Abstract
Introduction:
Although evaporative heat loss capacity is reduced in burn-injured individuals with extensive skin grafts, the thermoregulatory strain due to a prior burn injury during exercise-heat stress may be negligible if the burn is located underneath protective clothing with low vapor permeability.
Purpose:
To test the hypothesis that heat strain during exercise in a hot-dry environment while wearing protective clothing would be similar with and without a simulated torso burn injury.
Methods:
Ten healthy individuals (8M/2F) underwent three trials wearing: Uniform (combat uniform, tactical vest, and replica torso armor plates), Uniform with a 20% total body surface area (TBSA) simulated torso burn (Uniform + Burn), or shorts (and sports bra) only (Control). Exercise consisted of treadmill walking (5.3 km·h–1; 3.7 ± 0.9% grade) for 60 min at a target heat production of 6.0 W·kg−1 in 40.0 ± 0.1°C; 20.0 ± 0.6% relative humidity conditions. Measurements included rectal temperature, heart rate, rating of perceived exertion, and thermal sensation.
Results:
No differences in rectal temperature (P ≥ 0.85), heart rate (P ≥ 0.99), thermal sensation (P ≥ 0.73), or rating of perceived exertion (P ≥ 0.13) occurred between Uniform + Burn and Uniform trials. In the Control trial, however, core temperature, heart rate, thermal sensation, and rating of perceived exertion were lower compared to the Uniform and Uniform + Burn trials (P ≤ 0.04 for all).
Conclusion:
A 20% TBSA simulated torso burn injury does not further exacerbate heat strain when wearing a combat uniform. These findings suggest that the physiological strain associated with torso burn injuries is not different from non-injured individuals when wearing protective clothing during an acute exercise-heat stress.
Keywords: Military, core temperature, burn survivor, evaporative heat loss, heat strain, exercise-heat stress
INTRODUCTION
Following a severe burn injury, removal of damaged tissue and subsequent skin grafting leads to the destruction and denervation of sweat glands (1–4), causing impaired/absent sweating within grafted skin. Extensive skin grafting, therefore, greatly reduces the capacity for whole-body evaporative heat dissipation, which exacerbates the elevation in core temperature during physical activity (2, 5–8). This adverse effect raises the risk for a heat illness during exercise-heat stress compared to non-injured individuals. Whether burn injuries induce similar decrements in thermoregulatory capacity when protective clothing is worn has not yet been determined.
In many occupations, workers are required to wear unique clothing and use equipment that protects them from physical and/or environmental hazards, but also impose a substantial thermoregulatory burden by restricting body heat dissipation to the external environment. For example, to protect against projectile and fragmentation injury, military personnel typically wear a combat uniform and body armor, which simultaneously inhibit evaporative heat dissipation from the torso surface (9–12). Many police officers wear similar ensembles. Thus, compared to a minimal clothing ensemble, protective clothing with body armor exacerbate heat strain, increases the risks of heat illness, and impairs duty performance during prolonged periods of work and ambient heat stress (12, 13). Whether a burn injury located on the torso underneath a protective clothing/body armor ensemble further increases thermoregulatory strain is currently unknown, as the detrimental effects of burn injuries are primarily identified under semi-nude conditions (i.e., only shorts, socks, and shoes were worn) (4, 5, 14). Given the expectation that protective clothing and body armor impede sweat evaporation, then the absence of sweat production from extensively-grafted torso skin in a burned individual should not exaggerate the thermoregulatory strain. In other words, evaporative heat loss from the torso is likely negligible when protective clothing and body armor with low vapor permeability are worn, regardless of whether there is a torso burn injury. This question is particularly pertinent given that (i) ~20–25% of burn injuries in recent military conflicts include burns on the torso (15), and (ii) the US Army’s Standards of Medical Fitness Army Regulation 40–501 which states, pertaining to burn injuries as an exclusion, that “extensive burns on the torso will most significantly impair heat dissipation” (16).
The present study evaluated whether heat strain during exercise in a hot-dry environment, while wearing military protective clothing (combat uniform, tactical vest, with front and back replica armor plates), would be similar with and without a simulated torso burn injury. Specifically, we tested the hypothesis that exercise-heat stress will lead to similar levels of heat strain, regardless of a simulated torso burn injury, when protective clothing with low vapor permeability is worn. This information may be important in determining whether soldiers and police officers with healed torso burn injuries, who also must wear protective clothing during training and operations, should or should not be excluded from service due the potential for exacerbated heat strain.
