Abstract
Aim
To verify if transverse acetabular ligament (TAL) can be used as an anatomical landmark to reliably orient the cup in primary total hip arthroplasty and compare it to acetabular cups placed with the help of mechanical angle guide (MAG) device.
Materials and methods
Thirty Five patients with primary total hip arthroplasty, all performed by the same surgeon were included in the study. All patients had undergone surgery by anterolateral approach and all were cementless total hip arthroplasty. TAL was used as a reference guide for positioning of the cup in one group while MAG device was used in the other. Post operatively CT was done to confirm the version and inclination of the acetabular cup and the femoral stem version. SPSS was used for statistical analysis.
Results
18 males and 17 females were included. The most common etiological cause for THR was secondary osteoarthritis due to AVN (40%). At 18 months follow up, there was just 1 case of dislocation in group in which angle guide device was used. The mean anteversion of the acetabular cup on CT findings was 23.82° by using TAL while 18.35° with help of MAG device (P < 0.05). All were within Leweniks safe zone.
Conclusions
The TAL and MAG device both can be effectively used to align the acetabulum component. TAL is patient specific intraoperative landmark which is not affected by patient positioning while angle guide device can give false positive assessment of cup version.
Keywords: Transverse acetabular ligament, Hip arthroplasty, Anteversion, Dislocation, Inclination
1. Introduction
Anteversion of acetabular cup plays a very important role in determining the success of total hip arthroplasty (THA) surgery. Faulty placement of the acetabular cup can lead to variety of short term (post-operative dislocation of joint, leg length discrepancy) and long term complications (excessive wear and osteolysis).
The most commonly cited paper regarding anteversion of the acetabular component was published in 1978 by Lewinnek.1 It described “Safe zone” of anteversion as between 5° and 25° of radiographic anteversion. Later Murray et al. described three types of acetabular cup anteversion -anatomical, operative and radiographic.2 They concluded that all 3 types of version were different as they had different plane of reference, so they developed conversion nomograms.
In this study, to achieve the best position of cup TAL (transverse acetabular ligament) has been used as an intraoperative anatomical landmark in one group and commercially available mechanical angle guide (MAG) device has been used in the other group. Viste et al. did a cadaveric study in which they tried to verify if TAL (transverse acetabular ligament) as a patient specific anatomical landmark and if it can be used for cup orientation.3 They concluded that TAL’s reliability as a landmark for cup placement needed more research to confirm it. Many orthopaedic companies have developed acetabular component positioning devices in order to improve the accuracy. The primary aim of this study was to evaluate the validity of TAL in proper placement of acetabular cup. The secondary goal was to compare the cup anteversion and inclination achieved by using TAL with those acetabular cups placed with the help of MAG device. The null hypothesis was that there would be no difference in acetabular cup version and inclination achieved by two techniques and that both could be used for placement of acetabular cup within the safe zone.
2. Patients and methods
This prospective study was started in September 2016 and the data was collected over the next 3 years. 40 consecutive patients undergoing primary un-cemented total hip arthroplasty were included. Patients with history of previous acetabular, pelvic fractures, hip disorders during childhood, any previous surgery around hip were excluded. All cases where anaesthetist used Trendelenburg or Reverse Trendelenburg position were excluded. All patients with in age group of 20 and 80 years were included. Randomised controlled trial was not carried out. In the first 20 patients TAL was used while in the second 20 patients MAG device was used for placement of cup. Only thirty five patients could be followed up for a minimum of eighteen months while 5 were lost to follow up (1 patient from the former group while 4 from later group). In the beginning of the study, sample size was not calculated. After completion of the study, power was calculated for primary outcome. Power was 90% when calculated at 5% level of significance with detected difference of 5.47° and number of samples in group 1 were 19 and group 2 were 16. All surgeries were performed by the same experienced surgeon having more than 15 years of professional experience in total hip arthroplasty. All the cases were done in lateral decubitus position through direct lateral Hardinge’s approach using the intermuscular and interneural planes. Patient was positioned with the use of three posts (at sacrum, at anterior superior iliac spine and symphysis pubis). Cementless press-fit acetabular component (Pinnacle; DePuy)4 and a cementless femoral component (Corail; DePuy)5 were implanted.The tribiologic pairing consisted of polyethylene and ceramic liners with metal and ceramic modular head with variable head diameters. Per-operatively, the surgeon used TAL as a reference guide for positioning of the acetabular cup in one group of patients while in other group final position of the cup was done by using MAG device Once adequate acetabular reaming was done, the acetabular cup prosthesis was mounted on the MAG device. The MAG device could be adjusted to place the cup in 0,10, 20 and 30° of anteversion or retroversion; while the inclination was fixed at 45°. To achieve the desired inclination the handle of the MAG was kept parallel to the operating room floor and for the desired anteversion the attached rod was aligned with the long axis of the body. (Fig. 1, Fig. 2). All surgeries were done in spinal combined with epidural anesthesia.
