Abstract
Exercise is touted as the ideal prescription to treat and prevent many chronic diseases. We examined changes in utilization and cost of medication classes commonly prescribed in the management of chronic conditions following participation in 12-months of supervised exercise within the Veterans Affairs Gerofit program. Gerofit enrolled 480 veterans between 1999 and 2017 with 12-months participation, with 453 having one or more active prescriptions on enrollment. Active prescriptions overall and for five classes of medications were examined. Changes from enrollment to 12 months were calculated, and cost associated with prescriptions filled were used to estimate net cost changes. Active prescriptions were reduced for opioids (77 of 164, 47%), mental health (93 of 221, 42%), cardiac (175 of 391, 45%), diabetes (41 of 166, 25%), and lipid lowering (56 of 253, 22%) agents. Cost estimates resulted in a net savings of $38,400. These findings support the role of supervised exercise as a favorable therapeutic intervention that has impact across chronic conditions.
Keywords: veteran, elderly, polypharmacy, exercise, cost
Introduction
Exercise is a powerful therapeutic intervention that has beneficial impacts on pulmonary and cardiovascular diseases, metabolic disorders, muscle, bone and joint diseases, cancer, and depression (Vina et al., 2012). Furthermore, the impact of exercise is comparable to medications on diabetes outcomes (reduced Hemoglobin A1C), elevated blood pressure, lipid control, and thrombosis (Fiuza-Luces et al., 2013). Increasing physical activity is one of the first line recommendations in the guidelines for the treatment of hypertension, diabetes, and lipids. (American Diabetes Association, 2019; Grundy et al., 2019; Whelton et al., 2018) However, investigators have not described the impact of exercise on changes relating to polypharmacy in older adults despite anecdotal reports from exercise participants that they were able to reduce medications across a variety of categories following initiation of exercise (Blumenthal et al., 1999). Hence, there is a critical evidence gap on the impact of exercise on prescribed medications used to manage chronic conditions.
The Department of Veterans Affairs (VA) has supported an exercise program for older veterans, Gerofit, as a VA Best Practice (Elnahal et al., 2017). Established in 1986 at the Durham VA Geriatric Research, Education and Clinical Center, Gerofit has served as an ongoing clinical outpatient program for older veterans. Gerofit outcomes include improved fitness, physical function, well-being, reduced cardio-metabolic risk factors, and longevity (Cowper et al., 1991; Morey et al., 1996, 1989, 2018, 2002). Building on anecdotal reports of reductions in prescribed medications following program participation we aimed to determine if 12-month continuous Gerofit exercise program participants reduced the number of active prescriptions overall and across five classes of medications (opioids, mental health, cardiac, diabetes, and lipid lowering), numbers of fills of medications, and cost of medications.
Methods
Study Design and Participants
This was a single center, retrospective pre- and post-exercise intervention study at the Durham VA Health Care System (DVAHCS). Participants included veterans enrolled in the Gerofit program between 1999, with the advent of computerized medical record keeping, and 2017. Program eligibility criteria includes referral to program by primary care provider indicating stable health, cognitively and physically able to function independently in a group setting, and free of acute health conditions that restricts physical activity such as a recent stroke or cardiovascular event within prior 6 months. Program participants meet 3 days weekly for supervised exercise. Of note, Gerofit is largely focused on older veterans, that is, ages 65 and above; but during the early development of the program, some younger veterans with multiple chronic conditions and poor physical function were accepted into the program and are included in this analysis. For inclusion in this study, program participants had to have at least one note in each quarter from their start in the program, be active in Gerofit for 12 continuous months, and have one or more active medications on their profile from the DVAHCS pharmacy upon enrollment. Gerofit is considered a clinical program and program participants signed a research consent form that allows for the analysis of program outcomes. The informed consent was reviewed and is approved annually by the local Institutional Review Board.
Gerofit Exercise Program
Following enrollment in Gerofit, each person underwent a functional assessment that served as the basis for developing a personalized exercise program based on documented functional impairments (Morey et al., 2018; Rikli & Jones, 1999). Each person received an exercise program tailored to functional deficits that included an aerobic component, targeted progressive strength training, and group-based balance, tai chi, and core conditioning classes. Participants were supervised by clinical exercise physiologists who provided individual guidance until each person demonstrated competency with their exercise prescription. Individuals were then guided towards progression of exercise that followed national recommended guidelines (Nelson et al., 2007). Functional assessments were conducted quarterly the 1 year and served as the basis for systematic tailored exercise prescription updates. (Rikli & Jones, 1999) Notes were entered into the computerized medical record to document continued attendance in the program. Because this is an ongoing clinical service, there was no control group.
