Abstract
Objectives
To compare the effectiveness and safety of the Braidin® slender 7 Fr sheath with a standard 6 Fr sheath for treating left main bifurcation disease.
Methods
From January 2017 to March 2019, 277 patients with left main bifurcation disease who underwent the transradial approach for percutaneous coronary intervention were divided into the slender 7 Fr sheath group (Braidin® slender 7 Fr sheath, n = 154) and standard 6 Fr sheath group (n = 123). Pathological features, surgical effect, and complications were evaluated.
Results
The rate of using the classic crush technique was significantly higher in the slender 7 Fr sheath group than in the standard 6 Fr sheath group. The slender 7 Fr sheath group had a significantly shorter operation time than the standard 6 Fr sheath group. There were no significant differences in the radial artery occlusion rate after surgery and at 1 month of follow-up between the groups. Multivariate logistic regression analysis showed that 6 Fr and Braidin slender 7 Fr sheaths did not predict radial artery occlusion.
Conclusion
The Braidin slender 7 Fr sheath has a superior operative process and similar safety for the radial artery as that of the standard 6 Fr sheath for treating left main bifurcation disease.
Keywords: Left main bifurcation, Braidin® slender 7 Fr sheath, two-stent technology, transradial artery, percutaneous coronary intervention, major adverse cardiocerebrovascular events, radial artery occlusion
Introduction
With development of interventional technology, the safety and feasibility of transradial coronary intervention have been confirmed in clinical trials. These trials have shown that transradial coronary intervention has the advantages of less bleeding, faster recovery, lower complications, and the surgical outcome is comparable with transfemoral coronary intervention.1
Left main bifurcation disease (LM bifurcation) is a difficult and high-risk disease in interventional treatment during which a standard 6 Fr sheath is commonly used.2 However, some complex bifurcation lesions often require two-stent technology during treatment,3 and sometimes, large-sized guiding is required as support during interventional treatment. For such complex lesions, transfemoral coronary intervention with a standard 7 Fr sheath is often used. However, transfemoral coronary intervention is characterized by a high risk of bleeding and difficulty in compressing hemostasis.4 The inner diameter (ID) of the radial artery is relatively small, and transradial coronary intervention with a standard 7 Fr sheath can cause greater damage compared with transradial coronary intervention with a 6 Fr sheath.
In recent years, the transradial Braidin® slender 7 Fr sheath, which was independently developed in China, has increased in use with continuous development of interventional techniques. The outer diameter (2.72 mm) of the Braidin slender 7 Fr sheath is equivalent to that of a standard 6 Fr sheath. Additionally, the ID (2.46 mm) of the Braidin slender 7 Fr sheath is equivalent to that of a standard 7 Fr sheath, which has less damage to blood vessels. The Braidin slender 7 Fr sheath is compatible with 7 Fr guiding. A previous study showed use of the Terumo slender 7 Fr sheath (GSS) in interventional therapy.5 However, no studies have evaluated application of the Braidin slender 7 Fr sheath in interventional treatment. Therefore, this study aimed to examine the effectiveness and safety of the Braidin slender 7 Fr sheath compared with the traditional standard 6 Fr sheath for treating LM bifurcation.
Materials and methods
Study population
From January 2017 to March 2019, patients with LM bifurcation who underwent the transradial approach for percutaneous coronary intervention (PCI) from two heart centers (Cangzhou Central Hospital and Beijing Anzhen Hospital, Capital Medical University) were retrospectively included in our study in a consecutive manner. Patients were divided into two groups on the basis of the size of the radial arterial sheath as follows: the slender 7 Fr sheath group and the standard 6 Fr sheath group. This study was approved by the ethics committees of Beijing Anzhen Hospital and Cangzhou Central Hospital. All patients signed informed consent.
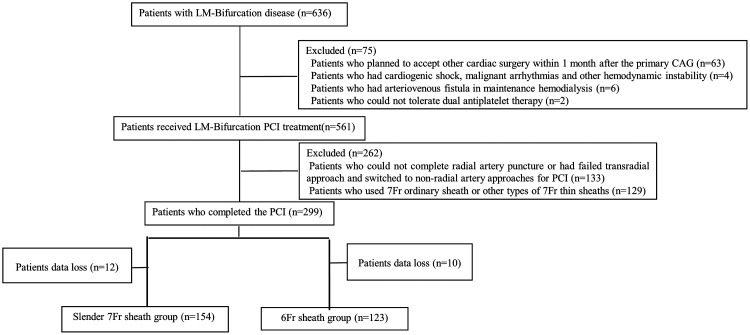
Inclusion criteria were patients who were diagnosed with LM bifurcation by coronary angiography and received LM-PCI treatment at the two centers. Standardized surgical procedures, including single stent technology, double stent technology, the crush technique, and the culotte technique, in LM-PCI were used in the two centers. Exclusion criteria were as follows: 1) patients who planned to accept other cardiac surgery within 1 month after the primary coronary angiography; 2) patients who had preoperative cardiogenic shock, malignant arrhythmias, or other types of hemodynamic instability; 3) patients who had arteriovenous fistula in maintenance hemodialysis; 4) patients who could not tolerate anticoagulation and antiplatelet therapy; 5) patients who could not complete radial artery puncture or had failed the transradial approach and switched to a non-radial artery approach for PCI; 6) patients who used a 7 Fr ordinary sheath or other types of 7 Fr thin sheaths; and 7) patients with lost data. A flow diagram of this study is shown in Figure 1.