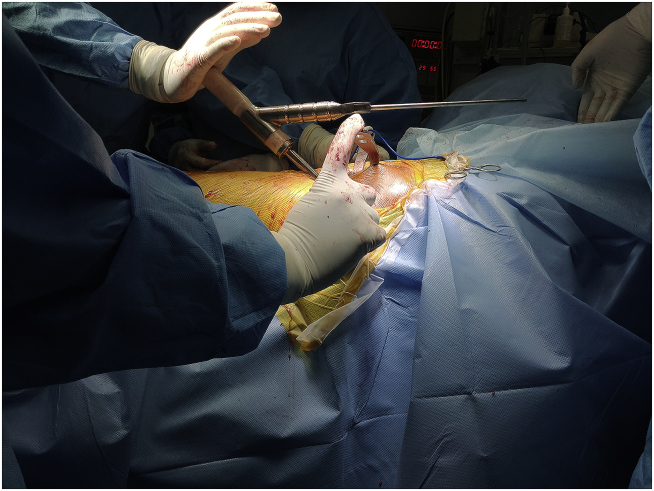
Fig. 1.
Angle guide device used to check inclination of acetabular cup.
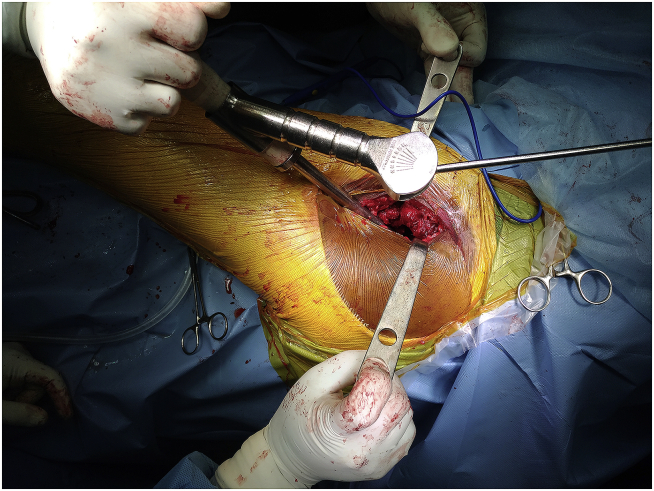
Fig. 2.
Angle guide device used check anteversion of acetabular cup.
Post operatively 3D-CT scans (Mx8000; Philips Medical systems, Highland heights, Ohio)6 of pelvis was done to confirm the version and inclination of the acetabular cup. Each scan was performed at 1 mm intervals and 1 mm thickness with a field of view of 300 mm and a pitch of 0.58. Three hundred to 350 frames per scan were done. This data were stored in the Digital imaging and communications in Medicine (DICOM) format. The radiologist who calculated the anteversion and inclination was blinded about the study. The inclination of the cup was calculated on coronal section in CT scan. A horizontal line was drawn connecting both inferior pubic rami. The angle between this line and a line drawn by connecting the points of the acetabular cup were measured (Fig. 3). For calculating anteversion of the cup transverse section of the CT was taken at the level of the acetabulum. A line was drawn connecting both the edges of the cup. The angle formed by this line with the horizontal line along the anterior edge of the pelvis calculated the anteversion (Fig. 4). Femoral stem version was calculated in order to find out the combined version of acetabular cup and femoral stem. The central axis of the femoral neck of stem and the posterior femoral condylar axis were used as references. In a study carried out by Dorr et al.7 the anteversion of the femoral stem was calculated by using both epicondylar plane and posterior condylar plane. Both reference planes were found to have good correlation coefficient. The study had ethical approval and all patients gave informed consent.
