Abstract
Background:
The cause of death (COD) statement is a vital statistic that refers to the disease(s) and process(es) that lead to death. Obtaining accurate COD is valuable for mortality prevention priorities. The statements are formulated using International Classification of Diseases and related health problems, version 10 (ICD-10) system. However, physicians may be unfamiliar with these standards or fail to use them and instead refer to mechanisms or manner of death when stating COD. We present results of an of assessment of quality of COD statements in decedent cases reviewed during a one-month mortuary-based surveillance at Kenyatta National Hospital (KNH) and the City mortuaries in Nairobi, Kenya in 2015.
Methods:
Quality elements reviewed were completeness, correctness and order of stating the immediate (ICOD), antecedent, underlying (UCOD), and other significant causes (OSCs) as per the ICD 10 standards, in all deaths reported among adolescents and adults aged 15 years or older at the two mortuaries. COD were assessed for correct sequencing from immediate, antecedent, to underlying compared with autopsy pathology and clinical findings where available. Errors in COD statements were classified as missing or containing incomplete information such as: lack of underlying cause of an injury; incorrect words or statements; presence of more than one competing COD; use of the mechanism of death or anatomic and physiologic processes or signs and symptoms, and or laboratory results as CODs. Pearson’s χ-squared test was used to compare proportions.
Results:
Out of 810, 610 (75.3%) deaths having HIV statuses were abstracted and 356 had at least one COD documented; 114 (32%) females and 242 (68%) males; 239 (67.1%) from KNH and 117 (32.9%) City mortuary. The cases from City mortuary had higher rates of correct statements on 116 (99.1%) ICOD, 90 (89.1%) UCOD, and 40 (81.6%) OSCs, compared to KNH Mortuary; 50 (20.9%), 200 (90.1%) and 62 (76.5%) respectively, p < 0.001. The most common type of errors was incomplete information and citing mechanisms of death as the COD.
Conclusions:
In addition to revising national forms to conform to ICD-10, there is a need for periodic training of individuals responsible for completing death certificates. This will improve correctness and completeness of COD in order to provide reliable mortality data in Kenya.
Keywords: Cause of death (COD), Errors for COD statements, ICD-10, Mortuary surveillance, Death certificate (DC)
1. Background
A death certificate (DC) is an important document for medicolegal reasons, inheritance purposes, processing life insurance claims, and national health planning.1 A key element in the DC is the cause of death (COD) statement that consists of words indicating CODs and other significant conditions or diseases present that may or may not have contributed to death. The World Health Organization International Classification of Diseases and related health problems, Version 10 (ICD-10) is designed to promote international comparability in the collection, processing, classification, and presentation of mortality statis tics, hence it is a useful tool in writing COD statements.2 The ICD-10 also provides a format for reporting CODs on the DC. The reported conditions are then translated into medical codes through use of a classification structure according to the selection and modification rules contained in the ICD. The ICD coding rules improve the usefulness of mortality statistics by giving preference to certain categories of causes, by consolidating conditions, and by systematically selecting a single COD from a reported sequence of conditions. The single selected cause is called the underlying cause of death (UCOD). The UCOD is usually preceded by an immediate COD (ICOD). The UCOD is defined as (1) the disease or injury that initiated the train of morbid events leading directly to death or (2) the circumstances of the accident or violence, which produced the fatal injury. The aim for proper identification of the UCOD is to support prevention of future occurrences of similar deaths.3 Other significant causes (OSC) are the non-underlying CODs, but may contribute to mortality. The combination of underlying and non-underlying causes forms the multiple CODs. In determining the ICOD and UCOD, physicians use the principle of Occam’s razor, where the simplest explanation that could give rise to the observations is selected. Although these guidelines for COD statements are widely available, they are often not utilized by physicians in the filling of DCs.
Quality COD statements are prerequisites for quality DCs and COD statistics. These data are a cornerstone for health policy-making and medical research worldwide. The data provide statistical information useful for mortality surveillance, epidemiologic research, public health planning, and resource allocation for health and safety research projects.3
COD coding practices remain inadequate in most developing countries.4 In Kenya, as in most low- and medium-income countries, death notification is done by medical doctors at various levels of training and experience. Most deaths are certified by junior doctors, mainly interns, clinical officers, and medical officers, while fewer are certified by pathologists where postmortems are conducted. The information is entered in a death notification form (D1), and a copy is referred to the registrar of births and deaths at the Attorney General’s offices. The officers who subsequently abstract the information from these notification forms are non-medical personnel, and therefore require that COD statements be clear to support proper abstraction. COD statements that are abstracted and transferred into DCs are used for purposes of generating vital statistics. Poor quality COD statements therefore may have financial, medicolegal, and policy implications.