Figure 1.
Flow diagram of selection of the patients.
LM, left main; CAG, coronary angiography; PCI, percutaneous coronary intervention.
Description of the sheaths
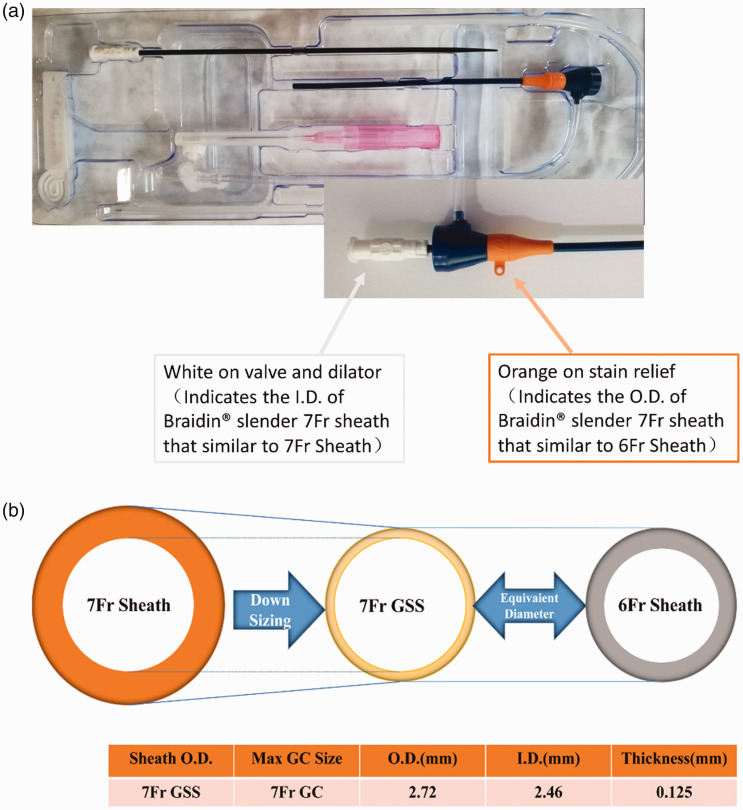
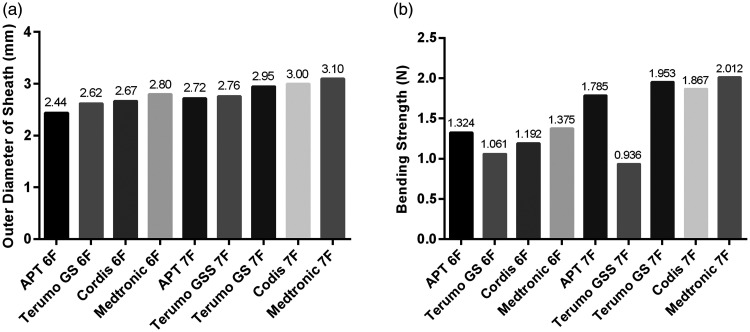
The Braidin slender 7 Fr sheath (Advanced Polymer and Titanium Medical, Xiangxiang, China) was used in the slender 7 Fr sheath group for the transradial approach in PCI. The wall thickness of this sheath is 0.125 mm, which is only half of the wall thickness of a conventional 7 Fr sheath. The ID of the Braidin slender 7 Fr sheath is 2.46 mm (0.097″), which is compatible with a 7 Fr guiding catheter. The inner wall of the sheath tube has a hydrophilic coating, which guarantees a smooth passage of the 7 Fr guiding catheter. The outer diameter (OD) of the Braidin slender 7 Fr sheath is 2.72 mm, which is similar to the commonly used 6 Fr interventional sheath, with an OD of 2.62 mm (Figure 2a and 2b). The OD of a conventional 7 Fr sheath is 2.95 mm. The ODs of sheaths from different manufacturers are shown in Figure 3a.
Figure 2.
a). Measurement method of the OD of the Braidin slender 7 Fr sheath and standard 6 Fr sheath. b). Diagram of the OD of a conventional 7 Fr sheath, the 7 Fr GSS (Terumo), and a 6 Fr sheath
OD, outer diameter; ID, inner diameter.
Figure 3.
The a) outer diameter and b) bending strength of sheaths from different manufacturers.
The sheath wall of the Braidin slender 7 Fr sheath has a three-layer tubular body structure reinforced by a steel wire mesh, with a bending strength of 1.324 N, which is stronger than other products (Figure 3b). The distal end of this sheath has a hydrophilic coating to reduce friction with the skin, while the operator’s holding section does not have this coating to reduce slippage and facilitate the operation.
Transradial approach for PCI
All patients were provided aspirin (Bayer HealthCare Manufacturing S.r.l., Berkley, CA, USA) 100 mg once daily and clopidogrel bisulfate (Sanofi Winthrop Industrie, Paris, France) 75 mg once daily orally for 3 days before surgery. A preoperative routine auxiliary examination and cardiovascular risk factor assessment were completed.
