnion junction [16,18]. However, the determination to revise these patients remains controversial. High complication rates after revision for MoM, namely infection and instability, make the decision to proceed with surgery difficult [8].
For those undergoing a primary MoM THA, the average time from surgery to revision is also unclear. One study found that 78% of revised cases within their study population were within 1 year of index surgery. This percentage increased to 92.5% within 3 years of index surgery [19]. Longer term data were not presented, and whether or not later revisions are occurring is largely unknown.
The goal of this retrospective review was to evaluate the medium- to long-term survivorship of the Pinnacle Ultamet MoM articulations, by evaluating the rate of revision and rate of osteolysis with regard to the femoral head size, neck length, stem offset, and cup abduction angles.
Material and methods
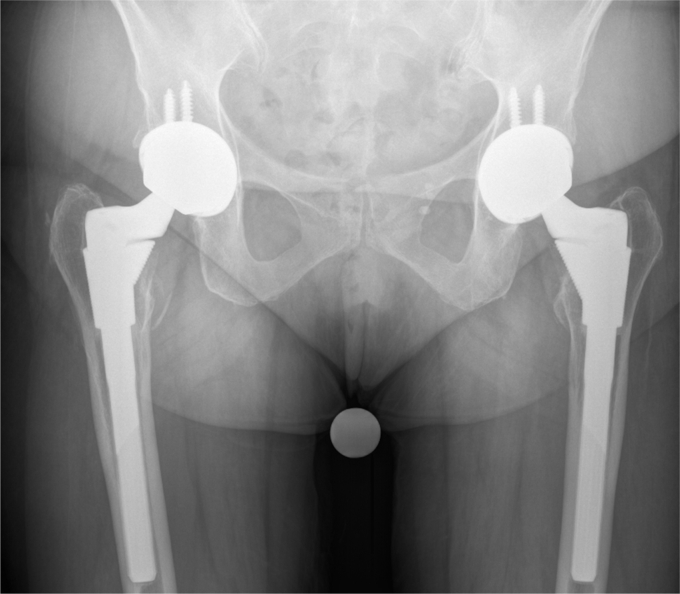
A retrospective review was conducted using the hospital’s electronic medical record and practice specific records for all primary THA procedures performed at a single institution between January 2003 and May 2008 by a single surgeon using a capsular repairing posterior approach. The study received expedited IRB approval. Follow-up was conducted through May 2019. Only procedures using the Pinnacle Ultamet (DePuy Orthopaedics Inc., Warsaw, IN) MoM articulation with the S-ROM (DePuy Orthopaedics Inc., Warsaw, IN) stem were included. Patients who returned for any amount of follow-up were included in the analysis. Patients who never returned to clinic for any postoperative follow-up were considered lost to follow-up and not included in the final analysis. Surveillance of MoM THAs included manual review of the surgeon’s electronic medical record to document the date of the most recent encounter. Encounters were reviewed for any revision details, chromium/cobalt levels, and/or metal artifact reduction sequence (MARS) MRI results. The primary outcome was the incidence rate of revision calculated using person-years as the unit of measurement; the incidence rate of osteolysis was calculated as a secondary outcome. Patient demographic and implant details were also collected. Radiographs from patients’ most recent follow-up visit (Image 1) were assessed for presence of osteolysis, and cup abduction angles were measured. Osteolysis was assessed on the most recent anteroposterior radiograph of the pelvis, or the radiograph immediately before revision, in those cases. Radiolucencies around the femoral stem and acetabular socket were assessed in comparison to prior radiographs to determine if there was progressive bone loss around the hip implant. Cases with progressive bone loss around the implants seen on the radiograph were recorded as positive for osteolysis. Revision THA procedures were recorded with corresponding dates and indications. Incidence rates for revision and osteolysis were calculated in regard to the femoral head size (28 mm, 36 mm, and 40 mm), stem offset (+0-4 mm, +6 mm, +8 mm, and +12 mm), neck length (0 mm, 3 mm, 6 mm, and 9 mm), and cup abduction angles (≤40°, 41°-50°, and >50°). Abduction angles were measured by a single, joint arthroplasty fellowship–trained reviewer who was not blinded. A horizontal line was drawn between the pelvic teardrops on the first postoperative standing anteroposterior image. An angle was then measured between this line and a second line that was drawn through the 2 farthest points apart, or bisecting the open face, on the acetabular socket. Unadjusted incidence rate ratios (IRRs) and 95% confidence intervals (CIs) are presented for the relative rate of experiencing each outcome.
