Abstract
Introduction
Multiple hereditary exostosis (MHE) is the formation of benign, cartilage-capped bony outgrowths predominantly extending from the metaphysis of long bones that presents with reduction in growth, deformity, restricted motion, short stature and premature osteoarthritis.
Aim
To review the clinical and radiological results of a stemless reverse shoulder arthroplasty in a case of MHE.
Case
81-year-old, right hand dominant short-statured retired male engineer with long standing shoulder pain and restricted movements on the background of an old proximal humeral fracture managed conservatively.
The radiographs revealed osteoarthritis and a mal-united proximal humerus fracture on the background of MHE with 3 plane bone deformity and a lack of medullary canal.
Results
The patient underwent a stemless reverse shoulder arthroplasty. At 6 months post operatively the patient had recovered well with a range of movement including: forward flexion 110°, external rotation 20° and abduction of 80°. Internal rotation remained limited to buttocks. Improved ADLIER, Subjective shoulder value and Constant Murley score compared to pre-operative figures.
Conclusion
The stemless humeral component relies on metaphyseal impaction for stability. When the humeral canal is malformed or in presence of malunited distal fractures, it circumvents the need of navigating a deformed diaphysis with encouraging postoperative results.
Keywords: Deformity, Fracture, Multiple hereditary exostosis, Osteoarthritis, Shoulder, Stemless prosthesis
Reverse total shoulder arthroplasty is routinely being used for the management of rotator cuff deficient glenohumeral joint arthritis.3, 4, 5 Recently there is an increasing role for stemless humeral components as they are bone preserving and rely on metaphyseal fixation3, 4, 5
Multiple hereditary exostosis (MHE) is the formation of benign, cartilage-capped bony outgrowths predominantly extending from the metaphysis of long bones.6 Typically, it causes chronic pain with reduced range of movement as well as occasionally causing impingement on nerve, vessels and muscles, reduced growth, deformity, and premature osteoarthritis.6
Diagnosis of MHE occurs most often by 12 years old and has a predominance of 1 in 50,000. It has autosomal dominant inheritance with EXT1/EXT2 mutation.2
MHE can present with reduction in growth, deformity, restricted motion, short stature, and premature osteoarthritis.2,6
An 81-year-old, right hand dominant short-statured retired male engineer presented to orthopaedics with long standing shoulder pain and restricted movements on the background of a conservatively managed old proximal humerus fracture. The 8 month old fracture was sited proximal to an achondroplastic right humeral shaft on top which he also had an extensive past medical history including; vasculitis, small IgG Kappa paraprotein, ischaemic heart disease, diet controlled diabetes and meningioma with vision loss in his right eye.