All patients underwent the transradial approach for PCI after adequate local anesthesia with 2% lidocaine hydrochloride. Application of a slender 7 Fr sheath or standard 6 Fr sheath was determined on the basis of the characteristics of the disease and the preference of the operator. After insertion of the sheath (slender 7 Fr sheath or 6 F sheath), all patients were administered 3000 IU heparin (Tianjin Biochemical Pharmacy, Tianjin, China) in the sheath at the beginning of the angiography, and adjunctive heparin was provided during PCI if required (100 IU/kg of body weight). The use of intravascular ultrasound and an intra-aortic balloon pump depended on the patient’s condition and discretion of the operator. All patients were oppressed by a disposable radial hemostatic device (Terumo TR Band; Terumo Corp., Tokyo, Japan), during which the hemostatic device was gradually decompressed and hemostasis was finally completed. After hemostasis was completed, all patients were diagnosed by palpation of radial artery pulsation and ultrasound to determine the patency of the radial artery. All patients received dual antiplatelet therapy with aspirin 100 mg once daily and clopidogrel bisulfate 75 mg once daily if there were no obvious bleeding events and contraindications after the operation. The use of other cardiovascular system drugs, including β-inhibitors and angiotensin-converting enzyme inhibitors, was determined on the basis of the clinical situation of the patients.
Definitions
Successful hemostasis of the radial artery was defined as when the hemostatic device could be successfully removed within 6 hours after surgery. The Medina classification method was used for description of lesion classification in this study.6 The total kissing balloon diameter was defined as the sum of the diameters of kissing balloons during the operation of the two-stent technology. The proximal optimization technique was defined as use of a short balloon with a larger diameter to dilate the proximal main branch of the bifurcation lesion.7
Definite thrombosis was defined as stent thrombosis confirmed by angiography and the patient met the diagnostic criteria for acute myocardial infarction, or there was pathological evidence of stent thrombosis, which was confirmed after a recent autopsy or salvage thrombosis. Probable thrombosis was defined as unexplained death within 30 days after PCI or any myocardial infarction that was related to documented acute ischemia in the territory of the implanted stent without angiographic confirmation of stent thrombosis and in the absence of any other obvious cause.8 Major adverse cardiocerebrovascular events (MACCE) were defined as the sum of all-cause death, myocardial infarction, cerebral infarction, and any form of revascularization.8
Transradial artery spasm was defined as the inability to manipulate guidewires and catheters smoothly and painlessly or to remove the interventional sheath in the same way at the end of the procedure.9 Vascular access-site complications were defined as any documented vascular damage and included perforations, arterial dissection, pseudoaneurysm, complications requiring surgical intervention, and moderate to severe (grade II) local hematomas. Local hematoma was classified according to the Early Discharge after Transradial Stenting of Coronary Arteries standard as follows: Class I, hematoma diameter ≤5 cm; Class II, hematoma diameter ≤10 cm; Class III, >10 cm, but not above the elbow; Class IV, extending above the elbow; and Class V, anywhere with ischemic threat of the hand.10 The pain score was classified according to Aminian et al.11 as follows: the amount of pain when the sheath was removed was none (score = 1), slight (score = 2), moderate (score = 3), or extreme (score = 4). Sheath failure was defined as vascular complications and failure of the surgical procedure caused by any device deformity. Radial artery occlusion (RAO) was defined as the absence of a radial pulse assessed clinically together with the absence of flow as assessed by a Doppler ultrasound examination of the radial artery.12 Angiographic success was defined as that after completion of PCI, a Thrombolysis in Myocardial Infarction blood flow level of 3 with final residual stenosis <20%, and there was no death, myocardial infarction, emergency bypass, or other adverse events before discharge.
Follow-up and clinical evaluation
Ultrasound examination of the radial artery at a 1-month follow-up was performed in all patients. Patients could revisit at any time when they had symptoms or had evidence of myocardial ischemia. The rates of in-hospital and 1-month MACCE, in-hospital and 1-month definite stent thrombosis, and in-hospital and 1-month probable stent thrombosis were measured. Four patients were lost to follow-up.
Statistical analysis
All analyses were performed using SPSS version 24.0 software (IBM Corp., Armonk, NY, USA). Categorical variables were compared by the chi-square test or Fisher’s exact test and values are shown as number (percentage). Quantitative variables are shown as mean ± standard deviation. Normally distributed data were compared by the t test or analysis of variance and variables with a skewed distribution were compared by the Wilcoxon rank-sum test. A two-tailed probability value of P < 0.05 was considered as statistically significant.
Results
We included 277 patients with LM bifurcation undergoing the transradial approach for PCI (n = 145 in Cangzhou Central Hospital and n = 132 in Beijing Anzhen Hospital, Capital Medical University). There were 154 patients in the slender 7 Fr sheath group and 123 patients in the standard 6 Fr sheath group. There were no significant differences in age, sex, heparin dosage, glomerular filtration rate, and other baseline data between the two groups (Table 1).
Table 1.
