Abstract
Introduction
We conducted a prospective study to find out change in limb length (lengthening/shortening) after total knee arthroplsty in unilateral and bilateral total knee arthroplasty (TKA) because few literature is available regarding limb length discrepancy in TKA in comparison to total hip arthroplasty. Limb length discrepancy (LLD) may lead to low back pain and gait abnormalities.
Material and methods
We divided 58 patients into two groups: Group A (28 patients) includes patients who underwent unilateral TKA and Group B (30 patients) includes patients who underwent bilateral TKA. We assessed the patients clinico-radiologically in terms of limb length (supine position), deformity, Sagital-flexion deformity/extensor lag, coronal - varus/valgus, range of motion, knee stability, patellar tracking and Hip-knee-ankle angle preoperatively and postoperatively.
Results
In group A, mean limb length difference (operated limb gained length as compared to unoperated limb) was 1.11 cm. Out of 22 patients (78%) in whom limb length discrepancy was present, only 7 patients (31%) having limb length discrepancy perceived it. In group B, mean limb length difference was 1.03 cm. Fourteen patients (47%) in group B had LLD but none of them perceived it. Clinically 22 patients (78%) in group A and 14 patients (47%) in group B had LLD. Radiologically 25 patients (89%) in group A and 22 patients (73%) in group B had LLD. Out of the 7 patients who perceived LLD, all had LLD radiologically too.
Conclusion
We reckoned that limb length discrepancy is more common in unilateral TKA. Limb length discrepancy of 2 cm or more is perceived by the patients operated for unilateral TKA. But in bilateral TKA, none of the patient perceived LLD because in this group LLD was less than 2 cm. Limb length discrepancy may leads to dissatisfaction of the patients and poor functional outcome.
Keywords: Limb length discrepancy, Total knee replacement, Clinico-radiological, Unilateral, Bilateral
1. Introduction
Limb length discrepancy (LLD) is quite common after total hip arthroplasty (THA) with incidence ranges from 1% to 27%.1 Mean LLD has been reported to vary from 3 mm to 17 mm after THA.2, 3, 4 Postoperatively, Change in limb length is not commonly seen in total knee arthroplasty (TKA), yet clinical outcome in some patients are suboptimal.5 Prosthetic malalignment, radiographic loosening and comorbidities are the reasons given for suboptimal results.6 One possible underlying variable is change in limb length. LLD after TKA is mostly due to lengthening of the operated limb.7, 8, 9 Severity of osteoarthritis and preoperative coronal plane deformity (varus/valgus) plays major role in postoperative limb length.5 LLD may lead to low back pain and gait abnormalities.10 LLD after TKA is one of the reasons for litigations against orthopaedic surgeons.11 The incidence of LLD after TKA has not been well documented in literature. So, we conducted a prospective study to find out change in limb length (lengthening/shortening) after TKA in unilateral and bilateral total knee arthroplasty.
2. Material and methods
The present prospective study was conducted from November 2015 to May 2019 after approval by institutional review board. We included all patients with severe degenerative primary osteoarthritis, failed conservative treatment, difficulty in walking, disturbance of daily routine activities due to pain/deformity (varus/valgus), patients with more than three months follow up and used midvastus approach in all. We excluded the patients with active infection, co-morbid conditions-psychiatric illness, rheumatoid arthritis, post traumatic secondary osteoarthritis, neuromuscular disorders, patient not motivated for physiotherapy, patient not ready to undergo life style modifications required after arthroplasty, patient with less than three months follow up. A total of 58 patients (23 males and 35 females) were included in this study. The mean age of the patient was 66.4 years. The 58 patients were divided into two groups. Group A (28 patients) includes patients who underwent unilateral TKA. Group B (30 patients) includes patients who underwent bilateral TKA. Patients with unilateral TKA did not go for bilateral TKA for reasons that were personal or financial.
Initial assessment of the patients was done regarding the severity of pain, deformity, swelling, any previous treatment. History of co-morbidities was taken and involvement of other joints was also ruled out. The preoperative assessment included limb length (supine position), deformity, Sagital-flexion deformity/extensor lag, coronal - varus/valgus, range of motion, knee stability, patellar tracking.