Image 1.
Normal radiograph at 14.1 y of follow-up.
Results
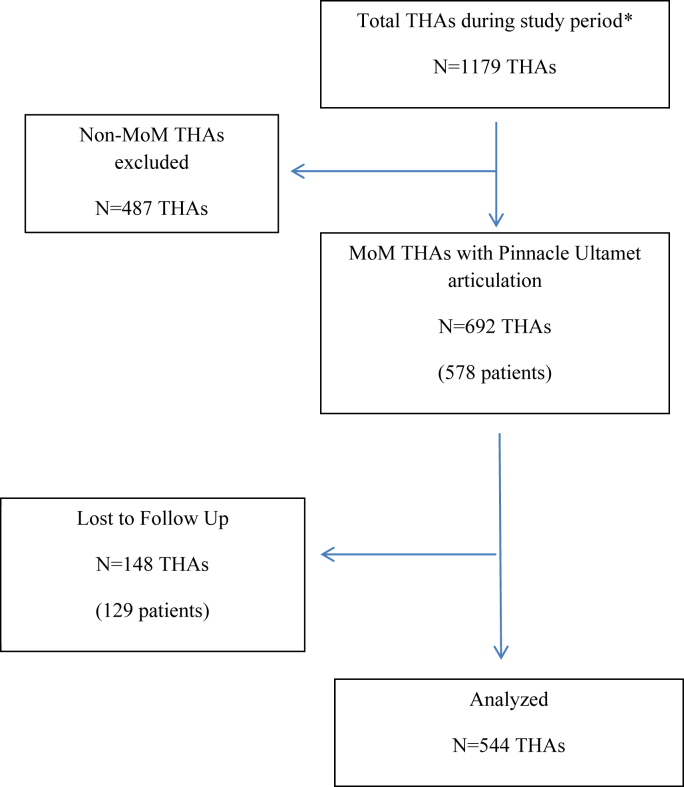
During the study timeframe, 692 THAs were identified (Fig. 1), with 544 (79%) patients returning for a median follow-up of 10.3 years (interquartile range [IQR] = 6.0-12.3). The median time to revision was 7.5 years (IQR = 5.3-9.9) among 27 total revision surgeries. The range of time to revision was 0.1-14.1 years. Patients had a mean age of 55.9 ± 8.1 years at surgery and a mean body mass index of 29.3 ± 5.7 (Table 1).
Figure 1.
Consort Diagram. ∗Primary THAs from a single surgeon at a single institution for the study period January 2003-May 2008.
Table 1.
Patient demographic and surgical characteristics, 2003-2008.