Baseline characteristics of the two groups.
| Slender 7 Fr sheath group (n = 154) | 6 Fr sheath group (n = 123) | P value | |
|---|---|---|---|
| Age (years) | 61.83 ± 10.64 | 60.64 ± 13.53 | 0.429 |
| Male sex (n, %) | 105 (68.2) | 75 (61) | 0.212 |
| Height (m) | 1.68 ± 0.08 | 1.69 ± 0.09 | 0.401 |
| Weight (kg) | 71.92 ± 10.06 | 71.15 ± 12.19 | 0.578 |
| BMI (kg/m2) | 25.44 ± 2.78 | 24.84 ± 2.97 | 0.083 |
| Hypertension (n, %) | 76 (49.4) | 54 (43.9) | 0.367 |
| Diabetes mellitus (n, %) | 48 (31.2) | 29 (23.6) | 0.161 |
| Dyslipidemia (n, %) | 25 (16.2) | 30 (24.4) | 0.091 |
| Current smoking (n, %) | 35 (22.7) | 36 (29.3) | 0.215 |
| Previous MI (n, %) | 27 (17.5) | 15 (12.2) | 0.218 |
| Previous PCI (n, %) | 49 (31.8) | 29 (23.6) | 0.130 |
| Previous CABG (n, %) | 3 (1.9) | 3 (2.4) | 1.000 |
| Previous stroke (n, %) | 7 (4.5) | 10 (8.1) | 0.217 |
| Previous homolateral radial access (n, %) | 75 (48.7) | 54 (43.9) | 0.426 |
| Peripheral artery disease (n, %) | 5 (3.2) | 10 (8.1) | 0.074 |
| Heparin (IU) | 10191.56 ± 1006.25 | 10115.45 ± 1219.18 | 0.578 |
| Aspirin (n, %) | 154 (100) | 123 (100) | NS |
| P2Y12 inhibitor (n, %) | 154 (100) | 123 (100) | NS |
| Successful radial artery hemostasis (n, %) | 132 (85.7) | 105 (85.4) | 0.935 |
| Creatinine | 69.53 ± 20.62 | 65.97 ± 13.26 | 0.098 |
| GFR (mL/min/1.73 m2) | 87.69 ± 23.38 | 89.79 ± 21.40 | 0.439 |
| LVEF | 61.37 ± 6.55 | 62.89 ± 7.28 | 0.068 |
Values are mean ± standard deviation or n (%).
BMI, body mass index; MI, myocardial infarction; PCI, percutaneous coronary intervention; CABG, coronary artery bypass grafting; GFR, glomerular filtration rate; LVEF, left ventricular ejection fraction.
Pathological features and surgical effect
The slender 7 Fr sheath group had a significantly higher mean Synergy between Percutaneous Coronary Intervention with Taxus and Cardiac Surgery (SYNTAX) score than the standard 6 Fr sheath group (P < 0.01, Table 2). The number of patients with Medina classification of 1,1,1 in the slender 7 Fr sheath group was significantly higher than that in the standard 6 Fr sheath group (P = 0.001). The number of patients with LM bifurcation combined with multiple-vessel disease in the slender 7 Fr sheath group was significantly higher than that in the standard 6 Fr sheath group (P = 0.004).
Table 2.
Pathological features and surgical effect of the two groups.
| Slender 7 Fr sheath group (n = 154) | 6 Fr sheath group (n = 123) | P value | |
|---|---|---|---|
| SYNTAX score | 28.66 ± 5.35 | 26.20 ± 4.81 | <0.001 |
| Medina classification (n, %) | |||
| 1,1,1 (%) | 73 (47.4) | 34 (27.6) | 0.001 |
| 0,1,1 (%) | 13 (8.4) | 16 (13) | 0.217 |
| 1,0,1 (%) | 36 (23.4) | 29 (23.6) | 0.969 |
| 1,1,0 (%) | 32 (20.8) | 44 (35.8) | 0.005 |
| LM bifurcation (n, %) | |||
| LM without other vessel disease | 16 (10.4) | 29 (23.6) | 0.003 |
| LM with single-vessel disease | 32 (20.8) | 30 (24.4) | 0.474 |
| LM with multiple-vessel disease | 106 (68.8) | 64 (52) | 0.004 |
| Maximal used catheter size (n, %) | |||
| 6 | 15 (9.7) | 123 (100) | <0.001 |
| 7 | 139 (90.3) | 0 (0) | <0.001 |
| Number of catheters used (n, %) | |||
| 1 | 146 (94.8) | 111 (90.2) | 0.145 |
| 2 | 8 (5.2) | 12 (9.8) | 0.145 |
| ≥3 | 0 (0) | 0 (0) | – |
| LM stent techniques (n, %) | |||
| One-stent | 70 (45.5) | 56 (45.5) | 0.990 |
| One-stent with final kissing | 43 (27.9) | 34 (27.6) | 0.959 |
| One-stent without final kissing | 27 (17.5) | 22 (17.9) | 0.939 |
| Two-stent | 84 (54.5) | 67 (54.5) | 0.990 |
| Main vessel stent diameter(mm) | 3.55 ± 0.37 | 3.07 ± 0.29 | <0.01 |
| Side branch stent diameter (mm) | 3.13 ± 0.43 | 2.63 ± 0.22 | <0.01 |
| Total kissing balloon diameter (mm) | 6.66 ± 0.64 | 5.81 ± 0.44 | <0.01 |
| Final kissing balloon (n, %) | 115 (74.7) | 101 (82.1) | 0.138 |
| Crush technique (including DK crush, step crush) (n, %) | 57 (37) | 32 (26) | 0.051 |
| Classical crush technique (n, %) | 38 (66.7) | 0 (0) | <0.001 |
| Cullote technique (n, %) | 17 (11) | 22 (17.9) | 0.104 |
| T typing (n, %) | 7 (4.5) | 13 (10.6) | 0.054 |
| SKS (n, %) | 3 (1.9) | 0 (0) | 0.257 |
| POT technique (n, %) | 93 (60.4) | 52 (42.3) | 0.003 |
| IVUS (n, %) | 23 (14.9) | 20 (16.3) | 0.762 |
| IABP (n, %) | 3 (1.9) | 1 (0.8) | 0.632 |
| Operation time (minutes) | 68.18 ± 33.66 | 77.55 ± 26.45 | 0.010 |
| Contrast volume (mL) | 179.68 ± 58.54 | 175.04 ± 59.66 | 0.516 |
| Total radiation dose (mGy) | 3344.93 ± 1942.43 | 3409.09 ± 972.00 | 0.721 |
Values are mean ± standard deviation or n (%).
