Abstract
Glutathione (GSH) was initially identified and characterized for its redox properties and later for its contributions to detoxification reactions. Over the past decade, however, the essential contributions of glutathione to cellular iron metabolism have come more and more into focus. GSH is indispensable in mitochondrial iron-sulfur (FeS) cluster biosynthesis, primarily by co-ligating FeS clusters as a cofactor of the CGFS-type (class II) glutaredoxins (Grxs). GSH is required for the export of the yet to be defined FeS precursor from the mitochondria to the cytosol. In the cytosol, it is an essential cofactor, again of the multi-domain CGFS-type Grxs, master players in cellular iron and FeS trafficking. In this review, we summarize the recent advances and progress in this field. The most urgent open questions are discussed, such as the role of GSH in the export of FeS precursors from mitochondria, the physiological roles of the CGFS-type Grx interactions with BolA-like proteins and the cluster transfer between Grxs and recipient proteins.
Keywords: glutathione, glutaredoxin, iron-sulfur cluster, iron
1. Introduction
Glutathione, the γ-l-glutamyl-l-cysteinyl-glycine tri-peptide, is a ubiquitous nucleophile required in redox homeostasis, detoxification, and iron homeostasis [1]. Since the reactivity of glutathione (GSH) itself with proteins, small molecules, and xenobiotics is too low to be significant in vivo, see for instance, [2], GSH-dependent reactions need to be catalyzed by enzymes. These enzymes include glutaredoxins (Grxs), glutathione peroxidases (GPxs), glutathione reductase (GR), glutathione S-transferases (GSTs), and protein disulfide isomerases (PDIs) [1]. Nevertheless, the functions of GSH depend on the reactivity of its cysteinyl thiol group. Thiols can complex metals, be alkylated to thioethers, but they can also be oxidized to disulfides. In the case of glutathione, two molecules of reduced GSH can be oxidized to form glutathione disulfide (GSSG). Re-reduction is catalyzed by GR at the expense of NADPH. Being present in millimolar concentrations in most organisms, GSH was characterized as the “redox buffer” of the cell. In fact, the loss of GSH-utilizing enzymes may result in disrupted redox homeostasis, as in the case for GPxs [3,4], with effects as dramatic as cell death by a process named ferroptosis induced by the lack of GPx4 activity [5,6,7]. The loss of glutathione itself, however, firstly results in defects in cellular iron homeostasis [8,9]. The enzymes that catalyze or mediate most glutathione functions in iron metabolism are the iron-sulfur cluster (FeS)-containing Grxs.
In this review, we will address the functions of both GSH and FeS-Grxs in iron metabolism. This topic has been addressed before, see for instance [9,10,11,12]. The focus of this review is on mammalian cells, however, we take into account other taxa when discussing ground-breaking and major findings, both to illustrate the high degree of conservation in the systems as well as some unique aspects.
2. Glutathione, Glutaredoxins, and Iron-Metabolism
As early as 1972, Tanaka and coworkers reported that, in vitro, GSH may be able to complex iron, resulting in absorption spectra resembling those of FeS clusters [13]. It took nearly two decades before the essential function of GSH in the synthesis and maturation of FeS cluster proteins in vivo was discovered in yeast. Defects in the biosynthesis of FeS proteins in Saccharomyces cerevisiae are associated with a more than two-fold increase of GSH [14]. However, this increase was apparently not caused by concomitant disturbances in redox metabolism. In fact, the depletion of GSH impaired the maturation of FeS proteins substantially, most of all affecting the non-mitochondrial FeS proteins [15].