Baseline investigations and radiographs (X - ray both knee antero-posterior (AP) and lateral (standing), B/L scannogram, skyline view) was done for all patients. All the knees implanted were semi-constrained, fixed bearing, cemented implants. Bicompartmental knee arthroplasty was done; resurfacing of patella was not done. Same implant (Freedom, Maxx) was used in all patients to avoid any bias in observations. All the surgeries were performed by the senior author under tourniquet. An epidural catheter was used in all cases and kept it for 24 h postoperatively for pain relief. Jones bandage was applied postoperatively for four days. Postoperative rehabilitation included ankle physiotherapy and active straight leg raising (SLR) started next day. Flexion, muscle strengthening exercises and weight bearing started on first postoperative day. Wound inspection and removal of Jones bandage on fourth day. Staples removed after 2 weeks. Stairs climbing started within a week. Patient uses walker for 3–6 weeks and after that stick was advised. Patient allowed for unsupported walk after 8 weeks. Patients were followed up regularly in arthroplasty clinic at 6 weeks, 3 months, 6 months, 12 months and yearly.
Clinical assessment was done by limb length measurement. It was done in supine position. The pelvis was squared and the lower limb was kept parallel to the long axis of the body and both the limbs were in identical position. The limb length measurement (cm) was done from anterior superior illiac spine to medial malleolus using measuring tape. The measurement was taken twice and the mean value was taken. Stability and patellar tracking was also assessed clinically. Every patient was asked if he or she perceived any limb length discrepancy and the answer was recorded as ‘YES’ or ‘NO’.
Radiological assessment included measurement of limb length and hip-knee-ankle (HKA) angle from full length scanogram of both lower limbs in preoperative and postoperative period. In this study, Zero was considered neutral, negative values were given to valgus deformity and positive values to varus deformity. The femoral mechanical axis was obtained by joining centre of femoral head to the intercondylar notch. The tibial mechanical axis was obtained by joining the centre of tibial plateau to centre of tibial plafond. The HKA is defined as angle between these two axes. Limb length was measured from centre of femur head to centre of tibial plafond.
All statistical analysis was done using Microsoft office 2010. The calculation of averages and standard deviations (SD) was done using data analysis tool. The unpaired t-test was used for calculating P values of different categories.
3. Results
Demographics of the selected patients have been listed in Table 1. Varus deformity was more common. No patients with valgus deformity were present in our study.
Table 1.
Patients demographic.
| Parameter | Whole sample | Unilateral (varus/valgus) | Bilateral (varus/valgus) |
|---|---|---|---|
| Number of patients | 58 | 28/0 | 30/0 |
| Age | 64.5 | 64 | 65 |
| BMI | 30.85 | 30.69 | 31.02 |
| Female | 35 | 14 | 21 |
In group A (unilateral group), mean limb length difference (operated limb gained length as compared to unoperated limb) was 1.11 cm. Six patients (22%) had no change in length, 11 patients (39%) had increased length of 1 cm, 4 patients (14%) had increased length of 1.5 cm and 7 patients (25%) had increased length of 2 cm. Out of 22 patients (78%) in whom limb length discrepancy was present, only 7 patients (31%) having limb length discrepancy of 2 cm perceived it, and in these 7 patients, 4 patients complained it by themselves and 3 patients told on asking specifically about the change in limb length (Table 2, Table 3).
Table 2.
