Abstract
Background
The incidence of septic arthritis is 2–10/100,000. Morbidity is higher with persistent joint dysfunction in up to 30%. Osteoarthritic knee with infection presents a rare challenge, with no established approach for treatment exists. We present our experience of managing infected degenerative joint disease (DJD) with two-stage primary arthroplasty similar to the management of periprosthetic joint infection.
Patients and methods
Four patients presented to us between 2016 and 2018 with advanced DJD associated with coexistent joint sepsis with or without adjacent osteomyelitis. The diagnosis of joint sepsis with periarticular osteomyelitis was made based on clinical presentation, radiographic findings, inflammatory serological markers, and culture of knee joint aspirate. All were operated with primary arthroplasty in two stages of debridement with a static spacer followed by antibiotics and implantation.
Discussion
With no established method of treating DJD superadded with infection, our experience adds valuable information in treating the same. Our 2-staged primary arthroplasty had a short antibiotic duration between stages, a mean of 63.5 days, and stopped within 3 days of 2ndstage reducing hospital stay, morbidity, and cost.
Our approach is a very viable method of treating infected DJD with a minimum drug holiday time of two weeks before implantation with a better outcome, reducing the recurrence rate of infection.
Though a small number with a minimum follow-up of 24 months, we believe we provide valuable additional information.
Conclusion
All patients had painless return to early activities with no signs of recurrent infection. Our approach is a very viable and could serve as a cost-effective method treatment for an infected arthritic knee.
Keywords: Septic knee, Osteoarthritis, Stage, Primary, TKR, MRI
1. Introduction