On 1st clinical examination he had ongoing pain of his right shoulder scoring a pain severity of 8/10 which was particularly worse at night-time and with a reduced ability to perform his activities of daily living (ADLs). His should was non-tender on palpation with the following range of movement: external rotation 35°, forward elevation 100° and internal rotation to the sacroiliac joint. No neurological deficit was noted. The patient had a weakened and painful rotator cuff scoring a Subjective Shoulder Value (SSV) of 3/10, ADLEIR Score of 13/36 and Constant Murley score of 29.
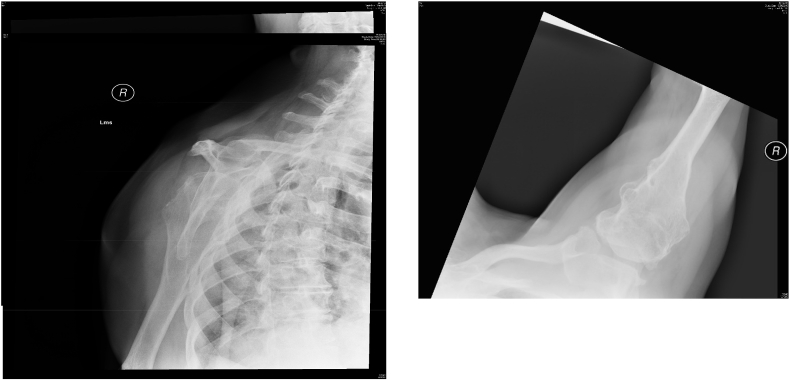
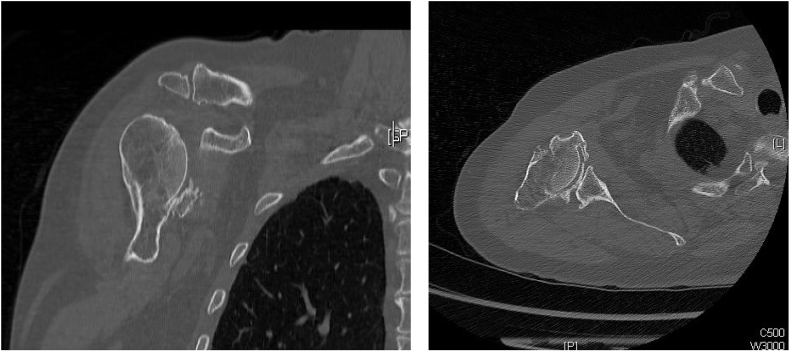
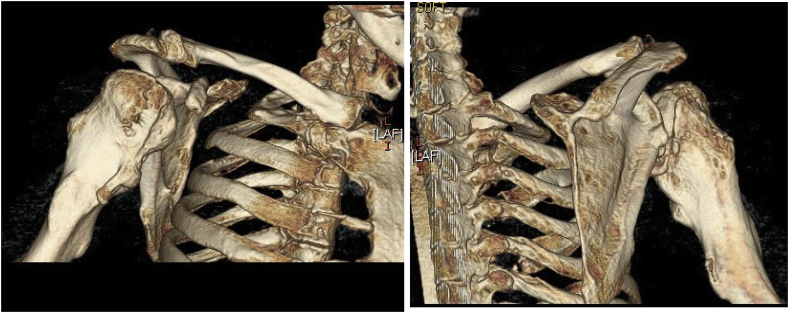
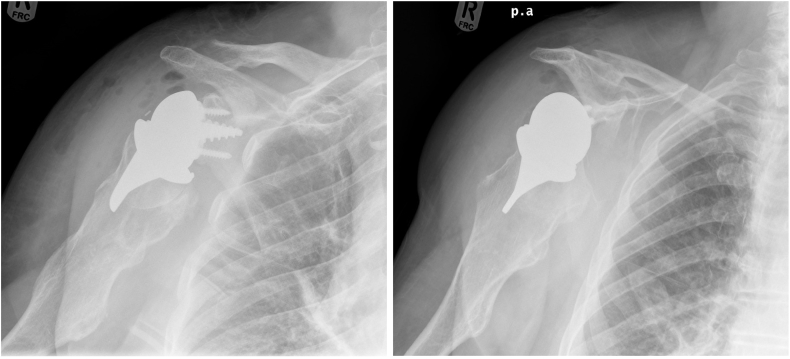
Radiographs showed a varus healed right proximal humerus fracture (Fig. 1), osteophytes around the glenohurmeral joint and a short dysplastic humeral shaft. The Computer Tomography (CT) scan with 3D reconstruction showed a 3-plane bone deformity with a narrow, deformed medullary canal riddled with exostoses. (Fig. 2, Fig. 3) Considering his altered bone morphology, a stemless uncemented (Verso; Innovative Design Orthopaedics, UK) reverse total shoulder arthroplasty was performed. Fig. 4 shows day 1 post-operative radiographs and Fig. 5 shows 1 month post-operative radiography.
Fig. 1.
Fig. 1.1 and 1.2 shows AP and axial x-rays of patients right shoulder at initial presentation.
Fig. 2.
Fig. 2.1 and 2.2: CT of patients right humerus highlighting the non-united comminuted proximal humerus fracture.
Fig. 3.
Fig. 3.1 and 3.2: 3D reconstructed CT of patients’ right shoulder, Aanterior and Posterior views highlighting the underlying deformity of the humuers
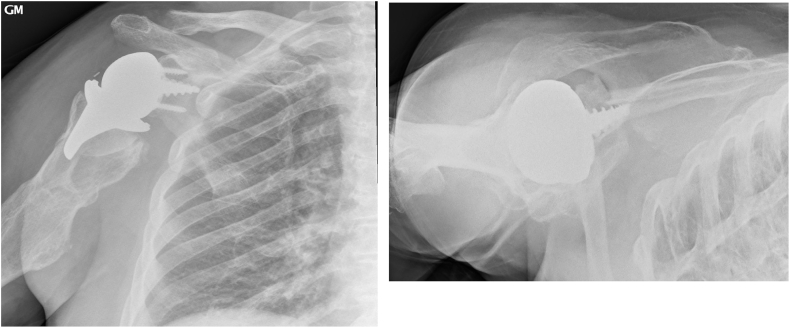
Fig. 4.
Fig. 4.1 and 4.2: Day 1 post-operative radiographs of right reverse short stemmed shoulder arthroplasty.
Fig. 5.
Fig. 5.1 and 5.2 showing 1-month post-operative AP and axial right shoulder radiographs.
One-month post operatively the patient reported marked reduction in pain with the following movements: forward flexion 100°, external rotation 20° and internal rotation to the sacroiliac joint. Neurovascular status remained normal and radiographs showed good alignment of prosthesis.
At 6 months post operatively the patient had recovered well with a range of movement including: forward flexion 110°, external rotation 20° and abduction of 80°. Internal rotation remained limited to buttocks. His post-operative scoring had significantly improved to ADLIER score 31/36, Constant Murley Score 71 and SSV of 8/10 which corresponded to his increase in ADLs.
1. Discussion
This patient presented with a unique set of issues including the presence of multiple exostosis in a short humerus along with a malformed, narrow medullary canal which was further compounded by the malunited proximal humerus fracture, cuff deficiency and glenohumeral arthritis. An analysis of the CT scan revealed the presence of an exostosis just beneath the humeral head (proximal humeral shaft) along with an eccentric narrow medullary canal and a deformed humeral shaft.