The quality of COD statements may vary by age group. The elderly, for example, may have the most errors because multiple natural diseases or co-morbidities such as cerebrovascular, cardiovascular or neurologic disease and/or dementia. In ascertaining COD, some of these causes might be overlooked hence the dictum that “the elderly die with their disease and not of their disease”. In addition, death certificates for the elderly often list other conditions such as pathological fractures that may be mistaken as an UCOD.3
Various studies have shown variable and high death certificate completion. In a U.S. study conducted in Atlanta, GA about 47% of the errors in DCs involved omissions, incomplete, and incorrect information.5 Maharjan, in an intensive care unit study, found that 78.4% of DCs had errors. This included errors in the terminology, serialization, or completeness of the COD statement.1
In our study, the immediate, underlying, and other CODs statements in all the available cases among adolescents and adults aged 15 years or older were reviewed, completeness and correctness of each of the statements using the ICD-10 criteria was determined.
2. Methodology
2.1. Study setting and design
The study was carried out as part of the HIV/AIDS mortality surveillance study at the Kenyatta National Hospital (KNH) Mortuary and the City Mortuary, the two largest mortuary facilities in Kenya. The two are in Nairobi, the capital of Kenya. The study was descriptive and cross-sectional. All deaths regardless of the underlying cause among adolescents and adults aged 15 years or older that occurred from Jan 29 to Mar 3, in 2015 at both mortuaries were included in the analysis. Since the purpose of the primary study was to estimate the HIV-associated mortality, all the records included in this manuscript had an HIV status available. Additionally, the targeted age group was based on the definition of age for patients considered to be adults for clinical and programmatic considerations in HIV programs worldwide. The data were obtained from the postmortem case summaries of the COD statements following autopsy at KNH Mortuary and City Mortuary in Nairobi. Deaths occurring at KNH also had in-patient medical records and COD certified by the attending physician whereas most cadavers at City mortuary are from accidents scenes and other trauma and injuries and hence will not have a medical record.
2.2. Data retrieval and analyses
A team of medical health records officers who had undergone training in ICD10 coding rules retrieved and reviewed all files and death notification documents from the hospital records or mortuary data for KNH and City Mortuary cases respectively. The team of abstractors were supervised by a pathologist and the principal investigator of the project.
The COD statements in the DCs and notifications contains two parts as per ICD-10. Part I for reporting the sequence of events leading to death, namely the ICOD, proceeding backwards from the final disease or condition that resulted in death. Generally, only one condition should be listed per line. A specific COD, namely the UCOD, was expected to be reported in the last entry in Part I of the death notification form. Therefore, the last event was expected to come first, and the first event to come last chronologically. Part II of the COD statement details OSCs that may or may not have contributed to the death but did not lead to the underlying cause.6,7 In order to be considered a properly completed COD section, it was expected to provide an etiologic explanation of the sequence, type, and association of events resulting in death.7 The sequence and logic of the events and occurrences was also reviewed. The reviewers worked independently and looked for the errors in the statements as follows: missing information; improper sequencing of information on the COD; incorrect words or statements on the COD. We also checked for incomplete information such as lack of underlying cause of an injury. We looked for improper sequencing such as: more than one competing COD at one level (e.g. inclusion of hypertension and diabetes mellitus as UCODs); use of the mechanism of death such as cardio-respiratory arrest; use of anatomic and physiologic processes like a space occupying lesion; use of signs and symptoms and laboratory results such as breathlessness or pancytopenia among others. Upon completion of the review process, the panel of authors, collated and published the findings.
The CODs were grouped as per a modified Global Burden of Disease (GBD) system,8 as follows: Ia) Communicable diseases, perinatal, maternal, and nutritional, excluding HIV/AIDS; Ib) HIV/AIDS-related deaths; II) Non-communicable diseases; and III) Injuries and unnatural deaths. Thus, we subdivided HIV/AIDS-related deaths from other Group I causes.
