Abstract
Frontal lobe epilepsy is a common neurological disorder with a broad spectrum of symptoms. Frontal lobe epilepsy presenting with vertigo is extremely rare, and the relevant pathogenesis remains unclear. Herein, we report a case of frontal lobe epilepsy manifesting as vertigo, and we review the relevant literature. A 34-year-old woman presented with a 10-year history of general tonic–clonic seizures. In the month prior to admission, she experienced nocturnal seizures on two occasions. Video electroencephalogram monitoring showed frequent clinical seizures during which the patient felt transient vertigo. The ictal electroencephalogram revealed a medium-amplitude spike and slow wave complex originating from the frontal lobes. The patient was treated with oral sodium valproate, levetiracetam, and lamotrigine. After a 6-month follow-up period, her seizures were well controlled. Our findings expand the symptom spectrum of epilepsy, suggesting that vertigo can be an uncommon clinical manifestation of frontal lobe epilepsy. Although the pathological correlation between vertigo and epilepsy remains elusive, our findings indicate that vestibular cortical neurons may participate in periodic epileptiform discharges of the frontal lobe. Clinicians should be aware of a potential diagnosis of epilepsy in patients presenting with vertigo as the onset symptom because this condition is usually underdiagnosed.
Keywords: Frontal lobe epilepsy, vertigo, vestibular cortex, case report, electroencephalogram, tonic–clonic seizures
Introduction
Frontal lobe epilepsy is a neurological disorder that is characterized by brief, recurring, partial seizures originating from the frontal lobe. It is the second most common type of epilepsy, following temporal lobe epilepsy.1 The clinical manifestations of frontal lobe epilepsy differ considerably depending on the region of the frontal cortex that is affected. Clinical manifestations include abnormal tonic posture, repetitive vocal outbursts, and dystonic motor movements.2 However, frontal lobe epilepsy manifesting as vertigo is extremely rare.3 Furthermore, the pathogenesis of vertigo in frontal lobe epilepsy remains unclear.
Herein, we report a case of frontal lobe epilepsy manifesting as vertigo, and review the relevant literature. Our findings expand the symptom spectrum of epilepsy and provide suggestive evidence for the pathological correlation between vertigo and epilepsy.
Case report
This case was reported according to the ethical guidelines of the Declaration of Helsinki and was approved by the Human Ethics Committee of Peking Union Medical College Hospital, China. Written informed consent was obtained from the patient for the publication of this report.
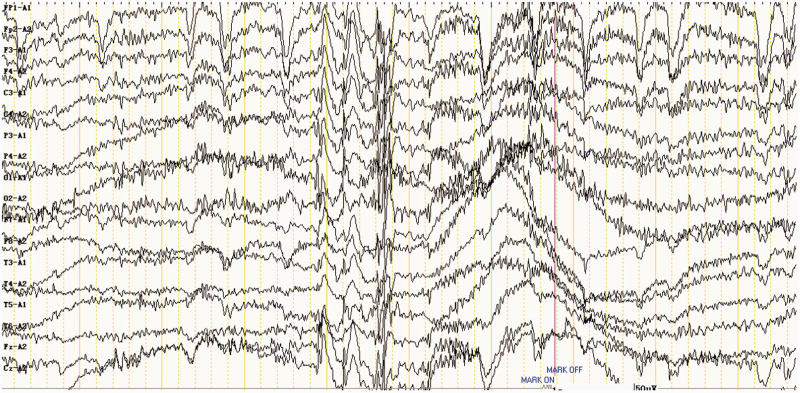
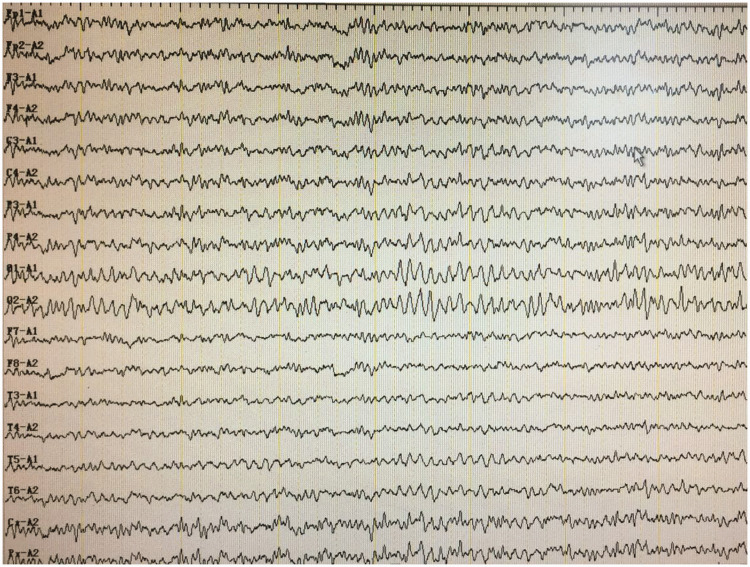