Demographics, Clinical and Medication Data Collection
Data were collected from the DVAHCS medical records and VA corporate data warehouse, including baseline demographics (included age, sex, race), active medication orders, and prescriptions filled. Active medication orders were captured at enrollment in Gerofit and at 12 months after enrollment. Medications were grouped into five classes of medications based on anecdotal reports from program participants about reductions in these classes of medications: opioids, mental health (including sedative/hypnotics, antidepressants, and antipsychotics), cardiovascular (including beta blockers, alpha blockers, calcium channel blockers, peripheral vasodilators, diuretics, ace inhibitors, angiotensin receptor blockers, and antihypertensive combinations), diabetic (oral and injectable agents), and lipid lowering.
Analysis
The overarching goal of this analysis was to describe on an aggregate level the overall 12-month change in prescribing for the five medication classes listed above (opioids, mental health, cardiovascular, diabetic, and lipid lowering). This analysis was constructed in two ways.
First, at each time point (starting and 12 months later) each subject was classified as “yes” or “no” in having at least one medication within each of the five classes. Each subject for each medication class was then further classified into categories of “Decrease,” “Same” or “Increase” to describe the 12-month change in prescribing.
Second, medications were grouped as described above into the five classes, and costs were calculated by multiplying the quantity supplied by the price per unit. This information was then used to calculate average costs per fill overall and within each class of medications. Net changes over 12 months in cost were calculated by subtracting the cost related to increases from the cost related to decreases in fills and associated costs for the prescriptions fills.
Results
Participant Characteristics
A total of 480 veterans were active for at least 12 months in the Gerofit program at the DVAHCS. Of these patients, 453 met inclusion criteria of having at least one active medication on their profile from the DVAHCS pharmacy at the time of enrollment. The mean age of the cohort at enrollment was 67 years, ranging from ages 31 to 91, 94% male, 43% Caucasian. At baseline, the percent of patients with at least one active prescription in the respective medication classes was 36% on an opioid, 49% on a mental health medication, 86% on a cardiac medication, 37% on a diabetes medication, and 56% on a lipid lowering medication (Table 1).
Table 1.
Baseline Characteristics of Eligible Participants (n = 453).
| Age, mean years | 67 ± 10 |
| Gender, % male | 94 |
| Race, % | |
| White | 43.7 |
| Black | 50.8 |
| Other | 5.5 |
| Service Connected, % | 63.3 |
| *Usual Gait Speed, mean meters/second | 1.1 ± 0.2 |
| *6-minute walk, mean meters | 478.2 ± 104.6 |
| Opioids, n (%) | 164 (36) |
| Mental Health, n (%) | 221 (49) |
| Cardiac, n (%) | 391 (86) |
| Diabetes, n (%) | 166 (37) |
| Lipid Lowering, n (%) | 253 (56) |
Note. *Functional data only available for n = 101 due to changes in functional assessment battery.
Medications
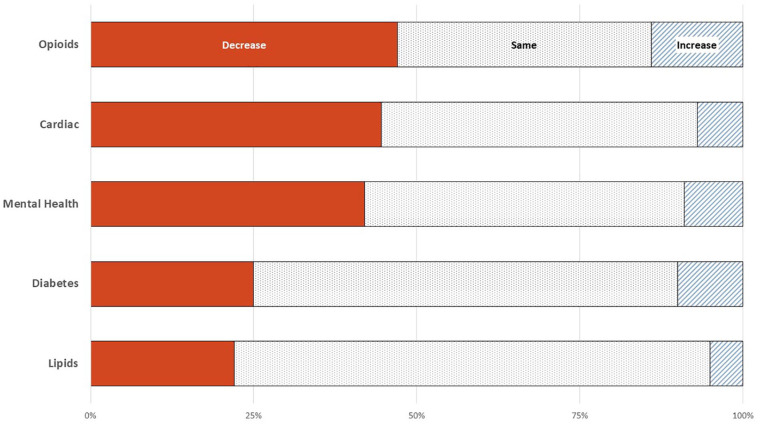
After 12 months of participation in Gerofit, the percentage of patients that reduced the number of active prescriptions in the respective categories by at least one was 47% in opioids, 42% in mental health medications, 45% in cardiac medications, and 25% diabetes medications, and 22% lipid lowering medications, respectively. The percentage of patients that had no change in the respective categories was 39% in opioids, 49% in mental health and cardiac medications, 65% in diabetes, and 73% in lipid lowering medications, respectively. The percentage of patients that increased in the respective categories by at least one was 14% in opioids, 9% in mental health medications, 7% in cardiac medications, 10% in diabetes, and 5% in lipid lowering medications, respectively (Figure 1). This resulted in net changes of 33% decrease both in opioids and mental health medications, 38% decrease in cardiac medications, 14% decrease in diabetes medications, and 17% decrease in lipid lowering medications, respectively.
