Abstract
Background: Gastroesophageal reflux disease (GERD) is a common gastrointestinal disorder that results from regurgitation of acid from the stomach into the esophagus. Treatment available for GERD includes lifestyle changes, antacids, histamine-2 receptor antagonists (H2RAs), proton pump inhibitors (PPIs), and anti-reflux surgery. Aim: The aim of this review is to assess the cost-effectiveness of the use of PPIs in the long-term management of patients with GERD. Method: We searched in PubMed to identify related original articles with close consideration based on inclusion and exclusion criteria to choose the best studies for this narrative review. The first section compares the cost-effectiveness of PPIs with H2RAs in long-term heartburn management. The other sections shall only discuss the cost-effectiveness of PPIs in 5 different strategies, namely, continuous (step-up, step-down, and maintenance), on-demand, and intermittent therapies. Results: Of 55 articles published, 10 studies published from 2000 to 2015 were included. Overall, PPIs are more effective in relieving heartburn in comparison with ranitidine. The use of PPIs in managing heartburn in long-term consumption of nonsteroidal anti-inflammatory drug (NSAID) has higher cost compared with H2RA. However, if the decision-maker is willing to pay more than US$174 788.60 per extra quality-adjusted life year (QALY), then the optimal strategy is traditional NSAID (tNSAID) and PPIs. The probability of being cost-effective was also highest for NSAID and PPI co-therapy users. On-demand PPI treatment strategy showed dominant with an incremental cost-effectiveness ratio of US$2197 per QALY gained and was most effective and cost saving compared with all the other treatments. The average cost-effectiveness ratio was lower for rabeprazole therapy than for ranitidine therapy. Conclusion: Our review revealed that long-term treatment with PPIs is effective but costly. To achieve long-term cost-effective approach, we recommend on-demand approach to treat heartburn symptoms, but if the symptoms persist, treatment with continuous step-down therapy should be applied.
Keywords: proton pump inhibitors, cost-effectiveness, economic evaluation, heartburn, gastroesophageal reflux disease, long-term management
Introduction
Gastroesophageal reflux disease (GERD) is a common gastrointestinal disorder that results from regurgitation of acid from the stomach into the esophagus. The prevalence of GERD ranged from 23% in South America, 18.1% to 27.8% in North America, 11.6% in Australia, 8.8% to 25.9% in Europe, 8.7% to 33.1% in Middle East, and 7.8% in East Asia.1 Heartburn and regurgitation are cardinal symptoms for GERD, and other symptoms include water brash, dysphagia, epigastric pain, belching, nausea, chest pain or discomfort, and bloating.2,3 However, patient may experience extra-esophageal symptoms such as cough, throat clearing, throat pain or burning, hoarseness, wheezing, and sleeping disturbances. Several medical therapies include antacids, histamine-2 receptor antagonists (H2RAs), PPIs, Gaviscon, transient lower esophageal sphincter relaxation (TLESR) reducers, Carafate, and prokinetics. However, due to profound and consistent acid suppression of PPIs, they remained as the most effective therapy for GERD. Currently, omeprazole, esomeprazole, lansoprazole, rabeprazole, pantoprazole, dexlansoprazole, omeprazole with sodium bicarbonate are available as over-the-counter (OTC) and prescribed medications. In particular, compared with other medications, PPIs significantly improved controlling symptoms of various phenotypic presentations of GERD.4,5 The treatment for GERD requires long-term management for their conditions.
Health economics plays an important role to understand the benefits of treatment and is an interface between economics and medicine. Although multiple factors are taken into account when deciding a medicine for treatment, economic evaluation can invoke the cost of treatment and thereby understand the patient outcomes for every dollar spent. In light of the enormous burden of GERD, PPIs account for more than 50% of prescriptions, resulting in around US$10 billion in annual direct health care costs in United States.6 Reviewing these economic evaluation of PPIs in GERD from different countries can provide a greater understanding of therapeutic management strategies and can also help to estimate the economic outcomes of the PPIs in GERD. We aimed to review the potential cost saving that could obtained for the long-term management of GERD, focusing on clinical outcomes of PPIs.
Methods
This is a narrative review of pharmacoeconomic evaluation of cost-effective analysis studies on the use of PPIs in long-term management of GERD. We searched quality literatures indexed in PubMed published in English language from January 2000 to December 2015. The MESH search string used was as follows: “cost-benefit analysis” OR “cost effectiveness analysis” OR “economic evaluation” “Quality-Adjusted Life Years” OR “Incremental Cost-Effective Ratio” OR “benefits and costs” AND “heartburn” OR “gastroesophageal reflux” OR “GERD” OR “gastric acid reflux” “esophagitis” AND “proton pump inhibitors” OR “dexlansoprazole” OR “esomeprazole” OR “lansoprazole” OR “omeprazole” OR “pantoprazole” OR “rabeprazole.”
Inclusion/Exclusion Criteria
Titles of the search results were screened, and abstracts were identified and reviewed for removal of duplicate and irrelevant literatures. We used predetermined inclusion and exclusion criteria as shown in Table 1.
Table 1.
Inclusion and Exclusion Criteria.
| Inclusion criteria | Exclusion criteria |
|---|---|
| Articles published from the year 2000 onward | The articles only include nonpharmacological intervention(s) |
| Duration of studies should be more than 4 weeks | Pediatric subjects |
| The subjects have to be above 18 years old | |
| The interventions should be proton pump inhibitors and/or histamine-2 receptor antagonist |
The results of our review were categorized into subsection focusing on the following:
Comparing the cost-effectiveness of PPIs with that of H2RA in the long-term heartburn management regardless of the etiology which could be NSAID-induced ulcer, erosive esophagitis, or others.
Cost-effectiveness of PPIs in 5 different strategies: continuous (step-up, step-down, and maintenance), on-demand, and intermittent therapies.
The outcomes were measured as quality-adjusted life year (QALY), an increase in 1 QALY indicates an increase in 1 year of perfect health due to PPIs.