SYNTAX, Synergy between Percutaneous Coronary Intervention with Taxus and Cardiac Surgery; LM, left main; DK, double kissing; SKS, simultaneous kissing stenting; POT, proximal optimization technique; IVUS, intravascular ultrasound; IABP, intra-aortic balloon pump.
With regard to surgical techniques, there were no significant differences in the number of patients who received one-stent technology and two-stent technology between the two groups. Among the patients who received two-stent technology, the mean main vessel stent diameter in the slender 7 Fr sheath group was significantly larger than that in the standard 6 Fr sheath group (P < 0.01). Similarly, the mean side branch stent diameter in the slender 7 Fr sheath group was significantly larger than that in the standard 6 Fr sheath group (P < 0.01). The mean total kissing balloon diameter in the slender 7 Fr sheath group was significantly larger than that in the standard 6 Fr sheath group (P < 0.01).
The rate of using the classic crush technique in the slender 7 Fr sheath group was significantly higher than that in the standard 6 Fr sheath group (P < 0.001). The proximal optimization technique was used in significantly more patients in the slender 7 Fr sheath group than in the standard 6 Fr sheath group (P = 0.003). Three cases of simultaneous kissing stenting technology were completed in the slender 7 Fr sheath group, while there were no cases in the standard 6 Fr sheath group.
The slender 7 Fr sheath group had a significantly shorter operation time than the standard 6 Fr sheath group (P = 0.010). There were no significant differences in the contrast volume and total radiation dose between the two groups (Table 2).
Clinical effect
There was no significant difference in the angiographic success rate between the two groups of patients (Table 3). There were no significant differences in the in-hospital MACCE and 1-month MACCE rates between the two groups. There were no significant differences in the in-hospital definite stent thrombosis and 1-month definite stent-thrombosis rates between the two groups. No significant differences were observed in the in-hospital probable stent thrombosis and 1-month probable stent thrombosis rates between the two groups.
Table 3.
Comparison of the clinical effect between the two groups.
| Slender 7 Fr sheath group (n = 154) | 6 Fr sheath group(n = 123) | P value | |
|---|---|---|---|
| Angiographic success (n, %) | 152 (98.7) | 121 (98.4) | 1.000 |
| In-hospital MACCE (n, %) | 1 (0.6) | 1 (0.8) | 1.000 |
| In-hospital stent-thrombosis (n, %) | |||
| Definite | 1 (0.6) | 1 (0.8) | 1.000 |
| Probable | 0 (0) | 0 (0) | – |
| One-month MACCE (n, %) | 3 (1.9) | 4 (3.3) | 0.704 |
| One-month stent thrombosis (n, %) | |||
| Definite | 1 (0.6) | 1 (0.8) | 1.000 |
| Probable | 0 (0) | 2 (1.6) | 0.196 |
MACCE, major adverse cardiocerebrovascular events.
Complications of the radial artery
There were no significant differences in complications, including transradial artery spasm, vascular access site complications, local hematoma, the pain score, arteriovenous fistulas, and sheath bending, between the two groups (Table 4). The RAO rate in the slender 7 Fr sheath group appeared to be higher than that in the standard 6 Fr sheath group, but there was no significant difference. Similarly, the RAO rate at 1 month of follow-up in the slender 7 Fr sheath group appeared to be higher than that in the standard 6 Fr sheath group, but this was not significant.
Table 4.
Complications of the radial artery between the two groups.
| Complications (n, %) | Slender 7 Fr sheath group (n = 154) | 6 Fr sheath group (n = 123) | P value |
|---|---|---|---|
| Transradial artery spasm | 13 (8.4) | 9 (7.3) | 0.731 |
| Vascular access-site complications | 12 (7.8) | 10 (8.1) | 0.918 |
| Hematoma | |||
| No hematoma | 131 (85.1) | 105 (85.4) | 0.944 |
| Local hematoma | 23 (14.9) | 18 (14.6) | 0.944 |
| Type I | 16 (10.4) | 12 (9.8) | 0.862 |
| ≥Type II | 7 (4.5) | 6 (4.9) | 0.897 |
| Pain score | |||
| None | 50 (32.5) | 52 (42.3) | 0.093 |
| Slight | 63 (40.9) | 45 (36.6) | 0.464 |
| Moderate | 33 (21.4) | 20 (16.3) | 0.277 |
| Extreme | 8 (5.2) | 6 (4.9) | 0.905 |
| Arteriovenous fistula | 2 (1.3) | 1 (0.8) | 1 |
| Sheath bending | 1 (0.6) | 4 (3.3) | 0.175 |
| Sheath failure | 1 (0.6) | 4 (3.3) | 0.175 |
| RAO | 10 (6.5) | 7 (5.7) | 0.782 |
| RAO at 1 month of follow-up | 9 (5.8) | 6 (4.9) | 0.724 |
RAO, radial artery occlusion.
