Highlights
-
•
In the hepatobiliary system anatomical variations can happen.
-
•
Though type II choledochal cyst has great outcome after surgery, it has differentials to think about before exploration.
-
•
The anatomic variation in choledochal cyst will cause diagnostic and management challenges.
Abbreviations: CC, choledochal cyst; GB, gall bladder; CHD, common hepatic duct; CBD, common bile duct
Keywords: Children, Choledochal cyst, Gall bladder duplication, Anatomical variant, Biliary tree
Abstract
Introduction
Choledochal cyst (CC) is an uncommon congenital disease of the biliary tract. There are five main types of CC with several recognized sub-types. However, occasional variants with a difficulty in diagnosis and management do occur.
Presentation of the case
We report a case of a nine years old female child diagnosed with CC who presented with right quadrant abdominal pain with unremarkable physical findings. Investigation using abdominal CT scan suggested type II choledochal cyst. The intraoperative finding revealed an unusual site of the cyst that is at the confluence of common hepatic duct (CHD) posteriorly. The cyst was successfully excised and the child is doing well on her follow ups.
Discussion
In the management of choledochal cyst the anatomy should be clearly defined with detailed investigations like Abdominal CT Scan or cholangiography before surgical excision as abnormal variants which usually do not fit into the known classification types and subtypes. This might confuse with other differentials like gall bladder duplication. Surgical excision is the gold standard management option.
Conclusion
This case report will alert surgeons that there are different anatomic variant of choledochal cysts out of the known classifications and with meticulous dissection will help proper excision and avoid unnecessary complications.
1. Introduction
Choledochal cysts (CC) are a rare congenital abnormality of the biliary system that consist of cystic dilatations of the extrahepatic biliary tree, intrahepatic biliary ducts or both and the incidence in western countries has been reported to be 1:100,000 to 1:150,000 while it is very common in Japan with an estimated incidence of 1:1000–13,000 [[1], [2], [3], [4], [5]]. By Todani et al. CC are commonly classified into five main types with several sub types while some anatomical configurations which do not readily fall into the Todani modification have also been described in literatures [[2], [3], [4], [5]].
Here we report a case in a 9 years old female child who was diagnosed with CC, which does not fall into the common classification system and has a diagnostic and management difficulty. She was managed at Menellik II hospital which is an affiliate tertiary hospital of Addis Ababa University, College of health science. This work has been reported according to the SCARE 2018 criteria and SCARE checklist is also attached as a separate document [6].
2. Presentation of the case
A nine years old female child who was otherwise healthy presented with right upper quadrant abdominal pain of two years duration. The pain is colicky and intermittent which usually occurs postprandial and worse after ingestion of fatty meals. It is sometimes accompanied by upper abdominal bloating, discomfort and infrequent vomiting of ingested matter. Otherwise, she has good appetite; no weight loss; no color change in the eyes, skin, urine or stool; no skin itching; no previous attack of cholecystitis. She has no known family history of biliary diseases; no other known chronic medical or psychiatric illness and known congenital anomaly. For the above complaint she visited different clinics and managed only with analgesics and antacids but no significant improvement.
The physical examination was unremarkable. She is a well looking girl with normal BMI and vital signs are in the normal range; no icterus of the sclera; flat & soft abdomen with no mass or tenderness and no scratch marks on the skin.
Basic investigations showed normal hemogram, organ function test and coagulation profile.
Abdominal ultrasound showed focal biliary duct dilatation at the hepatic hilum measuring 1.9 × 1.5 cm with internal low level echo fluid levels and moderately distended gall bladder free of stones with the conclusion being CC as the most probable diagnosis and recommending Abdominal CT Scan.
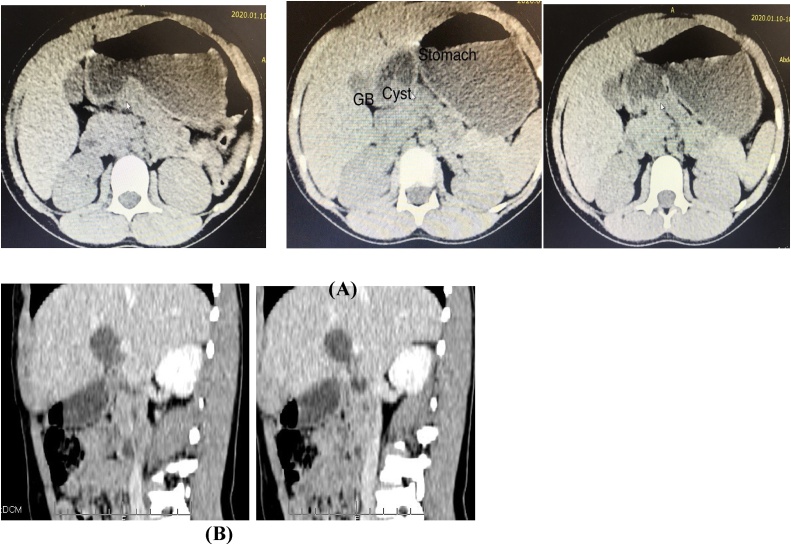
Abdominopelvic CT scan showed well defined round hypodense mass at the porta hepatis measuring 3 × 2.7 cm with smooth and thin wall which appears to communicate with the biliary tree. The common bile duct was to have normal caliber. There is no evidence of biliary tree obstruction and the conclusion was cystic mass at the porta hepatis likely to be type II CC (Fig. 1).