METHODS
Ethical Approval
The Institutional Review Boards of the University of Texas Southwestern Medical Center, Texas Health Presbyterian Hospital Dallas, and the Human Research Protections Office of the Defense Health Agency approved the study protocol and associated informed consent, which conformed to standards set forth in the Declaration of Helsinki. Written informed consent was provided by all participants prior to participation in the study.
Participants
Ten participants (8 males/2 females), reported to be physically active and non-smoking as well as free of any known cardiovascular, metabolic, or neurological disease, were recruited for the study. Participant characteristics are presented in Table 1.
Table. 1.
Subject characteristics
| Sex | Age (yr) | Body mass (kg) | Height (m) | TBSA (m2) | Body mass index (kg·m−2) |
|---|---|---|---|---|---|
| Men | 31 ± 5 | 74.6 ± 6.1 | 1.77 ± 0.1 | 1.90 ± 0.1* | 23.7 ± 1.6 |
| Women | 23 ± 4 | 65.6 ± 11.7 | 1.65 ± 0.0 | 1.70 ± 0.1 | 23.8 ± 4.0 |
| Combined | 30 ± 6 | 72.5 ± 7.6 | 1.75 ± 0.07 | 1.87 ± 0.1 | 23.8 ± 2.0 |
TBSA, total body surface area; Unpaired t-test was used for single comparisons between participant characteristics
Significantly different from females (P ≤ 0.05). Values are means ± SD.
Instrumentation and Measurements
A urine sample was obtained to measure urine specific gravity (Atago Inc., Bellevue, WA) and to confirm female participants were not pregnant (Fisher Healthcare, Pittsburg, PA). Nude and clothed body masses were measured with a platform scale (Mettler Toledo PBD655-BC120, Toledo, OH) and height was measured with a stadiometer (Detecto, Webb City, MO). Total body surface area (TBSA) was calculated based on body mass (in kg) and standing height (in meters) as (17):
Rectal temperature (Trec) was measured using a general-purpose thermocouple probe inserted approximately 10 cm beyond the anal sphincter (Mon-a-therm, Mallinckrodt Medical, St. Louis, MO). Heart rate (HR) was obtained from an electrocardiogram (ECG; GE Medical Systems, Madison, WI). Trec and HR were recorded at a sampling frequency of 25 Hz (Biopac MP150, Santa Barbara, CA). Systolic (SBP) and diastolic (DBP) arterial blood pressures were measured with an automated electrosphygmomanometer (Tango+, SunTech Medical, Raleigh, NC), and mean arterial pressure (MAP) was calculated as ((SBP/3) + (DBP · 2/3)). Thermal sensation was assessed using an 8-point scale with 0.5-point increments (0.0 “unbearably cold” to 8.0 “unbearably hot”) (18). Ratings of perceived exertion (RPE) were assessed using the Borg scale (6 to 20 units) (19). After calibration according to the manufactureŕs instructions, expired gases and volumes were measured via open-circuit spirometry and analyzed using a metabolic cart (True-One 2400, Parvo Medics Inc., Salt Lake City, UT) to determine rates of oxygen uptake (VO2) and carbon dioxide production (VCO2). Metabolic rate (M) was calculated by indirect calorimetry from VO2 and the respirational exchange ratio (RER):
Where is the caloric equivalent per liter oxygen for oxidation of carbohydrates (21.12 (kJ· l−1 O2)) and is that of fat (19.61 (kJ· l−1 O2)). The rate of external work (Wk) was calculated as:
where 9.81 (m·s−2) is acceleration due to gravity and 2.237 is a conversion factor to convert US Standard units to Metric units (mph to m/s). The rate of metabolic heat production was taken as the difference between metabolic rate and external work rate.
To replicate the effect of a burn injury on impaired evaporative heat loss, absorbent material with a vapor-impermeable exterior was placed on the torso. By trapping sweat within the absorbent material, evaporative cooling was effectively prevented (8, 20). After estimating a participant’s TBSA, absorbent patches were cut to 20% of TBSA and placed around the entire trunk. The absorbent material was held in place using surgical tape and a stress test elastic vest retainer (Surgilast, Derma Sciences, Princeton, NJ).