Data chart for Unilateral group (LLD and its perception)
| Patient | Pre op. limb length |
Post op. limb length |
LLD (cm) | Perception | ||
|---|---|---|---|---|---|---|
| Right (cm) | Left (cm) | Right (cm) | Left (cm) | |||
| 1 | 74 | 74 | 75 | 74 | 1 | No |
| 2 | 78 | 78 | 80 | 78 | 2 | Yes |
| 3 | 71 | 71 | 71 | 72 | 1 | No |
| 4 | 85.5 | 85.5 | 87 | 85.5 | 1.5 | No |
| 5 | 76 | 76 | 76 | 78 | 2 | Yes |
| 6 | 81 | 81 | 81 | 81 | 0 | No |
| 7 | 81 | 81 | 81 | 82 | 1 | No |
| 8 | 80 | 80 | 80 | 80 | 0 | No |
| 9 | 75 | 75 | 76 | 75 | 1 | No |
| 10 | 77 | 77 | 77 | 78.5 | 1.5 | No |
| 11 | 83 | 83 | 83 | 84.5 | 1.5 | No |
| 12 | 71 | 71 | 73 | 71 | 2 | Yes |
| 13 | 79 | 79 | 79 | 81 | 2 | Yes |
| 14 | 83 | 83 | 84 | 83 | 1 | No |
| 15 | 86 | 86 | 88 | 86 | 2 | Yes |
| 16 | 81 | 81 | 81 | 82 | 1 | No |
| 17 | 75 | 75 | 77 | 75 | 2 | Yes |
| 18 | 79 | 79 | 79 | 79 | 0 | No |
| 19 | 87 | 87 | 87 | 88 | 1 | No |
| 20 | 81 | 81 | 81 | 83 | 2 | Yes |
| 21 | 78 | 78 | 78 | 79 | 1 | No |
| 22 | 73 | 73 | 73 | 74.5 | 1.5 | No |
| 23 | 75 | 75 | 75 | 75 | 0 | No |
| 24 | 72 | 72 | 72 | 73 | 1 | No |
| 25 | 81 | 81 | 82 | 81 | 1 | No |
| 26 | 86 | 86 | 86 | 86 | 0 | No |
| 27 | 73 | 73 | 73 | 74 | 1 | No |
| 28 | 74 | 74 | 74 | 74 | 0 | No |
Table 3.
Data chart for Bilateral group (LLD and its perception).
| Patient | Pre. Op limb length |
Post. Op limb length |
LLD (cm) | Perception | ||
|---|---|---|---|---|---|---|
| Right, (cm) | Left (cm) | Right (cm) | Left (cm) | |||
| 1 | 78 | 78 | 78 | 78 | 0 | No |
| 2 | 79.5 | 79.5 | 80 | 80 | 0 | No |
| 3 | 86.5 | 86.5 | 87 | 87 | 0 | No |
| 4 | 78 | 78 | 78 | 78 | 0 | No |
| 5 | 87 | 87 | 87 | 87 | 0 | No |
| 6 | 77 | 77 | 77 | 78 | 1 | No |
| 7 | 80 | 80.5 | 81 | 81 | 0 | No |
| 8 | 83 | 83 | 83 | 84.5 | 1.5 | No |
| 9 | 83 | 83 | 83 | 84 | 1 | No |
| 10 | 85 | 85 | 86 | 85 | 1 | No |
| 11 | 85 | 85 | 86 | 85 | 1 | No |
| 12 | 74 | 74 | 74 | 74 | 0 | No |
| 13 | 75 | 75 | 75 | 75 | 0 | No |
| 14 | 78.5 | 78.5 | 79 | 79 | 0 | No |
| 15 | 88 | 88 | 89 | 88 | 1 | No |
| 16 | 78 | 78 | 78 | 79 | 1 | No |
| 17 | 82 | 82 | 82 | 82 | 0 | No |
| 18 | 75 | 75 | 75 | 76 | 1 | No |
| 19 | 82.5 | 82.5 | 83 | 83 | 0 | No |
| 20 | 79 | 79 | 79 | 80 | 1 | No |
| 21 | 89 | 89 | 89 | 89 | 0 | No |
| 22 | 77 | 77 | 77 | 78 | 1 | No |
| 23 | 73 | 73 | 73 | 73 | 0 | No |
| 24 | 83 | 83 | 83 | 84 | 1 | No |
| 25 | 85 | 85 | 85 | 86 | 1 | No |
| 26 | 78 | 77 | 78 | 77 | 1 | No |
| 27 | 86 | 86 | 86 | 87 | 1 | No |
| 28 | 77 | 77 | 77 | 77 | 0 | No |
| 29 | 82.5 | 82.5 | 83 | 83 | 0 | No |
| 30 | 80.5 | 80.5 | 81 | 81 | 0 | No |
In group B (bilateral group), mean limb length difference was 1.03 cm. Sixteen patients (53%) had no change in length, 13 patients (44%) had increased of 1 cm and 1 patient (3%) had increased length of 1.5 cm. None of the patients in this group perceived any change in their leg length (Table 3, Table 4).