Results
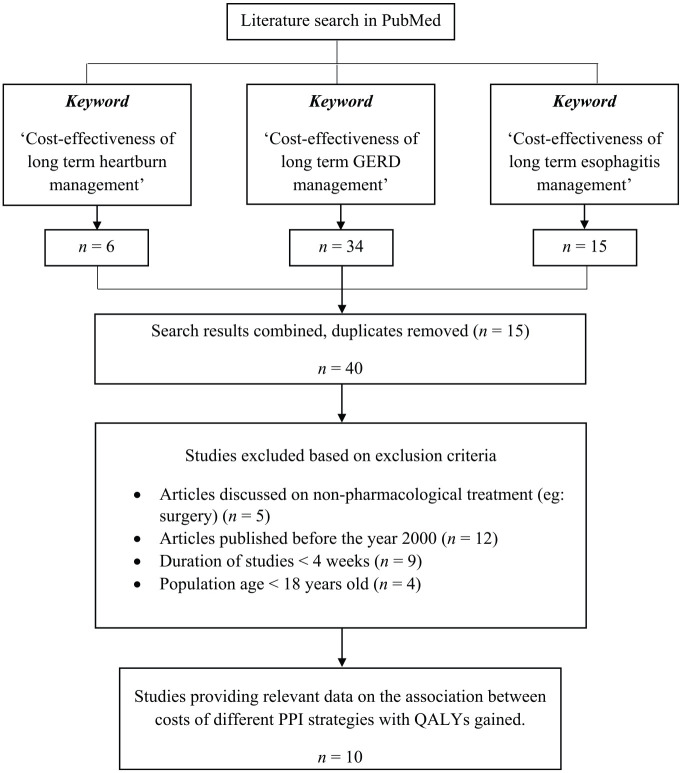
The initial search identified 55 articles from PubMed using different keywords, and the flow of information was shown in Figure 1. After exclusion criteria were applied and the results were combined, the abstracts and manuscripts of 55 articles were reviewed for initial inclusion, were combined, and finally 10 articles were reviewed in the final review.7-16 Of the 10 included studies published between 2000 and 2015, 4 studies were from the United States,7-9,16 2 from the United Kingdom,10,12 and one each from Canada,11 Switzerland,13 Ireland,14 and the Netherlands.15 Cost-effective analysis was performed using Markov model,8,10 decision analysis,7,9,11 cost-utility15 and one study used incremental cost-effectiveness ratio (ICER).12 Two were randomized controlled trials (RCTs)13,16 and one is retrospective-population cohort study.14
Figure 1.
Flow chart of information.
Note. GERD = gastroesophageal reflux disease; PPI = proton pump inhibitor; QALYs = quality-adjusted life in years.
Cost-effective characteristics were assessed by the following studies: 2 studies compared the cost-effectiveness of treatment by PPI with that by H2RA,12,15 1 study assessed the cost-effectiveness of intermittent PPI treatment,11 4 studies maintenance treatment,7,8,11,13 2 studies step-up treatment,9,16 1 study step-down treatment,14 and 3 studies on-demand PPI treatment.7,10,13 The economic outcomes for each of these variables were summarized in Table 2 to Table 7.
Table 2.
Cost-effectiveness of Treatment by PPI Compared With H2RA.
| Author | Year | Methodology | Outcome | Conclusion | Limitation |
|---|---|---|---|---|---|
| Elliott et al12 (UK) | 2006 | • Systematic reviews of outcomes and UK cost data were combined in an incremental economic analysis.
• Incremental cost-effectiveness ratios were generated for QALYs gained. • The meta-analysis included patients with chronic arthritis (primarily rheumatoid arthritis and osteoarthritis) who require • regular NSAIDs for more than 3 weeks. |
• Mean expected cost for tNSAID and PPI is £200 for 0.4988 QALY gained, whereas mean expected costs for tNSAID and H2RA is £120 per 0.4982 QALY gained.
• The incremental increase in QALYs gained by using tNSAID and PPI costs more than cost per QALYs gained by using tNSAID and H2RA. • If the decision-makers pay up to 140 000 pounds per extra QALY, the optimal strategy is tNSAID/H2RA. • If the decision-makers pay over 140 000, the optimal strategy is tNSAID/PPI. |
• The tNSAID and PPI is safer strategy compared with tNSAID and H2RA.
• The tNSAID and PPI is more costly strategy compared with tNSAID and H2RA. |
• To combine data from different sources, the authors assumed that the source populations are comparable (which is a limitation of all models).
• Direct health care costs were available only as reported estimation from clinicians. • There is very little information on the relative effectiveness of the 5 strategies due to the lack of head-to-head studies. |
| de Groot et al15 (the Netherlands) | 2013 | • A cost-utility analysis to compare 8 gastroprotective strategies managing a hypothetical cohort of 60-year old patients with rheumatoid arthritis or osteoarthritis and requiring chronic NSAID therapy:
- NSAID mono-therapy - NSAID + PPI - NSAID/PPI single-tablet - NSAID + H2RA - NSAID/H2RA - NSAID + misoprostol - NSAID/misoprostol single-tablet formulation - Coxib monotherapy • Markov model developed by using decision-analysis software (Tree Age Pro 2009, Tree Age Software, Inc, Williams town, Massachusetts). • Through a series of 3-month Markov transition cycles, the cohort over a 5-year time horizon was followed. • QALYs were used as effectiveness outcome. • Overall outcome was the incremental cost-effectiveness ratio evaluating differences in both costs and QALYs. • A cost-effectiveness threshold of €20 000 per QALY gained was determined following Dutch national guidelines. We discounted all utilities at an annual rate of 3%, as recommended by the US Panel on Cost-Effectiveness in Health and Medicine |
• For average-risk patients, NSAID + PPI co-therapy was the most cost-effective.
• By using Monte Carlo analysis, the strategies were compared across cohorts of 10 000 patients, considering different probabilities and risks. • For a WTP threshold of €20 000 per QALY gained, the probability of being cost-effective was the highest for NSAID and PPI co-therapy users with 57%, followed by NSAID and H2RA with 17%. • If the WTP threshold was below €13 000, the probability of being cost-effective was also the highest for NSAID and PPI co-therapy. |
• NSAID + PPI co-therapy is the most cost-effective strategy in all patients with chronic arthritis irrespective of their risk for gastrointestinal complication. | • Probability estimates used in the model are from heterogeneous studies.
• Different patient groups, follow-up periods, and quality of data make it difficult to precisely estimate the mean probability. |
Note. PPI = proton pump inhibitor; H2RA = histamine-2 receptor antagonist; QALYs = quality-adjusted life years; NSAID = nonsteroidal anti-inflammatory drug; tNSAID = traditional nonsteroidal anti-inflammatory drug; WTP = willingness to pay.
Table 7.
Cost-effectiveness of On-demand PPI Treatment.
| Author | Year | Methodology | Outcome | Conclusion | Limitation |
|---|---|---|---|---|---|
| Wahlqvist et al10 (UK) | 2002 | • Patient and model: Markov model evaluates the cost-effectiveness of on-demand treatment with esomeprazole (20 mg) compared with the 2 omeprazole treatment strategies (intermittent and conventional care). The time frame of the analysis was 6 months and the model was made with a cycle length of 2 weeks. The timing of relapses, drug prescriptions, visits, and endoscopies were taken into account for each Markov cycle.