Experimental Protocol
Three experimental trials were completed in a randomized counterbalanced order at the same time of day, separated by at least 48 hours, in which participants wore: a combat uniform (both pants and shirt), tactical vest with replica torso armor plates, socks, and running shoes (Uniform); combat uniform, tactical vest with replica torso armor plates (7.12 ± 0.16 kg total mass), socks, and running shoes with a 20% simulated burn injury imposed on the torso (Uniform + Burn); or only shorts, socks, underwear, shoes and sports bra for females (Control). Prior to the first trial, the subjects underwent medical screening including a 12-lead ECG and supine blood pressure measurements. Before each trial, participants were asked to refrain from exercise and alcohol intake for 24 hours, caffeine for 12 hours, and anti-inflammatory drugs 36 hours. Participants were also instructed to consume a light meal with 500 ml of water 3 hours prior to the trial. Urine specific gravity was assessed shortly after arrival at the laboratory, with a value of ≤1.025 accepted as euhydrated (21). Participants recorded their nude body mass and then dressed in athletic shorts, socks, running shoes, and a sports bra for female participants. After instrumentation, participants donned the combat uniform (both pants and shirt) and tactical vest with replica armor plates in the Uniform and Uniform + Burn trials. An instrumented and clothed body mass was then collected. Participants entered an environmental chamber, which was regulated at 40.0 ± 0.1°C and 20.0 ± 0.6% relative humidity throughout experimentation. Baseline measurements were obtained with the subjects standing on the treadmill. Exercise then commenced at a treadmill speed of 5.3 km·h−1 and an initial incline between 2% and 4%. Expired gases were collected for 3 min of rest and during exercise between 0–10, 25–35 and 50–60 min. In each trial, the grade of the treadmill was adjusted, as needed, to target the desired mass-specific rate of metabolic heat production of 6.0 W·kg−1. This exercise intensity was selected as it represents the metabolic demand associated with a military foot patrol (22). Whole-body sweat loss was calculated as the difference in nude body mass before and after the trial minus the water ingested during the trial, with correction for respiratory and metabolic mass exchange (23). Due to a technical issue, one participantś whole-body sweat loss could not be measured in a trial, and that measure was therefore excluded from the whole-body sweat loss analysis. Arterial blood pressures were collected at baseline and at 15-min intervals throughout exercise. Thermal sensation and RPE were obtained every 20 min.
Data and Statistical Analyses
Trec and HR are represented as 2-min averages at each time point. A one-way repeated measures analysis of variance (ANOVA) compared whole-body sweat loss, and rates of metabolic heat production between trials. Time-dependent measures were compared using two-way repeated-measures analysis of variance (ANOVA) with the independent factors of time (time points: 0, 15, 30, 45, and 60 min for Trec, and HR; 20, 40, and 60 min for thermal sensation and RPE) and condition (Control, Uniform, Uniform + Burn). A Bonferroni correction was applied for post-hoc multiple comparisons. Statistical analyses were performed with Prism 8 (GraphPad Prism version 8.2.0, San Diego, CA). Data are reported as mean ± standard deviation. Alpha was set at the 0.05 level.
RESULTS
All individuals were able to complete the 60 min of exercise in each trial. The rate of metabolic heat production was not different between the two uniformed trials (Uniform: 6.0 ± 0.3 W·kg–1; Uniform + Burn: 6.0 ± 0.3 W·kg–1; P = 0.84), while the control trial was slight lower compared to the uniformed trials (5.8 ± 0.3 W·kg–1; P ≤ 0.03). The average coefficient of variation for the rate of metabolic heat production per kg body mass (W·kg–1) between participants for the three trials was 3.1 ± 1.7%.
Trec increased from baseline (Control: 36.62 ± 0.4°C; Uniform: 36.65 ± 0.4°C; Uniform + Burn: 36.62 ± 0.3°C; P ≥ 0.96) during exercise (main effect of time: P < 0.001) and this increase was significantly influenced by the clothing conditions (interactive effect: P < 0.001) (Fig. 1). By 60 min of exercise, Trec increased to a greater extent in the Uniform and Uniform + Burn trials compared to Control (P ≤ 0.002). However, the 60-min change in Trec was not different between the two uniformed trials (P > 0.99).