2.3. Data analyses
The data were entered in Epi-Info™, cleaned and analyzed using Stata (version 14.1, Stata Corp, College Station, TX, USA). The dependent variable was the occurrence of error in the DC while independent variables were sex, age, and presence of infection (sepsis), organ failure, hemorrhage, or multiple injuries among others. Descriptive data analysis was performed to show the prevalence and types of errors in DCs and the other related variables. Comparative analysis was performed amongst different types of errors prevalent in ICODs, UCODs, and OSCs. Pearson’s chi-squared test was used to determine the association of occurrence of error in DCs with the independent variables. A p-value of <0.05 was considered as the cut-off point for statistical significance.
3. Results
A total of 810 eligible decedents were identified that met the study inclusion criteria. Out of these, 610 had data on HIV status available, of whom 356 had at least one COD documented. Reasons for unavailability of COD included transfer of cadaver to another facility prior to autopsy and/or inability to trace the medical record or pathology report. Of the 356 with at least one COD, 114 (32%) were females and 242 (68%) males. Fifty-one percent of the decedents were aged between 25 and 44 years. The cases from KNH Mortuary and City Mortuary were 239 (67.1%) and 117 (32.9%) respectively (Fig. 1). A summary of CODs is presented elsewhere,.9 City Mortuary had a majority of correctly stated CODs regardless of cause. The cases from City Mortuary had a higher proportion of correct statements on 116 (99.1%) ICOD, 90 (89.1%) UCOD, and 40 (81.6%) OSCs, compared to KNH Mortuary that had 50 (20.9%), 200 (90.1%) and 62 (76.5%) respectively. Differences were significant for ICOD, p < 0.001. ICODs had a majority of incorrect statements for all types of disease categories, as per GBD. The UCOD and OSCs were mostly correctly stated (Table 1).
Fig. 1. Number of cases with causes of death at City Mortuary and Kenyatta National Hospital Mortuary, Kenya, 2015, n = 356.
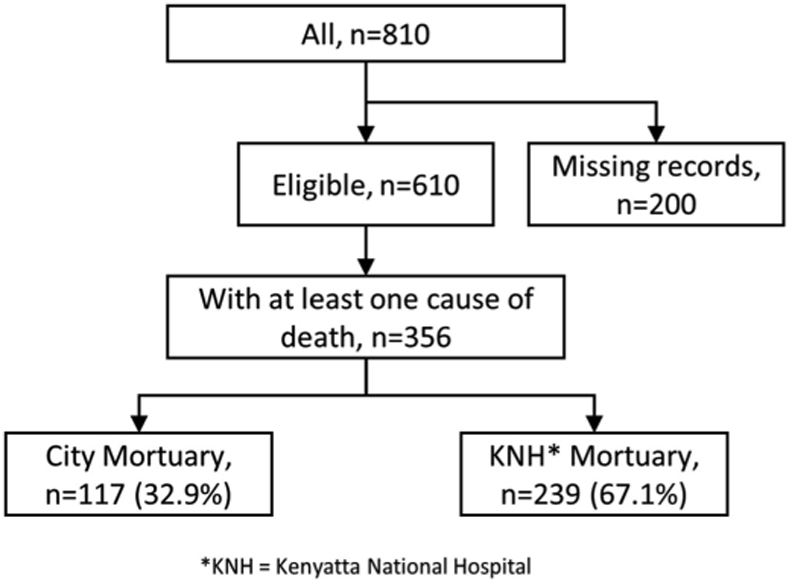
The figure shows the number of records with at least one cause of death reviewed at city and Kenyatta National Hospital mortuaries.
Table 1.
Distribution of correctly stated causes of death by sex, mortuary, and Global Burden of Disease Group using ICD -10 criteria, Kenya, 2015, n = 356.
| Variable |
Total (any COD) |
Immediate COD (n= 356) |
Underlying COD (n= 323) |
OSCa (n = 130) |
|||
|---|---|---|---|---|---|---|---|
| N (%b) | N (%c) | pd | N (%c) | pd | N (%c) | pd | |
| Total | 356 | 166 (46.6) | 290 (89.8) | 102 (78.5) | |||
| Sex | <0.001 | 0.154 | 0.593 | ||||
| Female | 114 (32) | 23 (20.2) | 97 (93.3) | 23 (82.1) | |||
| Male | 242 (68) | 143 (59.1) | 193 (88.1) | 79 (77.5) | |||
| Mortuary | <0.001 | 0.787 | 0.494 | ||||
| City | 117 (32.9) | 116 (99.1) | 90 (89.1) | 40 (81.6) | |||
| KNHe | 239 (67.1) | 50 (20.9) | 200 (90.1) | 62 (76.5) | |||
| GBD classesf | <0.001 | 0.292 | 0.716 | ||||
| Ia (excluding HIV) | 28 (7.9) | 10 (35.7) | 17 (81) | 6 (85.7) | |||
| Ib (HIV) | 45 (12.6) | 5 (11.1) | 38 (92.7) | 17 (77.3) | |||
| II | 147 (41.3) | 30 (20.4) | 114 (87.7) | 23 (71.9) | |||
| III | 136 (38.2) | 121 (89) | 121 (92.4) | 56 (81.2) | |||
NOTE: n = 356 contained at least one documented COD, the UCOD and OSC were not available for the entire n.