Infection of joints is a relatively uncommon condition that has been on a gradual rise, especially in adults, owing to a surge in invasive procedures associated with immunocompromised status.1 The incidence of septic arthritis is reported to be 2–10 per 100,000 patients with a higher rate being noted in elderly and young children.1 The morbidity associated with this condition is substantially high with persistent joint dysfunction in up to 30% of the patients.2
An osteoarthritic knee superadded with infection, as septic arthritis or with additional periarticular osteomyelitis, presents a further challenge to the orthopaedician. The treatment should be aimed at providing a painless, functional joint without the risk of recurrence of infection. The increasing expectations of patients with respect to early return to pain-free activities pose a further challenge.
Currently, there is no established approach for the treatment of DJD with sepsis. We present our experience of managing infected DJD with two-stage primary arthroplasty similar to the management of periprosthetic joint infection.
2. Patients and methods
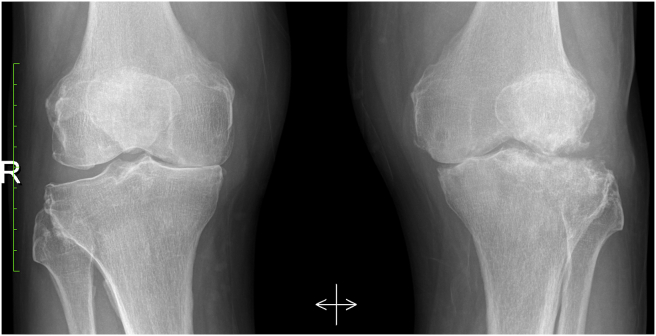
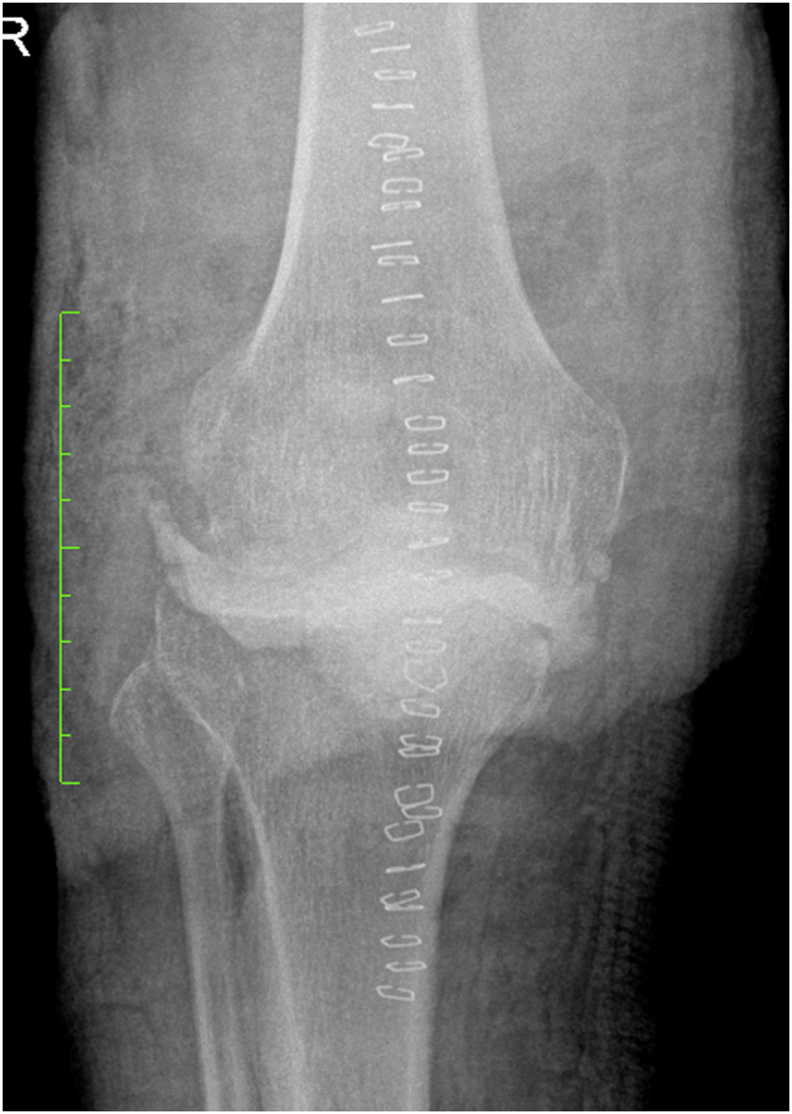
A series of four patients who presented with advance DJD with joint sepsis with or without osteomyelitis between January 2016 and December 2018, were followed up for a minimum of 24 months. The diagnosis of joint sepsis or periarticular osteomyelitis was based on clinical presentation, radiographic and MRI findings, inflammatory serological markers, and culture of knee joint aspirate (Fig. 1A, Fig. 1B, Fig. 1C, Fig. 1D, Fig. 1E).
Fig. 1A.
Pre-operative X-ray of knee AP view.
Fig. 1B.

Pre-operative X-ray of knee lateral view.
Fig. 1C.

Pre-operative coronal view CT image with tibial plateau bone loss.
Fig. 1D.
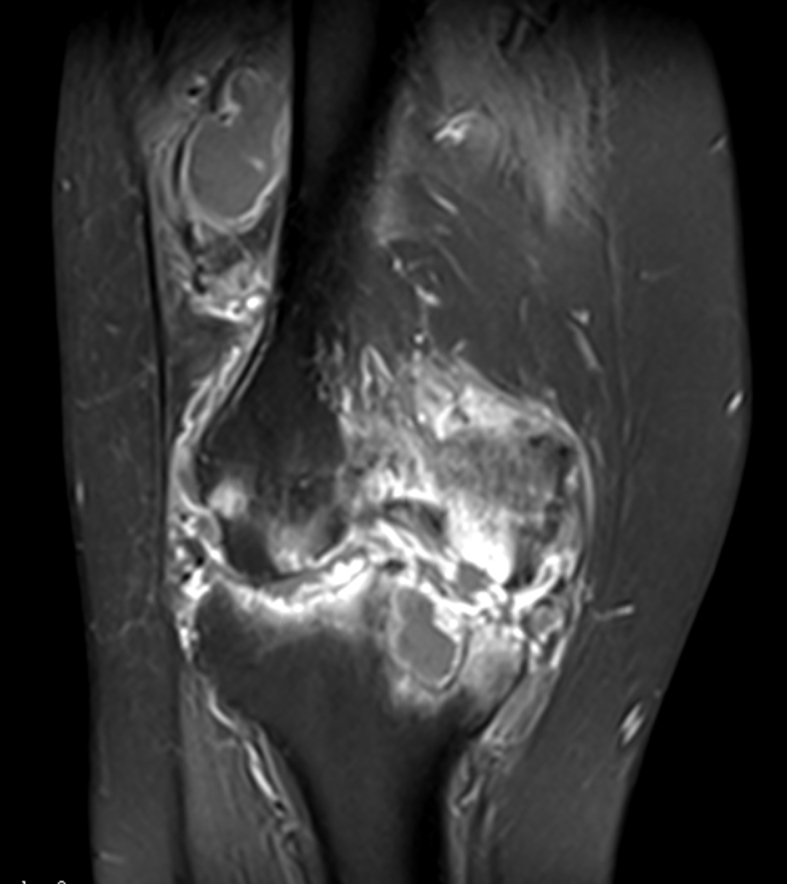
Pre- operative coronal view MRI T1 STIR image.