• Patient management assumptions: Patient management assumptions used in the analysis were based mainly on a UK physician survey (involving 10 gastroenterologists and 15 general physicians) of patient management in clinical practice. • Effectiveness: The number of expected relapses per patient was used as the effectiveness measure in the cost-effectiveness analysis. • Unit costs and sensitivity analysis: Drug costs were calculated with regard to consumed medication during the study period. • The number of expected relapses per patient was used as the effectiveness measure in the cost-effectiveness analysis. Two clinical trials investigating the efficacy and safety of on-demand treatment with esomeprazole 20 mg for symptom control in patients with GERD without esophagitis. • Both studies were multicentered, randomized, double-blind, parallel group, 6-month comparative studies of esomeprazole 20 mg with placebo. Patients were instructed to take the study tablets when required to control symptoms. Patients in these 2 studies were also provided with antacids as rescue medication. The primary efficacy variable was “discontinuation due to unwillingness to continue” (due to insufficient control of heartburn, adverse events, or other reasons). In the first study, patients were randomized in equal proportions to on-demand treatment with esomeprazole 20 mg (n = 170) or placebo (n = 172). • In the second study, patients were randomized in proportions 2:1 to on-demand treatment with esomeprazole 40 mg (n = 293), esomeprazole 2 0 mg (n = 282), or placebo (n = 146). • Otherwise, both studies had essentially identical study protocols and were carried out at about the same point in time, with both doses of esomeprazole giving similar results. • To assess the proportion of patients relapsing during on-demand treatment with esomeprazole 20 mg, results were pooled as if the 2 studies were one large study in the current analysis. • The frequency of tablet intake was estimated in the clinical studies using Medical Event Monitoring System devices (Aardex Ltd, Switzerland) fitted to the drug containers, which recorded each time the container was opened. A pooled analysis on the average number of esomeprazole 20 mg tablets taken per patient each day was also carried out to estimate drug consumption during on-demand treatment. |
• Cost-effectiveness analysis: The results indicate that the on-demand esomeprazole strategy is the most effective while being cost saving compared with either of the omeprazole strategies.
• The results of the cost-effectiveness analysis in terms of expected direct medical costs per patient and expected number of relapses per patient. • The expected number of relapses per patient during on-demand therapy with esomeprazole 20 mg was 0.10. Using the “lower limit” for a probability of relapse during no drug treatment (47%, ie, placebo results from the clinical studies) resulted in 0.57 expected relapses per patient in the intermittent omeprazole strategy and 0.47 relapses in the conventional care omeprazole strategy. • Furthermore, the esomeprazole strategy incurred 16% lower direct medical costs than the intermittent omeprazole strategy and 34% lower costs compared with the conventional care omeprazole strategy. • The corresponding figures when using a 75% “upper limit” probability of relapse during no drug treatment were 1.12 relapses per patient in the intermittent omeprazole strategy and 0.75 in the conventional care omeprazole strategy. When considering the upper limit, the cost reduction by using the on-demand esomeprazole strategy increased to 57% compared with the intermittent omeprazole strategy and 61% compared with the conventional care omeprazole strategy. Thus, the results indicate that the on-demand esomeprazole strategy is the most effective while being cost saving compared with either of the omeprazole strategies. • Sensitivity analysis: The results indicate a cost saving of 26% to 55% still being made with the on-demand esomeprazole strategy (where direct medical costs were US$79.67), compared with a “low-dose” conventional care strategy. |
• The data clearly demonstrate that on-demand esomeprazole 20 mg therapy is associated with significantly better effectiveness and lower costs than a strategy consisting of intermittent 4-week treatment courses of omeprazole 20 mg once daily. | • The endpoint used in this primary care study (symptoms of any severity on at least 2 days during the previous week) may not correspond to a definition of relapse in clinical practice. |
| Szucs et al13 (Switzerland) | 2009 | • Open-label, randomized, multicenter study comparing the 2 long-term management options with esomeprazole 20 mg—continuous daily or on-demand treatment during 26 weeks—in endoscopically uninvestigated patients seeking primary care in Switzerland for symptoms suggestive of GERD who demonstrated complete relief of symptoms after an initial treatment of 4 weeks with esomeprazole 40 mg.
• Patients found to meet all the inclusion criteria and none of the exclusion criteria at the end of the initial treatment course were randomized in equal proportions to continuous treatment with esomeprazole 20 mg 4 times a day or on-demand treatment with esomeprazole 20 mg. For the randomization, a centrally compiled, computer-generated list was used, which was based on a block size of 4. Each site received a kit consisting of a list of randomization numbers and sealed randomization envelopes for 4 patients. The investigator was instructed to consecutively allocate the lowest available randomization number, but open the randomization envelopes containing the information on the allocated treatment group only at randomization. It had been planned that each site would recruit 4 patients (or an exact multiple of 4). Each patient in the continuous treatment arm was instructed to take 1 tablet once daily. • In the on-demand arm, the patient was instructed to take one tablet daily if needed for the relief of heartburn and to stop when the heartburn is adequately controlled. The study drugs were packed in bottles, and every patient received in total 2 bottles of 100 tablets esomeprazole 20 mg free of charge. The distribution schedule of the study drugs from general practitioner to patient was at the discretion of the general practitioner, ie, the treating physician decided when to distribute study drugs and whether to distribute them all at once or at several occasions. Compliance was determined by counting the tablets returned by the patient. |
• The patients in the on-demand group experienced slightly more frequently GERD symptoms than those in the continuous group. At the end of the 6-month maintenance phase, 94% of the patients in the on-demand group and were classified as “satisfied” (score = 1-4) with their treatment, whereas 74% of the patients were reported to be “very satisfied” (score = 1-2), Wilcoxon rank sum test (score = 1-7): P < .056.