Figure 1.
Change in medications from baseline to 12 months of participation in Gerofit. Each row indicates a class of medications with the respective change over 12-months from the entire cohort within each class of medications represented by solid (left), dotted (center), and striped (right). The solid shows percent of veterans that decreased by one or more medications in the respective category, the dotted shows those that remained on the same number of medications, and the striped shows veterans who increased by one or more medications in the respective category. Baseline sample within each category; opioids (n = 164), mental health (n = 221), cardiac (n = 391), diabetes (n = 166), and lipids (n = 253).
When comparing prescriptions filled in the pre-Gerofit baseline 12-month period to the post-12-month period, 55% of patients had a decrease in their overall number of fills, with an average associated cost decrease of $473 per fill, or $117,254 overall. Comparatively, 45% of patients had an increase in overall number of fills, with an average associated cost increase of $387 per fill, or $78,858, and this yields a net reduction of overall costs of $38,396. When broken down by medication categories, a net reduction was found in mental health ($5,719), cardiac ($3,661), and diabetes medications ($2,212), and a net increase was found in opioids ($216) and lipid lowering medications ($1,075).
Discussion
In this cohort of Gerofit patients, supervised exercise was associated with reductions in medication usage across various categories of medication classes. Costs associated with increases or decreases in the number of filled prescriptions for medications was greater for decreased medication use resulting in a net cost saving for the institution. To our knowledge, we are the first to report this type of finding across multiple categories of medications commonly used to manage chronic diseases. Exercise has been and continues to be recommended in the treatment of various diseases. The most recent ADA guidelines recommends lifestyle management as a fundamental aspect of diabetes care, including physical activity (American Diabetes Association, 2019). Similarly, the most recent high blood pressure guidelines recommend increasing physical activity via structured exercise, and cholesterol guidelines recommend engaging in moderate-to-vigorous physical activity (Grundy et al., 2019; Whelton et al., 2018). The Centers for Disease Control and Prevention chronic pain guidelines support exercise therapy as an effective nonpharmacologic treatment option in managing chronic pain, including chronic low back pain, as well as osteoarthritis of the knee and hip (Dowell et al., 2016). The VA/DOD Major Depressive Disorder guidelines even incorporate exercise as an adjunct in the management of major depression (Veterans Health Administration, Department of Defense, 2017). Despite exercise being incorporated into treatment guidelines, there is a paucity of published literature that directly examines the impact of exercise on specific prescribed medication usage. Williams and Barry reported that vigorous exercise was associated with decreased hypertensive, diabetic and hypercholesterolemia medication use in a cross-sectional review of 107,032 runners in comparisons between most fit and least fit, defined as best reported race time, and self-reported medication use (Williams & Franklin, 2007). Comparing medication data from the most and least fit quartiles was associated with 58% to 87% lower use of the classes of medications used (Williams & Franklin, 2007). Similarly, among men in the Veterans Exercise Testing Study, veterans in the highest quartile of fitness by direct treadmill testing had lower health care costs than men in the lowest quartile of fitness, but the contribution of medication costs were not detailed in these studies (de Souza de Silva et al., 2019; Myers et al., 2019).
To our knowledge, we are the first to report the impact of exercise retrospectively on prescribed medication use following 1 year of supervised exercise. We also believe we are the first to directly calculate actual direct cost savings from a supervised exercise intervention. Of note, reductions in medication usage occurred across various classes of medications. Clinic-based counseling to increase exercise is most prevalent for obesity and diabetes management (Wee et al., 1999), but we provide evidence of benefit cutting across additional systems, including mental health, pain, and cardiovascular, which is highly consistent with the vast literature that supports exercise as a “pluripotent” therapeutic intervention (Pedersen & Saltin, 2015).
Deprescribing medications among older adults is a difficult issue for physicians. A recent survey of 750 physicians working with older adults (Primary Care, Cardiology, Geriatrics) revealed that just over 80% of those physicians considered deprescribing cardiovascular medications for patients in the last month (Goyal et al., 2019). The largest barrier to deprescribing was a concern of interfering with another physicians’ treatment. The dramatic reduction seen within cardiac medications of the Gerofit cohort may represent a health system wide effect of synergistic care. Patients may have improving cardiovascular profiles through exercise, and physicians are receiving quarterly updates on patients’ functional improvement.