| Sample characteristics | ||
|---|---|---|
| Time to revision, y, median (IQR) | 7.5 | (5.3-9.9) |
| Follow-up time, y, median (IQR) | 10.3 | (6.0-12.3) |
| Age, years, μ (sd) | 55.9 | (8.1) |
| Body mass index, kg/m2, μ (sd) | 29.3 | (5.7) |
| Diagnosis, n (%) | ||
| Osteoarthritis (OA) | 505 | 93% |
| Secondary OA | 29 | 5% |
| Other | 10 | 2% |
| Stem Offset (mm), n (%) | ||
| 0 to +4 | 35 | 6% |
| +6 | 74 | 14% |
| +8 | 198 | 36% |
| +12 | 237 | 44% |
| Head size (mm), n (%) | ||
| 28 | 89 | 16% |
| 36 | 445 | 82% |
| 40 | 10 | 2% |
| Head length (mm), n (%) | ||
| 0 | 306 | 56% |
| 3 | 166 | 31% |
| 6 | 62 | 11% |
| 9 | 10 | 2% |
| Cup abduction angle, n (%) | ||
| ≤40° | 188 | 35% |
| 41°-50° | 313 | 58% |
| >50° | 43 | 8% |
The overall incidence rate of revision was 5.4 revisions per 1000 person-years, which was equivalent to 3.9% revisions of the 692 THAs that were identified. The incidence rate for ALTR-specific revision was 3.0 revisions per 1000 person-years. Reasons for revision included ALTR with mechanically assisted crevice corrosion (MACC) (37.0%), ALTR without MACC (7.4%), ALTR with component impingement (22.2%), failed hardware (11.1%), instability (7.4%), and infection (14.8%). Hips with a cup abduction angle of ≤40° had revisions at nearly twice the rate of those with an angle of 41°-50° (IRR = 1.98, 95% CI: 0.92, 4.29) (Table 2). Longer neck lengths also appeared to experience revisions at a faster rate than those with shorter neck lengths. In particular, hips with a neck length of 9 mm had an increased rate of revision (IRR = 5.94, 95% CI: 1.33, 26.55) relative to those with a neck length of 0 mm (Table 3). The rate of revision was otherwise similar between implants of different offsets and head sizes.
Table 2.
Incidence of revision and osteolysis by the cup abduction angle.
| ≤40° | 41°-50° (REF) | >50° | Total | |
|---|---|---|---|---|
| Revisions | ||||
| Revisions, N | 14 | 12 | 1 | 27 |
| Person-years | 1705.7 | 2901.8 | 415.9 | 5023.4 |
| Incidence ratea | 8.2 | 4.1 | 2.4 | 5.4 |
| Incidence rate ratio (IRR), 95% CI |
1.98 (0.92, 4.29) |
REF |
0.58 (0.08, 4.47) |
|
| Osteolysis | ||||
| Osteolysis, N | 14 | 18 | 2 | 34 |
| Person-years | 1705.5 | 2930.0 | 415.5 | 5051.0 |
| Incidence ratea | 8.2 | 6.1 | 4.8 | 6.7 |
| Incidence rate ratio (IRR), 95% CI | 1.34 (0.66, 2.69) | REF | 0.78 (0.18, 3.38) |
Per 1000 person-years.
Table 3.
Incidence of revision and osteolysis by the implant neck length (mm).
| 0 (REF) | 3 | 6 | 9 | Total | |
|---|---|---|---|---|---|
| Revisions, N | 12 | 8 | 5 | 2 | 27 |
| Person-years | 2874.8 | 1496.8 | 571.2 | 80.6 | 5023.4 |
| Incidence ratea | 4.2 | 5.3 | 8.8 | 24.8 | 5.4 |
| Incidence rate ratio (IRR), 95% CI |
REF |
1.28 (0.52, 3.13) |
2.10 (0.74, 5.95) |
5.94 (1.33, 26.55) |
|
| Osteolysis, N | 18 | 10 | 6 | 0 | 34 |
| Person-years | 2897.6 | 1513.3 | 559.6 | 80.5 | 5051.0 |
| Incidence ratea | 6.2 | 6.6 | 10.7 | 0.0 | 6.7 |
| Incidence rate ratio (IRR), 95% CI | REF | 1.06 (0.49, 2.30) | 1.73 (0.69, 4.35) | b |
Per 1000 person-years.
IRR not calculated because zero events occurred.