Table 4.
Limb length discrepancy radiologically (LLD).
| Laterality | 0.1–1 cm | 1.1–2 cm | 2.1–3 cm |
|---|---|---|---|
| Group A | 16 | 9 | – |
| Group B | 21 | 1 | – |
Clinically 22 patients (78%) in group A and 14 patients (47%) in group B had LLD. Radiologically 25 patients (89%) in group A and 22 patients (73%) in group B had LLD. Of the 7 patients who perceived LLD, all had LLD radiologically too.
The average radiological increase in limb length was 1.02 cm in unilateral (group A) and 0.74 cm in bilateral (group B) patients (Table 7, Table 8).
Table 7.
Measurement results for group A (Unilateral).
| Parameter | Whole sample, Varus>0 Mean (SD) |
|---|---|
| Pre op. HKA | 10.60 (0.68) |
| Post op. HKA | −5.10 (0.54) |
| Change in alignment | −15.70 (3.96) |
| Lengthening, (cm) | 1.02 (0.54) |
| P value | 0.829 |
Table 8.
Radiological measurements for group B (Bilateral).
| Parameter | Whole sample, Varus>0 Mean (SD) |
|---|---|
| Pre op. HKA(R/L) | 10.40 (4.61)/14.80 (0.75) |
| Post op. HKA(R/L) | −5.50 (0.6)/−5.540 (0.47) |
| Change in alignment(R/L) | −16.010 (0.89)/−20.360 (0.97) |
| Lengthening, (cm) (R/L) | 0.74 (1.7) |
| P value | 0.862 |
The patients were also separated in two groups depending on their Kellgren and Lawrence (KL) grades. Those with severe deformity demonstrated average lengthening of 1.33 cm in group A and 0.77 cm in group B. Those with mild to moderate deformity showed average lengthening of 0.62 cm in group A and 0.69 cm in group B (Table 9). The limb length of these two groups were compared postoperatively and did not find to be significant (p > 0.5).
Table 9.
Measurement results grouped by preoperative Kellgren and Lawrence grade.
| Pre op. KL grade |
||
|---|---|---|
| 1 and 2 |
3 and 4 |
|
| Group A/Group B [R/L] Mean (SD) |
Group A/group B [R/L] Mean (SD) |
|
| Pre op. HKA | 10.770(1.8)/[10.10(0.97)/14.30(1.8)] | 10.40(1.9)/[10.60(2.3)/15.00(2.4)] |
| Post op. HKA | −5.250(1.3)/[-5.50(1.2)/-5.70(1.2)] | −5.00(1.97)/-[5.50(2.3)/-5.40(1.6)] |
| Change in alignment | −16.020(2.4)/[-15.60(1.7)/-19.70(1.9)] | −15.50(3.17)/[-16.10(3.2)/-22.50(8.8)] |
| Lengthening,(cm) | 0.62(0.5)/0.69(0.4) | 1.33(1.6)/0.77(1.7) |
| P value | 0.942/0.919 | 0.819/0.875 |
The mean pre-operative HKA was 10.6 in group A and 14.6/14.8 (R/L) in group B. The mean post-operative HKA was −5.1 in group A and −5.53/-5.54 (R/L) in group B. (Table 5, Table 6). None of the patients had flexion deformity/extensor lag exceeding 50
Table 5.