Fig. 1.
Abdominopelvic CT scan of the patient before surgery demonstrating a well defined round hypodense mass at the porta hepatis adjacent to the gall bladder.
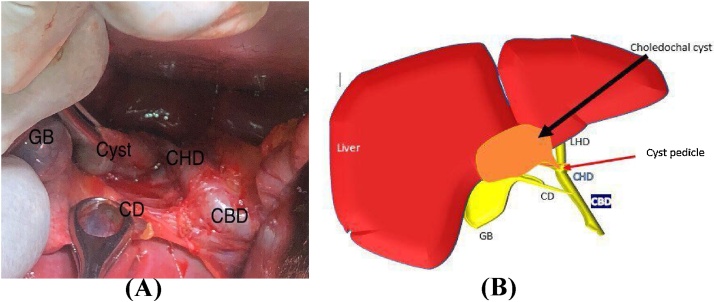
She was then explored on elective base after waiting for bed for two months. At laparotomy, the whole length of the common bile duct (CBD), whole extrahepatic bliary tree and also the gall bladder (GB) anatomy evaluated thoroughly. A 5 × 3 × 2 cm sized cyst with a narrow (0.2 cm diameter and 0.5 cm length) pedicle arising from the confluence of the right and left hepatic duct just posteriorly at the level of the porta hepatis with normal hepatic and common bile duct was found (Fig. 2) which did not fit with any of the current recognized CC classification types. Intraoperaatively on table cholangiography was not done since it was not available in our operative theatre. There is no separate vascular supply to this cyst and it is not sharing with the normally found gall bladder vascularity. With through mobilization the cyst was completely excised and the pedicle ligated and closed with absorbable suture.
Fig. 2.
Intraoperative finding of the unusual choledochal cyst variant which is a 5 × 3 × 2 cm sized cyst with a narrow (0.2 cm diameter and 0.5 cm length) pedicle arising from the confluence of the right and left hepatic duct just posteriorly at the level of the porta hepatis (A) Image taken intraoperatively and (B) schematic description of intraoperative finding.
There was only mild adhesion to the liver capsule and the gallbladder but there was no any intraoperative complication and the tissue was sent for histopathology examination. The the gall bladder was mobilized well after properly ligating the cystic artery and cystic duct and finally cholecystectomy done.
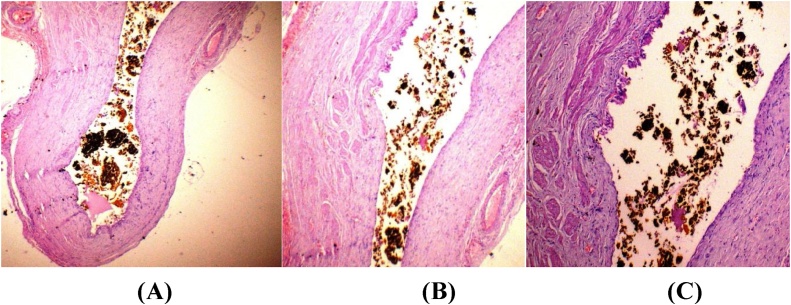
The patient had stayed in recovery room for two hours and transferred to the ward and was put on IV analgesics and also continued with prophylactic antibiotics for 24 h. She had a good post-operative recovery and was discharged in the second postoperative day. She was also seen in the follow-up clinic on the second week of surgery, after two months and after six months where she has no complaint with a normal liver and biliary function tests and normal liver and biliary tree architecture on ultrasound scan. Postoperative macroscopic examination revealed unilocular cystic structure filled with bile. Microscopic sections showed cyst wall focally lined by bland columnar cells with subepithelial fibrotic wall, scanty inflammatory and disorganized smooth muscle but not well formed muscular layer (Fig. 3). The lumen was filled with bile and no metaplasia or dysplasia seen.
Fig. 3.