Other significant causes.
Column percentage.
Row percentage.
p-value.
Kenyatta National Hospital.
Global Burden of Disease classes: Ia Communicable diseases, perinatal, maternal, and nutritional, excluding HIV/AIDS; Ib HIV/AIDS-related deaths; II Non-communicable diseases and; III Injuries and unnatural deaths.
Most of the errors on the ICOD were due to either incomplete information or citing a mechanism of death as a COD (Table 2). All of the errors on the ICOD for City Mortuary, (66) were due to incomplete information; while at KNH 18 (8.8%) errors were due to incomplete information and 187 (91.2%), were due to reporting mechanism of death as a cause for KNH. This difference in cause of errors by mortuary was statistically significant (p < 0.001).
Table 2.
Types of errors and statements on immediate, underlying and other significant causes of death at City Mortuary and Kenyatta National Hospital Mortuary, based on the ICD-10 two-tier format, Kenya 2015.
| All |
Mortuary |
|||
|---|---|---|---|---|
| Error types | N (%) | City, N (%) | KNH, N (%) | P values |
| Types of errors for ICODa | <0.001 | |||
| Incomplete information | 84 (31.0) | 66 (100) | 18 (8.8) | |
| Mechanism of death | 187 | 0 (0) | 187 (91.2) | |
| (69.0) | ||||
| Types of errors for UCODb | 0.402 | |||
| Improper sequence | 9 (5.8) | 1 (2.9) | 8 (6.6) | |
| Incorrect statement | 3 (1.9) | 1 (2.9) | 2 (1.7) | |
| Incomplete informationc | 84 (31) | 66 (100) | 18 (8.8) | |
| >1 competing COD | 5 (3.2) | 0 (0) | 5 (4.1) | |
| Mechanism of death | 187 (69) | 0 (0) | 187 (91.2) | |
| Physiologic process | 5 (3.2) | 1 (2.9) | 4 (3.3) | |
| Symptomsd | 14 (9) | 1 (2.9) | 13 (10.7) | |
| Statements on OSCe | 0.051 | |||
| None | 303 | 115 (99.1) | 188 (94.9) | |
| (96.5) | ||||
| Present | 11 (3.5) | 1(0.9) | 10 (5.1) | |
NOTE: n = 356 contains all data including undocumented COD.
132 (35.2%) records that had multiple errors.
Immediate COD.
Underlying COD.
Lack of information on the underlying cause of blunt force trauma.
Pancytopenia.
Other significant COD.
The most common type of error for the UCOD was incomplete information, such as lack of information on the cause of blunt force trauma, as seen in majority of the injury-related deaths. The difference in reasons for errors in the UCOD was not statistically significant between the two sites (p = 0.402). Most cases did not have OSCs cited, but 10 out of 11 reported OSCs were from the City Mortuary. This difference in presence of OSC between mortuaries was not statistically significant (p = 0.051).
The sequence of stating the COD statement was mostly correct with City Mortuary at 100 (85.5%) and KNH Mortuary at 228 (97.4%), (Table 3). Most errors were due to incomplete information stated. Only 57 (16.2%) cases from both sites had complete information stated. The correct terminology was used in a total of 166 (46.6%) cases; most of the correct statements were from City Mortuary 116 (99.1%).
Table 3.