Data for unilateral group (HKA and polyethylene liner size)
| Patients | Pre op. HKA0 | Post op. HKA0 | Polyethylene liner size | Limb length discrepancy (LLD) cm | ||
| Operated knee(o) | ||||||
| Right | Left | Right | Left | |||
| 1 | 10.6(o) | 10.0 | −5.6 | 10.0 | 9 | 1 |
| 2 | 10.2(o) | 10.5 | −5.8 | 10.5 | 11 | 2 |
| 3 | 9.5 | 10(o) | 9.5 | −4.3 | 9 | 1 |
| 4 | 11.8(o) | 11 | −5.5 | 11 | 9 | 1.5 |
| 5 | 12.0 | 12.4(o) | 12 | −4.8 | 9 | 2 |
| 6 | 10 | 10.1(o) | 10 | −5.2 | 9 | 0 |
| 7 | 10.5 | 11(o) | 10.5 | −6.4 | 9 | 1 |
| 8 | 11.4(o) | 11 | −5.8 | 11 | 9 | 0 |
| 9 | 9.6(o) | 9.2 | −5.1 | 9.2 | 9 | 1 |
| 10 | 11.5 | 12(o) | 11.5 | −6.1 | 9 | 1.5 |
| 11 | 10 | 10.2(o) | 10 | −4.9 | 9 | 1.5 |
| 12 | 13(o) | 12.5 | −4.2 | 12.5 | 11 | 2 |
| 13 | 11.5 | 12(o) | 11.5 | −5.1 | 9 | 2 |
| 14 | 10.2(o) | 10 | −4.4 | 10 | 9 | 1 |
| 15 | 9.8(o) | 10 | −5.3 | 10 | 11 | 2 |
| 16 | 9.7 | 10.1(o) | 9.7 | −5.1 | 9 | 1 |
| 17 | 10.6(o) | 10.5 | −5.6 | 10.5 | 11 | 2 |
| 18 | 10.2(o) | 10.0 | −5.8 | 10 | 9 | 0 |
| 19 | 11 | 11.2(o) | 11 | −5.4 | 9 | 1 |
| 20 | 9.6 | 10(o) | 9.6 | −4.4 | 9 | 2 |
| 21 | 10.0 | 10.4(o) | 10 | −3.8 | 11 | 1 |
| 22 | 10.0 | 10.6(o) | 10 | −4.6 | 9 | 1.5 |
| 23 | 10.3(o) | 10 | −5.4 | 10 | 9 | 0 |
| 24 | 10 | 10.3(o) | 10 | −5.1 | 9 | 1 |
| 25 | 10.8(o) | 10.5 | −4.8 | 10.5 | 11 | 1 |
| 26 | 9.6(o) | 9.5 | −5.0 | 9.5 | 9 | 0 |
| 27 | 10.5 | 10.6(o) | 10.5 | −5.4 | 9 | 1 |
| 28 | 10.3(o) | 10 | −5.2 | 10 | 9 | 0 |
Table 6.
Data for Bilateral group (HKA and polyethylene liner size)
| Patients | Pre op. HKA0 |
Post op. HKA0 |
Polyethylene liner |
Limb length discrepancy (LLD) cm | |||
|---|---|---|---|---|---|---|---|
| Right | Left | Right | Left | Right | Left | ||
| 1 | 12.5 | 12.8 | −5.4 | −6 | 9 | 9 | 0 |
| 2 | 16 | 16.4 | −6.1 | −5.8 | 11 | 9 | 0 |
| 3 | 15 | 15.8 | −5 | −5.4 | 11 | 11 | 0 |
| 4 | 14 | 14.2 | −5.3 | −6.1 | 9 | 9 | 0 |
| 5 | 15 | 14.9 | −5.8 | −5.9 | 9 | 9 | 0 |
| 6 | 15 | 15.1 | −6.2 | −5.4 | 9 | 11 | 1 |
| 7 | 14 | 14 | −6.8 | −4.6 | 11 | 11 | 0 |
| 8 | 13.7 | 13.9 | −4.9 | −5.2 | 9 | 11 | 1.5 |
| 9 | 15 | 14.6 | −5.5 | −5.7 | 11 | 11 | 1 |
| 10 | 15 | 15.2 | −6.4 | −5.6 | 9 | 9 | 1 |
| 11 | 14.5 | 15 | −7.1 | −5.1 | 11 | 11 | 1 |
| 12 | 14.5 | 14.7 | −5.0 | −5.0 | 9 | 11 | 0 |
| 13 | 14.2 | 14.6 | −5.4 | −6.4 | 9 | 9 | 0 |
| 14 | 15 | 15.4 | −5.1 | −4.9 | 11 | 11 | 0 |
| 15 | 15 | 16 | −4.6 | −5.6 | 11 | 11 | 1 |
| 16 | 15 | 15.2 | −5.6 | −6.5 | 11 | 11 | 1 |
| 17 | 14 | 14 | −5.8 | −6.0 | 9 | 9 | 0 |
| 18 | 14.8 | 14.6 | −5.3 | −5.1 | 11 | 11 | 1 |
| 19 | 15.2 | 15 | −5.2 | −5.8 | 11 | 11 | 0 |
| 20 | 14 | 14.7 | −5.0 | −5.3 | 9 | 11 | 1 |
| 21 | 15.5 | 15 | −6.0 | −5.3 | 9 | 9 | 0 |
| 22 | 15 | 15.5 | −6.3 | −5.6 | 9 | 11 | 1 |
| 23 | 14 | 14 | −5.8 | −5.0 | 9 | 9 | 0 |
| 24 | 14 | 13.9 | −5.3 | −4.9 | 9 | 9 | 1 |
| 25 | 15.5 | 15.6 | −5.0 | −6.5 | 9 | 11 | 1 |
| 26 | 14 | 14.4 | −5.8 | −5.1 | 11 | 9 | 1 |
| 27 | 15.5 | 16.1 | −5.5 | −5.7 | 11 | 11 | 1 |
| 28 | 14 | 14.3 | −4.7 | −5.3 | 9 | 9 | 0 |
| 29 | 14.5 | 14.7 | −5.0 | −5.6 | 11 | 11 | 0 |
| 30 | 15 | 15 | −5.1 | −5.8 | 9 | 9 | 0 |
The clinical and radiological limb length difference was also compared in both groups and was not found to be significant.
4. Discussion