Fig. 1E.
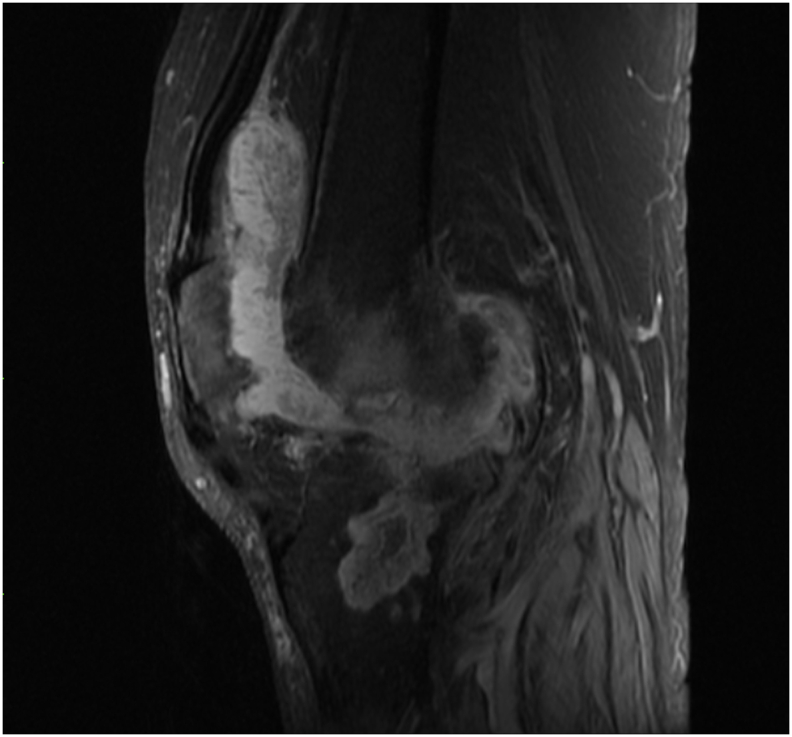
Saggital view MRI proton density fat saturation image.
All of them had joint sepsis, one of whom had additional proximal tibial osteomyelitis and the extent of bony involvement assessed with MRI. All the patients had a history of previous invasive procedures involving the affected knee - two patients had received an intra-articular injection; one patient had undergone knee arthroscopy and one patient had undergone proximal tibial plating, which we believe to be the likely cause of the infection.
The pre-operative assessment included a joint range of motion (ROM), radiological examination with a weight-bearing posteroanterior view, full length weight bearing and lateral radiographs of the knee, and blood parameters including total and differential white cell count, ESR, and CRP.
Approval from the Institutional Ethical committee board was taken, and patients consented for the procedure after being explained the same. The patients also consented for the publication.
3. Surgical technique
3.1. First stage
Using the conventional medial parapatellar approach the knee was exposed without inflating the tourniquet under spinal anesthesia. Six to eight biopsy samples involving the synovium and bone were taken from the different compartments of the knee and from suspicious tissues. Extensive debridement done debriding the knee of all necrotic soft tissue (Fig. 2A, Fig. 2B). After inflating the tourniquet based on the radiological imaging, the bone cuts of the distal femur and proximal tibia done with jig resecting up to the normal healthy bone in all the patients extramedullary. The femoral cut was done with the trochlear notch as the reference and the cartilage covering of posterior condyle was curetted/burred. A betadine wash given for 5 min. Two batches of 40 g of PMMA cement Palacos1 R (Biomet Inc, Warsaw, IN, USA) were each mixed with 4 g of Vancomycin and 1 g of Gentamycin. Cement spacer was molded by hand each for femur, tibia, and placed without any pressure when in a late doughy state to prevent complete bonding (Fig. 3A, Fig. 3B).
Fig. 2A.