2.1. Iron-Sulfur Cluster Biogenesis
FeS clusters are essential for life. They participate in the transfer of electrons, are cofactors in enzymatic catalysis, control the stability of biomolecules, and act as regulatory elements [16,17,18]. Mitochondria are essential for FeS cluster biogenesis. Not only are all the FeS clusters required for energy conversion synthesized here, the maturation of cytosolic FeS clusters also depends on a yet to be defined mitochondrial precursor [19,20]. Mitochondrial FeS cluster biogenesis and the cluster transfer to target apo-proteins have been studied to great detail and reviewed comprehensively before, e.g., in [21,22,23]. In brief, Fe2S2 centers are synthesized from iron and cysteine-derived sulfur by the early iron-sulfur cluster (ISC) synthesis machinery. From there, the Fe2S2 centers are likely transferred to the monothiol Grx5 with the aid of a heat shock protein of 70 kDa (Hsp70) chaperone system, the details of which will be discussed below. In the present models, Grx5 acts as a hub, from which the FeS centers are (1) either directly, or with the help of additional “targeting factors”, transferred to Fe2S2 target proteins or (2) transferred to a protein complex composed of the assembly factors ISCA1, ISCA2, and IBA57, where they are combined to Fe4S4 centers [24]. Only recently, Lill and co-workers succeeded in biochemically reconstituting the assembly of Fe4S4 clusters [25]. The process requires the ISC machinery, holo-Grx5, and reduced Fdx2 for the reductive fusion of two Fe2S2 clusters into one Fe4S4 cluster. These clusters are trafficked by ISC-targeting factors, such as proteins from the BolA family and iron-sulfur cluster scaffold homolog 1 (NFU1) to apo-target proteins such as the mitochondrial aconitase (ACO2). The maturation of the Fe4S4 centers in the complex I (NADH-ubiquinone oxidoreductase, NDUF) subunits NDUFS1, NDUFV1, and NDUFS2, 7, and 8 seems to require the P-loop NTPase Ind1 (iron–sulfur protein required for NADH-dehydrogenase) [26]. The molecular mechanisms of cluster insertion and the recipient protein pre-requisites are still unclear.
The insertion of FeS proteins into apo-target proteins requires their cysteinyl sulfur ligands to be in the reduced thiol state. Under normal conditions in yeast mitochondria, this seems to be independent of the major thiol reducing systems, i.e., the GSH/Grx and thioredoxin (Trx) systems [27]. However, for mammalian cells and proteins, a number of conditions have been characterized that lead to the oxidation of such cysteinyl residues, for instance, in complex I subunits NDUFS1 and NDUFV1 in a murine Parkinson’s disease model as a consequence of GSH depletion [28]. In general, GSH appears to be a crucial factor for complex I activity, especially in neurons [29,30,31].
From groundbreaking work in yeast cells, it was established that cytosolic FeS biogenesis depends on a sulfur compound generated inside mitochondria [32]. This not yet specified sulfur compound (X-S) must be exported as source for cytosolic FeS cluster synthesis. This compound must be transported into the cytosol in an ATP-dependent manner. The ATP-binding cassette (ABC) transporter Atm1 (in human ABCB7), located in the inner mitochondrial membrane, soon came into focus as the prime candidate for this function [32]. Atm1/ABCB7 may also be the link for the necessity of GSH for the maturation of cytosolic FeS proteins. Structural analyses revealed a large cavity in the dimeric Atm1 close to the inner membrane surface that can accommodate GSH [33,34,35]. In fact, the size of the cavity also allows for the binding of GSH as part of a larger not yet defined substrate transported by Atm1 [34]. Mutations in the binding site of ABCB7 that inhibit binding of a GSH moiety result in decreased functions of cytosolic FeS proteins and mitochondrial iron overload [33,36,37]. The same phenotype is caused by GSH or Atm1 depletion in yeast [15]. Atm1 and the Arabidopsis thaliana homolog ATM3 transport GSSG with increased ATPase activity but neither Fe2+ nor reduced GSH stimulate the ATPase activity of the transporter [38]. Atm1 also transports GS-S-SG (glutathione trisulfide) [38]. Since substantial data suggest that only a sulfur compound is required as the mitochondrial contribution to cytosolic FeS biogenesis (for a summary, see [34]), such per- or poly-sulfides are compelling candidates as endogenous substrates. More recently, however, intact Fe2S2 clusters ligated by four GSH molecules have also been suggested as Atm1 substrate [39]. This is supported by recent kinetic studies that reported the transport of (GSH)4Fe2S2 by Atm1 with a ~100-fold increased activity in the presence of the cluster [40]. The open questions, in addition to the nature of the transported compound, are the generation of this GSH derivative(s) from the Grx5/GSH-ligated Fe2S2 cluster in mitochondria (see below) as well as the link to the cytosolic iron sulfur cluster assembly machinery (CIA). In vitro, the GSH-ligated Fe2S2 cluster itself can be used to reconstitute apo-proteins [41].