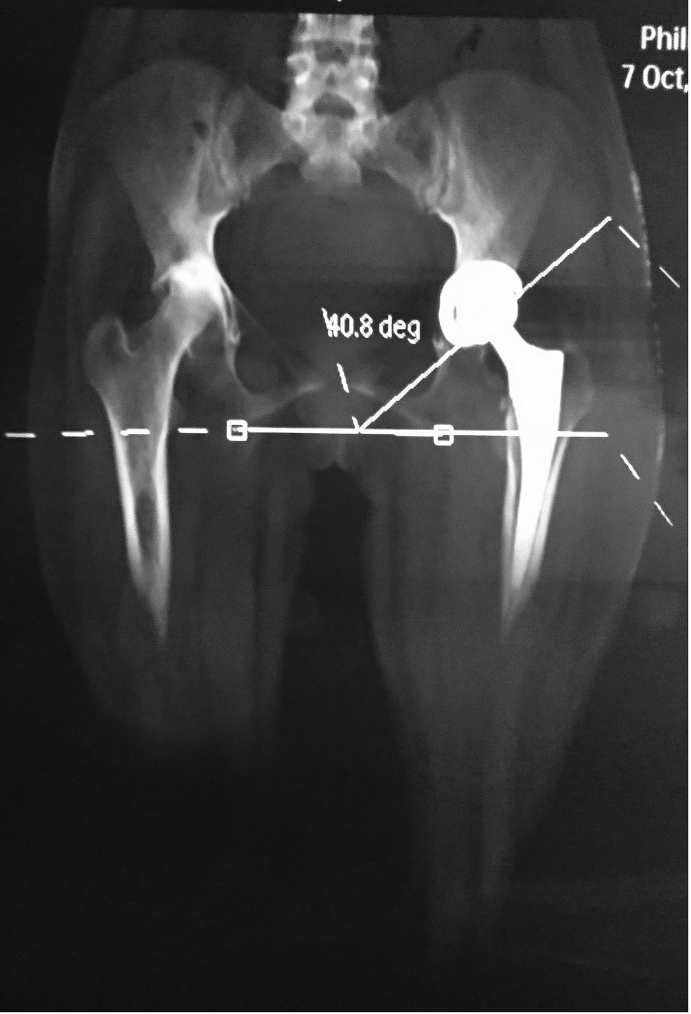
Fig. 3.
Post operative CT scan showing inclination of acetabular cup.
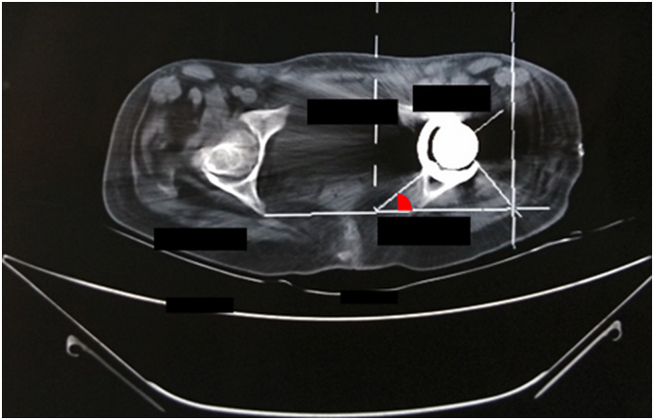
Fig. 4.
Post operative CT scan showing anteversion of acetabular cup.
2.1. Statistics
The data was analysed by using statistical software SPSS version 20. Categorical data was expressed as frequency and percent. Quantitative variable expressed as mean, standard deviations (SD), and minimum maximum. Chi square/Fischer exact test was used to compare categorical variable between the groups. Independent T test was used to test the statistical significance between the two surgical techniques. Confidence interval for difference was estimated. P value < 0.05 was considered as statistically significant.
3. Results
At the time of statistical analysis the study included 19 patients in the first group i.e. TAL was used for placement of acetabular cup and 16 patients in the second group i.e. MAG device was used. The demographic detail of the patients is shown in Table 1. There was no significant difference between the age groups and BMI of both the groups, which made them more comparable. Metal on poly was the most commonly used combination.
Table 1.