A conventional stemmed reverse shoulder arthroplasty could probably have been done with a bold resection of the humeral head. However, in addition to sacrificing significant bone stock, it could have been difficult to navigate the stem down the deformed humeral shaft.4 Moreover, there would be a high risk of an intra-operative peri-prosthetic fracture.7 Additionally, a traumatic peri-prosthetic fracture with a stemmed prosthesis, in the future, could significantly jeopardize the prosthesis as these fractures commonly occur near the tip of the stem and often necessitates a revision arthroplasty.7
A stemless reverse shoulder prosthesis relies on the metaphyseal bone impaction for stability. The Verso prosthesis has three tapered hydroxyapatite coated fins which provide immediate press-fit metaphyseal fixation into the cancellous bone of the humeral metaphysis.1,4 In osteoporotic bone, grafting i.e. using cancellous chips form the humeral head, can be used in the form of impaction grafting.3 The primary advantage of this is that there is no violation to the diaphysis and preserves bone.3 Moreover, if a peri-prosthetic fracture does occur, it is more likely to occur in the metaphyseal region which can be conservatively managed in a sling compared to a major revision arthroplasty or open reduction and internal fixation most commonly needed with fractures around a stemmed prosthesis.3,4 In this single case and in other cases where the humeral canal is malformed or in presence of malunited distal fractures, a short prothesis would circumvent the need of navigating a deformed diaphysis.
The survivorship of this prosthesis has been documented in various early to mid-term studies from independent centres.3, 4, 5 The largest series is of ninety-eight consecutive patients who underwent a stemless reverse shoulder arthroplasty.4 With a mean follow-up of 50 months (24–84 months), they showed an excellent function with a mean Constant- Murley Score increasing from 14 to 59 and a subjective shoulder value of 8/10 on latest follow-up. Another study revealed 100% survivorship of the prosthesis in the early to mid-term for a series of 37 reverse shoulder arthroplasties with excellent clinical function post operatively3 and significant improvement in the range of motion, oxford score and ADLEIR score.
A search of the literature to identify any papers involving; shoulder; arthroplasty; multiple hereditary exostosis; MHE did not yield any results further identifying the rarity of this case report.
2. Conclusion
This case report in distinctive. There is no reported case of reverse shoulder arthroplasty conducted for an arthritic shoulder with a mal-united fracture on the background of MHE in the literature. Using a short stemmed reverse prosthesis as the solution of deformities of the humerus could be extrapolated to conditions like malunited diaphyseal fractures, other tumours around proximal humerus and presence of diaphyseal metal work in the humerus as the prosthesis relies on metaphyseal fixation only. Moreover, the stemless components help to avoid excessive bone resection and the clinical and radiological results thus far are encouraging.
References
- 1.Atoun E., Van Tongel A., Hous N. Reverse shoulder arthroplasty with a short metaphyseal humeral stem. Int Orthop. 2014;38:1213–1218. doi: 10.1007/s00264-014-2328-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Jones K.B., Hilton M.J., Pacifici M. Multiple hereditary exostosis; elucidating the pathogenesis of a rare skeletal disorder through interdisciplinary research. Connect Tissue Res. 2014;55(2):p80–88. doi: 10.3109/03008207.2013.867957. [DOI] [PubMed] [Google Scholar]
- 3.Leonidou A., Virani S., Buckle C., Yeoj C., Relwani J. Reverse shoulder arthroplasty with a cementless short metaphyseal humeral prosthesis without a stem; survivorship, early to mid-term clinical and radiological outcomes in a prospective study from an independent centre. Eur J Orthop Surg Traumatol. 2019 doi: 10.1007/s00590-019-02531-2. [DOI] [PubMed] [Google Scholar]
- 4.Levy O., Narvani A., Hous N. Reverse shoulder arthro- plasty with a cementless short metaphyseal humeral implant with- out a stem: clinical and radiologic outcomes in prospective 2- to 7-year follow-up study. J Shoulder Elbow Surg. 2016;25:1362–1370. doi: 10.1016/j.jse.2015.12.017. [DOI] [PubMed] [Google Scholar]
- 5.Micheloni G.M., Salmaso G., Berti M. Cementless metaphyseal reverse shoulder arthroplasty: our preliminary experience. Acta Biomed. 2019;90(suppl 1):47–53. doi: 10.23750/abm.v90i1-S.8064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Webb E. Hereditary multiple exostosis. J Med Radiat Sci. 2015;62:p56. [Google Scholar]
- 7.Zumstein M.A., Pinedo M., Old J., Boileau P. Problems, complications, reoperations, and revisions in reverse total shoulder arthroplasty: a systematic review. J Shoulder Elbow Surg. 2011;20:146–157. doi: 10.1016/j.jse.2010.08.001. [DOI] [PubMed] [Google Scholar]