Figure 1—
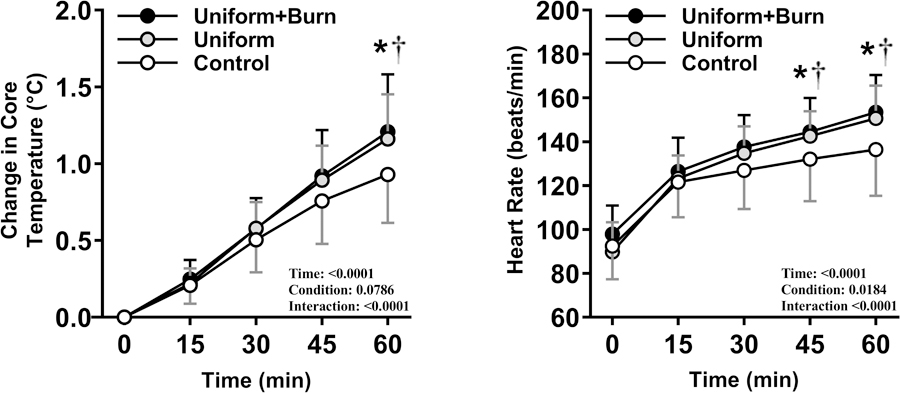
The change in core temperature (left) and heart rate (right) throughout exercise at 40°C and 20% RH while wearing a military combat uniform (Uniform), a military combat uniform with a simulated burn injury (Uniform + Burn), or shorts and shoes with females also wearing a sports bra (Control). * difference between Control and Uniform + Burn (P < 0.05). † difference between Control and Uniform (P < 0.05). Values are mean ± SD for 10 participants.
Whole-body sweat losses were 880 ± 120 g, 1144 ± 165 g, and 1174 ± 210 g in the Control, Uniform, and Uniform + Burn trials, respectively. A significant effect of condition was observed for whole-body sweat loss, with differences being evident between Control and Uniform (P < 0.001) and between Control and Uniform + Burn trial (P < 0.001), but not between the two uniformed trials (P > 0.99).
HR increased throughout the protocol (main effect of time: P = 0.02) and was significantly affected by the clothing conditions (interactive effect: P < 0.001). In the two Uniformed trials, HR was greater compared to Control at 45 and 60 min (P ≤ 0.01), but no difference between Uniform and Uniform + Burn trials was observed at any time (P ≥ 0.08) (Fig. 1). MAP responses were unaffected by the clothing ensembles (interactive effect: P = 0.76).
RPE were higher in Uniform compared to Control at every time point (P ≤ 0.01), and were different between Control and Uniform + Burn at 60 min (P < 0.03). That said, there were no differences in RPE between Uniform and Uniform + Burn trials at any time (P ≥ 0.13) (Fig. 2). Thermal sensation increased over time (main effect of time: P < 0.001) but without an interactive effect (P = 0.10). There was also a main effect of Condition for thermal sensation (P = 0.012), with post-hoc evaluations revealing differences between Control and both Uniform and Uniform + Burn trials (P<0.001) but not between Uniform and Uniform + Burn trials (P = 0.20; Fig. 2).
Figure 2—
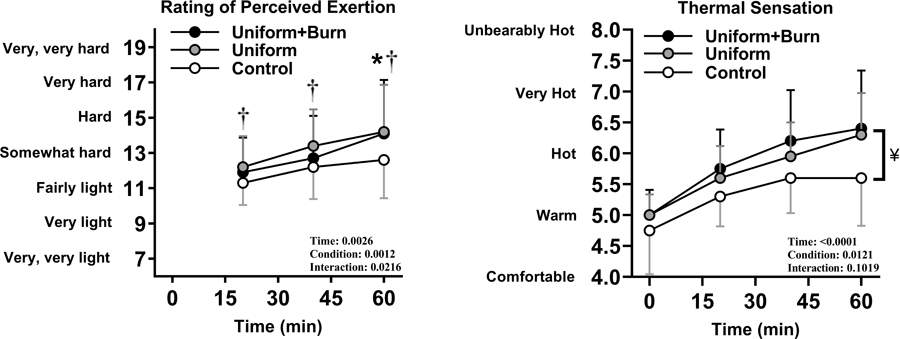
Rating of perceived exertion (left) and thermal sensation (right) throughout exercise at 40°C and 20% RH while wearing a military combat uniform (Uniform), a military combat uniform with a simulated burn injury (Uniform + Burn), or shorts and shoes with females also wearing a sports bra (Control). * difference between Control and Uniform + Burn (P < 0.02). † difference between Control and Uniform (P < 0.05). ¥ main effect differences between Control and both Uniform and Uniform + Burn for thermal sensation. There were no main effect differences between Uniform and Uniform + Burn for this variable. Values are mean ± SD for 10 participants.