Details of the patients included in the study.
| Parameter | TAL group | Angle Guide Device group | |
|---|---|---|---|
| Age (years) (Mean) | 51.52 | 54.81 | |
| Follow up (months) (mean) | 12.2 | 13.5 | |
| Body mass index (kg/m2) (mean) | 31.51 | 32.58 | |
| Sex | Male Female |
10 9 |
8 8 |
| Liner | Poly Ceramic |
11 8 |
11 5 |
| Head | Metal Ceramic |
11 8 |
8 8 |
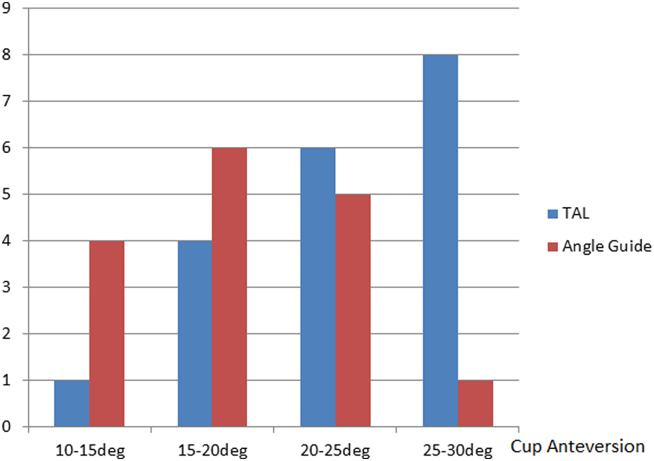
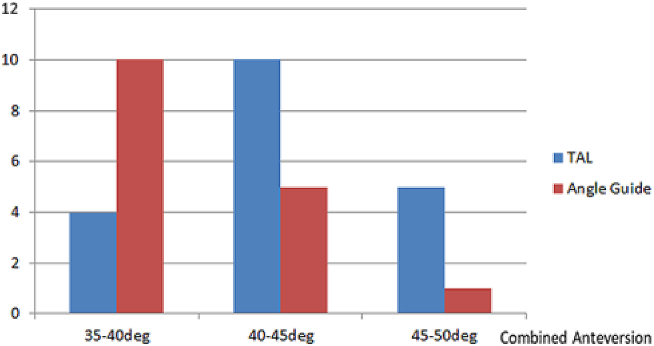
Fig. 5 shows anteversion of the acetabular cup in both groups of patients (10°–30°), while Fig. 6 shows the combined femoral and acetabular version (35°–50°). The mean acetabular cup version and femoral stem version in both groups of patients were as shown in Table 2. There was a significant difference (P = 0.0032) in the acetabular cup version placed by using TAL and angle guide device even though all were in safe zones. The combined anteversion of both the group of patients was also significantly different. (P = 0.0042) The difference in the femoral stem version and the inclination of the acetabular cup was not significant between the 2 groups. (Table 2).
Fig. 5.
Comparison of anteversion of acetabular cup in both groups.
Fig. 6.
Comparison of Combined anteversion of acetabular cup in both groups.
Table 2.
Acetabulur cup anteversion & inclination, Femoral neck version recordings (degrees).
| Variable | Group | Mean ± SD | Min- max | Difference 95% CI | P value |
|---|---|---|---|---|---|
| Acetabular version | TAL | 23.8 ± 4.9 | 13.9–29.7 | 5.4 (1.9, 8.9) | 0.0032 |
| MAG | 18.3 ± 5.2 | 10.1–29.7 | |||
| Femoral Version | TAL | 19.1 ± 6.2 | 8.1–30.7 | 1.3 (−2.5,5.1) | .494 |
| MAG | 20.4 ± 4.6 | 11.8–28.5 | |||
| Combined Version | TAL | 42.9 ± 3.4 | 37–49.6 | 4.1 (1.4, 6.9) | 0.0042 |
| MAG | 38.8 ± 4.5 | 35.2–45.9 | |||
| Acetabular Inclination | TAL | 44.8 ± 4.9 | 36.6–54.2 | 0.5 (−2.8, 3.9) | 0.74 |
| MAG | 44.2 ± 4.8 | 35.8–51.8 |
MAG- Mechanical angle guide.