• The difference of the adjusted mean direct medical costs between the treatment groups was CHF 88.72 (95% CI: CHF 41.34-153.95) in favor of the on-demand treatment strategy (Wilcoxon rank sum test: P < .0001). The mean number of clinic visits to the investigator for any reason required per patient was 0.52 (SD = 0.663) for those in the on-demand group. • Adjusted direct nonmedical costs and the productivity loss were similar in both treatment groups during the 6-month maintenance phase. Hence, health care payers will obtain net savings by implementing the use of on-demand esomeprazole. • These results confirm that the maintenance therapy through 6 months with respect to patients’ satisfaction and symptom control, defined no need for change of therapy, can be performed with a continuous, as well as by an on-demand schedule using esomeprazole 20 mg daily. The treatment with continuous esomeprazole was more efficient than the on-demand therapy with regard to remission of heartburn. • The adjusted direct medical costs of a 6-month on-demand treatment with esomeprazole 20 mg in patients with GERD were significantly lower compared with a continuous treatment with esomeprazole 20 mg once a day. |
• The data clearly demonstrate that on-demand esomeprazole 20 mg therapy is associated with significantly better effectiveness and lower costs than a strategy consisting of intermittent 4-week treatment courses of omeprazole 20 mg once daily. | • The endpoint used in this primary care study (symptoms of any severity on at least 2 days during the previous week) may not correspond to a definition of relapse in clinical practice. |
| Gerson et al7 (USA) | 2000 | • On-demand PPI Arm: Empirical treatment with an 8-week course of PPI therapy administered on demand when GERD symptoms reoccur. Patients in this group require at most three 8-week courses (24 weeks) of medication per year. Patients failing on-demand therapy (recurrence of symptoms earlier than 2 months without medication) receive continuous PPI therapy, and endoscopy is performed only if symptoms recur on daily PPI therapy. | • The researchers had done a decision analysis on on-demand PPI strategy in which the empirical treatment with an 8-week course of PPI therapy administered on demand when GERD symptoms recur. Patients in this group require at most three 8-week courses (24 weeks) of medication per year. Patients failing on-demand therapy (recurrence of symptoms earlier than 2 months without medication) receive continuous PPI therapy, and endoscopy is performed only if symptoms recur on daily PPI therapy.
• On-demand PPI strategy is the most cost-effective approach with discounted incremental cost-effectiveness ratio of US$20 934 per QALY gained by patient with mild to severe GERD symptoms and $379 223 per QALY gained for patient with mild GERD symptoms. On-demand PPI was dominant with an incremental cost-effectiveness ratio of $2197/QALY gained. |
• On-demand PPI strategy is the most cost-effective approach | • An analysis of lifetime costs—not known how long patient can expect symptomatic relief.
• Only few of the prior studies used QALYs as a utility measurement, and obtained their estimates through a modified Delphi process. • Prior models did not allow patients to switch from H2RAs to PPIs without endoscopy, often did not include the option of Nissen fundoplication, or sent patients without response to PPI for a Nissen without consideration of promotility therapy. • None of the models included patients with nonerosive disease. |
Note. PPI = proton pump inhibitor; GERD = gastroesophageal reflux disease; CHF = congestive heart failure; CI = confidence interval; QALYs = quality-adjusted life in years; H2RAs = histamine 2 receptor antagonists.
PPIs Versus H2RA
Of the studies comparing PPI therapy with H2RA, One study compared the cost-effectiveness between PPIs and H2RA in long-term management of heartburn side effects due to consumption of NSAID more than 3 months period.12 The result showed that the use of PPI in patient on NSAID-induced ulcer is found to be much safer than H2RA, but the cost is higher. According to this study,12 consumption of traditional NSAID (tNSAID) and H2RA co-therapy is the least costly while tNSAID and PPI is the costliest strategy. Mean expected cost for tNSAID and PPI is US$249.71 for 0.4988 QALY gain, whereas mean expected cost for tNSAID and H2RA is US$149.82 per 0.4982 QALY gain. The incremental increase in QALYs gained by using tNSAID and PPI costs more than cost per QALY gained using tNSAID and H2RA. After conducting ICER, it is concluded that if the decision-maker is willing to pay up to US$174 788.60 per extra QALY, the optimal strategy is tNSAID and H2RA. On the other hand, if the decision-maker is willing to pay more than US$174 788.60 per extra QALY, then the optimal strategy is tNSAID and PPI (Table 2).
Another similar study by de Groot et al15 showed that NSAID and PPI co-therapy was the most cost-effective treatment for patients. Besides, NSAID and PPI co-therapy is the most cost-effective strategy in all patients with chronic arthritis irrespective of their risk for gastrointestinal complications. By using Monte Carlo analysis, the strategies were compared across cohorts of 10 000 patients, considering different probabilities and risks. For a willingness-to-pay (WTP) threshold of US$21 288.60 per QALY gained, the probability of being cost-effective was the highest for NSAID and PPI co-therapy users with 57%, followed by NSAID and H2RA with 17%. If the WTP threshold was below US$13 838.24, the probability of being cost-effective was also the highest for NSAID and PPI co-therapy.
Intermitted PPI Treatment
According to Goeree et al11 study, the strategy with intermittent PPI was defined as acute treatment with a PPI (eg, omeprazole 20 mg or lansoprazole 30 mg once daily) for 4 weeks and no further treatment with prescription medications until recurrence. A decision-analytic model was used and the calculated incremental cost per QALY was US$9098.80 (Table 3).
Table 3.
Cost-effectiveness of Intermittent PPI Treatment.
| Author | Year | Methodology | Outcome | Conclusion | Limitation |
|---|---|---|---|---|---|
| Goeree et al11 (Canada) | 2002 | • Strategy C: Intermittent PPI. Acute treatment with a PPI (eg, omeprazole 20 mg or lansoprazole 30 mg once daily) for 4 weeks and no further treatment with prescription medications until recurrence. | • Using a decision-analytic model, the calculated incremental cost per QALY in CDN$ is 12 206. | • Incremental cost per QALY CDN$12 206 | • For the symptom relief and symptom recurrence meta-analyses, a majority of studies relied on endoscopy results as a primary entry criterion and outcome measure, whereas symptoms were typically a secondary criterion.
• The authors used moderate-to-severe heartburn as primary measure of GERD symptoms. • 1-year time horizon for the study may be too short to capture long-term complications such as Barrett esophagus or esophageal stricture. • This study used inputs (ie, costs), which are specific to the province of Ontario only. |
Note. PPI = proton pump inhibitor; QALYs = quality-adjusted life in years; GERD = gastroesophageal reflux disease.
Maintenance PPI Treatment
Another strategy done by Goeree et al11 was continuous maintenance PPI with acute treatment with a PPI (eg, omeprazole 20 mg or lansoprazole 30 mg once daily) for 4 weeks followed by continuous maintenance treatment with a PPI of the same dose. The outcome in terms of incremental cost per QALY for same maintenance dose of PPI is US$73 367.40. Furthermore, maintenance PPI therapy has the highest expected cost per patient over 1 year but also has the lowest expected number of recurrences, expected weeks with heartburn symptoms, and highest QALYs.
Kaplan-Machlis et al8 have done a study to evaluate the effectiveness and the costs of continuous maintenance treatment of PPI (omeprazole) for symptomatic GERD in primary care clinics in West Virginia. In the study, 268 patients who aged more than 18 years with GERD were enrolled and randomly given omeprazole sodium 20 mg once daily for up to 6 months. Recruited study patients also did not receive PPI or H2RA treatment in the previous 30 days. Then, the total cost for omeprazole treatment is assessed. This total cost included direct medical costs, direct nonmedical costs, and indirect costs. As a result, it is shown that 5-year direct medical costs per patient when given omeprazole were notably lower in Denmark, Norway, and Sweden (differences were DKK 8703 [US$1475], NOK 32 992 [US$5155], and SEK 13 036 [US$1946], respectively) (Table 4).