DISCUSSION
The aim of this study was to investigate whether the detrimental effects of a burn injury underneath a protective ensemble is similar when military protective clothing was worn during exercise-heat stress. Compared to a seminude condition (Control), wearing a combat uniform (Uniform) exaggerates the increase in core temperature during 60 min of exercise-heat stress. However, when a simulated torso burn was imposed (Uniform + Burn), the elevation in core temperature did not differ from the non-burned Uniform trial. Similarly, elevations in HR and RPE were higher in Uniform compared to Control, but did not differ from Uniform + Burn trials. These findings indicate that a simulated torso burn injury of 20% TBSA does not cause any additional thermoregulatory burden during exercise in the heat, relative to solely wearing protective clothing.
During uncompensable heat stress, the magnitude of the elevation in core temperature reflects the net difference over time between the rate of combined environmental and metabolic heat gain (when environmental temperature is greater than skin temperature) and the maximal rate of evaporative heat loss (24, 25); the latter of which is strongly influenced by clothing vapor resistance. The increase in Trec was 0.23°C (~25%) greater in the Uniform trial relative to the Control trial (Fig. 1). Although a very small (perhaps undetectable) component of that Trec difference may be due to a slightly lower average rate of metabolic heat production in the Control trial, the observed core temperature difference predominately reflects the high clothing vapor resistance, and thus the lower potential for evaporative heat loss, of the uniform trials. This finding is consistent with previous studies involving equivalent work duration, similar work intensities, and hot-dry conditions, thus reaffirming that military protective clothing has detrimental thermoregulatory effects in the heat (13, 26, 27). Our key finding, however, was that when a 20% TBSA torso simulated burn injury was imposed underneath protective clothing in the Uniform + Burn trial, the change in Trec after 60 min of exercise-heat stress was not different to that observed in the Uniform trial (i.e., without a simulated burn injury) (Fig. 1). Since the rate of metabolic heat production and environmental conditions were matched between Uniform and Uniform + Burn trials, the absence of any difference in Trec responses indicates that the simulated burn injury in Uniform + Burn does not exacerbate the detrimental effect of wearing a clothing ensemble with low vapor permeability, and thus did not further reduce the potential for evaporative heat loss beyond the Uniform trial. This finding suggests that burn survivors with extensive skin grafting across the torso are likely to be at no greater risk for a heat-related illness during short periods of uncompensable heat stress if protective clothing with high vapor resistance is worn.
Similar to the Trec responses, whole-body sweat losses were higher in the uniformed trials compared to the Control trial. This finding is primarily explained by a reduction in evaporative potential since sweat loss depends on overall heat load and the evaporative cooling capacity (28). Importantly, the absence of difference in whole-body sweat loss between the two uniformed trials supports our contention that evaporative potential is not further altered by the ~20% TBSA simulated burn.
HR for the Control trial was lower than the two uniformed groups in the last half of the trial, indicating greater cardiovascular strain in the uniform trials (Fig. 1). Further, the magnitude of cardiovascular drift – the progressive rise in HR during prolonged exercise (29) – was attenuated in Control compared to the uniformed trials, but was not different between uniformed trials (Fig. 1). Greater cardiovascular drift, and the attendant rise in perceived exercise intensity associated with prolonged exercise-heat stress, impair physical performance (30, 31). Based on the HR responses observed herein, a burn injury covered by a protective clothing ensemble is unlikely to exacerbate cardiovascular strain or reduce work performance compared to a non-injured individual wearing the same ensemble.
RPE is highly associated with increases in core temperature and HR during exercise at a constant work intensity (32, 33). RPE responses in this study were higher in the two uniformed trials compared to the Control trial, which is consistent with previous findings (32, 33). The subjective estimate of thermal sensation correlates well with mean skin temperature (34). The participants in this study found the environmental conditions to be “warm” upon entry into the environmental chamber, and thermal sensation increased throughout exercise. Subsequent evaluation revealed a slightly higher rating of thermal perception for both the Uniform and the Uniform + Burn trails, both relative to the Control trial. However, an absence of a difference in thermal sensation between the Uniform and Uniform + Burn trials suggests that the combination of a torso burn injury and the evaluated clothing ensemble does not further increase thermal sensation over the clothing ensemble alone.