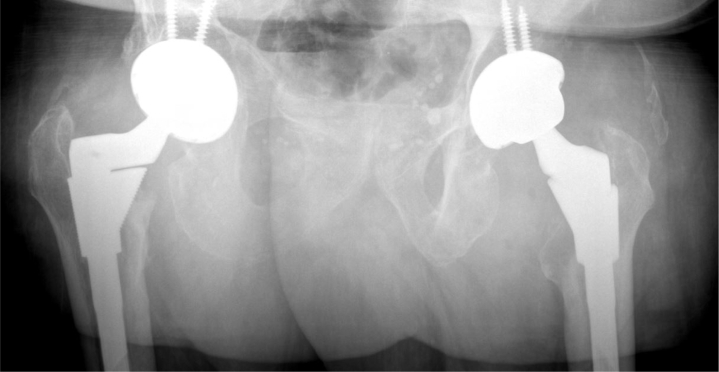
There were 34 cases that had radiographic evidence of osteolysis (Image 3) at follow-up. The overall rate of osteolysis was 6.7 osteolysis events per 1000 person-years. Hips with a stem offset of >+8 had a decreased rate of osteolysis relative to those with an offset of +8 (IRR = 0.51, 95% CI: 0.24, 1.08) (Table 4). Rates of osteolysis were similar between implants of different head sizes, neck lengths, and cup abduction angles.
Image 3.
Radiograph with osteolysis present at 8.5 y of follow-up.
Table 4.
Incidence of revision and osteolysis by implant offset (mm).
| +0-4 | +6 | +8 (REF) | +12 | Total | |
|---|---|---|---|---|---|
| Revisions | |||||
| Revisions, N | 3 | 3 | 13 | 8 | 27 |
| Person-years | 375.0 | 675.4 | 1978.4 | 1994.6 | 5023.4 |
| Incidence ratea | 8.0 | 4.4 | 6.6 | 4.0 | 5.4 |
| Incidence rate ratio (IRR), 95% CI |
1.22 (0.35, 4.27) |
0.68 (0.19, 2.37) |
REF |
0.61 (0.25, 1.47) |
|
| Osteolysis | |||||
| Osteolysis, N | 1 | 3 | 20 | 10 | 34 |
| Person-years | 374.8 | 671.4 | 2013.7 | 1991.3 | 5051.2 |
| Incidence ratea | 2.7 | 4.5 | 9.9 | 5.0 | 6.7 |
| Incidence rate ratio (IRR), 95% CI | 0.27 (0.04, 2.00) | 0.45 (0.13, 1.51) | REF | 0.51 (0.24, 1.08) |
Per 1000 person-years.
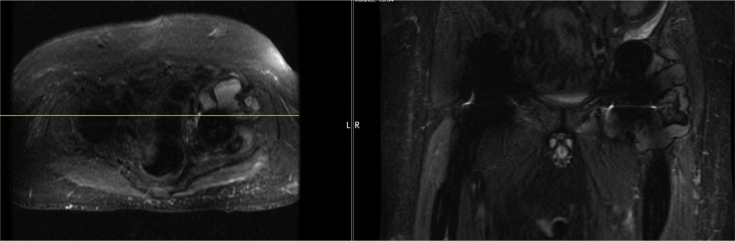
We were unable to report chromium/cobalt levels because of inconsistency of serum ion level testing. Not all subjects who were revised had chromium/cobalt levels tested and if they did, this only served as one factor in the surgeon’s decision to perform a revision. While 70 subjects had a MARS MRI after their index surgery to check for the presence of a pseudotumor, only 14 (51.9%) of the revised cases had a MARS MRI, which makes it difficult to report pseudotumor trends among revised and unrevised populations.
Discussion
The results of this study suggest that the survivorship of MoM hips may be relatively high (5.4 revisions per 1000 person-years). Grübl et al. [13] had previously reported a high survivorship of with a 98.6% probability of survival at 10 years of follow-up in their cohort of MoM THAs.