Correctness, completeness, and sequencing of immediate cause of death by mortuary, global burden of disease, sex, and age.
| Variable |
Total |
With correct statement |
With complete statement |
With correct sequence |
|||
|---|---|---|---|---|---|---|---|
| N (%a) | N (%b) | p-value | N (%b) | p-value | N (%b) | p-value | |
| Total | 356 | 166 (46.6) | 57(16.2) | 328 (93.5) | |||
| Mortuary | <0.001 | <0.001 | <0.001 | ||||
| City | 117 (32.9) | 116 (99.1) | 34 (29.1) | 100 (85.5) | |||
| KNH | 239 (67.1) | 50 (20.9) | 23 (9.8) | 228 (97.4) | |||
| GBD for UCOD | <0.001 | 0.066 | 0.804 | ||||
| Group Iac | 46 (14.6) | 8 (17.4) | 4 (8.9) | 44 (97.8) | |||
| Group Ia & II | 3 (0.9) | 0 (0) | 0 (0) | 3 (100) | |||
| Group Ibd | 15 (4.7) | 2 (13.3) | 3 (20) | 15 (100) | |||
| Group II | 97 (30.7) | 13 (13.4) | 10 (10.3) | 94 (96.9) | |||
| Group IIIe | 116 (36.7) | 106 (91.4) | 26 (22.4) | 114 (98.3) | |||
| Undassifiable | 39 (12.3) | 8 (20.5) | 3 (8.1) | 33 (94.3) | |||
| Sex | <0.001 | 0.828 | 0.110 | ||||
| Female | 114 (32) | 23 (20.2) | 19 (16.8) | 110 (96.5) | |||
| Male | 242 (68) | 143 (59.1) | 38 (15.9) | 218 (92) | |||
| Age categories | <0.001 | 0.032 | 0.085 | ||||
| 15-24 | 40 (11.2) | 32 (80) | 11 (27.5) | 37 (92.5) | |||
| 25-34 | 96 (27) | 59 (61.5) | 20 (20.8) | 88 (91.7) | |||
| 35-44 | 86 (24.2) | 37 (43) | 15 (17.4) | 83 (96.5) | |||
| 45-54 | 53 (14.9) | 19 (35.8) | 7(14) | 43 (86) | |||
| 55-64 | 36 (10.1) | 12 (33.3) | 2 (5.6) | 36 (100) | |||
| 65-74 | 21 (5.9) | 4(19) | 2(10) | 17 (89.5) | |||
| 75+ | 24 (6.7) | 3 (12.5) | 0(0) | 24 (100) | |||
Column percentages.
Row percentages.
Non-HIV/AIDS-related.
HIV/AIDS-related.
Injuries and unnatural COD.
4. Discussion
4.1. Burden of disease and COD
In this study, the COD statements were categorized into ICOD, UCOD, and OSC, and comprised 4 major groups of diseases according to the 2010 GBD.10 We found that more than a third of UCODs in both mortuaries were non-communicable diseases (NCDs) followed by injuries and unnatural causes, while HIV/AIDS was responsible for just over 10% of deaths. The Institute for Health Metrics and Evaluation-led GBD 2013 estimated that about 1 in 3 deaths among 15–80 year old in Kenya were due to non-communicable causes.11 This is similar to what we found in this study. In contrast, the GBD 2013 report indicated that HIV accounted for 1 in 4 deaths, while injuries and unnatural causes only accounted for 7% of deaths in Kenya among 15–80 year old. Our study took place in Nairobi, where HIV prevalence is estimated to be slightly below the national average, and antiretroviral treatment coverage is above average,12 which should contribute to lower HIV-associated mortality. In addition to traditional NCD risk factors, like tobacco smoking, high blood pressure, and unhealthy diet, and nontraditional risk factors such as air pollution and excessive alcohol consumption also play a role in an increased number of deaths from NCDs.13 Similarly, the high proportion of deaths from injuries and unnatural causes can be accounted for by the growth of motorization between 1990 and 2013 in Kenya14; the inclusion of City Mortuary, which receives primarily medico-legal cases due to injuries and unnatural causes, may have contributed to the higher rates of external COD seen in our study. A retrospective study done in 2014 on the demographic profile and pattern of fatal injuries in Nairobi revealed that injuries resulted to 10.6% of all deaths recorded at the Department of Civil Registration.15 Other studies on trauma deaths outside the hospitals showed that injury mortality rates have increased in developing countries due to systems that are unreliable for primary prevention purposes,16 unsafe environments and poor access to quality health care.14,17
Under the ICOD statements, group I and II diseases were stated with the most errors, whereas for group III diseases, the COD statements were mostly correct. This may be because communicable (group I) and NCDs (group II) have more complicated disease processes when compared to injuries and unnatural causes (group III), hence more errors in stating the ICOD.
We found that there was a greater number of deaths in males than females, with a majority (over ⅔) aged 25–64 years - the productive age group.