The biogenesis of cytosolic and nuclear FeS-proteins requires numerous proteins and is facilitated by the CIA, summarized in [42]. Overall, the process can be divided into two steps. First, a Fe4S4 cluster is assembled on a scaffold complex. Second, this cluster is transferred and inserted into recipient apo-proteins. Apart from the yet to be determined component X-S that has to be supplied by the mitochondrial FeS synthesis machinery, the cytosolic FeS protein biogenesis requires an iron source and the supply of electrons. The latter are supplied by the NADPH-dependent diflavin oxidoreductase 1 (NDOR1) and the FeS protein anamorsin/CIAPIN1 (see Figure 1) [43,44,45,46]. The first step is the assembly of the Fe4S4 cluster on the cytosolic FeS scaffold complex (see Figure 1) [47,48,49]. The heterotetrameric complex consists of two P-loop NTPases, CFD1 (cytosolic FeS cluster-deficient protein 1) and NBP35 (nucleotide-binding protein 35). The complex binds two Fe4S4 clusters, one at the N-terminus of NBP35 and the second one is transiently ligated between CFD1 and NBP35 [50]. The nature and source of the iron for the formation of this first cytosolic FeS cluster is still unclear. Multi-domain Grxs like yeast or mammalian Grx3 may be potential candidates. They do play a general role in iron trafficking through the cytoplasm in a GSH-dependent manner [51,52] (details below). Potentially, they function in concert with a BolA family protein [10,53,54,55,56]. In the second step, the primarily assembled cluster is transferred and inserted into target proteins. This is facilitated by IOP1 (iron-only hydrogenase-like protein) and the CIA-targeting complex [57]. IOP1 may acts as a CIA adapter protein, mediating the contact between early and late parts of the CIA machinery, although the exact mechanism is still under discussion (see Figure 1) [47,58,59]. Probably, cytosolic iron-sulfur protein assembly protein 1 (CIA1), CIA2b, and MMS19 (MMS19 nucleotide excision repair protein homolog) build variable hetero-complexes, called the CIA-targeting complexes, that directly interact with specific cytosolic and nuclear apo-FeS proteins (see Figure 1) [58,60].
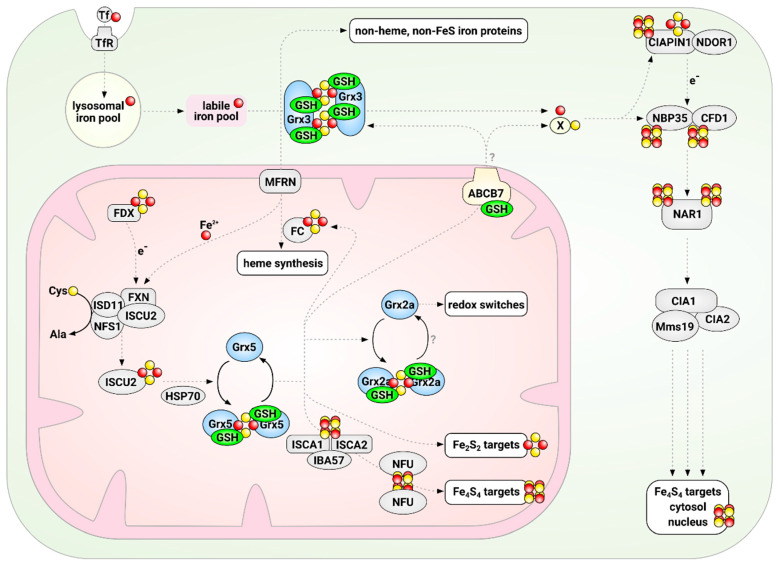
Figure 1.