Subjects were followed up for a median time of 10.3 years (IQR = 6.0-12.3) (Table 1).The primary endpoint of the study was revision, which occurred at median of 7.5 years (IQR = 5.3-9.9) after index surgery. The time to revision was much later in our study (range = 0.1-14.1 years) when compared with previous literature (range = 1-3 years) [19]. However, Matharu et al. [20] reported a 5-year survivorship of 92.3%, which points to the variability in survivorship among MoM implants. This makes predicting who may need revision based on life of the implant difficult and likely inaccurate.1
The cup abduction angle had a statistically significant correlation with revision and failure. Lower cup abductions angles seemed to correlate with increased risk of revision, contradictory to previous literature which pointed to increased risk of revision with higher cup abduction angles [16], [21]. The high abduction angle was thought to lead to edge loading and subsequent metal wear. In this study, the wear may be related to neck-on-cup impingement and has less to do with the actual MoM articulation. A study by Haan et al found mechanical symptoms such as impingement, to be the main presenting symptoms for revision in MoM THAs [22]. It is possible that flatter cups, or smaller abduction angles, may lead to more of this type of impingement and need for revision.
Implants with longer neck lengths were also more likely to undergo a revision when compared to those with a neck length of 0 mm (IRR: 5.94, 95% CI: 1.33, 26.55) (Table 3). This suggests that the trunnion may be the significant metal ion generator, as the longer neck length may lead to more strain and micromotion along the stem-head junction. It has been previously reported that the S-ROM stem may lead to increased metal ions and possible metallosis because of its modular features at the stem/body junction. The S-ROM stem has been used extensively with MoM THA, and although its modular feature offers a variety of offsets and neck lengths, it has an additional metal junction [7]. Laaksonen et al. [7] found that S-ROM stems were 3.8 times more likely to have osteolysis and 7.8 times more likely to have radiolucency than those treated with Summit stems. Thirty three percentages of their S-ROM stems experienced osteolysis. Another study found that 5.9% of hips with S-ROM stems experienced osteolysis at a minimum 2-year follow-up, 2 of which underwent revision [9]. On the contrary, Hothi et al. [23] found the S-ROM to be protective compared with the Summit and Corail. Overall, our data suggest that when using this modular stem, the trunnion may be overwhelmed by longer neck heads. Nassif et al. [24] found a greater likelihood of fretting and corrosion in the thicker 11/13 tapers with longer contact lengths. It is possible that the different taper (11/13) on the S-ROM may not be able to withstand the potentially greater forces associated with a longer neck length.
Previous studies have shown that when using metal heads, larger sizes produce greater stress at the trunnion and are associated with greater revision rates [19,[25], [26], [27]]. In this study, the femoral head size and offset had no correlation with whether or not the patient was revised, or had any signs of ALTR (Table 5). However, the head size may not show significant correlation because of the low number of 32 mm heads used in this cohort. If more patients had 32 mm heads in place, instead of 36 mm, there may have been enough power to see a statistical difference. It is also possible that the 36 mm head on the S-ROM taper does not have a true effect on MACC, but it is impossible to determine without increased power.
Table 5.
Incidence of revision and osteolysis by the implant head size (mm).
| 28 | 36 (REF) | 40 | Total | |
|---|---|---|---|---|
| Revisions, N | 3 | 23 | 1 | 27 |
| Person-years | 843.3 | 4123.2 | 56.9 | 5023.4 |
| Incidence ratea | 3.6 | 5.6 | 17.6 | 5.4 |
| Incidence rate ratio (IRR), 95% CI |
0.64 (0.19, 2.12) |
REF |
3.15 (0.43, 23.31) |
|
| Osteolysis, N | 2 | 32 | 0 | 34 |
| Person-years | 851.4 | 4142.8 | 56.9 | 5051.1 |
| Incidence ratea | 2.3 | 7.7 | 0.0 | 6.7 |
| Incidence rate ratio (IRR), 95% CI | 0.30 (0.07, 1.27) | REF | b |
Per 1000 person-years.
IRR not calculated because zero events occurred.