Restoration of limb length is the primary goal of any arthroplasty surgery [11]. LLD in TKA has not been studied much in literature.12 So, this study is done to delineate the frequency and characteristics of LLD in total knee arthroplasty. Our study demonstrated LLD which is not significant, this is inconsistent with the studies done earlier. Bhave et al.13 in his study demonstrated that the operated limb gained length as compared to contralateral nonopearted limb. In our study, limb lengthening is more common in unilateral TKA than bilateral TKA. Seven patients in group A perceived LLD and none in group B.
Several other trends were found from the results of our study which needs further research in the future. Patients with more severe mal-alignment had greater increase in length but it was insignificant in our study. Lang et al.8 also demonstrated similar results but his results were statistically significant. Lang et al. found no difference in length based on KL grade. In current study, increase in limb length was more in KL grade 3 and 4 than in KL grade 1 and 2. This could be because of increased joint space reduction in severe osteoarthritis where tibial insert acts as a source of increase in limb length but in mild to moderate osteoarthritis joint space is maintained and so we did not find any change in limb length and another reason might be the size of tibial insert which we have used. Further studies are needed to explain these findings. There are several limitations in this study. Flexion contracture may have affected the limb length measurement. Aaron et al.14 suggested that limb length measurement is not affected much if the flexion deformity is < 150. Second, It may be possible that deformity other than coronal plane affected the limb length which got unrecognized. Third, identifying the bony landmarks on x-rays was difficult for measuring the angles. Fourth, while taking limb length clinically, it was difficult to exactly locate the anterior superior illiac spine (ASIS) in obese patients.
The number of patients having radiological LLD was more than clinical LLD. Also, radiological change in the length was less than length measured clinically. Limb length difference obtained by clinical and radiological means was statistically compared but was found insignificant. This could be because of the limitations of this study as mentioned.
Various methods have been described in literature to avoid limb lengthening in THA but none in TKA.15 This is because in TKA, priorities are given to ligament and gap balancing, preoperative deformity correction.8 Fang et al.16 demonstrated in his study that maintaining postoperative HKA between 2.40 to 7.20 valgus produces improved outcome. Their study showed poor outcome if the alignment was not maintained within this range. So, a detailed study is needed to find out the methods to prevent limb lengthening in TKA without compromising alignment and stability.
5. Conclusion
We reckoned that limb length discrepancy is common after TKA especially in unilateral TKA. Limb length discrepancy of 2 cm or more is perceived by the patients operated for unilateral TKA. But in bilateral TKA, none of the patient perceived LLD because in this group LLD was less than 2 cm. Limb length discrepancy may leads to dissatisfaction of the patients and poor functional outcome. So, further studies are needed to know the incidence of LLD in total knee arthroplasty and measures to prevent the incidence of limb length discrepancy intra-operatively.