Glutathione and glutaredoxins in iron-sulfur cluster synthesis and maturation in mammalian cells. The initial synthesis of Fe2S2 clusters is catalyzed by the mitochondrial iron-sulfur cluster synthesis machinery on the scaffold protein ISCU2. From there, clusters are distributed in a process that depends on the CGFS-type Grx5 to Fe2S2 and Fe4S4 target proteins, e.g., in the mitochondrial electron chain. In addition, a yet to be uncovered compound “X” is exported in a glutathione (GSH)-dependent manner to the cytosol, where it serves as substrate for the cytosolic iron-sulfur cluster assembly machinery. The multi-domain CGFS-type Grx3 is in some way required for the distribution of iron from the so-called labile iron pool to most, if not all, cellular iron-dependent processes. Glutaredoxins are depicted in light blue, GSH in green, iron in red, and sulfur in yellow.
2.2. Glutaredoxins
Grxs form a branch of the Trx family, for an overview see [61]. Bacterial Grxs represent the most basic representation of the Trx-fold, consisting of a four-stranded central β-sheet surrounded by three α-helices, and Grxs of higher organisms frequently display additional N- and C-terminal helices (Figure 2). In 1976, the first Grx was defined as a GSH-dependent electron donor for ribonucleotide reductase (RNR) and thus DNA synthesis [62]. In the following years, Grxs were comprehensively characterized as oxidoreductases that catalyze the formation and reduction of disulfides, i.e., inter- and intra-molecular protein disulfides, and with high specificity disulfides between protein thiols and GSH, i.e., reversible (de-)glutathionylation. For comprehensive reviews on this topic, see for instance [61,63,64,65,66,67], and for a summary of the characteristics of the human Grxs, see Table 1. In brief, these redox-active Grxs (CPYC-type or class I Grxs) contain a consensus Cys-Pro-Tyr-Cys active site motif and catalyze thiol-disulfide exchange reactions in two connected reaction mechanisms. The formation and reduction of protein disulfides require both active site cysteinyl residues and (de-)glutathionylation of only the more N-terminal. The mechanisms were thus termed dithiol and monothiol reaction mechanisms. Both reactions are initiated by a nucleophilic attack of the more N-terminal cysteinyl residue, which is characterized by a particularly low pKa value ≤ 5 [66,68,69,70], on the target disulfide. In the case of the dithiol reaction mechanism, the intermediate disulfide between the Grx and the target protein is reduced by the more C-terminal cysteinyl residue. The monothiol mechanism results in a reduced protein and a disulfide between the Grx and GSH (see Figure 2). Reduction of the Grx with a disulfide in the active site by GSH results in the same Grx-GSH mixed disulfide, which can be reduced by another molecule of GSH, completing both reaction cycles. Both reactions are fully reversible, as Grxs catalyze both the oxidation and reduction of target proteins. A second class of Grxs came into focus much later. These proteins share the consensus active site motif Cys-Gly-Phe-Ser, hence CGFS-type or class II Grxs. With few exceptions [71,72], CGFS-type Grxs are inactive as oxidoreductases. Instead, these proteins function in cellular iron metabolism [10,51,52,73,74], see below.
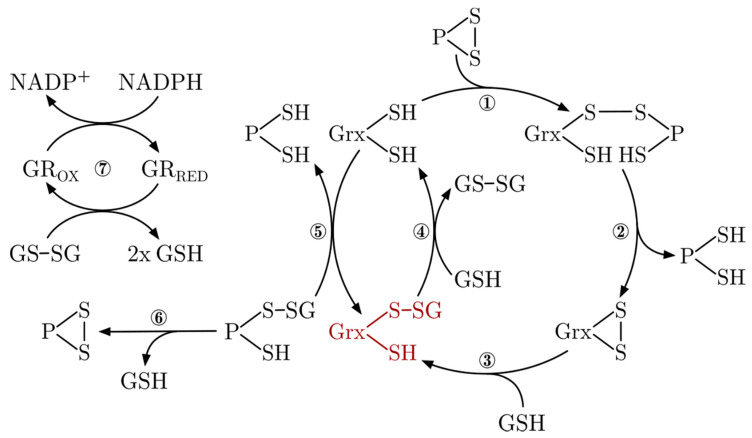
Figure 2.