Microscopic examination shows cyst wall focally lined by bland single layer of columnar cells with sub epithelial fibrotic wall, scanty inflammatory and disorganized smooth muscle but not well formed muscular layer. (Hematoxylin and eosin stain, (A) low power magnification, 40X, (B and C, high power magnification, 100X and 400X respectively).
3. Discussion
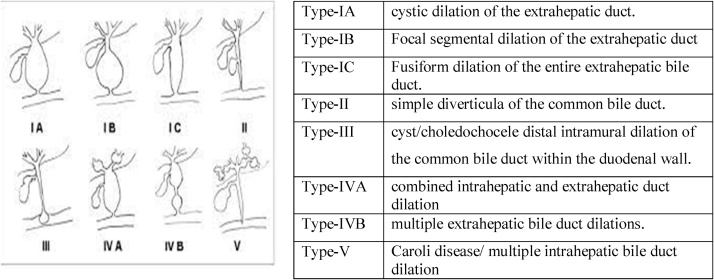
The classification of choledochal cyst was tired to be refined and updated by different scholars in the past decades and published at different literatures and textbooks so that an acceptable classification modalities are in use [[1], [2], [3], [4], [5],7]. From the widely and currently used Todani classification which is described at Fig. 4 type II choledochal cyst which is a true diverticulum from the CBD accounts for around 2% of all the CC classification [4,5,7].
Fig. 4.
Modified Todani et al. classification of choledochal cyst.
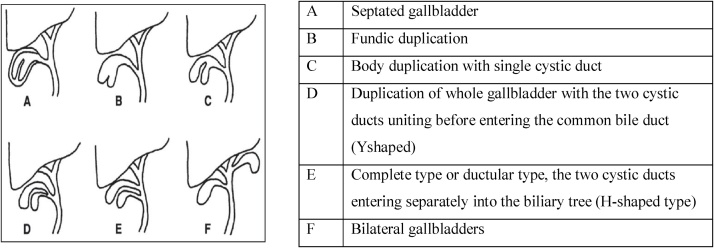
Type II CC can also be a differential for gall bladder duplication which is a rare variant of GB anatomical anomalies with a frequency of 1:3000–4000 [[8], [9], [10]]. As described in Fig. 5 GB duplication can have a common cystic duct and arterial supply if it is the splitted group or it can originate separately from the CHD, CBD or one of the hepatic duct with its own vascular supply arising from the hepatic artery or the cystic artery [8,9]. On pathologic examination duplication of a GB has a muscular wall with an epithelial linings while CCs have a firm, fibrotic wall and contain variable quantities of bile. The cysts are lined by biliary-type epithelium, although the surface may be denuded in older patients. The wall contains disorganized smooth muscle bundles with fibrous tissue and dystrophic calcifications in some cases [10,11].
Fig. 5.
Boyden classification of congenital duplication of the gallbladder.
In our case the pedicle of the cyst attaches to the posterior wall of common hepatic duct with 0.2 cm diameter and 0.5 cm length. In addition to not having a proper muscular wall and deficient epithelial lining it also has no its own vascular supply which makes it against GB duplication [8,10].
The peculiar pathologic description of this patient goes for CC [2]. Unlike the normally described type II CC which arises from CBD as a diverticulum, our patients cyst aroused from the posterior wall of CHD with a short and narrow pedicle [[1], [2], [3], [4], [5],7].
Abdominal ultrasound (US) scan is the first line of investigation with a good sensitivity while Computed tomography (CT) scan is the most accurate one and helpful in properly assessing cyst, its wall and intrahepatic involvement with a great help in planning surgery. Though there was no image sent with the ultrasound description, there was size difference with the CT Scan and it might be due to expert and machine dependence of the ultrasound. There was size discrepancy between the CT Scan of the patient and intraoperative finding which might be due to a two months waiting between the investigation and intervention that results in the growth of the cyst due to secretion and inflammation. Though not done in this patient because of cost, the different types of cholangiographies like MRCP, ERCP are the most sensitive and gold standard ones [7].
Differential diagnosis must be considered before surgery including gallbladder duplication, gallbladder diverticula, gallbladder fold, Phrygian cap, pericholecystic fluid, focal adenomyomatosis, and intraperitoneal fibrous bands and should be checked on the preoperative investigations and also during exploration [12]. And the best option of management of type II choledochal cyst is complete excision [4,8].
4. Conclusion
Surgeons should be aware of the possibility of anatomical variant in choledochal cysts, which is out of the normal classification and be ready for the management challenge that can be addressed with meticulous dissection and proper excision and this will help to avoid unnecessary complications. This case report will alert surgeons that there are different anatomic variant of choledochal cysts out of the known classifications.
Conflicts of interest
We declare that there is no conflict of interests.