The most common cause of total hip replacement in this study was secondary osteoarthritis due to avascular necrosis of femoral head (40%). The other causes are shown in Table 3. Mean acetabular cup size and femoral head size in TAL group was 48.84 mm and 33.47 mm respectively while in the other group these were 48.5 mm and 31 mm respectively.
Table 3.
Causes of Total Hip replacements in patients included in this study-.
| SN | Cause | Nos. | Percentage |
|---|---|---|---|
| 1. | Secondary OA due to AVN | 14 | 40.0 |
| 2. | Primary OA | 2 | 5.7 |
| 3. | Neck of Femur | 12 | 34.3 |
| 4. | Post septic sequelae | 7 | 20.0 |
4. Discussion
Archbold et al.8 described 4 types of TAL during total hip arthroplasty. Most common type was the ones which were immediately visible on exposure of the acetabulum, then the ones which were covered by soft tissue which could be easily removed by blunt dissection, the third type in which the TAL was covered by an osteophyte and the rarest when no TAL was found.
Even till today hip dislocation is the second commonest cause for revision of a primary hip arthroplasty.9 Thus it is important to improvise our techniques in order to reduce the number of post operative hip dislocation. The findings of this study show that if the acetabular cup and stem is placed correctly then there are high chances of not having a dislocation of hip and this can be better ensured by using either the TAL or the MAG device.
In this study, only one patient had dislocation even after following all the patients for more than 18 months. It has been seen that almost 80% of the dislocations after primary hip replacement occurs within first 2 months after surgery. A high inclination angle has been associated with an increased rate of dislocation.10 According to National Joint registry9 the dislocation rate is highest in all types of primary THA in the 1st year after surgery and it falls later.
There are other factors as well which contributed to the stability of the hip replacements included in this study. Posterior approach to hip has been reported to have higher rate of dislocation.11 In this study anterolateral approach was used in all cases in lateral decubitus. These could contribute to decrease in intra-operative movement of the pelvis.12 This helped to improve the accuracy of MAG device. It has been seen that there is more intra-operative movement with the posterior approach than with the lateral approach in THA because of the intact strong anterior capsule and ilio-femoral ligament, coupled with the strong retraction and the leg-twisting manoeuvre, which lead to an increased torque to the pelvis.
Surgical experience of the operating surgeon has also been reported to be directly correlated to the rate of dislocation.11 The chances of having a hip dislocation are higher in the first 30 hips that a surgeon performs, the risk of dislocation is decreased by 50% for every ten primary THAs that a surgeon does annually.13 In this study, all THA were performed by the same experienced surgeon performing more than 10 primary THAs annually for last 10 years.
Several studies have reported different acetabular cup anteversion and inclination with different techniques. (Table 4). DiGioia et al.14 reported a wide range of acetabular version and inclination in past with MAG and they considered it as inadequate in achieving the desired goal. In the present study, the mechanical guide showed greater variation in acetabular cup version than the TAL group of THAs (Table 2) but all were within safe zones. As a result of which there was just one hip dislocation in the MAG group. Therefore, MAG can be still used for acetabular cup placement along with proper precautions for rigid positioning of the patient. More complex mechanical devices using anterior pelvic plane have been tested in cadavers.15 They also found it helpful to increase the accuracy in positioning of the acetabular cup, but uses of such devices have their own drawbacks like increased surgery time and complications associated with reference pin placement. Similarly MRI-based patient-specific instrumentation guide have been used during THA.16 These require preoperative and postoperative CT scans as well. These have proven to increase the accuracy of acetabular cup placement but at the same time increase the total cost on healthcare system and exposes patient to radiation which could be avoided by using simpler methods. Grammatopoulos et al.17 did a in vitro study using a hemipelvic model to check surgeons accuracy at acetabular cup placement. It was found that use of mechanical alignment guide did improve variability in anteversion by one third but it was still about ± 10°. It was concluded that better guides were required. In present study, the variability was less but it still existed.
Table 4.