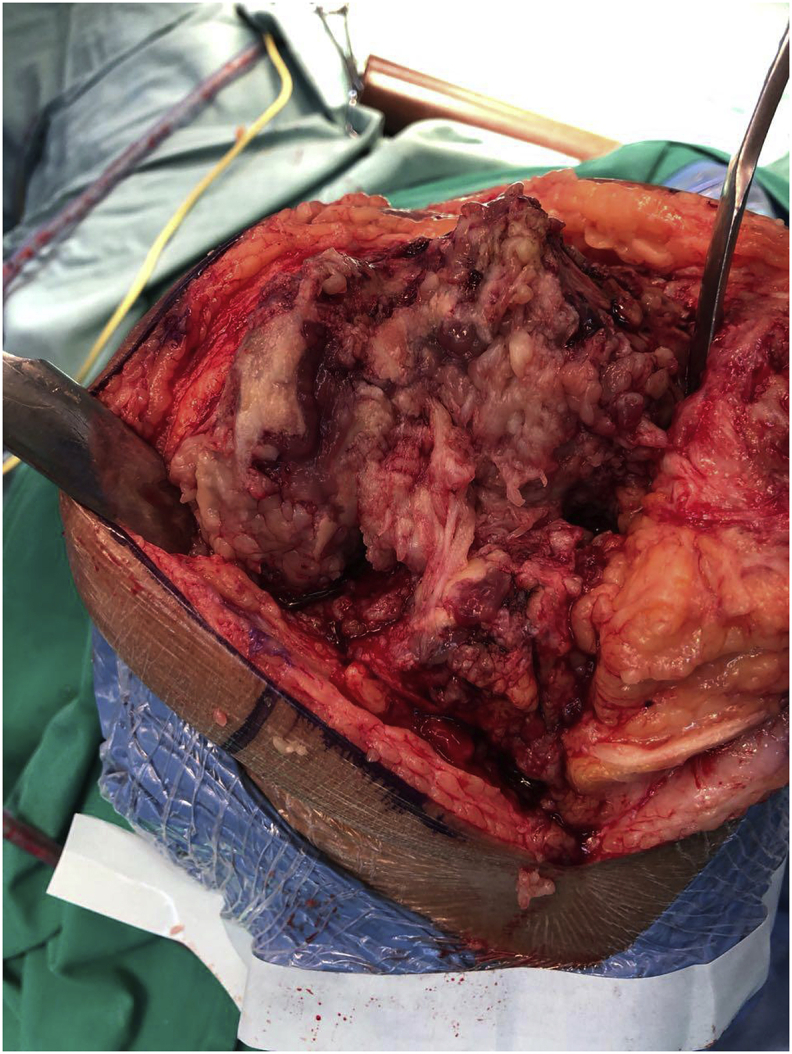
Image showing the infected knee with necrotic tissue after arthrotomy.
Fig. 2B.
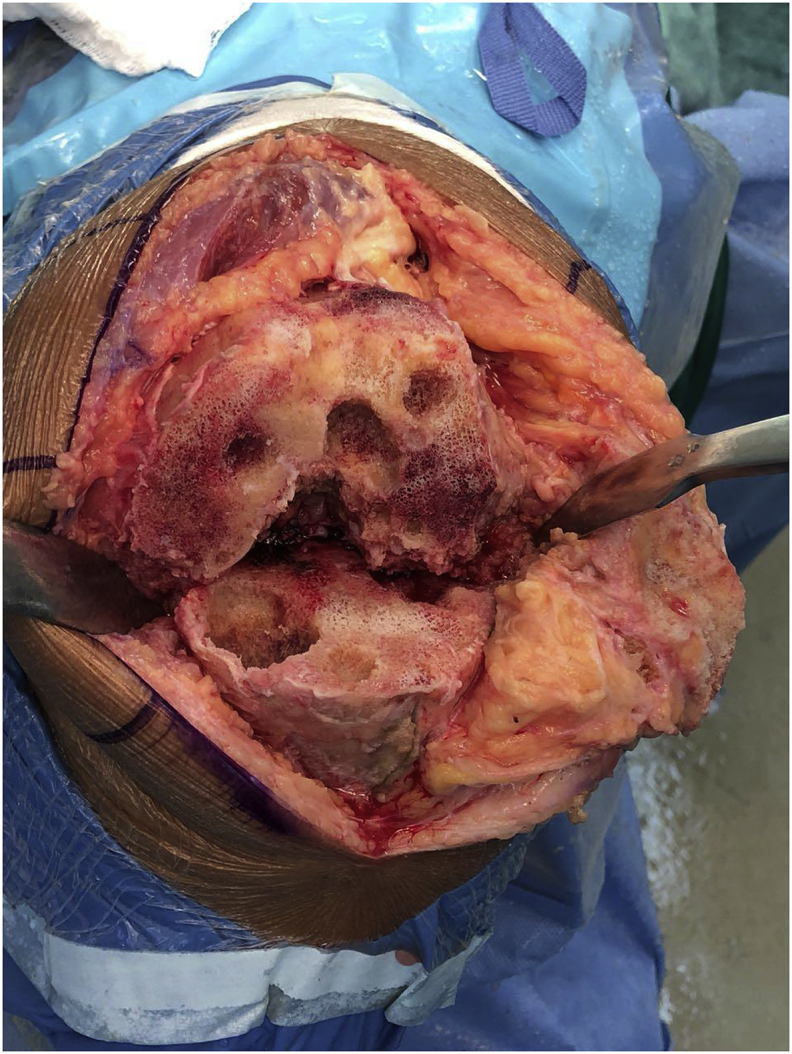
Image post debridement and extensive synovectomy.