Table 4.
Cost-effectiveness of Maintenance PPI Treatment.
| Author | Year | Methodology | Outcome | Conclusion | Limitation |
|---|---|---|---|---|---|
| Goeree et al11 (Canada) | 2002 | • Strategy E: Maintenance PPI. Acute treatment with a PPI (eg, omeprazole 20 mg or lansoprazole 30 mg once daily) for 4 weeks followed by continuous maintenance treatment with a PPI (same dose). | • Maintenance PPI not only has the highest expected cost per patient over 1 year but also has the lowest expected number of recurrences, expected weeks with heartburn symptoms, and highest QALYs. | • Incremental cost per QALY is CDN$98 422 | • For the symptom relief and symptom recurrence meta-analyses, a majority of studies relied on endoscopy results as a primary entry criterion and outcome measure, whereas symptoms were typically a secondary criterion.
• The authors used moderate-to-severe heartburn as primary measure of GERD symptoms. • 1-year time horizon for the study may be too short to capture long-term complications such as Barrett esophagus or esophageal stricture. • This study used inputs (ie, costs), which are specific to the province of Ontario only. |
| • Strategy G: Step-down maintenance PPI. Acute treatment with a PPI (eg, omeprazole 20 mg or lansoprazole 30 mg once daily) for 4 weeks followed by continuous maintenance treatment with a low-dose PPI (eg, omeprazole 10 mg or lansoprazole 15 mg once daily). | • Dominated through extended dominance | • Dominated through extended dominance | |||
| Gerson et al7 (USA) | 2000 | • PPI-Continuous Arm: Empirical treatment with continuous daily maintenance PPI therapy, without the performance of endoscopy unless there is symptomatic failure. | • A study of continuous PPI therapy as an empirical treatment with continuous daily maintenance PPI therapy, without the performance of endoscopy unless there is symptomatic failure.
• The researchers stated that the outcome of continuous PPI therapy is dominated by on-demand PPI. |
• The researchers stated that the outcome of continuous PPI therapy is dominated by on-demand PPI. | • An analysis of lifetime costs—not known how long patient can expect symptomatic relief.
• Only few of the prior studies used QALYs as a utility measurement and obtained their estimates through a modified Delphi process. • Prior models did not allow patients to switch from H2RAs to PPIs without endoscopy, often did not include the option of Nissen fundoplication, or sent patients without response to PPI for a Nissen without consideration of promotility therapy. • None of the models included patients with nonerosive disease. |
| Kaplan-Machlis et al8 (USA, RCT) | 2000 | • In the study, 268 patients who aged more than 18 years with GERD were enrolled and randomly given omeprazole sodium, 20 mg once daily for up to 6 months.
• Recruited study patients also did not receive PPI or H2RA treatment in the previous 30 days. • Then, for the data analysis, the total cost for omeprazole treatment is assessed. This total cost included direct medical costs, direct nonmedical costs, and indirect costs. |
• As a result, it is shown that 5-year direct medical costs per patient when given omeprazole were notably lower in Denmark, Norway, and Sweden (differences were DKK 8703 [US$1475], NOK 32 992 [US$5155], and SEK 13 036 [US$1946], respectively).
• When indirect costs (loss of production due to GERD-related sick leave) were also included, the cost of surgical treatment increased substantially and exceeded the cost of medical treatment in all countries. |
• It is shown that 5-year direct medical costs per patient when given omeprazole were notably lower in Denmark, Norway, and Sweden (differences were DKK 8703 [US$1475], NOK 32 992 [US$5155], and SEK 13 036 [US$1946], respectively). | • A potential problem with this particular study is that the cost estimates may stem primarily from charges rather than estimates of the true costs.
• The patient completed the questionnaire on traveling and sick leave every 6 months. This rather long period may give rise to recall errors. • Furthermore, the response rate decreased somewhat during the course of the study. Due to these limitations, the estimates of direct medical costs were deemed to be more reliable than the estimates of total costs. |
| Szucs et al13 (Switzerland) | 2009 | • Open-label, randomized, multicenter study comparing the 2 long-term management options with esomeprazole 20 mg—continuous daily or on-demand treatment during 26 weeks—in endoscopically uninvestigated patients seeking primary care in Switzerland for symptoms suggestive of GERD who demonstrated complete relief of symptoms after an initial treatment of 4 weeks with esomeprazole 40 mg.
• Patients found to meet all the inclusion criteria and none of the exclusion criteria at the end of the initial treatment course were randomized in equal proportions to continuous treatment with esomeprazole 20 mg every day. or on-demand treatment with esomeprazole 20 mg. For the randomization, a centrally compiled, computer-generated list was used, which was based on a block size of 4. Each site received a kit consisting of a list of randomization numbers and sealed randomization envelopes for 4 patients. • The investigator was instructed to consecutively allocate the lowest available randomization number, but open the randomization envelopes containing the information on the allocated treatment group only at randomization. It had been planned that each site would recruit 4 patients (or an exact multiple of 4). Each patient in the continuous treatment arm was instructed to take 1 tablet once daily. • In the on-demand arm, the patient was instructed to take 1 tablet daily if needed for the relief of heartburn and to stop when the heartburn is adequately controlled. The study drugs were packed in bottles, and every patient received in total 2 bottles of 100 tablets esomeprazole 20 mg free of charge. The distribution schedule of the study drugs from general practitioner to patient was at the discretion of the general practitioner, ie, the treating physician decided when to distribute study drugs and whether to distribute them all at once or at several occasions. Compliance was determined by counting the tablets returned by the patient. |
• At the end of the 6-month maintenance phase, 93% of the patients treated continuously were classified as “satisfied” (score = 1-4) with their treatment, whereas 77% of the patients, were reported to be “very satisfied” (score = 1-2), Wilcoxon rank sum test (score = 1-7): P < .056.
• The mean number of clinic visits to the investigator for any reason required per patient was 0.50 (SD = 0.647) for those in the continuous group. |
• The data clearly demonstrate that on-demand esomeprazole 20 mg therapy is associated with significantly better effectiveness and lower costs than a strategy consisting of intermittent 4-week treatment courses of omeprazole 20 mg once daily. However, the treatment with continuous esomeprazole was more efficient than the on-demand therapy with regard to remission of heartburn. | • The endpoint used in this primary care study (symptoms of any severity on at least 2 days during the previous week), may not correspond to a definition of relapse in clinical practice. |
Note. PPI = proton pump inhibitor; QALYs = quality-adjusted life in years; GERD = gastroesophageal reflux disease; H2RA = histamine 2 receptor antagonists; RCT = randomized controlled trial.