Perspectives
The Standards of Medical Fitness for the U.S. Army and the U.S Department of Defense exclude individuals with significant thermoregulatory dysfunction (16, 35). These standards state that “extensive burns on the torso will most significantly impair heat dissipation” (16). On the surface, this standard seems appropriate given that some of the highest regional sweat rates are located on the torso, particularly along the spinal column, over the scapulae, and at the lower back (36). More recently, United States Department of Defense’s Medical Standards for Appointment, Enlistment, or Induction into the Military Services have determined that, “Prior burn injury involving 18 percent or more body surface area (including graft sites)” does not meet the standard. These Standards formed the basis for the present investigation. In contrast to these standards, in the present investigation core temperature responses at a fixed rate of metabolic heat production were similar between Uniform and Uniform + Burn trials. Thus, a 20% TBSA burn injury on the torso is unlikely to further impair heat dissipation when protective clothing with low vapor permeability is worn. Based on these observations, the US Army and the Department of Defense should consider re-evaluating medical standards pertaining to burned soldiers, focusing on the amount of non-injured skin that is available for heat dissipation(5), rather than the anatomical location and %TBSA injured, when determining whether a soldier or recruit with a burn injury meets their Standard (5).
Considerations
The current study was not conducted in individuals with a burn injury but rather in healthy non-injured individuals. This trial would have been extremely difficult to perform appropriately in burn survivors as the regional distribution of a burn injury will differ greatly between individuals (37). Other factors, like heat acclimatization and aerobic capacity, the latter of which is disproportionately low in burn survivors compared with age-matched normative values (38), would further make a reasonable comparison between actual burn survivors and non-burned control individuals difficult. Thus the within-subject design of the current study minimizes the variability that would otherwise occur had a cross-sectional study been performed.
The hot, low-humidity environmental conditions in this study caused the skin-air gradient to favor dry heat gain, resulting in a higher evaporative heat loss requirement. At higher humidity levels, maximum evaporation is further reduced, making it harder to evaluate whether a burn injury would impact core temperature regulation. The employed environmental conditions maximized the chances that we would see differences in core temperature between the uniformed trials. Regardless, the interpretation of the findings are constrained to a high heat and low humidity environment. That said, due to the level of vapor impermeability and high thermal insulation posed by the employed uniform, we proposed that the thermoregulatory strain between uniformed burn-injured and uniformed non-burn-injured trials would probably be the same regardless of ambient temperature and humidity. A different clothing ensemble, consisting of a semi-permeable garment to allow for greater evaporative potential, would perhaps be of greater advantage to the non-burned individuals than those with burn injuries.
The required exercise workload was selected to be similar to moderate intensity duties that a soldier may be required to perform (39, 40). We cannot comment on whether similar results would have been observed should a higher or lower intensity workload been performed.
In the contemporary operational environment, modular scalable armor is often used, allowing soldiers to tailor their protection accordingly to the anticipated level of risk (12). If the threat of a ballistic or fragmentation injury is high, armor may be reconfigured to cover a larger body surface area, but at the expense of thermoregulatory capacity. If the threat level is low, armor can be scaled down to minimize the thermoregulatory penalty. In contrast to those operational options, only one combat uniform ensemble was tested in this study. A different armor configuration may evoked different rate of heat storage, as the surface area of coverage would be different.
CONCLUSION
In summary, a 20% TBSA simulated torso burn injury does not exacerbate thermoregulatory strain during exercise in a hot-dry environment while wearing a military combat uniform. These findings demonstrate that soldiers with burn injury to the torso are at no additional risk of heat strain compared to non-injured soldiers when both are wearing the same military combat ensemble. In light of these findings, the US Army’s Standards of Medical Fitness (16), stating that an extensive torso burn “will most significantly impair heat dissipation”, may require re-evaluation.
ACKNOWLEDGEMENTS
We sincerely thank all the study volunteers for their participation. This work was supported by awards from the Department of Defense (W81XWH-15-1-0647 to CGC), National Institutes of Health (R01GM068865 to CGC), and a Natural Sciences and Engineering Research Council of Canada Postdoctoral Fellowship (to MNC).
Footnotes
CONFLICTS OF INTEREST
The authors have no conflicts of interest to disclose. The results of the study are presented clearly, honestly, and without fabrication, falsification, or inappropriate data manipulation, and the results of the present study do not constitute endorsement by ACSM.