Glutaredoxin reaction mechanisms. Protein disulfides are reduced via a mechanism that involves both active site cysteinyl residues of the CxxC-type Grxs. A reduced Grx forms a mixed disulfide with the thiol of a target protein and its N-terminal active site Cys (1). This intermediate is reduced by the C-terminal active site Cys, releasing the reduced substrate target protein (2). The oxidized Grx can be sequentially reduced by two molecules of GSH (3+4). A Grx-S-SG mixed disulfide (red) can easily be formed from reduced Grx and glutathione disulfide (GSSG) in the reverse reaction (4). Reduced Grx can also catalyze the reversible (de-)glutathionylation of a target protein in a mechanism that only requires the N-terminal active site Cys (5). Some glutathionylated proteins containing two adjacent Cys can also oxidize and form an intra-molecular disulfide by releasing GSH (6). GSSG is reduced to two molecules of GSH by glutathione reductase (GR) at the expense of NADPH.
Table 1.
Human glutaredoxins. Abbreviations: c: cytosol, m: mitochondria, n.a.: not available, n: nucleus.
| Protein Name | Accession | Gene | Active Site | Functions and Reactions | FeS | Locali-Zation |
|---|---|---|---|---|---|---|
| Grx1 | P35754 | Glrx | CPYC | Oxidoreductase, (de-)glutathionylation [75,76] | no | c/n |
| Grx2a | Q9NS18 | Glrx2 | CSYC | Oxidoreductase, FeS as redox sensor [16,77,78] | Fe2S2 | m |
| Grx2b | Q9NS18-2 | Glrx2 | CSYC | Not analyzed [77,79] | Fe2S2 | c/n |
| Grx2c | n.a. | Glrx2 | CSYC | Oxidoreductase, FeS as redox sensor [16,77,78] | Fe2S2 | c/n |
| Grx3 | O76003 | Glrx3 | 2·CGFS | Fe/S biogenesis, iron trafficking [52,80] | 2·Fe2S2 | c |
| Grx5 | Q86SX6 | Glrx5 | CGFS | Fe/S biogenesis [81,82] | Fe2S2 | m |
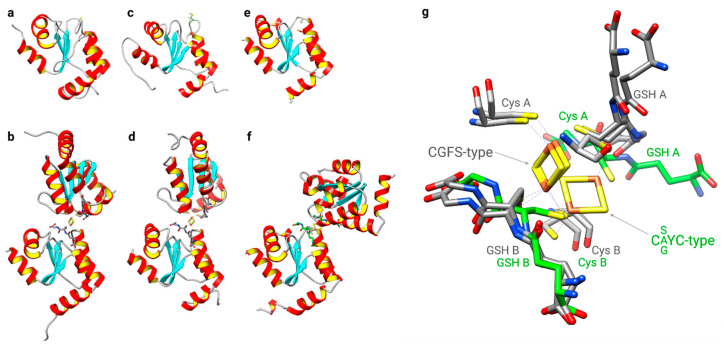
For decades, Grxs were characterized as co-factorless oxidoreductases [67]. It therefore came as a big surprise when the first two FeS-Grxs were described, Arabidopsis thaliana GrxC1 [83,84] and human Grx2 [16,85]. In both cases, it turned out that the exchange of the prolyl residue in the CPYC consensus active site for a glycyl and seryl residue, respectively, was sufficient to allow cluster ligation [84,85]. The second big surprise was the mode of cluster ligation itself in these proteins. The clusters are ligated in a dimeric holo-complex at the interface of two hardly interacting Grx monomers [84,86]. The [Fe2S2]2+ clusters are ligated by the two more N-terminal cysteinyl residues of the active site and the thiol groups of two non-covalent bound GSH molecules [84,85,86]. These were the first examples of FeS clusters co-ligated by GSH. Following these two C(non-P)YC-type Grxs, all CGFS-type Grxs have been characterized as Fe2S2-proteins, see for instance [10,74,80,81,87]. Both Grx sub-families bind the FeS cluster in a very similar way at the interface of the dimeric holo-complex, including co-ligation by GSH. However, one particular feature separates the two groups: the relative orientation of the Grx monomers in the holo-complex towards each other (Figure 3). Compared to the CGFS-type Grxs, the position of one monomer in the C(non-P)YC-type Grxs is tilted by approximately 90° toward the site relative to the other monomer. The sequestration of the N-terminal active site cysteinyl residue in the holo-complex of the redox-active, yet FeS-binding, Grxs suggests that the cluster serves as a regulatory mechanism controlling the activity of the proteins, for instance, by increased levels of GSSG or nitrogen oxide (NO) [16,88], or that it may serve other redox-independent functions [16,89].