The revised GBD cites higher mortality among men than women and is mainly due to injuries, whereas in women, group I diseases, notably HIV/AIDS, are the major contributors. In a paper on the epidemiologic transition, Joshua A. Salomon et al. noted a strikingly different shift in patterns of COD for men, from group III to group II, compared to a shift towards group II then III in women.18
4.2. Correctness and completeness of COD
In terms of correctness and completeness, City Mortuary had a higher number of correctly-stated CODs than KNH. The ICOD was the most correctly-stated, while OSC was frequently missing. This could be explained by the fact that most of the decedents received at this site were non-hospital deaths, secondary mainly to injuries and unnatural causes. The causes of the injuries were blunt force trauma, road traffic accidents, or firearm injuries. Death from traumatic injuries classically follows a trimodal pattern – immediate, early, and late. Immediate deaths follow unpreventable injuries to the heart, great vessels, spinal cord, and the brain. These are usually the causes of non-hospital deaths received at the mortuary and are, therefore, identifiable by the certifier by following the patterns of physical injuries observed, as demonstrated by Okemwa et al.19 The CODs, however, were most correctly stated at KNH. This is probably due to the availability of clinical information and investigations, as opposed to deaths due to injuries where this information is often lacking. Hospital deaths tend to have multiple complications secondary to surgeries and a myriad of diseases, hence more errors on ICOD. In an academic setting, death certification errors were attributed to house staff inexperience, fatigue, time constraints, and unfamiliarity with the deceased and perceived lack of importance of the DC.20 The same reason could be used to explain the trend seen at KNH since the center is a teaching and referral institution where multiple certifiers are formally trained and practice writing DCs. Weaknesses in the current D1 form may have contributed to errors in COD statements. Although the form is generally structured using the ICD-10 format, it lacks clear user guidance and has not been revised for almost 10 years.
For ICOD, the most common error varied with the site of data collection. At KNH, the listing of the mechanism of death, such as cardiorespiratory arrest as the COD was common. Mechanism of death refers to the physiologic derangement or biological disturbance produced by the cause of death.21 Listing of the mechanism of death without any underlying cause may occur because most physicians tend to confuse cause and mechanism. Medical therapy often attempts to ameliorate these mechanisms, e.g., shock, rather than the cause, e.g., sepsis, thereby focusing attention on mechanism.22 An American Medical Association study supports the above finding stating that the commonest error occurred in listing of the mechanism as the ICOD.23 Mechanistic terminal events are often erroneously reported as COD. In general, these events should never be reported in the DC as one of the CODs. They are extremely non-specific and diminish the quality of mortality statistics. However, data from the City Mortuary had the most common source of error under ICOD being incomplete information. As mentioned earlier, most of the decedents at this site are secondary to pre-hospital deaths. In these cases, not much clinical history is available, leading to incomplete information as a major source of error when filling in the DCs.
For UCOD, the most common type of error was incomplete information. A study by George James et al., in 1955 comparing the inaccuracies between the DC and autopsy certificate revealed that the major source of errors was due to lack of sufficient information to confirm the true COD.24 Incomplete information was a major problem for trauma cases due to lack of information regarding the source of the blunt force. In a study by Gladwell Koku et al., the leading cause of injury under trauma cases was assault by blunt force at 30.5%.17 Since blunt force is a major contributor in trauma-related deaths, more details regarding the source would therefore help in reducing the errors observed.
For the ICOD statements, the differences observed between KNH Mortuary and City Mortuary were statistically significant whereas in UCOD and OSC statements, the differences between the two hospitals had no statistical significance.
The sequence in writing the COD statements was mostly correct at both sites at 93.5%. The ICD-10 outlines a standard format for COD statements.25 This can explain why most of the COD statements have the correct sequence. City Mortuary had a higher number of correct statements when compared to KNH Mortuary at 69.9% and 30.1% respectively. The difference in correctness by site could be because KNH has multiple certifiers tasked with filling in the DC among other duties. City Mortuary on the other hand has pathologists who are trained to fill in the DCs.
The COD statements are complete in under a fifth of the cases in both sites of data collection. Only 10% had correct, complete, and sequenced statements. Jacqueline Messite et al. demonstrated how the accuracy of DC completion varied with the level of physician training and experience.26 Many healthcare workers faced with the task of filling DCs do not receive adequate training in this area, resulting in errors that undermine the quality of data retrieved. However, implementation of a simple educational intervention may go a long way in improving the accuracy of death certification.27 Although the topic of death certification is included in many medical school curricula, it has little practical significance at this early stage of medical education.22 Some practitioners may perceive death certification as unglamorous routine paper work and all this eventually contributes to the errors observed.