We further analyzed effects of the 6 Fr sheath and slender 7 Fr sheath on the RAO rate. In multivariate analysis, we adjusted for factors, including sex, previous homolateral radial access, successful hemostasis, spasm, vascular access site complications, diabetes mellitus, pain during the procedure, and local hematoma, to study the effects of the 6 Fr sheath and slender 7 Fr sheath on the RAO rate. Multivariate logistic regression analysis showed that the 6 Fr sheath and slender 7 Fr sheath were not predictors of the RAO rate (Table 5).
Table 5.
Effects of the 6 Fr sheath and slender 7 Fr sheath on the RAO rate.
| RAO (n, %) |
Univariate analysis |
Multivariate analysis |
||||||
|---|---|---|---|---|---|---|---|---|
| Yes (15, 5.4) | No (262, 94.6) | Odds ratio | P value | 95% CI | Odds ratio | P value | 95% CI | |
| 6 Fr sheath | 6 (4.9) | 117 (95.1) | Reference | – | – | Reference | – | – |
| Slender 7 Fr sheath | 9 (5.8) | 145 (94.2) | 1.210 | 0.724 | 0.419–3.498 | 1.789 | 0.365 | 0.509–6.294 |
RAO, radial artery occlusion; CI, confidence interval.
Discussion
In this study, we found that the slender 7 Fr sheath group was equivalent to the standard 6 Fr sheath group regarding the surgical effect of LM bifurcation lesions (i.e., angiological success, in-hospital MACCE, and in-hospital stent thrombosis), and the slender 7 Fr sheath group had a better operative process and shorter surgical time. Additionally, the slender 7 Fr sheath group had a significantly higher SYNTAX score than the standard 6 Fr sheath group. There was no significant difference in the RAO rate after surgery and after 1 month of follow-up between the two groups, which indicated that the slender 7 Fr sheath group had as good safety of the radial artery as that in the standard 6 Fr sheath group.
The RAO rate in the slender 7 Fr sheath group (6.5%) in our study is similar to that of a study by Rashid et al.13 (7.69%) in which transradial coronary intervention was used. Additionally, the RAO rate in the slender 7 Fr sheath group in our study is similar to that of the standard 6 Fr sheath in Batchelor et al.’s study (5.3%).14 We speculate that the similar OD of the sheath tube may be the reason for this similarity between studies. The RAO rate after 1 month of follow-up of the two groups in our study is similar to that of the standard 6 Fr sheath in studies by Batchelor et al.15 and Hahalis et al.16 This finding indicated that the slender 7 Fr sheath did not increase the RAO rate compared with the standard 6 Fr sheath, which is commonly used for treating LM bifurcation. The incidence of transradial artery spasm (8.4%) in the slender 7 Fr sheath group in our study is lower than that of the Tremuo slender 7 Fr sheath used in Aminian et al.’s study.5 This difference between studies may be attributed to the smaller OD of the slender 7 Fr sheath. Additionally, there were no significant differences in the rates of RAO, transradial artery spasm, local hematoma, and vascular access site complications between the two groups in our study. All of these results preliminarily confirm the safety of the radial artery using the slender 7 Fr sheath for the transradial approach for PCI.
The SYNTAX score is important for evaluating the short-term surgical effect and long-term prognosis of LM-PCI, and LM-PCI can achieve a similar effect as coronary artery bypass grafting for patients with a low (≤22) and moderate (22–32) SYNTAX score.17 Therefore, LM-PCI was used in patients of this study, with a mean SYNTAX score of 27.57 ± 5.26. The slender 7 Fr sheath group had a significantly higher SYNTAX score, a larger number of patients had a Medina classification of 1,1,1, and a larger number of patients with LM bifurcation combined with multiple-vessel disease compared with the standard 6 Fr sheath group. A slender 7 Fr sheath combined with 7 Fr guiding is preferred for these patients because the high support force of 7 Fr guiding can complete release of the stent and final kissing balloon dilatation safely and quickly.18
In the current study, no significant difference was found in the number of patients who received two-stent technology between the two groups. However, the main vessel stent diameter and total kissing balloon diameter of patients who received two-stent technology in the slender 7 Fr sheath group were significantly larger than those in the standard 6 Fr sheath group. The reason for this finding may be because 7 Fr guiding can complete the large-caliber (two 3.5-mm or more balloons) kissing technology owing to its higher supporting force and ID than 6 F guiding. Three cases of SKS technology were completed in the slender 7 Fr sheath group, while there were no cases in the standard 6 Fr sheath group. This is because 6 Fr guiding could not complete simultaneous release of the main and branch stents.