REFERENCES
- 1.Davis SL, Shibasaki M, Low DA et al. Impaired cutaneous vasodilation and sweating in grafted skin during whole-body heating. J Burn Care Res 2007; 28 (3): 427–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Davis SL, Shibasaki M, Low DA et al. Sustained impairments in cutaneous vasodilation and sweating in grafted skin following long-term recovery. J Burn Care Res 2009; 30 (4): 675–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cramer MN, Moralez G, Huang MU, Crandall CG. No thermoregulatory impairment in skin graft donor sites during exercise-heat stress. Med Sci Sports Exerc 2019; 51 (5): 868–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.McGibbon B, Beaumont WV, Strand J, Paletta FX. Thermal regulation in patients after the healing of large deep burns. Plast Reconstr Surg 1973; 52 (2): 164–70. [DOI] [PubMed] [Google Scholar]
- 5.Ganio MS, Schlader ZJ, Pearson J et al. Nongrafted skin area best predicts exercise core temperature responses in burned humans. Med Sci Sports Exerc 2015; 47 (10): 2224–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ganio MS, Gagnon D, Stapleton J, Crandall CG, Kenny GP. Effect of human skin grafts on whole-body heat loss during exercise heat stress: a case report. J Burn Care Res 2013; 34 (4): e263–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Davis SL, Shibasaki M, Low DA et al. Skin grafting impairs postsynaptic cutaneous vasodilator and sweating responses. J Burn Care Res 2007; 28 (3): 435–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cramer MN, Moralez G, Huang M, Kouda K, Poh PYS, Crandall CG. Exercise thermoregulation with a simulated burn injury: impact of air temperature. Med Sci Sports Exerc 2019; 52 (3): 712–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.McLellan TM, Havenith G. Protective clothing ensembles and physical employment standards. Appl Physiol Nutr Metab 2016; 41 (6 Suppl 2): S121–30. [DOI] [PubMed] [Google Scholar]
- 10.McLellan TM, Daanen HA, Cheung SS. Encapsulated environment. Compr Physiol 2013; 3 (3): 1363–91. [DOI] [PubMed] [Google Scholar]
- 11.Havenith G, Holmer I, den Hartog EA, Parsons KC. Clothing evaporative heat resistance--proposal for improved representation in standards and models. Ann Occup Hyg 1999; 43 (5): 339–46. [PubMed] [Google Scholar]
- 12.Potter AW, Gonzalez JA, Karis AJ, Xu X. Biophysical assessment and predicted thermophysiologic effects of body armor. PLoS One. 2015; 10 (7). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Caldwell JN, Engelen L, van der Henst C, Patterson MJ, Taylor NA. The interaction of body armor, low-intensity exercise, and hot-humid conditions on physiological strain and cognitive function. Mil Med 2011; 176 (5): 488–93. [DOI] [PubMed] [Google Scholar]
- 14.Roskind JL, Petrofsky J, Lind AR, Paletta FX. Quantitation of thermoregulatory impairment in patients with healed burns. Ann. Plast. Surg 1978; 1: 172–6. [DOI] [PubMed] [Google Scholar]
- 15.Wolf SE, Kauvar DS, Wade CE et al. Comparison between civilian burns and combat burns from Operation Iraqi Freedom and Operation Enduring Freedom. Ann Surg 2006; 243 (6): 786–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Department of the Army. Army Regulation 40–501 Standards of medical fitness. 2011.
- 17.DuBois D, DuBois EF. Fifth paper the measurement of the surface area of man. Arch Int Med 1915; 15 (5): 868–81. [Google Scholar]
- 18.Gagnon D, Romero SA, Cramer MN et al. Age Modulates Physiological Responses during Fan Use under Extreme Heat and Humidity. Med Sci Sports Exerc 2017; 49 (11): 2333–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Borg GA. Psychophysical bases of perceived exertion. Med Sci Sports Exerc 1982; 14 (5): 377–81. [PubMed] [Google Scholar]
- 20.Cramer MN, Moralez G, Huang M, Kouda K, Poh PYS, Crandall CG. Exercise core temperature response with a simulated surn injury: effect of body size. Med Sci Sports Exerc 2019; 52 (3): 705–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Cheuvront SN, Ely BR, Kenefick RW, Sawka MN. Biological variation and diagnostic accuracy of dehydration assessment markers. Am J Clin Nutr 2010; 92 (3): 565–73. [DOI] [PubMed] [Google Scholar]
- 22.Lau W, Roberts W, Forbes-Ewan C. Physiological performance of soldiers conducting long range surveillance and reconnaissance in hot, dry environments. Melbourne, Australia: DSTO Aeronautical and Maritime Research Laboratory. 1999.