One major limitation in this study was that the data retrieval and abstraction were performed independent of the primary authors of the statements, thus clarification on how specific CODs were assigned was also not possible. Although the data abstractors were trained on ICD-10 classification, the research team did not have any means for making corrections in the DC. Although the data retrieval team was also not an expert panel for validation of the COD statements, we feel this review can provide actionable insights into quality of COD statements.
5. Conclusions
City Mortuary had a higher quality of COD statements compared to KNH Mortuary. The DC of unnatural deaths mainly contribute to errors in the UCOD while natural deaths mainly contribute to errors in ICOD. While majority of the DCs had a correct sequence, less than half had the correct statement and less than a fifth had a complete statement. Poor quality of both immediate and underlying CODs could be attributable to lack of periodic refresher training.
Periodic training with feedback mechanisms should be put in place as a requirement for high-quality mortality data. This can be achieved by establishing systems that require training death certifiers on proficiency in DC filling. There is also a need to regularly review and harmonize DC forms and tools to ensure accuracy of data in the country’s death registries.
Acknowledgements
We would like to acknowledge the study investigators and consultants for their participation in the development of the protocol and oversight of the study or development of specimen collection techniques, the study staff, laboratorians, data abstractors, mortuary staff that collected specimens from City Mortuary and KNH Mortuary, those who assisted with KNH medical file reviews, and administrative support.
The Nairobi mortuary HIV surveillance study was conducted by the National AIDS and STI Control Programme (NASCOP), University of Nairobi Institute of Tropical and Infectious Diseases (UNITID), University of California, San Francisco (UCSF), and United States Centers for Disease Control and Prevention (CDC/Kenya, CDC/Atlanta).
Funding
This manuscript has been supported by the President’s Emergency Plan for AIDS Relief (PEPFAR) through the U.S. Centers for Disease Control and Prevention (CDC) under the terms as part of Cooperative Agreement number [U2GPS001814].
List of abbreviations
- COD
Cause of death
- DC
Death certificate
- GBD
Global burden of diseases
- HIV/AIDS
Human immunodeficiency virus/acquired immunodeficiency syndrome
- ICD-10
International classification of diseases and related health problems, version 10
- ICOD
Immediate cause of death
- NASCOP
National AIDS and STI control programme
- NCDs
No communicable diseases
- OSC
Other significant causes of death
- PEPFAR
President’s Emergency Plan for AIDS Relief
- UCOD
Underlying cause of death
Footnotes
Declaration of competing interest
The authors declare that there are no conflicts of interests. The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the funding agencies.
Ethics approval and consent to participate
This public health surveillance activity was approved by the United States Centers for Disease Control and Prevention, Center for Global Health as research that did not involve human subjects (because subjects were deceased) and did not require institutional review board review for human research. The KNH/University of Nairobi Ethical Review Committee also approved this study and did not require consent from next of kin.
Consent for publication
Not applicable.
Availability of data and material
All data generated or analyzed during this study are included in this published article.
References
- 1.Maharjan Leison, Shah A, Shrestha KB, Shrestha G. Errors in cause-of-death statement on death certificates in intensive care unit of Kathmandu, Nepal. BMC Health Serv Res. 2015;15:1–8. 10.1186/s12913-015-1168-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organization. In: International Statistical Classification of Diseases and Related Health Problems 10th Revision. ICD-10 Version:2016; 2016. [Google Scholar]
- 3.The Autopsy Committee and The Forensic Pathology Committee of the College of American Pathologists. Cause of Death Statements and Certification of Natural and Unnatural Deaths: Protocol and Options. 1997.
- 4.Sibai AM. Mortality certification and cause-of-death reporting in developing countries. Bull World Health Organ. 2004;82:83 10.1590/S0042-96862004000200002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hanzlick R. Quality assurance review of death certificates: a pilot study. Am J Forensic Med Pathol. 2005;26:63–65. 10.1097/01.paf.0000154110.84737.e0. [DOI] [PubMed] [Google Scholar]
- 6.Hardisty Sellers A Common errors in certifying the cause of death on the medical certification of death. Can Med Assoc J. 1938:468–473. [PMC free article] [PubMed] [Google Scholar]
- 7.Centers for Disease Control and Prevention. Physician’s Handbook on Medical Certification of Death. 2003.