Fig. 3A.
X-ray AP view of knee with static spacer.
Fig. 3B.

X-ray lateral view of knee with static spacer.
Appropriate intravenous antibiotics followed by oral were instituted in consultation with the Infectious Diseases Team, based on pre-operative and intra-operative cultures. The patients were transferred to the nearest peripheral health center to complete the course of intravenous antibiotics.
All patients were allowed toe-touch weight-bearing with a brace locked in extension.
Following the completion of the antibiotic course, patients were on a routine two weekly follow-up for clinical assessment and blood parameters – total and differential white cell count, ESR, and CRP. On return of inflammatory markers to normal, the antibiotics were stopped immediately. Patients received a minimum of 2 weeks drug holiday time. Inflammatory markers were later reassessed again, if in the normal range then progressed to stage 2. In case the inflammatory markers were still elevated, antibiotics were continued till markers were in the normal range.
3.2. Second stage
It consisted of removing the spacer, refreshing the bone cuts, and making the new posterior femoral cut if there were no apparent signs of infection/collection. Patients were counseled prior to the possibility of abandoning the surgery if there was evidence of persistent infection. Intra-operative swabs were collected without awaiting the results, which however were negative for gram staining and growth. TKA was performed with the standard anterior/posterior referencing and a posterior-stabilized prosthesis implanted after adequate ligament balancing and equalization of flexion and extension gaps. Patella was not resurfaced as a routine for primary TKA at our institution. The Persona, NexGENR, LegacyR Constrained Condylar Knee (LCCK) system (Zimmer Inc, Warsaw, IN, USA) used with antibiotic-impregnated bone cement which includes 0.5 g active gentamycin for each batch (Fig. 4A, Fig. 4B, Fig. 4C, Fig. 4D).
Fig. 4A.

LCCK AP view at 2 year follow-up.
Fig. 4B.

LCCK lateral view at 2 year follow-up.
Fig. 4C.
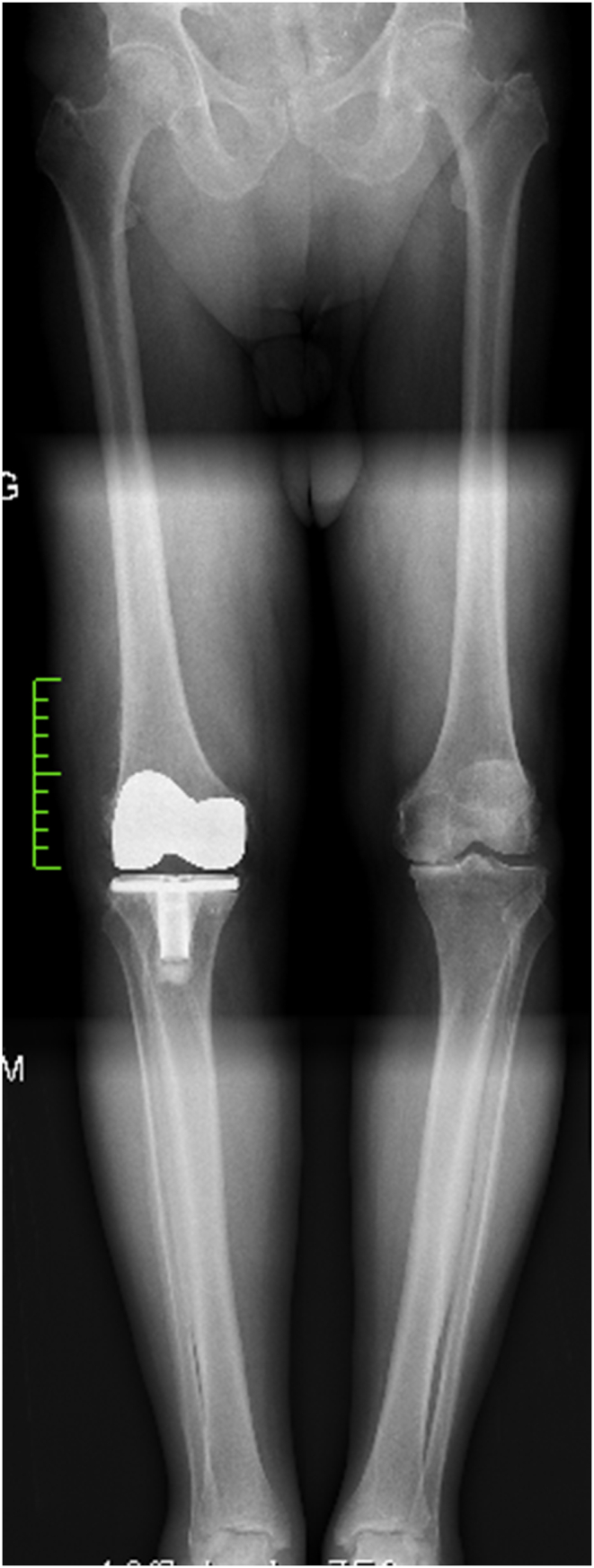
Persona knee full length AP view at 2 year follow-up.