With regard to the surgical technique, the rate of using the classic crush technique in the slender 7 Fr sheath group was significantly higher than that in the standard 6 Fr sheath group. The reason for this finding is because classic crush technology cannot be completed by 6 F guiding, while the slender 7 Fr sheath allows implementation of 7 Fr guiding and further classic crush technology, which might lead to more surgical options for LM bifurcation. Furthermore, classic crush technology can reduce the re-wire number of guidewires, optimize the surgical procedure, reduce the left main ischemic time, and reduce potential branch occlusion of step crush and double kissing crush due to frequent operations.3,19 Therefore, a slender 7 Fr sheath combined with 7 Fr guiding can provide crush technology with a greater advantage compared with 6 F guiding. In our study, there was no significant difference in angiographic success between the two groups, which is similar to the current success rate of studies on LM bifurcation lesions.20–22 The 1-month MACCE rates in the two groups in our study are similar to those in previous studies.2,23 The incidence of 1-month definite stent thrombosis and probable stent thrombosis in the two groups is also similar to that in previous studies.21 These results suggest that the slender 7 Fr sheath is effective for LM bifurcation lesions and can achieve good immediate surgical results.
The operation time in the slender 7 Fr sheath group was shorter than that in the standard 6 Fr sheath group, and shorter that of double kissing crush in a study by Chen et al.21 We speculate that this difference between studies may be because one-stent technology was performed in several cases in our study, which reduced the operation time. Additionally, the classic crush technique in patients in the slender 7 Fr sheath group could have reduced the number of re-wires and simplified the operation steps. However, no significant differences in the contrast volume and the total radiation dose were observed between the two groups, which is consistent with a study by Chen et al.1 This finding may due to the larger caliber (large imaging dose for each time) and short operation time of the slender 7 Fr sheath, and the smaller caliber (small imaging dose for each time) and long operation time of the standard 6 Fr sheath.
This study has some limitations. One of the limitations is that continuous observation of the arterial lumen area, intima–media thickness, and the remodeling process after injury of the radial artery were not evaluated. Additionally, the sample size was small. A large, randomized, controlled study should be carried out in the future to further investigate the long-term efficacy of the slender 7 Fr sheath.
Conclusion
The Braidin slender 7 Fr sheath is equivalent to the standard 6 Fr sheath regarding the surgical effect of LM bifurcation lesions. Additionally, the Braidin slender 7 Fr sheath optimizes the operative process and shortens the surgical time. There are no significant differences in the RAO rate after surgery and after 1 month of follow-up between the two types of sheaths. This indicates that the slender 7 Fr sheath has as good safety for the radial artery as that for the standard 6 Fr sheath.
Declaration of conflicting interest
The authors declare that there is no conflict of interest.
Funding
This work was supported by grants from the National Key Research and Development Program of China (2017YFC0908800), Beijing Municipal Administration of Hospitals’ Ascent Plan (DFL20150601) and Mission plan (SML20180601), and Beijing Municipal Health Commission “Project of Science and Technology Innovation Center” (PXM2019_026272_000006, PXM2019_026272_000005).
ORCID iD
Yujie Zhou https://orcid.org/0000-0002-9545-1984
References
- 1.Chen S, Redfors B, Liu Y, et al. Radial versus femoral artery access in patients undergoing PCI for left main coronary artery disease: analysis from the EXCEL trial. EuroIntervention 2018; 14: 1104–1111. DOI: 10.4244/eij-d-18-00711. [DOI] [PubMed] [Google Scholar]
- 2.Stone GW, Kappetein AP, Sabik JF, et al. Five-Year Outcomes after PCI or CABG for Left Main Coronary Disease. N Engl J Med 2019; 381: 1820–1830. DOI: 10.1056/NEJMoa1909406. [DOI] [PubMed] [Google Scholar]
- 3.Gao Z, Xu B, Yang Y, et al. Comparison between one-stent versus two-stent technique for treatment of left main bifurcation lesions: A large single-center data. Catheter Cardiovasc Interv 2015; 85: 1132–1138. DOI: 10.1002/ccd.25849. [DOI] [PubMed] [Google Scholar]
- 4.Romagnoli E, Biondi-Zoccai G, Sciahbasi A, et al. Radial versus femoral randomized investigation in ST-segment elevation acute coronary syndrome: the RIFLE-STEACS (Radial Versus Femoral Randomized Investigation in ST-Elevation Acute Coronary Syndrome) study. J Am Coll Cardiol 2012; 60: 2481–2489. DOI: 10.1016/j.jacc.2012.06.017. [DOI] [PubMed] [Google Scholar]
- 5.Aminian A, Iglesias JF, Van Mieghem C, et al. First prospective multicenter experience with the 7 French Glidesheath slender for complex transradial coronary interventions. Catheter Cardiovasc Interv 2017; 89: 1014–1020. DOI: 10.1002/ccd.26773. [DOI] [PubMed] [Google Scholar]