A 34-year-old woman presented with a 10-year history of general tonic–clonic seizures. The seizures lasted for 2 to 3 minutes each, with consciousness disturbance and no significant aura. Interictal electroencephalogram results were normal, and brain magnetic resonance imaging results revealed no abnormalities. The patient’s medical history was unremarkable. The patient was diagnosed with epilepsy, and oral sodium valproate was prescribed. During the administration of sodium valproate, her seizures were partially relieved; only transient unconsciousness and right-arm myoclonic movements persisted, at a frequency of approximately once per week (each attack lasting for several seconds). Seven years before presentation, the patient gradually reduced her dosage of sodium valproate. She stopped taking sodium valproate 4 years before presentation. One month prior to admission, she woke up suddenly during nocturnal sleep with palpitations, limb stiffness, and jerking movements. The attack lasted for approximately 10 minutes, during which she was unconscious. Two weeks before admission, the seizures reoccurred. During hospitalization, video electroencephalogram monitoring revealed frequent clinical seizures during which the patient felt transient vertigo (Supplemental videos 1 and 2). No nystagmus was observed. Ictal electroencephalogram results revealed a medium-amplitude spike- and slow-wave complex (4–5 Hz) originating from the frontal lobes (predominantly on the left side; Figure 1), which supported a diagnosis of frontal lobe epilepsy.4,5 Oral sodium valproate (0.5 g twice per day), levetiracetam (0.5 g twice per day), and lamotrigine (50 mg twice per day) were administered. At a 6-month follow-up, the frequency of seizures was markedly reduced (Figure 2).
Figure 1.
Ictal electroencephalogram of the patient showing a medium-amplitude spike- and slow-wave complex (4–5 Hz) originating from the frontal lobes (predominantly on the left side).
Figure 2.
Follow-up electroencephalogram of the patient showing no abnormalities.
Discussion
Vertigo and epilepsy are both common symptoms that are presented to general practitioners. Differential diagnosis is crucial for clinical treatment and determines patient prognosis. Thus, multidisciplinary collaboration should be encouraged.
Vertigo is a common neurological symptom with a life-time prevalence of 20% to 30% in the general population. However, epilepsy is an uncommon factor in central vertigo, and is difficult to diagnose. Although the concepts of vertigo and epilepsy have been investigated for centuries, the definitive association between these conditions remains unclear. In the nineteenth century, several scholars6 proposed the term ‘vertiginous epilepsy’. However, epilepsy-related vertigo is usually overlooked because of the low incidence of vertigo in epileptic patients. According to recent literature, epilepsy-related vertigo occurs in approximately 8.4% of all epileptic diseases, and the incidence is slightly higher in pediatric patients compared with the rates observed in adults.7 The most common epileptogenic foci are located in the temporal lobe (approximately 80% of all cases), followed by the parietal lobe, the occipital lobe, and the frontal lobe.8 Vertiginous epilepsy is thought to be caused by periodic epileptiform discharges of vestibular cortical neurons.