Fig. 4D.

Persona knee lateral view at 2 year follow-up.
Postoperative antibiotics were given for 3 days, till the intra-operative results of the 2nd stage was available. Post-implantation routine evaluation was done at 2, 4, 6 and 12weeks interval with clinical assessment and inflammatory marker assessment.
4. Results
All patients were male, the mean age was 62.75 years with a range of 56–66years. Three patients had conditions that could compromise immunity; two patients were diabetic, and one was an asthmatic on long-term steroid intake. Three patients had elevated inflammatory serological markers at presentation, while one patient, who was on a course of antibiotics before being transferred to our institution, had normal inflammatory markers.
All patients had positive pre-operative culture results which was reconfirmed by the cultures collected at the 1st stage (Table 1).
Table 1.
Demographics and history of patients in the study.
| Case | Age/Sex | History | Duration of symptoms | Micro-organism on culture | Antibiotics IV (days) | Antibiotics Oral(weeks) |
Pre-op ROM | Time required for normal CRP aftedr 1st stage | CRP(mg/L) /ESR(mm/hr) before implantation |
AORI classification | Implant used | Oxford knee score at 2 yr follow-up | Final follow-up(months) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 56/M | Septic knee with proximal tibial osteomyelitis post tibial plating | 13 months | Staphylococcus aureus | Tazocin(3)+ Cloxacillin(14) | Cloxacillin + Rifampicin – 7 wk | 30–110 deg | 12wk | 1.94 mg/L 5 mm/h |
Type 3 | RHK with augment | 37 | 32 |
| 2 | 65/M | Septic arthritis following the previous arthroscopy | 3 months | Achromobacter denitrificans | Meropenem (18) | Cotrimoxazole 6wk | 30–120 deg | 10wk | 2 mg/L 12 mm/h |
Type 2 | RHK | 49 | 41 |
| 3 | 65/M | Septic arthritis with osteomyelitis proximal tibia following repeated Intra-articular injections | 4 months | Achromobacter xylosoxidans | Vancomycin(1)+ Meropenem (18) | Cotrimoxazole 12wk | 15–90 deg | 8wk | 2.99 mg/L 10 mm/h |
Type 2 | LCCK | 41 | 26 |
| 4 | 66/M | Septic arthritis following repeated Intra-articular injections | 4 months | Staphylococcus epidermidis | Meropenem(35) | 0–100 deg | 7wk | 0 mg/L 10 mm/h |
Type 1 | Persona | 46 | 40 |
The mean ROM of the knee pre-operatively was 86.2O (10–120°), which improved post-operatively to 112.5O (0–130°). All patients had negative cultures after definitive surgery. The mean Oxford knee score pre-operatively and post-operatively at 2years were 23 and 41 respectively. The mean duration of antibiotics after first stage was 63.5 days (35–93 days) and duration of intravenous antibiotics being 22.25 days (17–35 days). The mean interval between the two stages was 4.3 months, with a range of 3–7.2 months. The salient findings are tabulated in Table 1.