There are two limitations of this study which are worthy of mention. First is the lack of a control group that might control for secular changes in health care delivery, an example of which is the dedicated efforts at reducing opioid use which may account for some of our findings in our reported reductions of opioid use. Future research with an appropriately matched control group in warranted. Secondly, we did not capture changes in doses of medications, which might have resulted in an underestimate of our findings. Again, future research could look at how exercise may assist in reducing doses of current medications, further strengthening the importance of exercise in the management of multiple comorbidities.
We believe this work provides a major contribution to the literature pertaining to the importance of exercise in health care (Morey et al., 2018). This contributes to a growing body of literature suggesting that exercise and prevention should be more prominently featured in our health care systems.
Acknowledgments
We are grateful to the veterans who have given so much of their time. The Durham Gerofit programs receives support from the Durham VA HealthCare System, the Durham VA Geriatric Research, Education and Clinical Care, and the National VA Program Offices of Geriatrics and Extended Care (GEC) and Rural Health. We would like to thank the GEC Data Analysis Center for their advice on this project. The views expressed by the authors of this manuscript and the contents do not represent the views of the Department of Veterans Affairs or the United States Government.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Marc J. Pepin  https://orcid.org/0000-0002-7560-4461
https://orcid.org/0000-0002-7560-4461
References
- American Diabetes Association. (2019). 5. Lifestyle management: Standards of medical care in diabetes-2019. Diabetes Care, 42(Suppl. 1), S46–S60. 10.2337/dc19-S005 [DOI] [PubMed] [Google Scholar]
- Blumenthal J. A., Babyak M. A., Moore K. A., Craighead W. E., Herman S., Khatri P., Waugh R., Napolitano M. A., Forman L. M., Appelbaum M., Doraiswamy P. M., Krishnan K. R. (1999). Effects of exercise training on older patients with major depression. Archives of Internal Medicine, 159(19), 2349–2356. 10.1001/archinte.159.19.2349 [DOI] [PubMed] [Google Scholar]
- Cowper P. A., Morey M. C., Bearon L. B., Sullivan R. J., DiPasquale R. C., Crowley G. M., Feussner J. R. (1991). The impact of supervised exercise on psychological well-being and health status in older veterans. Journal of Applied Gerontology, 10(4), 469–485. [DOI] [PubMed] [Google Scholar]
- de Souza de Silva C. G., Kokkinos P., Doom R., Loganathan D., Fonda H., Chan K., de Araújo C. G. S., Myers J. (2019). Association between cardiorespiratory fitness, obesity, and health care costs: The Veterans Exercise Testing Study. International Journal of Obesity, 43(11), 2225–2232. 10.1038/s41366-018-0257-0 [DOI] [PubMed] [Google Scholar]
- Dowell D., Haegerich T. M., Chou R. (2016). CDC guideline for prescribing opioids for chronic pain—United States, 2016. JAMA, 315(15), 1624–1645. 10.1001/jama.2016.1464 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elnahal S., Maddock E., Shaheen M. (2017). Best care everywhere by VA professionals across the Nation. U.S. Government Publishing Office. [Google Scholar]
- Fiuza-Luces C., Garatachea N., Berger N. A., Lucia A. (2013). Exercise is the real polypill. Physiology (Bethesda), 28(5), 330–358. 10.1152/physiol.00019.2013 [DOI] [PubMed] [Google Scholar]
- Goyal P., Anderson T. S., Bernacki G. M., Marcum Z. A., Orkaby A. R., Kim D., Zullo A., Krishnaswami A., Weissman A., Steinman M. A., Rich M. W. (2019). Physician perspectives on deprescribing cardiovascular medications for older adults. Journal of the American Geriatrics Society, 68(1), 78–86. 10.1111/jgs.16157 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grundy S. M., Stone N. J., Bailey A. L., Beam C., Birtcher K. K., Blumenthal R. S., Braun L. T., de Ferranti S., Faiella-Tommasino J., Forman D. E., Goldberg R., Heidenreich P. A., Hlatky M. A., Jones D. W., Lloyd-Jones D., Lopez-Pajares N., Ndumele C. E., Orringer C. E., Peralta C. A., . . . Yeboah J. (2019). 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA Guideline on the management of blood cholesterol: A report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Journal of the American College of Cardiology, 73(24), e285–e350. 10.1016/j.jacc.2018.11.003 [DOI] [PubMed] [Google Scholar]