In recent years, the vestibular cortex has been revealed to have structural and functional connections with the frontal lobe.9 Neurophysiological studies have reported that the vestibular cortex is located in the junctional zone of the temporal, parietal, and occipital lobes, while functional neuroimaging studies have shown that stimulating the vestibular cortex can activate the temporal and parietal lobes as well as partially activating the frontal lobe.10 Although the direct relationship between vertigo and the frontal lobe remains unclear, several studies11 have noted that vertiginous epilepsy is associated with an impairment in the frontal lobe (such as the anterior cingulate gyrus, precentral gyrus, inferior frontal gyrus, and middle frontal gyrus). Moreover, Kahane et al.12 reported that vestibular symptoms (including illusions of rotation and indefinable feelings of body motion) can be electrically induced in the frontal lobe. These findings suggest that the frontal lobe may be involved in vestibular function. Additionally, several studies13 have also proposed that vertigo may be caused by disturbances of ocular movement, as a result of frontal lobe impairment. Relevant animal experiments14 have demonstrated that the anterior cingulate gyrus and Brodmann area 6 represent the frontal vestibular cortex. Multiple patients15 have presented with episodes of epileptic rotational vertigo without nystagmus, in which video electroencephalogram results revealed a frontal onset of epileptic discharges, and magnetic resonance imaging revealed a lesion in the frontal lobe, supporting the aforementioned hypothesis.
Several scholars16 have proposed the concept ‘vestibulogenic seizures.’ This condition is thought to represent an idiopathic subtype of epileptic seizures with a benign clinical course and a potential familial inheritance. However, epilepsy with vestibular symptoms usually manifests as a disturbance of motion and perception, an ocular movement disorder, or a proprioception deficiency; nevertheless, epilepsy presenting with vestibular vertigo alone is extremely rare. Recently, two cases were reported of idiopathic epilepsy with vertigo as the sole onset symptom. The patients in both of these cases had a family history of epilepsy and responded well to anti-epileptic therapy.17
Notably, the patient in the current case presented with general tonic–clonic seizures, which is consistent with previous reports that approximately 23% of all vestibulogenic seizures manifest as general tonic–clonic seizures.18 To our knowledge, this is the first reported case of idiopathic epilepsy with vertigo as the sole onset symptom. After anti-epileptic treatment with combined sodium valproate, levetiracetam, and lamotrigine, the patient’s frontal lobe epilepsy was well controlled. Previous research has reported that lamotrigine has significant efficacy for the control of vestibulogenic seizures, and can help to prevent the recurrence of such seizures.19 However, the current evidence is limited to single case reports and short-term follow-up periods. Thus, the definitive pathogenesis of vestibulogenic seizures, as well as the optimal treatment options, require further research based on large-sample cohorts.
In conclusion, our findings expand the symptom spectrum of epilepsy, suggesting that vertigo can be an uncommon clinical manifestation of frontal lobe epilepsy. Although the pathological correlation between vertigo and epilepsy remains elusive, our findings indicate that vestibular cortical neurons may participate in periodic epileptiform discharges of the frontal lobe. Clinicians should be aware of a potential diagnosis of epilepsy in patients presenting with vertigo as the onset symptom because this condition is usually underdiagnosed.
Declaration of conflicting interest
The authors declare that there is no conflict of interest.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
ORCID iD
Xiangqin Zhou https://orcid.org/0000-0002-6434-4764
Supplemental Material
Supplemental material for this article is available online.