Figure 3.
Structural comparison of both classes of FeS glutaredoxins. Structures of (a) apo- [PDB:1YKA] and (b) dimeric CGFS-type holo-Grx4 [PDB:2WCL] from Escherichia coli, CGFS-type human (c) apo- [PDB:2MMZ] and (d) holo-Grx5 [PDB:2WUL], and CSYC-type human Grx2 in (e) apo- [PDB:2FLS] and (f) holo-form [PDB:2HT9]. (g) Details of the alternative cluster coordination conformations of the holo-complexes, CGFS-type Grxs with GSH and active site cysteinyl residue carbon traces in gray, CSYC-type with carbon traces in green. “A” and “B” refer to the two subunits in the dimeric holo-complexes composed of the two subunits A and B, two non-covalently bound GSHs and the bridging Fe2S2 cluster.
Although both types of Grxs discussed here share highly similar 3-D structures (see Figure 3), as well as all elements and residues required to bind GSH [9], they exhibit completely different activities—oxidoreductase versus transferase. The mechanistic basis for this profound difference was the subject of many investigations and speculations [81,87,90,91], until two studies recently characterized the molecular basis of their distinct activity profiles [92,93]. In brief, the key determinants of their function are unique loop structures just before the active site. The engineering of a CxxC-type Grx with a CGFS-type loop switched its function from oxidoreductase to FeS transferase in a zebrafish model and the introduction of a CxxC-type loop into a CGFS-type Grx abolished its FeS transferase activity and activated the oxidative half-reaction (Figure 2, reaction 5 reverse) of the oxidoreductase [92]. The reductive half-reaction, requiring the interaction with the second GSH molecule (Figure 2, reaction 4), is dependent on further elements, characterized in detail in [93]. Together, these studies explain how subtle structural differences determine the diverse Grx functions. An overview of the different classes of Grxs in different species is depicted in Figure 4.
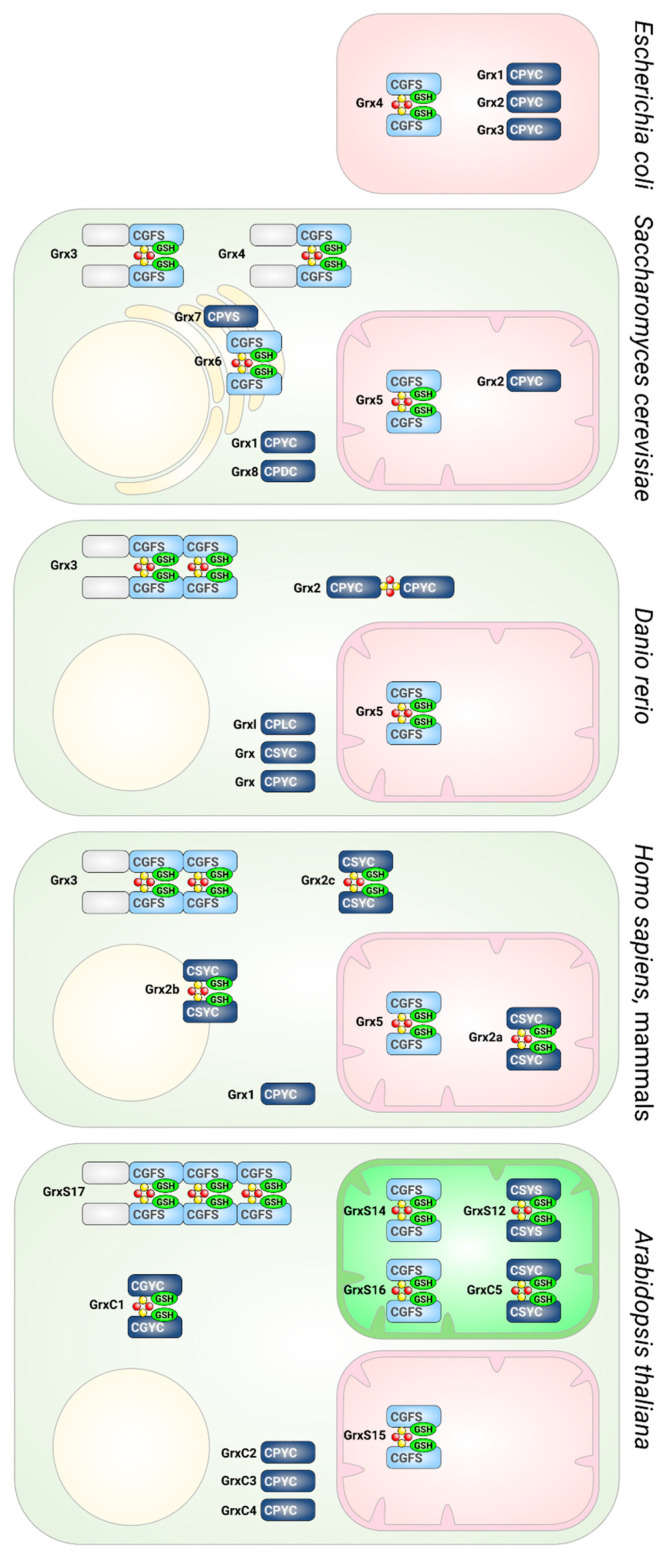
Figure 4.
Glutaredoxins in different species. Presence and subcellular localization of Grxs in Escherichia coli, Saccharomyces cerevisiae, Danio rerio, humans, and Arabidopsis thaliana. CGFS-type Grxs are depicted in light blue, CxxC-type in dark blue. The domain structures, active site sequences, and the ability to form FeS cluster-bridged holo-complexes are indicated.
2.2.1. Vertebrate- and Mammalian-Specific Glutaredoxin 2
Before it was described as an FeS protein, human Grx2 was characterized as a redox-active Grx with the ability to reduce mixed disulfides and effectively (de-)glutathionylate target proteins [79,94,95]. The human GLRX2 gene consists of five exons, including two alternative first exons (Ia and Ib) leading to three transcript variants. The core domain of Grx2, including the active site, is encoded by exon II-IV. GLRX2_v1 (exon Ia-II-III-IV) encodes the ubiquitously expressed Grx2a, including a mitochondrial