- 8.World Health Organisation (WHO). The Global Burden of Disease: 2004 Update. 2004. 10.1038/npp.2011.85. [DOI]
- 9.Nyagah LM, Young PW, Kim AA, et al. HIV-related deaths in Nairobi, Kenya: results from a HIV mortuary surveillance study. J Acquir Immune Defic Syndr. 2015;81: 18–23. https://doi.Org/10.1097/QAI.0000000000001975, 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lopez Alan D, Mathers CD, Ezzati M, Jamison DT, Murray CJ. Global Burden of Disease and Risk Factors. 2006. [PubMed] [Google Scholar]
- 11.Vos T, Barber RM, Bell B, et al. Global, regional, and national incidence, prevalence, and years lived with disability for 301 acute and chronic diseases and injuries in 188 countries, 1990-2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2015;386:743–800. 10.1016/S0140-6736(15)60692-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.National AIDS and STI Control Programme (NASCOP). Kenya AIDS Indicator Survey 2012: Final Report. 2014.
- 13.Benziger CP, Roth GA, Moran AE. The global burden of disease study and the preventable burden of NCD. Glob Heart. 2016;11:393–397. 10.1016/j.gheart.2016.10.024. [DOI] [PubMed] [Google Scholar]
- 14.Naghavi M, Wang H, Lozano R, et al. Global, regional, and national age-sex specific all-cause and cause-specific mortality for 240 causes of death, 1990-2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2015;385: 117–171. 10.1016/S0140-6736(14)61682-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gathecha Gladwell Koku, Githinji Wilfred Mwai, Maina Alfred Karagu. Demographic profile and pattern of fatal injuries in Nairobi, Kenya, January to June 2014. BMC Publ Health. 2017;17:1–7. 10.1186/sl2889-016-3958-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Saidi Hassan, Oduor Johannes. Trauma deaths outside the hospital: Uncovering the typology in Kenyan capital. J Forensic Leg Med. 2013;20:570–574. 10.1016/j.jflm.2013.04.016. [DOI] [PubMed] [Google Scholar]
- 17.GBD 2013 Mortality and Causes of Death Collaborators. Global, regional, and national age-sex specific all-cause and cause-specific mortality for 240 causes of death, 1990-2013: A systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2014;385:117–171. 10.1016/S0140-6736(14)61682-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Salomon JA, Murray CJL. The epidemiologic transition revisited: compositional models for causes of death by age and sex. Popul Dev Rev. 2002;28:205–228. 10.1111/j.1728-4457.2002.00205.x. [DOI] [Google Scholar]
- 19.Okemwa MP, Rogena EA, Rana F, Gatei DG. Pattern of road traffic fatalities in Nairobi. Ann Afr Surg. 2010;3:15–20. [Google Scholar]
- 20.Pritt BS, Hardin NJ, Richmond JA, Shapiro SL. Death certification errors at an academic institution. Arch Pathol. 2005;129. [DOI] [PubMed] [Google Scholar]
- 21.Kircher Tobias, Anderson Robert E. Cause of death. Proper completion of the Death Certificate. J Am Med Assoc. 1987;258:349–352. 10.1001/jama.1987.03400030065033. [DOI] [PubMed] [Google Scholar]
- 22.Gupta N, Bharti B, Singhi S, Kumar P, Thakur JS. Errors in Filling WHO Death Certificate in Children: Lessons from 1251 Death Certificates. vol. 60 2014. 10.1093/tropej/fmt059. [DOI] [PubMed] [Google Scholar]
- 23.Sehdev AESS, Hutchins GM. Problems with proper completion and accuracy of the cause-of-death statement. Am Med Assoc. 2001;161:277–284. 10.1001/archinte.161.2.277. [DOI] [PubMed] [Google Scholar]
- 24.James George, Patton Robert E. Accuracy of Cause-Of-Death Statements. 1995. [PMC free article] [PubMed] [Google Scholar]
- 25.World Health Organization (WHO). International Statistical Classification of Diseases and Related Health Problems 10th Revision. 2. World Health Organization; 2010. [Google Scholar]
- 26.Messite J, Stellman SD. Accuracy of death the need for formalized completion: the need for formalized physician training. J Am Med Assoc. 2017;275:794–796. [PubMed] [Google Scholar]
- 27.Myers KA, Farquhar DRE. Improving the accuracy of death certification. Can Med Assoc J. 1998;158:1317–1323. [PMC free article] [PubMed] [Google Scholar]