5. Discussion
No established guidelines exist for the treatment of arthritic knee superadded with infection in the demanding adults, while two-stage revision for knee replacement is an established practice as evidenced by multicentric studies but there are only a few articles that have studied two-stage revision for infective arthritis of the knee.3 With minimal options of treatment and an increasing need for an early return of functions, management of this condition, poses a big hurdle for surgeons and the public health care system. There are a few reports of treating arthritis with intractable infection by two-stage primary TKA. The associated incidence of prosthetic joint infection (PJI) is higher in patients with previously infected joint, with a reinfection rate of 5% in primary TKR.4, 5, 6, 7, 8 We report our experience of treating a small series of same.
Though with limitations of a small number of cases and with a minimum follow up of 2 years, we believe we provide valuable additional information.
While other authors have reported antibiotic administration of 6 weeks intravenously and a total antibiotic coverage of three to six months, our series needed a shorter antibiotic coverage of a mean 22.25 days intravenously and a mean 63.5 days of total duration of antibiotic coverage. The extended antibiotic coverage reported by other authors is likely to have resulted in prolonged hospital stay, higher morbidity, and the higher costs.4,6 Nevertheless, we were able test the absence of recurrence of infection by implementation of a drug holiday for a minimum of two weeks.
Our patients did not need long-term antibiotics after the 2nd stage of implantation. Prophylactic antibiotic chosen for the second surgery was dependent on the prior organisms grown and the sensitivity pattern. All the culture reports of all the patients turned out negative, following which antibiotics were discontinued. This is in contrast to other studies where antibiotics were routinely given for 3–6 months post-operatively.5, 6, 7
The mean interval between the two stages was 4.3 months (range: 3–7.2 months), which is comparable to the duration stated by Nazarian et al., who also used a similar static spacer and lesser than that of Shaikh et al. where an articulating spacer was used.4,6 Though infection eradication rates are comparable between articulating and static spacers, there is no evidence available on whether the type of spacer influences the infection eradication time.9 The use of static spacer, however, reduces the costs borne by the patients.
Our criteria of implantation in 2nd stage relied on a set of multiple factors: return of inflammatory serological markers to normal, drug holiday test of minimum two weeks, clinical signs that the knee is free of infection.10
Ghanem et al. and Stambough et al. have highlighted the need for multiple factors for assessing the eradication of infection before reimplantation in staged revision for infected knee arthroplasty in his prospective study.10,11
The role of serological inflammatory markers has long been debated, and their predictive value has been questioned, but various studies have shown that serial reduction and refinement of the threshold of markers is still a useful tool in screening infection.10,12,13
A drug holiday test of two weeks before implantation has been reported to reduce the rate of recurrence of infection.14,15 The implementation of the same in our series possibly contributed to good outcomes. Intra-operative testing for bacteria was not done in our series due to possibility of sampling errors, and poor reliability of Gram stain after a course of antibiotics and frozen section being inconclusive.13
Our technique is unique in not using intramedullary alignment guides during the first stage. This prevents breaching of the medullary canal. The trochlear notch was used as a reference, therefore, mitigating the chances of propagation of infection along the medullary canal in comparison to other reports where the medullary canal was breached.4,6 There was no recurrence of infection until final follow up in any of our patients. Similar results have been reported by other authors, however with longer course of antibiotics.4,6 At 2-year follow-up, the Oxford scores were better than preoperative scores and all patients were ambulant and satisfied with the outcome.
Though a small number with a minimum follow-up of 24 months, we believe that our technique and our series provide valuable information to this rare and challenging clinical condition.
6. Conclusion
All the patients in this series had painless return to early activities. At more than two years follow up, there were no signs of recurrence of infection with no prosthetic loosening or revisions. Substantially reduced duration of antibiotic course helps in reducing the morbidity of chronically infected patients. Staged primary knee replacement is a safe and reliable option for the treatment of infected DJD of the knee.
Declaration of competing interest
The authors have no affiliation with any organization with a direct or indirect financial interest in the subject matter discussed in the manuscript.
Contributor Information
Sam Supreeth, Email: supreethsam13@gmail.com.
Suwailim Al Ghanami, Email: dr_ghanami@yahoo.com.
Saseendar Shanmugasundaram, Email: ssaseendar@yahoo.co.in.
Raad Sabri Al Rawi, Email: dr_raad2000@yahoo.com.
Ali Redha Abdawani, Email: ali.abdwani@gmail.com.
Shenouda R. Abdelmasih, Email: shenodarezk@gmail.com.