Similarly, Szucs et al13 study found out that the percentage of patients satisfied with receiving conventional (continuous) treatment of esomeprazole 20 mg daily after 4 weeks of 40 mg daily esomeprazole is 93% (scale = 1-4), whereas 77% patients on this treatment were very satisfied (scale = 1-2) with the treatment received using Wilcoxon rank sum test (scale = 1-7: P < .0056).
Continuous Step-up Treatment of PPIs
In a study done by Funk et al16 in the United States, 2015, a Markov model with a 6-month cycle and a 30-year time horizon was used to examine the cost-effectiveness of PPIs for the management of GERD. Cost-utility was determined based on QALYs gained. A healthy patient with no GERD symptoms received 0.5 QALYs for every 6-month cycle, whereas patient who died received 0 QALYs for that cycle. Continuous step-up treatment was used where PPI treatment started with 20 mg omeprazole twice daily for patients with mild symptom. However, the dose was increased to 40 mg twice per day if the symptom persists. As a result, cost per QALYs gained through PP treatment is US$11 587.40 (Table 5).
Table 5.
Cost-effectiveness of Step-up PPI Treatment.
| Author | Year | Methodology | Outcome | Conclusion | Limitation of study |
|---|---|---|---|---|---|
| Funk et al16 (USA) | 2015 | • A Markov model with a 6-month cycle and a 30-year time horizon was used to examine the cost-effectiveness of PPI for the management of GERD.
• Utility was determined based on QALYs gained. A healthy patient with no GERD symptoms received 0.5 QALYs for every 6-month cycle, whereas patient who died received 0 QALYs for that cycle. Continuous step-up treatment is used where PPI treatment started with 20 mg omeprazole twice daily for patient with mild symptom. However, the dose is increased to 40 mg twice per day if the symptom persists. |
• As a result, cost per QALYs gained through PPI treatment is US$11 587.40. Therefore, PPI therapy is a cost-effective treatment over 30 years if PPIs are available at a less price. | • PPI therapy is a cost-effective treatment over 30 years if PPIs are available at a less price. | • Because our analysis extended to 30 years, the model assumed that shorter term failure rates would remain stable over the duration of the model; however, this assumption regarding the linearity of relapse rates is one limitation of the study.
• A second limitation is that there is a cohort of patients who may require intermittent PPI therapy after a Stretta or EsophyX, but would not be considered treatment failures. We were not able to account for this group of patients because published rates of “partial failures” do not exist. Our model assumed that patients who “relapsed” after a procedure were placed back onto the base case dosing regimen of 20 mg twice a day. • Another study limitation is that our analysis is from the payer’s perspective (the patient), not from a societal perspective. Thus, our model did not account for indirect costs such as losses in productivity owing to work absences. |
| Ofman et al9 (USA) | 2000 | • In this study, patients were assigned with 20 mg rabeprazole every day for 8 weeks. Patient who experienced the symptom after a full course of initial therapy will then receive 40 mg rabeprazole every day for an additional 8-week course. If symptoms prolonged after the second course of therapy, patients remained on high-dose rabeprazole for an additional 8 weeks and then underwent a surgical evaluation.
• The data analysis is based on average and incremental cost-effectiveness ratios. |
• As a result, the average cost-effectiveness ratio was lower for rabeprazole therapy than for ranitidine therapy (US$2748 per symptomatic recurrence prevented vs US$4719 per symptomatic recurrence prevented). | • The average cost-effectiveness ratio was lower for rabeprazole therapy than for ranitidine therapy (US$2748 per symptomatic recurrence prevented vs US$4719 per symptomatic recurrence prevented). The cost of preventing one additional symptomatic recurrence with rabeprazole rather than ranitidine was US$313 (incremental cost-effectiveness ratio). | • The quality of the model estimates largely depended on the quality of the results reported in the published literature, and in some instances, scant data were available. We did not consider medication compliance, although patients generally adhere better to once-daily, rather than multiple-dose, regimens.
• This analysis also did not consider health-related quality of life, patient preferences, satisfaction with care, or indirect costs; however, regimens that are most effective in relieving initial symptoms and maintaining symptom relief are most likely to favorably impact these outcomes. • Last, we used symptom response as the outcome measure and assumed that all asymptomatic patients have esophagitis that has been healed, yet there are patients whose symptoms are relieved but whose endoscopic findings have not resolved. The clinical significance of this finding, however, remains unclear, making it difficult to assess the impact of this assumption on the analysis. |
Note. PPI = proton pump inhibitor; QALYs = quality-adjusted life in years; GERD = gastroesophageal reflux disease.
On the contrary, Ofman et al9 studied the cost-effectiveness of rabeprazole versus generic ranitidine for symptoms resolution in patients with erosive esophagitis. In this study, patients were assigned with 20 mg rabeprazole every day for 8 weeks. Patient who still experienced the symptoms after a full course of initial therapy will then receive 40 mg rabeprazole every day for additional 8-week course. If the symptoms prolonged after the second course of therapy, patients remained on high-dose rabeprazole for an additional 8 weeks and then underwent a surgical evaluation. The data analysis was based on average ratio and ICERs. As a result, the average cost-effectiveness ratio was lower for rabeprazole therapy than for ranitidine therapy (US$2748 per symptomatic recurrence prevented vs US$4719 per symptomatic recurrence prevented).
Continuous Step-down PPI Treatment
A retrospective study done by Cahir et al14 from Ireland investigated the best long-term management treatment of GERD using continuous PPI treatment followed by maintenance step-down regimen of PPI (original and its generic bioequivalent) according to the National Institute for Health and Care Excellence guidelines. Five strategies were compared but the most significant in cost saving of continuous step-down therapy is the therapeutic switching and dose reduction whereby the patients on maximum dose of PPI switched and maintained to generic brand PPI with lower dose for a year with a reduction of 45.95% (US$43 001 336.96) of overall estimated annual net ingredient cost savings. This method has proven to reduce the recurrent symptoms of GERD in more than 70% of patients. About 58% of US veterans on long-term PPI discontinuing PPI use have no considerable change of life quality even after 1 year (Table 6).
Table 6.
Cost-effectiveness of Step-down PPI Treatment.
| Author | Year | Methodology | Outcome | Conclusion | Limitation |
|---|---|---|---|---|---|
| Cahir et al14 (Ireland) | 2012 | • The National Shared Services Primary Care Reimbursement Service of the Health Service Executive in Ireland (HSE-PCRS) pharmacy provides free health services, including medications to eligible persons in Ireland.