Hips with a stem offset of >+8 had a decreased rate of osteolysis relative to those with an offset of +8 (IRR = 0.51, 95% CI: 0.24, 1.08) (Table 4). However, rates of osteolysis did not correlate with revision rates as expected. This may be due to the low incidence of revision in this population in general, as well as the low incidence of osteolysis at follow-up. The 2 outcomes simply did not cross over because of the small numbers. With a larger sample, more could potentially be said about likelihood of undergoing a revision in regard to the presence of osteolysis.
We were not able to report revisions in regard to chromium/cobalt levels because of a lack of consistency in testing and timing of testing. We did not complete the tracking of metal ion levels for each subject during data collection because there was not a consistent pattern of people who were being tested and whether or not they went on to have a revision. Because not all patients in the cohort had metal ion levels checked, no definitive conclusions can be made regarding how this information should guide surgeons. However, laboratory tests could still prove useful for detecting potential problems in this population or at least alert the surgeon that there is metal debris present.
The lack of routine MRI use in this study also limits our ability to report whether or not MRI results had a correlation with those patients with osteolysis or who required revision surgery. From this study, recommendations regarding MRI are limited to the purposes of defining the extent of soft tissue destruction and proving the presence of ALTR, if not already clear from plain radiographs.
Previous literature has pointed to patterns that have emerged in ways to care for and diagnose issues surrounding MoM implants. These patterns have led to the establishment of an algorithmic approach to MoM arthroplasty management including review of clinical symptoms, radiographs (osteolysis and implant position), ion measurements, Erythrocyte sedimentation rate and C-reactive protein values, MARS MRI, joint aspiration, and implant track record [8].
The limitations of this article are those which are inherent to any retrospective study. Follow-up was incomplete, as a large proportion of patients did not come back for their routine 10-year clinic appointment. It is possible that participants received revision surgery elsewhere, which would lead to an underestimation of the rate of MoM revision. It is also possible that these patients were either deceased, had moved, or chose not to respond to the requests to come in for an appointment because they were not having problems with their MoM hip. Another limitation is that all hips in this study were implanted by a single surgeon, making these results less generalizable. Because of this, the study only reviewed a single type of implant by a single manufacturer, which again decreases the generalizability.
Conclusions
The low overall rate of revision for this MoM implant is reassuring for surgeons monitoring this patient population, particularly in the face of a potential difficult revision surgery, and serious postoperative complications. Lower cup abduction angles and longer neck lengths in MoM implants may predict the need for revision surgery. It is important for surgeons to take into account the implant specifications when making a diagnosis of ALTR and deciding whether or not to proceed with revision. MoM implants continue to be a challenge, but the data presented here, combined with patient evaluation and radiologic and laboratory studies, can help guide the treatment of this population, leading to prudent decision-making regarding if and when these patients should be revised.
Footnotes
One or more of the authors of this paper have disclosed potential or pertinent conflicts of interest, which may include receipt of payment, either direct or indirect, institutional support, or association with an entity in the biomedical field which may be perceived to have potential conflict of interest with this work. For full disclosure statements refer to https://doi.org/10.1016/j.artd.2020.02.010.
Conflict of interests: The authors declare the following financial interests/personal relationships which may be considered as potential competing interests: Royalties from a DePuy and Speakers bureau/paid presentations for DePuy.
Appendix A. Supplementary data
Appendix
Supplementary images
Image 2.
MRI with pseudotumor present at 8.5 y of follow-up.