References
- 1.García-arias Miriam, Balsa Alejandro, Mola Emilio Martín. Best practice & research clinical rheumatology septic arthritis. Best Pract Res Clin Rheumatol. 2011;25(3):407–421. doi: 10.1016/j.berh.2011.02.001. [DOI] [PubMed] [Google Scholar]
- 2.Ferrand Julien, El Samad Youssef, Brunschweiler Benoit. Morbimortality in adult patients with septic arthritis: a three-year hospital-based study. BMC Infect Dis. 2016;16(1):1–10. doi: 10.1186/s12879-016-1540-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Shanmugasundaram S., Ricciardi B.F., Briggs T.W.R., Sussmann P.S., Bostrom M.P. Evaluation and management of periprosthetic joint infection-an international, multicenter study. HSS J. 2014;10(1):36–44. doi: 10.1007/s11420-013-9366-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Nazarian D.G., De Jesus D., McGuigan F., Booth R.E. A two-stage approach to primary knee arthroplasty in the infected arthritic knee. J Arthroplasty. 2003;18(7 SUPPL. 1):16–21. doi: 10.1016/S0883-5403(03)00343-7. [DOI] [PubMed] [Google Scholar]
- 5.Kirpalani P.A., In Y., Choi N.Y., Koh H.S., Kim J.M., Han C.W. Two-stage total knee arthroplasty for non-salvageable septic arthritis in diabetes mellitus patients. Acta Orthop Belg. 2005;71(3) 315–20. [PubMed] [Google Scholar]
- 6.Shaikh A.A., Ha C.W., Park Y.G., Park Y.B. Two-stage approach to primary TKA in infected arthritic knees using intraoperatively molded articulating cement spacers. Clin Orthop Relat Res. 2014;472(7):2201–2207. doi: 10.1007/s11999-014-3545-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chang C.B., Chang M.J., Song M.K., Shin J.H., Yoon C., Kang S.B. Two-stage approach to total knee arthroplasty using colistin-loaded articulating cement spacer for vancomycin-resistant Pseudomonas aeruginosa infection in an arthritic knee. Eur J Orthop Surg Traumatol. 2019;29(1):227–230. doi: 10.1007/s00590-018-2268-x. [DOI] [PubMed] [Google Scholar]
- 8.Lee G.C., Pagnano M.W., Hanssen A.D. Total knee arthroplasty after prior bone or joint sepsis about the knee. Clin Orthop Relat Res. 2002;404:226–231. doi: 10.1097/00003086-200211000-00036. [DOI] [PubMed] [Google Scholar]
- 9.Ding H., Yao J., Chang W., Liu F. Comparison of the efficacy of static versus articular spacers in two-stage revision surgery for the treatment of infection following total knee arthroplasty: a meta-analysis. J Orthop Surg Res. 2017;12:151. doi: 10.1186/s13018-017-0644-6. Published 2017 Oct 17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ghanem E., Azzam K., Seeley M., Joshi A., Parvizi J. Staged revision for knee arthroplasty infection: what is the role of serologic tests before reimplantation? Clin Orthop Relat Res. 2009;467(7):1699–1705. doi: 10.1007/s11999-009-0742-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Stambough J.B., Curtin B.M., Odum S.M., Cross M.B., Martin J.R., Fehring T.K. Does change in ESR and CRP guide the timing of two-stage arthroplasty reimplantation? Clin. Orthop. Relat. Res. 2019;477(2):364–371. doi: 10.1097/01.blo.0000533618.31937.45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Alijanipour Pouya, Bakhshi Hooman, Parvizi Javad. Diagnosis of periprosthetic joint infection: the threshold for serological markers. Clin Orthop Relat Res. 2013;471(10):3186–3195. doi: 10.1007/s11999-013-3070-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kusuma S.K., Ward J., Jacofsky M., Sporer S.M., Della Valle C.J. What is the role of serological testing between stages of two-stage reconstruction of the infected prosthetic knee? Clin Orthop Relat Res. 2011;469(4):1002–1008. doi: 10.1007/s11999-010-1619-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chang M.C., Chang C.H., Tsai S.W., Hsu K.H., Chen W.M., Su Y.P. The efficacy of a drug holiday test on two-stage revision for infected total knee arthroplasty. J Chin Med Assoc: J Chin Med Assoc. 2019;82(6):500–504. doi: 10.1097/JCMA.0000000000000055. [DOI] [PubMed] [Google Scholar]
- 15.Preformed Articulating Knee Spacers in 2-Stage Total Knee Revision Arthroplasty. J Arthroplasty. 2012;27(8) doi: 10.1016/j.arth.2012.01.027. Minimum Follow-up et al. 1469–73. [DOI] [PubMed] [Google Scholar]