Different acetabular cup anteversion and inclination with different techniques.
| Authors | Technique | Mean Cup Anteversion (°) | Mean Cup inclination (°) |
|---|---|---|---|
| DiGioia et al.14 | MAG (n = 74) | 1 ±10 (33 to −26) | 44 ±4 (35–59) |
| Grammatopoulos et al.17 | TAL (n = 21) | 34 ± 7 (17–45) | NA |
| MAG (n = 21) | 23 ± 5 (13–35) | 42 ± 5 (24–49) | |
| Kievit et al.15 | MAG with APP (n = 16) | 13.4 (10.7–16.1) | 40.6 (37.7–43.4) |
| Inoue et al.16 | CT templating & PSI Initial group (n = 7) Later group (n = 7) |
27.4 ± 6.0 27.4 ± 4.5 |
44 ± 4.7 45.6 ± 2.6 |
| Kalteis et al.18 | TAL & posterior labrum (n = 39) | 18 (-1 to) | 41 (32–51) |
| Padgett et al.22 | MAG (n = 40) | NA | 42.1 ± 8.3 (23–57) |
| Meermans et al.23 | Free Hand (n = 100) | NA | 38.5 ± 7 (22–60) |
| Digital protractor (n = 100) | NA | 38.3 ± 4.7 (27–51) | |
| Our study | TAL (n = 19) | 23.8 ± 4.9 (21.4–26) | 44.8 ± 4.9 (42.4–47.2) |
| MAG (n = 16) | 18.3 ± 5.2 (15.5–21.1) | 44.2 ± 4.8 (41.6–46.8) |
APP- Anterior pelvic plane.
TAL- Transverse acetabular ligament.
MAG- Mechanical angle guide.
PSI- patient-specific surgical instrument guide.
Acetabular version and inclination has been measured intra-operatively with the help of computer assisted navigation after defining the acetabular plane with the help of TAL and posterior labrum in the past. The mean acetabular component inclination was found to be 41° (32–51) and anteversion of 18° (−1 to 36). It was found that there is only a moderate interobserver agreement and intra-observer reliability in the alignment of the acetabular component using the TAL and the posterior labrum.18 Thus, it can be said that even though TAL is a patient specific landmark but its use to place the cup can have variations between the surgeons.
Hasegawa et al.19 compared the stem and cup anteversion using CT scans of dislocated and non-dislocated total hips. Both the cup anteversion and the stem anteversion showed no differences among the groups. But the sum of cup and stem anteversion in posterior dislocated hips was significantly lesser than that in non-dislocated hips and the sum in anterior dislocated hips was significantly greater than that in non-dislocated hips. This proves the importance of calculation of combined anteversion.
Operative anteversion has been found to increase the radiographic inclination up to 6°.20 Thus, it is important to place the cup in correct version as it affects placement in other planes as well. Hill et al.21 published that due to adduction of the pelvis in the frontal plane there could be a difference between mean of operative inclination and radiographic inclination angle.
In our study the mean inclination using the MAG device for the acetabular cup positioning was 44.27 ± 4.85° (41.68–46.85). Padgett et al.22 did 40 hip replacements using the positioning device. Their mean cup abduction angle in the group was 42.1 ± 8.3° (23–57). In this study variation was lesser than Padgett et al.22 because the patient was placed firmly on the operating table with 2 posts anteriorly and 1 posteriorly. This minimised the patient movement during the surgery and so the pelvis could not rotate. The large variation in cup placement is a function of change in patient position during the procedure. It may be due to pelvic rotation taking place during the surgery, both in forward/backward rotation as well as shifting of the pelvis. In a study in UK23 it was found that more than 35% of orthopaedic surgeons were unhappy with the patient supports they used for patient positioning and only 31% of them considered their supports to be completely rigid. They concluded that it was very important to create awareness among orthopaedic community about patient support choices and monitoring of pelvic stabilisation.
The difference between the radiographic and operative angle of inclination of the acetabular cup has been studied with the help of digital protractor.24 The anteversion of the cup was determined by using TAL. There was significant difference between the radiographic (RI) and operative angle of inclination (OI) in between the groups where the cup was placed free hand and the other group which used the protractor. The anteversion did not have any major influence on RI-OI. Thus, it’s always better to have some guiding system (digital protractor or angle guide device) during the cup placement as it increases the accuracy and is better than doing just by free hand technique alone. Despite the fact that there was significant difference between the anteversion achieved by two techniques, all were within safe zones and there was only one dislocation reported. So, the comparison cannot prove the superiority of one technique over the other. This study proves that the accuracy of both techniques can be improved substantially by taking care of several other factors which can lead to hip dislocation. We recommend comparing the results to a group where the use of TAL is reinforced by MAG for acetabular cup placement.