References
- 1.Hosman A.H., van der Mei H.C., Bulstra S.K., Busscher H.J., Neut D. Effects of metal-on-metal wear on the host immune system and infection in hip arthroplasty. Acta Orthop. 2010;81(5):526. doi: 10.3109/17453674.2010.519169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Dumbleton J.H., Manley M.T. Metal-on-Metal total hip replacement: what does the literature say? J Arthroplasty. 2005;20(2):174. doi: 10.1016/j.arth.2004.08.011. [DOI] [PubMed] [Google Scholar]
- 3.Bozic K.J., Kurtz S., Lau E. The epidemiology of bearing surface usage in total hip arthroplasty in the United States. J Bone Joint Surg Am. 2009;91(7):1614. doi: 10.2106/JBJS.H.01220. [DOI] [PubMed] [Google Scholar]
- 4.Amstutz H.C., Grigoris P. Metal on metal bearings in hip arthroplasty. Clin Orthop Relat Res. 1996;329:S11. doi: 10.1097/00003086-199608001-00003. [DOI] [PubMed] [Google Scholar]
- 5.Cuckler J.M., Moore K.D., Lombardi A.V., McPherson E., Emerson R. Large versus small femoral heads in metal-on-metal total hip arthroplasty. J Arthroplasty. 2004;19(8, Supplement):41. doi: 10.1016/j.arth.2004.09.006. [DOI] [PubMed] [Google Scholar]
- 6.MacDonald S., McCalden R., Chess D. Metal-on-Metal versus polyethylene in hip arthroplasty: a randomized clinical trial. Clin Orthop Relat Res. 2003;406(1):282. doi: 10.1097/01.blo.0000043066.62337.9d. [DOI] [PubMed] [Google Scholar]
- 7.Laaksonen I., Galea V.P., Connelly J.W., Matuszak S.J., Muratoglu O.K., Malchau H. Inferior radiographic and functional outcomes with modular stem in metal-on-metal total hip arthroplasty. J Arthroplasty. 2018;33(2):464. doi: 10.1016/j.arth.2017.08.042. [DOI] [PubMed] [Google Scholar]
- 8.Lombardi J.A.V., Barrack R.L., Berend K.R. The Hip Society: algorithmic approach to diagnosis and management of metal-on-metal arthroplasty. J Bone Joint Surg Br. 2012;94-B(11_Supple_A):14. doi: 10.1302/0301-620X.94B11.30680. [DOI] [PubMed] [Google Scholar]
- 9.Park Y.-S., Moon Y.-W., Lim S.-J., Yang J.-M., Ahn G., Choi Y.-L. Early osteolysis following second-generation metal-on-metal hip replacement. J Bone Joint Surg Am. 2005;87(7):1515. doi: 10.2106/JBJS.D.02641. [DOI] [PubMed] [Google Scholar]
- 10.Huang D.-C.T., Tatman P., Mehle S., Gioe T.J. Cumulative revision rate is higher in metal-on-metal THA than metal-on-polyethylene THA: analysis of survival in a community registry. Clin Orthop Relat Res. 2013;471(6):1920. doi: 10.1007/s11999-013-2821-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cobb A.G., Schmalzreid T.P. The clinical significance of metal ion release from cobalt-chromium metal-on-metal hip joint arthroplasty. Proc Inst Mech Eng H. 2006;220(2):385. doi: 10.1243/09544119JEIM78. [DOI] [PubMed] [Google Scholar]
- 12.deSouza R.M., Parsons N.R., Oni T., Dalton P., Costa M., Krikler S. Metal ion levels following resurfacing arthroplasty of the hip. J Bone Joint Surg Br. 2010;92-B(12):1642. doi: 10.1302/0301-620X.92B12.24654. [DOI] [PubMed] [Google Scholar]
- 13.Grübl A., Marker M., Brodner W. Long-term follow-up of metal-on-metal total hip replacement. J Orthop Res. 2007;25(7):841. doi: 10.1002/jor.20381. [DOI] [PubMed] [Google Scholar]
- 14.Bolognesi M.P., Ledford C.K. Metal-on-Metal total hip arthroplasty: patient evaluation and treatment. J Am Acad Orthop Surg. 2015;23(12):724. doi: 10.5435/JAAOS-D-14-00183. [DOI] [PubMed] [Google Scholar]