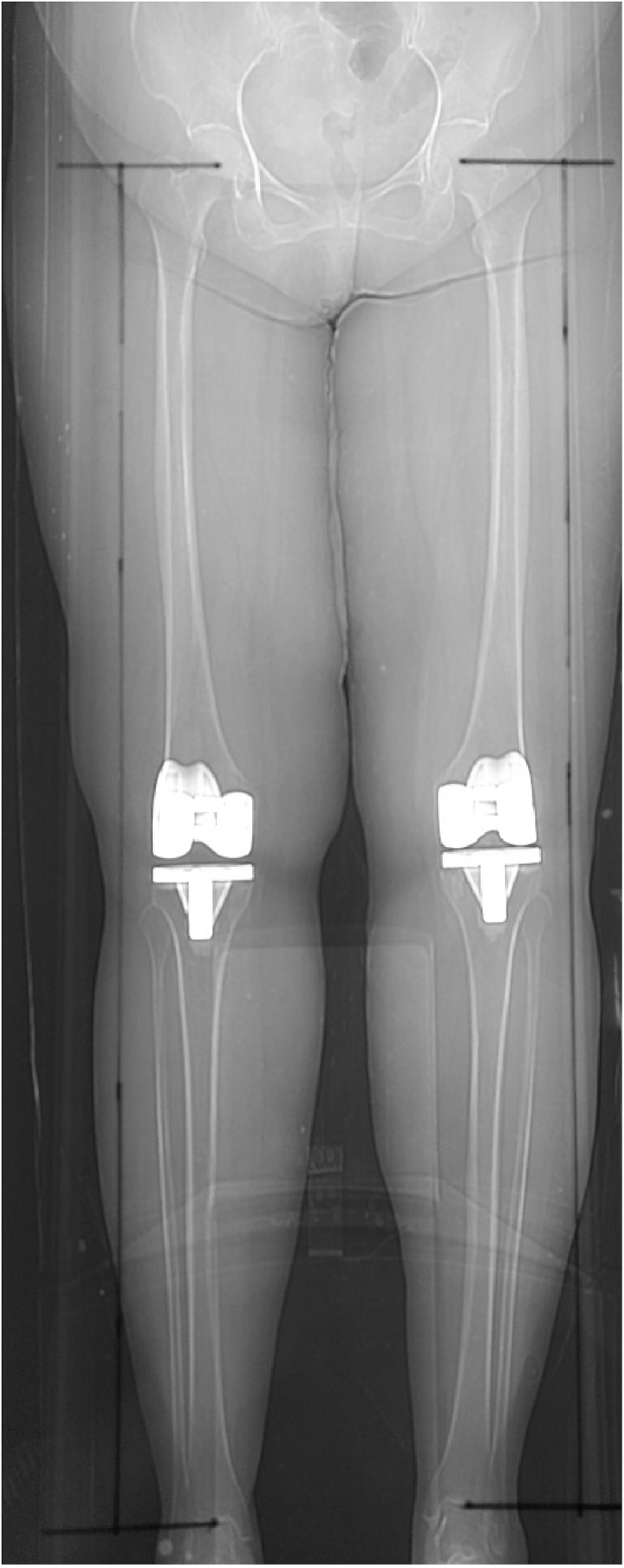
Scanogram-showing the landmark for limb length measurement: we take the length from the centre of femoral head to the centre of tibial plafond.
Declaration of competing interest
The authors have not received any funding for this work and have no conflict of interest, to declare.
Contributor Information
Aamir Bin Sabir, Email: absabir@hotmail.com.
Mohd. Faizan, Email: mohdfaizan2002@gmail.com.
Md. Ishtiaq, Email: istijnmc@gmail.com.
Latif Z. Jilani, Email: lzjilani@gmail.com.
Sohail Ahmed, Email: drsohailahmed@rediffmail.com.
Ziaul Hoda Shaan, Email: shaan.hoda007@gmail.com.