Funding
This study did not receive any funding.
Ethical approval
Exemption from ethical approval was obtained from the department of surgery ethics and research committee at Addis Ababa University college of health sciences.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Author contribution
Workye Tigabe and Hadush Tesfay collected the data and drafted the manuscript and they were the assisting surgeon. Tihitena Negussie was the lead surgeon of the case, involved in the conception of the case report, supervised other authors. Kassahun Raya and Dagnachew Tamrat did the pathologic assessment of the case and feedback on the manuscript about the pathology part. All authors involved on the management of this case, read, edited and approved the final manuscript.
Registration of research studies
Registry not required as this is not a first-in-man case report.
Guarantor
Tihitena Negussie (TN)
Pediatrics surgery Unit, Department of Surgery
Addis Ababa University, College of Health Sciences.
Provenance and peer review
Not commissioned, externally peer-reviewed.
Acknowledgments
We would like to express our gratitude to Dr. Tesfaye Kebede for radiologic description and Dr. Saleamlak Tigabie for the intraoperative image taking and schematic description.
Contributor Information
Workye Tigabie, Email: workye62@gmail.com.
Hadush Tesfay, Email: hadusheyma@gmail.com.
Dagnachew Tamrat, Email: dagnachewtamrat@gmail.com.
Kassahun Raya, Email: kassahunraya@gmail.com.
Tihitena Negussie, Email: tihutin@yahoo.com.
References
- 1.Sadiq J., Nandi B., Lakhoo K. An unusual variant of choledochal cyst: a case report. J. Med. Case Rep. 2009;3(December (1)):54. doi: 10.1186/1752-1947-3-54. [Google Scholar] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Soares K.C., Arnaoutakis D.J., Kamel I., Rastegar N., Anders R., Maithel S. Choledochal cysts: presentation, clinical differentiation, and management. J. Am. Coll. Surg. 2014;219(December (6)):1167–1180. doi: 10.1016/j.jamcollsurg.2014.04.023. [Google Scholar] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Baison G.N., Bonds M.M., Helton W.S., Kozarek R.A. Choledochal cysts: similarities and differences between Asian and Western countries. WJG. 2019;25(July (26)):3334–3343. doi: 10.3748/wjg.v25.i26.3334. [Google Scholar] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Giriyappa V., Bhavsar M., Vora H. Choledochal cysts: a review of literature. Saudi J. Gastroenterol. 2012;18(July-August (4)):230. doi: 10.4103/1319-3767.98425. [PubMed] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Singham J., Yoshida E.M., Scudamore C.H. Choledochal cysts: part 1 of 3: classification and pathogenesis. Can. J. Surg. 2009;52(October (5)):434–440. [PubMed] [PMC free article] [PubMed] [Google Scholar]
- 6.Agha R.A., Borrelli M.R., Farwana R., Koshy K., Fowler A., Orgill D.P., For the SCARE Group The SCARE 2018 statement: updating consensus surgical CAse REport (SCARE) guidelines. Int. J. Surg. 2018;60:132–136. doi: 10.1016/j.ijsu.2018.10.028. [Google Scholar] [DOI] [PubMed] [Google Scholar]
- 7.Ziegler Moritz M., Azizkhan Richard G., Allmen Daniel V., Weber Thomas R. 2nd ed. McGraw-Hill Education; 2014. Operative Pediatric Surgery; pp. 716–723. [Google Scholar] [Google Scholar]
- 8.Reddy O., Gafoor J., Suresh B., Prasad P. Duplication of gallbladder: a rare congenital malformation. J. Dr. NTR Univ. Health Sci. 2015;(September (4)):269–271. [Google Scholar] [Google Scholar]
- 9.Chintakayala B. Duplication of gallbladder. Open Access J. Surg. 2018;(October (5)):555773. [Google Scholar] [Google Scholar]
- 10.Al Rawahi A., Al Azrii Y., Al Jabril S., Alfadlil A., Al Aghbaril S. Duplicate gallbladder overview and management challenges. Clin. Surg. 2016;1(May):1016. [Google Scholar] [Google Scholar]
- 11.Yantiss R.K., editor. Frozen Section Library: Liver, Extrahepatic Biliary Tree and Gallbladder. first edition. Springer-Verlag New York; New York, USA: 2011. pp. 21–44. [Google Scholar] [Google Scholar]
- 12.Desolneux G., Mucci S., Lebigot J., Arnaud J.P., Hamy A. Duplication of the gallbladder. A case report. Gastroenterol. Res. Pract. 2009;(November):1–3. doi: 10.1155/2009/483473. [Google Scholar] [DOI] [PMC free article] [PubMed] [Google Scholar]