- 23.Mitchell JW, Nadel ER, Stolwijk JA. Respiratory weight losses during exercise. J Appl Physiol 1972; 32 (4): 474–6. [DOI] [PubMed] [Google Scholar]
- 24.Havenith G, Fiala D. Thermal indices and thermophysiological modeling for heat stress. Compr Physiol 2015; 6 (1): 255–302. [DOI] [PubMed] [Google Scholar]
- 25.Ravanelli N, Cramer M, Imbeault P, Jay O. The optimal exercise intensity for the unbiased comparison of thermoregulatory responses between groups unmatched for body size during uncompensable heat stress. Physiol Rep 2017; 5 (5). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Taylor NA, Burdon CA, van den Heuvel AM et al. Balancing ballistic protection against physiological strain: evidence from laboratory and field trials. Appl Physiol Nutr Metab 2016; 41 (2): 117–24. [DOI] [PubMed] [Google Scholar]
- 27.Pope JI, Sleno NJ, McLellan TM et al. Heat stress of current in-service and proposed prototype rainsuits for the Canadian Forces. Defence R & D Canada-Toronto; 2003.
- 28.Shapiro Y, Pandolf KB, Goldman RF. Predicting sweat loss response to exercise, environment and clothing. Eur J Appl Physiol Occup Physiol 1982; 48 (1): 83–96. [DOI] [PubMed] [Google Scholar]
- 29.Ekelund LG, Holmgren A. Circulatory and respiratory adaptation, during alng-term, non-steady state exercise, in the sitting position. Acta Physiol. Scand 1964; 62 (3): 240–55. [DOI] [PubMed] [Google Scholar]
- 30.Periard JD, Cramer MN, Chapman PG, Caillaud C, Thompson MW. Cardiovascular strain impairs prolonged self-paced exercise in the heat. Exp Physiol 2011; 96 (2): 134–44. [DOI] [PubMed] [Google Scholar]
- 31.Ely MR, Cheuvront SN, Roberts WO, Montain SJ. Impact of weather on marathon-running performance. Med Sci Sports Exerc 2007; 39 (3): 487–93. [DOI] [PubMed] [Google Scholar]
- 32.Galloway SD, Maughan RJ. Effects of ambient temperature on the capacity to perform prolonged cycle exercise in man. Med Sci Sports Exerc 1997; 29 (9): 1240–9. [DOI] [PubMed] [Google Scholar]
- 33.Nybo L, Nielsen B. Perceived exertion is associated with an altered brain activity during exercise with progressive hyperthermia. J Appl Physiol 2001; 91 (5): 2017–23. [DOI] [PubMed] [Google Scholar]
- 34.Gagge AP, Stolwijk JA, Hardy JD. Comfort and thermal sensations and associated physiological responses at various ambient temperatures. Environ Res 1967; 1 (1): 1–20. [DOI] [PubMed] [Google Scholar]
- 35.Department of Defense. Instruction 6130.03 - Medical standards for appointment, enlistment, or inductioin Into the military services. 2018.
- 36.Smith CJ, Havenith G. Upper body sweat mapping provides evidence of relative sweat redistribution towards the periphery following hot-dry heat acclimation. Temperature. 2019; 6 (1): 50–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Henane R, Bittel J, Banssillon V. Partitional calorimetry measurements of energy exchanges in severely burned patients. Burns. 1981; 7 (3): 180–9. [Google Scholar]
- 38.Ganio MS, Pearson J, Schlader ZJ et al. Aerobic fitness Is disproportionately low in adult burn survivors years after injury. J Burn Care Res 2015; 36 (4): 513–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.The Department of the Army. TB MED 507/AFPAM 48–152: Heat stress control and heat casualty management. Washington, D.C: 2003. [Google Scholar]
- 40.Welles AP, Buller MJ, Margolis L, Economos D, Hoyt RW, Richter MW. Thermal-work strain during Marine rifle squad operations in Afghanistan. Mil Med 2013; 178 (10): 1141–8. [DOI] [PubMed] [Google Scholar]