targeting sequence. GLRX2_v2 and v3 are products of the alternative splice donor sites of exon Ib, encoding the nuclear and cytosolic isoforms Grx2b and Grx2c. The expression of Grx2b and Grx2c is restricted to the testis in adult human tissues, but has also been demonstrated in various cancer cell lines [77]. In contrast, the mouse GLRX2 gene consists of six exons, three constitutive exons (II, III, IV), two alternative first exons (Ia, Ib), and one single cassette exon. Five transcript variants encode three protein isoforms. The mitochondrial Grx2a and the nuclear/cytosolic Grx2c are conserved from mouse to human. Testis-specific Grx2d is unique to mouse [96]. Grx2 shares 34% sequence homology with Grx1 and a CSYC active site motif, with the exchange of the prolyl for a seryl residue [79,94]. This altered active site sequence results in an increased affinity for glutathionylated proteins and it can be reduced by either GSH or thioredoxin reductase, combining characteristics of Trxs and Grxs. Dimeric inactive holo-Grx2 bridges an FeS cluster. Degradation of the cluster in oxidative conditions, e.g., a more oxidized glutathione pool, results in monomeric active Grx2, indicating a function as a redox sensor in vivo [16]. Monomerization and cluster disassembly can cause lipid peroxidation, a drop in mitochondrial membrane potential, and eventually cell death [97]. The mitochondrial Grx2a was shown to participate in the maintenance of the redox equilibrium under conditions that promote oxidative damage to mitochondrial proteins. Especially for cells over-expressing Grx2a, protective functions have been described [88,98,99]. Grx2a over-expression decreased susceptibility towards apoptosis induced by doxorubicin (DOX) [100]. Grx2 is essential for mitochondrial morphology and dynamics in cardiomyocytes in humans and mice [101]. The loss of mitochondrial Grx2 is connected to increased mitochondrial proton leaks and respiration in muscle cells [102]. Genomes of other vertebrate species, e.g., zebrafish, contain genes encoding homologs to the cytosolic Grx2 isoform. This cytosolic zfGrx2 is essential for brain development. Zebrafish with silenced expression of cytosolic Grx2 lose essentially all types of neurons by apoptotic cell death and fail to develop an axonal scaffold. Only the re-introduction of wildtype Grx2c could rescue the defects, but not in either of the redox-inactive active site mutants [103]. The over-expression of Grx2c in SH-SY5Y neuroblastoma cells during retinoic acid-induced differentiation increases axon length and the number of branching points by up to two-fold [103]. Cytosolic Grx2 also has an essential function for the vascular development and maintenance of cardiovascular function [104,105]. Zebrafish lacking cytosolic Grx2 have an impaired heart looping and defects in heart functionality due to a failed migration of cardiac neural crest cells [106]. This heart looping defect could be rescued