- Morey M. C., Cowper P. A., Feussner J. R., DiPasquale R. C., Crowley G. M., Kitzman D. W., Sullivan R. J. (1989). Evaluation of a supervised exercise program in a geriatric population. Journal of the American Geriatrics Society, 37, 348–354. [DOI] [PubMed] [Google Scholar]
- Morey M. C., Lee C. C., Castle S., Valencia W. M., Katzel L., Giffuni J., Kopp T., Cammarata H., McDonald M., Oursler K. A., Wamsley T., Jain C., Bettger J. P., Pearson M., Manning K. M., Intrator O., Veazie P., Sloane R., Li J., Parker D. C. (2018). Should structured exercise be promoted as a model of care? Dissemination of the Department of Veterans Affairs Gerofit Program. Journal of the American Geriatrics Society, 66(5), 1009–1016. 10.1111/jgs.15276 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morey M. C., Pieper C. F., Crowley G. M., Sullivan R. J., Puglisi C. M. (2002). Exercise adherence and 10-year mortality in chronically ill older adults. Journal of the American Geriatrics Society, 50(12), 1929–1933. [DOI] [PubMed] [Google Scholar]
- Morey M. C., Pieper C. F., Sullivan R. J., Crowley G. M., Cowper P. A., Robbins M. S. (1996). Five-year performance trends for older exercisers: A hierarchical model of endurance, strength, and flexibility. Journal of the American Geriatrics Society, 44, 1226–1231. [DOI] [PubMed] [Google Scholar]
- Myers J., de Souza E. S. C. G., Doom R., Fonda H., Chan K., Kamil-Rosenberg S., Kokkinos P. (2019). Cardiorespiratory fitness and health care costs in diabetes: The veterans exercise testing study. The American Journal of Medicine, 132(9), 1084–1090. 10.1016/j.amjmed.2019.04.006 [DOI] [PubMed] [Google Scholar]
- Nelson M. E., Rejeski W. J., Blair S. N., Duncan P. W., Judge J. O., King A. C., Macera C. A., Castaneda-Sceppa C., & American Heart Association. (2007). Physical activity and public health in older adults: Recommendation from the American College of Sports Medicine and the American Heart Association. Circulation, 116(9), 1094–1105. [DOI] [PubMed] [Google Scholar]
- Pedersen B. K., Saltin B. (2015). Exercise as medicine: Evidence for prescribing exercise as therapy in 26 different chronic diseases. Scandinavian Journal of Medicine & Science in Sports, 25(Suppl. 3), 1–72. 10.1111/sms.12581 [DOI] [PubMed] [Google Scholar]
- Rikli R. E., Jones C. J. (1999). Functional fitness normative scores for community-residing older adults, ages 60-94. Journal of Aging and Physical Activity, 7, 162–181. [Google Scholar]
- Veterans Health Administration and Department of Defense. (2017). VA/DoD Clinical Practice Guideline for the Management of Major Depressive Disorder. Retrieved September 20, 2019, from https://www.healthquality.va.gov/guidelines/MH/mdd/VADoDMDDCPGFINAL82916.pdf
- Vina J., Sanchis-Gomar F., Martinez-Bello V., Gomez-Cabrera M. C. (2012). Exercise acts as a drug; the pharmacological benefits of exercise. British Journal of Pharmacology, 167(1), 1–12. 10.1111/j.1476-5381.2012.01970.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wee C. C., McCarthy E. P., Davis R. B., Phillips R. S. (1999). Physician counseling about exercise. JAMA, 282(16), 1583–1588. 10.1001/jama.282.16.1583 [DOI] [PubMed] [Google Scholar]
- Whelton P. K., Carey R. M., Aronow W. S., Casey D. E., Jr., Collins K. J., Dennison Himmelfarb C., DePalma S. M., Gidding S., Jamerson K. A., Jones D. W., MacLaughlin E. J., Muntner P., Ovbiagele B., Smith S. C., Jr, Spencer C. C., Stafford R. S., Taler S. J., Thomas R. J., Williams K. A., Sr., Williamson J. D., Wright J. T., Jr. (2018). 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation, 138(17), e484–e594. 10.1161/cir.0000000000000596 [DOI] [PubMed] [Google Scholar]
- Williams P. T., Franklin B. (2007). Vigorous exercise and diabetic, hypertensive, and hypercholesterolemia medication use. Medicine & Science in Sports & Exercise, 39(11), 1933-1941. 10.1249/mss.0b013e318145b337 [DOI] [PMC free article] [PubMed] [Google Scholar]