- 15.Hart A.J.M., Muirhead-Allwood S.F., Porter M.F. Which factors determine the wear rate of large-diameter metal-on-metal hip replacements?: multivariate analysis of two hundred and seventy-six components. J Bone Joint Surg Am. 2013;95(8):678. doi: 10.2106/JBJS.J.01447. [DOI] [PubMed] [Google Scholar]
- 16.Langton D.J., Jameson S.S., Joyce T.J., Hallab N.J., Natu S., Nargol A.V.F. Early failure of metal-on-metal bearings in hip resurfacing and large-diameter total hip replacement. J Bone Joint Surg Br. 2010;92-B(1):38. doi: 10.1302/0301-620X.92B1.22770. [DOI] [PubMed] [Google Scholar]
- 17.Grammatopoulos G., Pandit H., Glyn-Jones S. Optimal acetabular orientation for hip resurfacing. J Bone Joint Surg Br. 2010;92-B(8):1072. doi: 10.1302/0301-620X.92B8.24194. [DOI] [PubMed] [Google Scholar]
- 18.Brock T.M., Sidaginamale R., Rushton S. Shorter, rough trunnion surfaces are associated with higher taper wear rates than longer, smooth trunnion surfaces in a contemporary large head metal-on-metal total hip arthroplasty system. J Orthop Res. 2015;33(12):1868. doi: 10.1002/jor.22970. [DOI] [PubMed] [Google Scholar]
- 19.Fabi D., Levine B., Paprosky W. Metal-on-Metal total hip arthroplasty: causes and high incidence of early failure. Orthopedics. 2012;35(7):e1009. doi: 10.3928/01477447-20120621-12. [DOI] [PubMed] [Google Scholar]
- 20.Matharu G.S., Judge A., Murray D.W., Pandit H.G. Outcomes after metal-on-metal hip revision surgery depend on the reason for failure. Clin Orthop Relat Res. 2018;476(2):245. doi: 10.1007/s11999.0000000000000029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ebramzadeh E., Campbell P.A., Takamura K.M. Failure modes of 433 metal-on-metal hip implants: how, why, and wear. Orthop Clin North Am. 2011;42(2):241. doi: 10.1016/j.ocl.2011.01.001. [DOI] [PubMed] [Google Scholar]
- 22.Haan R.D., Campbell P.A., Su E.P., Smet K.A.D. Revision of metal-on-metal resurfacing arthroplasty of the hip. J Bone Joint Surg Br. 2008;90-B(9):1158. doi: 10.1302/0301-620X.90B9.19891. [DOI] [PubMed] [Google Scholar]
- 23.Hothi H.S., Eskelinen A.P., Berber R. Factors associated with trunnionosis in the metal-on-metal Pinnacle hip. J Arthroplasty. 2017;32(1):286. doi: 10.1016/j.arth.2016.06.038. [DOI] [PubMed] [Google Scholar]
- 24.Nassif N.A., Nawabi D.H., Stoner K., Elpers M., Wright T., Padgett D.E. Taper design affects failure of large-head metal-on-metal total hip replacements. Clin Orthop Relat Res. 2013;472(2):564. doi: 10.1007/s11999-013-3115-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Smith A.J., Dieppe P., Vernon K., Porter M., Blom A.W. National joint registry of england and wales. Failure rates of stemmed metal-on-metal hip replacements: analysis of data from the National joint registry of england and wales. Lancet. 2012;379(9822):1199. doi: 10.1016/S0140-6736(12)60353-5. [DOI] [PubMed] [Google Scholar]
- 26.Del Balso C., Teeter M.G., Tan S.C., Howard J.L., Lanting B.A. Trunnionosis: does head size affect fretting and corrosion in total hip arthroplasty? J Arthroplasty. 2016;31(10):2332. doi: 10.1016/j.arth.2016.03.009. [DOI] [PubMed] [Google Scholar]
- 27.Dyrkacz R.M.R., Brandt J.-M., Ojo O.A., Turgeon T.R., Wyss U.P. The influence of head size on corrosion and fretting behaviour at the head-neck Interface of artificial hip joints. J Arthroplasty. 2013;28(6):1036. doi: 10.1016/j.arth.2012.10.017. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.