References
- 1.Kim YK, Lee DS, Lee SK, et al. (18)F-FDG PET in localization of frontal lobe epilepsy: comparison of visual and SPM analysis. J Nucl Med 2002; 43: 1167–1174. [PubMed] [Google Scholar]
- 2.Gold JA, Sher Y, Maldonado JR. Frontal lobe epilepsy: a primer for psychiatrists and a systematic review of psychiatric manifestations. Psychosomatics 2016; 57: 445–464. [DOI] [PubMed] [Google Scholar]
- 3.Kim KS, Kim YH, Hwang Y, et al. Epileptic nystagmus and vertigo associated with bilateral temporal and frontal lobe epilepsy. Clin Exp Otorhinolaryngol 2013; 6: 259–262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Britton JW, Frey LC, Hopp JL, et al. Electroencephalography (EEG): An Introductory Text and Atlas of Normal and Abnormal Findings in Adults, Children, and Infant Chicago: American Epilepsy Society, 2016. [PubMed] [Google Scholar]
- 5.Dieterich M, Brandt T. The parietal lobe and the vestibular system. Handb Clin Neurol 2018; 151: 119–140. [DOI] [PubMed] [Google Scholar]
- 6.Alpers BJ. Vertiginous epilepsy. Laryngoscope 1960; 70: 631–637. [DOI] [PubMed] [Google Scholar]
- 7.Bladin PF. History of “epileptic vertigo”: its medical, social, and forensic problems. Epilepsia 1998; 39: 442–447. [DOI] [PubMed] [Google Scholar]
- 8.Barr WB, Karantzoulis S. Temporal lobe epilepsy. In: Kreutzer J, DeLuca J, Caplan B, eds. Encyclopedia of Clinical Neuropsychology. New York: Springer International Publishing, 2017. 2547–2548 [Google Scholar]
- 9.Manzoni D. The cerebellum and sensorimotor coupling: looking at the problem from the perspective of vestibular reflexes. Cerebellum 2007; 6: 24–37. [DOI] [PubMed] [Google Scholar]
- 10.Morano A, Carnì M, Casciato S, et al. Ictal EEG/fMRI study of vertiginous seizures. Epilepsy Behav 2017; 68: 51–56. [DOI] [PubMed] [Google Scholar]
- 11.Ettinger AB. Review: epilepsy and the functional anatomy of the frontal lobe. Q Rev Biol 1996; 71: 149. [Google Scholar]
- 12.Kahane P, Hoffmann D, Minotti L, et al. Reappraisal of the human vestibular cortex by cortical electrical stimulation study. Ann Neurol 2003; 54: 615–624. [DOI] [PubMed] [Google Scholar]
- 13.Anoh-Tanon MJ, Bremond-Gignac D, Wiener-Vacher SR. Vertigo is an underestimated symptom of ocular disorders: dizzy children do not always need MRI. Pediatr Neurol 2000; 23: 49–53. [DOI] [PubMed] [Google Scholar]
- 14.Rios M, Treede RD, Lee JI, et al. Direct evidence of nociceptive input to human anterior cingulate gyrus and parasylvian cortex. Curr Rev Pain 1999; 3: 256–264. [DOI] [PubMed] [Google Scholar]
- 15.Kluge M, Beyenburg S, Fernández G, et al. Epileptic vertigo: evidence for vestibular representation in human frontal cortex. Neurology 2000; 55: 1906–1908. [DOI] [PubMed] [Google Scholar]
- 16.Barac B. Vertiginous epileptic attacks and so-called “vestibulogenic seizures”. Epilepsia 1968; 9: 137–144. [DOI] [PubMed] [Google Scholar]
- 17.Hewett R, Guye M, Gavaret M, et al. Benign temporo-parieto-occipital junction epilepsy with vestibular disturbance: an underrecognized form of epilepsy? Epilepsy Behav 2011; 21: 412–416. [DOI] [PubMed] [Google Scholar]
- 18.Kogeorgos J, Scott DF, Swash M. Epileptic dizziness. Br Med J (Clin Res Ed) 1981; 282: 687–689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cha YH. Migraine-associated vertigo: diagnosis and treatment. Semin Neurol 2010; 30: 167–174. [DOI] [PMC free article] [PubMed] [Google Scholar]