• Drugs are categorized into 4 classes: unbranded generic, branded generic, proprietary drug with a generic equivalent, and proprietary drug with no generic equivalent. • Five scenarios were identified according to published National Institute for Health and Care Excellence clinical guidelines for more cost-effective PPI prescribing: - Least expensive PPI at initiation - Therapeutic switching (cheaper brand/generic equivalent) - Dose reduction - Therapeutic switching and dose reduction - Therapeutic substitution • Costs were calculated as the NIC of the dispensed PPI and the total expenditure which included NIC and pharmacist dispensing fee. |
• The greatest cost savings were obtained by switching patients’ PPI therapy to the least expensive PPI and also stepping patients down to maintenance dose after 3 consecutive months at maximum therapeutic dosage.
• Regular maintenance low dose of most PPIs will prevent recurrent GERD symptoms in 70% to 80% of patients. • In the United States, 48% of Veterans adopted step-down therapy, whereas 58% of patients on long-term PPI therapy discontinued PPI use and remained asymptomatic with no significant change in quality of life after 1 year. • Total NIC was US$94 128 196.13 for claimants on PPI therapy during 2007. The estimated costing savings for each of the 5 scenarios in a 1-year period were: - US$39 447 368.13 (42% reduction); - US$31 572 626.24 (34%); - US$22 732 312.25 (24%); - US$43 250 442.78 (46%); - (v) US$37 363 297.55 (40%). |
• PPIs are highly effective but they are being overprescribed in Ireland for longer durations and at higher doses than current guidelines advice.
• As PPIs lose patent protection and cheaper generic equivalents become available on the market, potential cost savings could be obtained with limited impact on clinical outcomes. |
• Lack of detailed diagnostic information that determines clinical indications for PPI therapy in the database limited the investigation of individual patient factors and differences in drug indication |
Note. PPI = proton pump inhibitor; NIC = net ingredient cost; GERD = gastroesophageal reflux disease.
On-demand PPI Treatment
Szucs et al13 investigated the cost-effectiveness between on-demand and continuous treatment of esomeprazole 20 mg after the patients received initial treatment of esomeprazole 40 mg daily for 4 weeks. About 94% patients on on-demand therapy were classified under satisfied (scale = 1-4) and the percentage on very satisfied was 74% (scale = 1-2) using Wilcoxon rank sum test (score = 1-7: P < .0056) (Table 7). Similarly, Gerson et al7 study investigated using decision analysis on on-demand PPI strategy in which the empirical treatment with an 8-week course of PPI therapy administered on demand when GERD symptoms recurred. Patients in this group required at most three 8-week courses (24 weeks) of medication per year. Patients failing on-demand therapy (recurrence of symptoms earlier than 2 months without medication) received continuous PPI therapy, and endoscopy was performed only if symptoms recur on daily PPI therapy. According to this study, on-demand PPI strategy was the most cost-effective approach with discounted ICER of US$20 934 per QALY gained by patient with mild to severe GERD symptoms and US$379 223 per QALY gained for patient with mild GERD symptoms. On-demand PPI was dominant with an ICER of US$2197/QALY gained.
Discussion
This narrative review focuses on the cost-effectiveness of 5 different strategies for long-term management of heartburn by PPI. Then, the most cost-effective strategy is examined. The 5 strategies are continuous (step-up, step-down, and maintenance therapy), on-demand, and intermittent therapies. For continuous strategy, participants of the studies received treatment on daily basis. They also received increasing, decreasing, or same dose of PPI in step-up, step-down, and maintenance therapy, respectively. For on-demand therapy, participants received treatment only when the symptoms appear, whereas in intermittent therapy, PPI was given for certain period and then discontinued for a while before proceeding the treatment with the same dose.
Omeprazole is more effective in relieving heartburn compared with ranitidine with not much increment in cost.17,18 A study reported that 49.0% of patients treated with omeprazole improved heartburn resolution at 2 weeks and 58.6% at 4 weeks compared with 33.3% patients treated with ranitidine at 2 weeks and 35% at 4 weeks.8 The study also showed that patients who had been treated with omeprazole have 43% heartburn resolution, which was greater than the percentage number of patients treated with ranitidine, 24%.8,15
Based on these 5 strategies mentioned, they can be compared using incremental cost-effective ratio per QALY in US dollar monetary value. From Table 8, on-demand strategy has the lowest cost per QALY, whereas the maintenance treatment of PPI is documented to be the highest. Although on-demand strategy deemed to be the least costly among others, other perspectives should be taken into consideration such as the recurrence rate of heartburn and the WTP that may influence the result of the analysis.
Table 8.
ICER Per QALY.
| Step up | Maintenance | Intermittent | On-demand |
|---|---|---|---|
| US$11 587.40/QALY | US$73 367.40/QALY | US$9098.80/QALY | US$2197/QALY |
Note. ICER = incremental cost-effectiveness ratio; QALY = quality-adjusted life in years.
According to Wahlqvist et al,10 cost-effectiveness of intermittent, on-demand, and continuous esomeprazole was compared for long-term management and the effectiveness was determined by the probability of expected relapse occurred. On-demand therapy was shown to be the most effective and cost saving compared with all the other treatments. The expected relapse frequency per patient in on-demand therapy was the lowest, followed by intermittent and continuous treatment with 0.10, 0.57, and 0.47, respectively. In addition to the cheapest direct medical cost of on-demand PPI strategy, it exhibited a difference of 16% compared with intermittent strategy and of 34% compared with the continuous therapy. QALY as the outcome of treatment was also studied in some of the selected publications. The on-demand strategy has the lowest cost per QALY while the maintenance treatment of PPI is documented to be the highest.19,20
Finally, it was demonstrated that the long-term treatment with PPI is effective but costly. Nevertheless, the expected recurrent episodes, quality of life, patient’s satisfaction, and patient’s WTP has to be considered to decide the best treatment. To achieve long-term cost-effective approach, we recommend on-demand approach to treat heartburn symptoms, but if the symptoms persist, treatment with continuous step-down therapy should be applied.
Conclusion
Our literature search revealed that PPIs are more effective than H2RA in relieving heartburn. For continuous step-up strategy, PPIs are regarded as cost-effective if they are available at lower price. For continuous step-down strategy, the most significant cost-saving method is to switch to generic PPIs of a lower dose in the maintenance phase. This method has been proven to reduce GERD symptoms recurrence. Meanwhile, continuous maintenance strategy with PPI of the same dose was demonstrated as the costliest option; however, this strategy has the lowest expected number of recurrences, reduced expected weeks with heartburn symptoms, and highest QALY. PPI on-demand approach was the most cost-effective strategy with established patient’s satisfaction. However, we were not able to conclude the best PPI agent to be used in the treatment of heartburn because different PPIs were studied in different literatures. In addition, the cost per QALY for each strategy was obtained from different literatures, so the comparison was not totally appropriate.