- 6.Grundeken MJ, Collet C, Ishibashi Y, et al. Visual estimation versus different quantitative coronary angiography methods to assess lesion severity in bifurcation lesions. Catheter Cardiovasc Interv 2018; 91: 1263–1270. DOI: 10.1002/ccd.27243. [DOI] [PubMed] [Google Scholar]
- 7.Derimay F, Finet G, Souteyrand G, et al. Benefit of a new provisional stenting strategy, the re-proximal optimisation technique: the rePOT clinical study. EuroIntervention 2018; 14: e325–e332. DOI: 10.4244/eij-d-17-00941. [DOI] [PubMed] [Google Scholar]
- 8.Cutlip DE, Windecker S, Mehran R, et al. Clinical end points in coronary stent trials: a case for standardized definitions. Circulation 2007; 115: 2344–2351. DOI: 10.1161/circulationaha.106.685313. [DOI] [PubMed] [Google Scholar]
- 9.Kiemeneij F, Vajifdar BU, Eccleshall SC, et al. Measurement of radial artery spasm using an automatic pullback device. Catheter Cardiovasc Interv 2001; 54: 437–441. DOI: 10.1002/ccd.1307. [DOI] [PubMed] [Google Scholar]
- 10.Bertrand OF, De Larochelliere R, Rodes-Cabau J, et al. A randomized study comparing same-day home discharge and abciximab bolus only to overnight hospitalization and abciximab bolus and infusion after transradial coronary stent implantation. Circulation 2006; 114: 2636–2643. DOI: 10.1161/circulationaha.106.638627. [DOI] [PubMed] [Google Scholar]
- 11.Aminian A, Saito S, Takahashi A, et al. Comparison of a new slender 6 Fr sheath with a standard 5 Fr sheath for transradial coronary angiography and intervention: RAP and BEAT (Radial Artery Patency and Bleeding, Efficacy, Adverse evenT), a randomised multicentre trial. EuroIntervention 2017; 13: e549–e556. DOI: 10.4244/eij-d-16-00816. [DOI] [PubMed] [Google Scholar]
- 12.Garg N, Madan BK, Khanna R, et al. Incidence and predictors of radial artery occlusion after transradial coronary angioplasty: Doppler-guided follow-up study. J Invasive Cardiol 2015; 27: 106–112. [PubMed] [Google Scholar]
- 13.Rashid M, Kwok CS, Pancholy S, et al. Radial Artery Occlusion After Transradial Interventions: A Systematic Review and Meta-Analysis. J Am Heart Assoc 2016; 5: e002686. DOI: 10.1161/jaha.115.002686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Batchelor W, Dahya V, McGee D, et al. Ultrahigh-resolution ultrasound characterization of access site trauma and intimal hyperplasia following use of a 7F sheathless guide versus 6F sheath/guide combination for transradial artery PCI: Results of the PRAGMATIC trial. Am Heart J 2018; 198: 75–83. DOI: 10.1016/j.ahj.2017.11.017. [DOI] [PubMed] [Google Scholar]
- 15.Batchelor W, Dahya V, Tehrani B, et al. Radial artery remodeling following transradial percutaneous coronary intervention in men and women: insights from serial ultrahigh frequency ultrasonography. Cardiovasc Revasc Med 2019. DOI: 10.1016/j.carrev.2019.05.006. [DOI] [PubMed] [Google Scholar]
- 16.Hahalis G, Aznaouridis K, Tsigkas G, et al. Radial Artery and Ulnar Artery Occlusions Following Coronary Procedures and the Impact of Anticoagulation: ARTEMIS (Radial and Ulnar ARTEry Occlusion Meta-AnalysIS) Systematic Review and Meta-Analysis. J Am Heart Assoc 2017; 6: e005430. DOI: 10.1161/jaha.116.005430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Shlofmitz E, Genereux P, Chen S, et al. Left Main Coronary Artery Disease Revascularization According to the SYNTAX Score. Circ Cardiovasc Interv 2019; 12: e008007. DOI: 10.1161/circinterventions.118.008007. [DOI] [PubMed] [Google Scholar]
- 18.Burzotta F, Lassen JF, Banning AP, et al. Percutaneous coronary intervention in left main coronary artery disease: the 13th consensus document from the European Bifurcation Club. EuroIntervention 2018; 14: 112–120. DOI: 10.4244/eij-d-18-00357. [DOI] [PubMed] [Google Scholar]
- 19.Rab T, Sheiban I, Louvard Y, et al. Current Interventions for the Left Main Bifurcation. JACC Cardiovasc Interv 2017; 10: 849–865. DOI: 10.1016/j.jcin.2017.02.037. [DOI] [PubMed] [Google Scholar]
- 20.Chen SL, Sheiban I, Xu B, et al. Impact of the complexity of bifurcation lesions treated with drug-eluting stents: the DEFINITION study (Definitions and impact of complEx biFurcation lesIons on clinical outcomes after percutaNeous coronary IntervenTIOn using drug-eluting steNts). JACC Cardiovasc Interv 2014; 7: 1266–1276. DOI: 10.1016/j.jcin.2014.04.026. [DOI] [PubMed] [Google Scholar]
- 21.Chen SL, Zhang JJ, Han Y, et al. Double Kissing Crush Versus Provisional Stenting for Left Main Distal Bifurcation Lesions: DKCRUSH-V Randomized Trial. J Am Coll Cardiol 2017; 70: 2605–2617. DOI: 10.1016/j.jacc.2017.09.1066. [DOI] [PubMed] [Google Scholar]
- 22.Zhang J, Liu S, Geng T, et al. One-stent versus two-stent techniques for distal unprotected left main coronary artery bifurcation lesions. Int J Clin Exp Med 2015; 8: 14363–14370. [PMC free article] [PubMed] [Google Scholar]
- 23.Lee PH, Kwon O, Ahn JM, et al. Safety and Effectiveness of Second-Generation Drug-Eluting Stents in Patients With Left Main Coronary Artery Disease. J Am Coll Cardiol 2018; 71: 832–841. DOI: 10.1016/j.jacc.2017.12.032. [DOI] [PubMed] [Google Scholar]