References
- 1.Ranawat C.S., Rodriguez J.A. Functional leg length inequality following total hip arthroplasty. J Arthroplasty. 1997;12:359–364. doi: 10.1016/s0883-5403(97)90190-x. [DOI] [PubMed] [Google Scholar]
- 2.Sathappan S.S., ginat D., Patel V., Walsh M., Jaffe W.L., Di Cesare P.E. Effect of anaesthesia type on limb length discrepancy after total hip arthroplasty. J Arthroplasty. 2008;23:203–209. doi: 10.1016/j.arth.2007.01.022. [DOI] [PubMed] [Google Scholar]
- 3.Turula K.B., Frieberg O., Lindholm S., Tallroth K., Vankka E. Leg length inequality after total hip arthroplasty. Clin Orthop Relat Res. 1986;202:163–168. [PubMed] [Google Scholar]
- 4.Rand J.A., Ilstrup D.M. Comparison of Charnley and T-28 total hip arthroplasty. Clin Orthop Relat Res. 1983;180:201. [PubMed] [Google Scholar]
- 5.Tipton S., Sutherland J., Schwarzkopf R. Change in limb length after total knee arthroplasty. Geriatric Orthop. Surg. And Rehab. 2015;6(3):197–201. doi: 10.1177/2151458515588187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Vaidya S.V., Patel M.R., Panghate A.N., Rathod P.A. Total knee arthroplasty: limb length discrepancy and functional outcome. Indian J Orthop. 2010;44:300–307. doi: 10.4103/0019-5413.65159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Perttunen J.R., Anttila E., Söderga°rd J., Merikanto J., Komi P.V. Gait asymmetry in patients with limb length discrepancy. Scand J Med Sci Sports. 2004;14(1):49–56. doi: 10.1111/j.1600-0838.2003.00307.x. [DOI] [PubMed] [Google Scholar]
- 8.Lang J.E., Scott R.D., Lonner J.H., Bono J.V., Hunter D.J., Li L. Magnitude of limb lengthening after primary total knee arthroplasty. J Arthroplasty. 2012;27(3):341–346. doi: 10.1016/j.arth.2011.06.008. [DOI] [PubMed] [Google Scholar]
- 9.Chang M.J., Kang Y.G., Chang C.B., Seong S.C., Kim T.K. The patterns of limb length, height, weight, and body mass index changes after total knee arthroplasty. J Arthroplasty. 2013;28(10):1856–1861. doi: 10.1016/j.arth.2013.03.024. [DOI] [PubMed] [Google Scholar]
- 10.Goldstein Z.H., Yi P.H., Batko B. Perceived leg length discrepancy after primary total knee arthroplasty: Does knee alignment play a role? Am J Orthoped. Nov/Dec 2016;45(7):E429–E433. [PubMed] [Google Scholar]
- 11.Desai A.S., Dramis A., Board T.N. Leg length discrepancy after total hip arthroplasty: a review of literature. Curr. Rev. Musculoskelet. Med. 2013;6:336–341. doi: 10.1007/s12178-013-9180-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chinnappa J., Chen D.B., Harris I.A., MacDessi S.J. Predictors and functional implications of change in leg length following total knee arthroplasty. J Arthroplasty. 2017 doi: 10.1016/j.arth.2017.04.007. [DOI] [PubMed] [Google Scholar]
- 13.Bhave A., Mont M., Tennis S., Nickey M., Starr R., Etienne G. Functional problems and treatment solutions after total hip and knee joint arthroplasty. J Bone Joint Surg Am. 2005;87:9–21. doi: 10.2106/JBJS.E.00628. [DOI] [PubMed] [Google Scholar]
- 14.Aaron A., Weinstein D., Thickman D., Eilert R. Comparison of orthoroentgenography and computed tomography in the measurement of limb-length discrepancy. J Bone Joint Surg Am. 1992;74(6):897. [PubMed] [Google Scholar]
- 15.Woolson S.T., James M.H., Sawyer A. Results of leg length equalization for patients undergoing primary total hip replacement. J Arthroplasty. 1999;14:159–164. doi: 10.1016/s0883-5403(99)90119-5. [DOI] [PubMed] [Google Scholar]
- 16.Fang D.M., Ritter M.A., Davis K.E. Coronal alignment in total knee arthroplasty. Just how important is it? J Arthroplasty. 2009;24(6):39–43. doi: 10.1016/j.arth.2009.04.034. [DOI] [PubMed] [Google Scholar]