Limitation
Some of the main limitations of this study are the following:
This review only includes studies between 2000 and 2015, so studies published after 2015 are not part of this review as this review was initially completed in 2015 and thus limits the scope.
Second, studies published in PubMed database and in English language are included, which limits the range of this review.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Sana Shamim  https://orcid.org/0000-0001-8630-8644
https://orcid.org/0000-0001-8630-8644
References
- 1. El-Serag HB, Sweet S, Winchester CC, Dent J. Update on the epidemiology of gastroesophageal reflux disease: a systematic review. Gut. 2014;63:871-880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Boeckxstaens G, El-Serag HB, Smout AJ, Kahrilas PJ. Symptomatic reflux disease: the present, the past and the future. Gut. 2014;63:1185-1193. doi: 10.1136/gutjnl-2013-306393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Eusebi LH, Ratnakumaran R, Yuan Y, Solaymani-Dodaran M, Bazzoli F, Ford AC. Global prevalence of, and risk factors for, gastro-esophageal reflux symptoms: a meta-analysis. Gut. 2017;67:430-440. doi: 10.1136/gutjnl-2016-313589. [DOI] [PubMed] [Google Scholar]
- 4. Sigterman KE, van Pinxteren B, Bonis PA, Lau J, Numans ME. Short-term treatment with proton pump inhibitors, H2-receptor antagonists and prokinetics for gastro-oesophageal reflux disease-like symptoms and endoscopy negative reflux disease. Cochrane Database Syst Rev. 2013;(5):CD002095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Sandhu DS, Fass R. Current trends in the management of gastroesophageal reflux disease. Gut Liver. 2017;12:7-16. doi: 10.5009/gnl16615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Peery AF, Dellon ES, Lund J, et al. Burden of gastrointestinal disease in the United States: 2012 update. Gastroenterology. 2012;143(5):1179-1187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Gerson LB, Robbins AS, Garber A, Hornberger J, Triadafilopoulos G. A cost-effectiveness analysis of prescribing strategies in the management of gastroesophageal reflux disease. Am J Gastroenterol. 2000;95(2):395-407. [DOI] [PubMed] [Google Scholar]
- 8. Kaplan-Machlis B, Spiegler GE, Zodet MW, Revicki DA. Effectiveness and costs of omeprazole vs ranitidine for treatment of symptomatic gastroesophageal reflux disease in primary care clinics in West Virginia. Arch Family Med. 2000;9(7):624-630. [DOI] [PubMed] [Google Scholar]
- 9. Ofman JJ, Yamashita BD, Siddique RM, Larson LR, William MK. Cost effectiveness of rabeprazole versus generic ranitidine for symptom resolution in patients with erosive esophagitis. Am J Management Care. 2000;6(8):905-916. [PubMed] [Google Scholar]
- 10. Wahlqvist P, Junghard O, Higgins A, Green J. Cost effectiveness of proton pump inhibitors in gastro-oesophageal reflux disease without oesophagitis: comparison of on-demand esomeprazole with conventional omeprazole strategies. Pharmacoeconomics. 2002;20(4):267-277. [DOI] [PubMed] [Google Scholar]
- 11. Goeree R, O’Brien BJ, Blackhouse G, Marshall J, Briggs A, Lad R. Cost-effectiveness and cost-utility of long-term management strategies for heartburn. Value Health. 2002;5(4):312-328. [DOI] [PubMed] [Google Scholar]
- 12. Elliott RA, Hooper L, Payne K, Brown TJ, Roberts C, Symmons D. Preventing non-steroidal anti-inflammatory drug-induced gastrointestinal toxicity: are older strategies more cost-effective in the general population? Rheumatology. 2006;45(5):606-613. [DOI] [PubMed] [Google Scholar]
- 13. Szucs T, Thalmann C, Michetti P, Beglinger C. Cost analysis of long-term treatment of patients with symptomatic gastroesophageal reflux disease (GERD) with esomeprazole on-demand treatment or esomeprazole continuous treatment: an open, randomized, multicenter study in Switzerland. Value Health. 2009;12(2):273-281. [DOI] [PubMed] [Google Scholar]
- 14. Cahir C, Fahey T, Tilson L, Teljeur C, Bennett K. Proton pump inhibitors: potential cost reductions by applying prescribing guidelines. BMC Health Serv Res. 2012;12(1):408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. de Groot NL, Spiegel BM, van Haalen HG, de Wit NJ, Siersema PD, van Oijen MG. Gastroprotective strategies in chronic NSAID users: a cost-effectiveness analysis comparing single-tablet formulations with individual components. Value Health. 2013;16(5):769-777. [DOI] [PubMed] [Google Scholar]
- 16. Funk LM, Zhang JY, Drosdeck JM, Melvin WS, Walker JP, Perry KA. Long-term cost-effectiveness of medical, endoscopic and surgical management of gastroesophageal reflux disease. Surg. 2015;157(1):126-136. [DOI] [PubMed] [Google Scholar]
- 17. Van Pinxteren B, Sigterman KE, Bonis P, Lau J, Numans ME. Short-term treatment with proton pump inhibitors, H2-receptor antagonists and prokinetics for gastro-oesophageal reflux disease-like symptoms and endoscopy negative reflux disease. Cochrane Database Syst Rev. 2010;11:CD002095. [DOI] [PubMed] [Google Scholar]
- 18. MacLaren R, Campbell J. Cost-effectiveness of histamine receptor-2 antagonist versus proton pump inhibitor for stress ulcer prophylaxis in critically ill patients. Critical Care Med. 2014;42(4):809-815. [DOI] [PubMed] [Google Scholar]
- 19. Ponce J, Argüello L, Bastida G, Ponce M, Ortiz V, Garrigues V. On-demand therapy with rabeprazole in nonerosive and erosive gastroesophageal reflux disease in clinical practice: effectiveness, health-related quality of life, and patient satisfaction. Dig Dis Sci. 2004;49(6):931-936. [DOI] [PubMed] [Google Scholar]
- 20. Bayerdörffer E, Bigard MA, Weiss W, et al. Randomized, multicenter study: on-demand versus continuous maintenance treatment with esomeprazole in patients with non-erosive gastroesophageal reflux disease. BMC Gastroenterol. 2016;16(1):48. [DOI] [PMC free article] [PubMed] [Google Scholar]