There were some limitations of the study. Randomisation was not done during allocation of groups. The sample size was not large and a larger scale study can be carried out in future.
In conclusion, TAL can be used as a patient specific guide to acetabular cup placement and the MAG device is a useful tool to aid in socket position during primary total hip arthroplasty with due vigilance in table and patient positioning during surgery. Both are effective in placing the acetabular cup within safe zones, but the anteversion achieved by both techniques can differ significantly.
Contributor Information
Archit Agarwal, Email: dr.architagarwal@gmail.com.
Inder Pawar, Email: inderpawar67@yahoo.co.in.
Sandeep Singh, Email: dr.sandeepnew@gmail.com.
Deepti Randev, Email: deepti2689@gmail.com.
Hem Chandra Sati, Email: hem198617@yahoo.com.
References
- 1.Lewinnek G.E., Lewis J.L., Tarr R.I., Compere C.L., Zimmerman J.R. Dislocations after total hip-replacement arthroplasties. The Journal of bone and joint surgery. American volume. 1978 Mar;60(2):217–220. [PubMed] [Google Scholar]
- 2.Murray D.W. The definition and measurement of acetabular orientation. The Journal of bone and joint surgery. British volume. 1993 Mar;75(2):228–232. doi: 10.1302/0301-620X.75B2.8444942. [DOI] [PubMed] [Google Scholar]
- 3.Viste A., Chouteau J., Testa R., Cheze L., Fessy M.H., Moyen B. Is transverse acetabular ligament an anatomical landmark to reliably orient the cup in primary total hip arthroplasty? J Orthop Traumatol: Surgery & Research. 2011 May 1;97(3):241–245. doi: 10.1016/j.otsr.2010.07.012. [DOI] [PubMed] [Google Scholar]
- 4.Synthes DePuy. Pinnacle Hip Solutions. January 2020. https://www.jnjmedicaldevices.com/en-US/product/pinnacler-acetabular-cup-system Available from. cited.
- 5.Synthes DePuy. Coral Hip System. January 2020. https://www.jnjmedicaldevices.com/en-US/product/corail-total-hip-system Available from. cited.
- 6.Mx8000 January 2020. http://incenter.medical.philips.com/doclib/enc/fetch/2000/4504/577242/577256/588723/5144873/5144488/5145048/DICOM_Mx800-IDT_V_2.5.pdf%3fnodeid%3d5147723%26vernum%3d-2 Philips Medical systems Available from. cited.
- 7.Dorr L.D., Wan Z., Malik A., Zhu J., Dastane M., Deshmane P. A comparison of surgeon estimation and computed tomographic measurement of femoral component anteversion in cementless total hip arthroplasty. JBJS. 2009 Nov 1;91(11):2598–2604. doi: 10.2106/JBJS.H.01225. [DOI] [PubMed] [Google Scholar]
- 8.Archbold H.A., Mockford B., Molloy D., McConway J., Ogonda L., Beverland D. The transverse acetabular ligament: an aid to orientation of the acetabular component during primary total hip replacement: a preliminary study of 1000 cases investigating postoperative stability. The Journal of bone and joint surgery. British volume. 2006 Jul;88(7):883–886. doi: 10.1302/0301-620X.88B7.17577. [DOI] [PubMed] [Google Scholar]
- 9.National Joint Registry of England WNorthern Ireland and the Isle of Man.16th Annual Report. 2019. https://reports.njrcentre.org.uk/Portals/0/PDFdownloads/NJR%2016th%20Annual%20Report%202019.pdf Date [Google Scholar]
- 10.Biedermann R., Tonin A., Krismer M., Rachbauer F., Eibl G., Stöckl B. Reducing the risk of dislocation after total hip arthroplasty: the effect of orientation of the acetabular component. The Journal of bone and joint surgery. British volume. 2005 Jun;87(6):762–769. doi: 10.1302/0301-620X.87B6.14745. [DOI] [PubMed] [Google Scholar]
- 11.Morrey B.F. Instability after total hip arthroplasty. Orthop Clin N Am. 1992 Apr;23(2):237–248. Orthop Clin North Am. 1992 Apr;23(2):237-48. [PubMed] [Google Scholar]
- 12.Grammatopoulos G., Pandit H.G., Da Assunção R. Pelvic position and movement during hip replacement. The bone & joint journal. 2014 Jul;96(7):876–883. doi: 10.1302/0301-620X.96B7.32107. [DOI] [PubMed] [Google Scholar]
- 13.Hedlundh U., Ahnfelt L., Hybbinette C.H., Weckström J., Fredin H.A. Surgical experience related to dislocations after total hip arthroplasty. The Journal of bone and joint surgery. British volume. 1996 Mar;78(2):206–209. [PubMed] [Google Scholar]
- 14.DiGioia A.M., III, Jaramaz B., Plakseychuk A.Y. Comparison of a mechanical acetabular alignment guide with computer placement of the socket. J Arthroplasty. 2002 Apr 1;17(3):359–364. doi: 10.1054/arth.2002.30411. [DOI] [PubMed] [Google Scholar]
- 15.Kievit A.J., Dobbe J.G., Mallee W.H., Blankevoort L., Streekstra G.J., Schafroth M.U. Accuracy of cup placement in total hip arthroplasty by means of a mechanical positioning device: a comprehensive cadaveric 3d analysis of 16 specimens. HIP Int. 2019 doi: 10.1177/1120700019874822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Inoue D., Kabata T., Kimura H., Tsuchiya H. A prospective clinical trial to assess the accuracy of an MRI-based patient-specific acetabular instrument guide in total hip arthroplasty. Eur J Orthop Surg Traumatol. 2019 Jan 8;29(1):65–71. doi: 10.1007/s00590-018-2279-7. [DOI] [PubMed] [Google Scholar]
- 17.Grammatopoulos G., Alvand A., Monk A.P. Surgeons’ accuracy in achieving their desired acetabular component orientation. JBJS. 2016 Sep 7;98(17):e72. doi: 10.2106/JBJS.15.01080. [DOI] [PubMed] [Google Scholar]
- 18.Kalteis T., Sendtner E., Beverland D. The role of the transverse acetabular ligament for acetabular component orientation in total hip replacement: an analysis of acetabular component position and range of movement using navigation software. The Journal of bone and joint surgery. British volume. 2011 Aug;93(8):1021–1026. doi: 10.1302/0301-620X.93B8.25720. [DOI] [PubMed] [Google Scholar]
- 19.Hasegawa M., Komeno M., Sudo A., Uchida A. Computed tomographic evaluation of component position on dislocation after total hip arthroplasty. Orthopedics. 2006 Dec 1;29(12) doi: 10.3928/01477447-20061201-05. [DOI] [PubMed] [Google Scholar]
- 20.Beverland D.E., O’Neill C.K., Rutherford M., Molloy D., Hill J.C. Placement of the acetabular component. The bone & joint journal. 2016 Jan;98(1_Supple_A):37–43. doi: 10.1302/0301-620X.98B1.36343. [DOI] [PubMed] [Google Scholar]
- 21.Hill J.C., Gibson D.P., Pagoti R., Beverland D.E. Photographic measurement of the inclination of the acetabular component in total hip replacement using the posterior approach. The Journal of bone and joint surgery. British volume. 2010 Sep;92(9):1209–1214. doi: 10.1302/0301-620X.92B9.24476. [DOI] [PubMed] [Google Scholar]
- 22.Padgett D.E., Hendrix S.L., Mologne T.S., Peterson D.A., Holley K.A. Effectiveness of an acetabular positioning device in primary total hip arthroplasty. HSS J. 2005 Sep 1;1(1):64–67. doi: 10.1007/s11420-005-0109-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Rutherford M., O’Connor J.D., Hill J.C., Beverland D.E., Lennon A.B., Dunne N.J. Patient positioning and cup orientation during total hip arthroplasty: assessment of current UK practice. HIP Int. 2019 Jan;29(1):89–95. doi: 10.1177/1120700018760818. [DOI] [PubMed] [Google Scholar]
- 24.Meermans G., Goetheer-Smits I., Lim R.F., Van Doorn W.J., Kats J. The difference between the radiographic and the operative angle of inclination of the acetabular component in total hip arthroplasty: use of a digital protractor and the circumference of the hip to improve orientation. The bone & joint journal. 2015 May;97(5):603–610. doi: 10.1302/0301-620X.97B5.34781. [DOI] [PubMed] [Google Scholar]