by introduction of the active site mutant of zfGrx2 that is still able to catalyze monothiol mechanism reactions [106]. Grx2c also has an essential function in spermatogenesis, a process that includes the migration of spermatogenic cells through the close Sertoli cell formation [77]. Recent results indicate a correlation between Grx2c expression and cancer-specific survival in clear cell renal cell carcinoma patients [107]. In a proteomic approach, Schütte et al. were able to identify target proteins, e.g., collapsin response mediator protein (CRMP) 2, that undergoes thiol-disulfide exchange reactions catalyzed by Grx2 [108]. In models of Parkinson’s disease, the depletion of glutathione resulted in a dose-dependent Grx2 inhibition and, similar to gene silencing of Grx2, decreased iron incorporation into complex I and ACO2. The loss of Grx2 function also led to the activation of iron regulatory protein (IRP1), resulting in the increase in the iron uptake protein transferrin receptor, decreased levels of the iron storage protein ferritin, and mitochondrial iron accumulation. In the cytosol, the loss of Grx2 resembled iron starvation conditions.
2.2.2. Glutaredoxin 5
Human Grx5 is one of the central proteins in the mitochondrial ISC machinery, as well as in cluster trafficking and, therefore, iron homeostasis [109,110]. In humans, the maturation of mitochondrial FeS cluster-containing proteins can be divided into different steps. First, the initial Fe2S2 cluster is assembled on the iron-sulfur cluster enzyme ISCU (ISCU2) and involves at least 17 characterized proteins [111]. The human ISCU2-M140I variant can overcome the loss of frataxin. However, this is not by restoring its function in cluster assembly, but rather by the acceleration of cluster transfer from ISCU2 to Grx5 [112]. The release and transfer of the Fe2S2 cluster is facilitated by Hsp70 chaperones [22]. Chaperone binding enhanced the ATP-dependent cluster transfer from E. coli IscU in vitro [113]. In S. cerevisiae, the ATPase activity of the chaperone increased by Isu1 binding but not by interaction with Grx5. The association of Isu1, Grx5, and the chaperone is required for cluster transfer from Isu1 to Grx5 [114]. A study published in 2018, however, contradicted these findings by showing a cluster transfer from ISCU to Grx5 only in the absence of the human mitochondrial Hsp70 chaperones HSPA9 and HSC20 [115]. However, this study completely relied on in vitro data with assay times up to two hours, and therefore the results were mainly subjected to thermodynamic restrictions rather than physiological constraints.
Together with Grx5, ISCA1 and ISCA2 are proteins involved in the assembly of Fe4S4 clusters [22]. Until recently, only very slow rates of cluster transfer from Grx5 to ISCA1 and ISCA2 were demonstrated in vitro. Although new insights were provided by the structure of the ISCA2-IBA57 complex [10,11], the reductive fusion of the two Fe2S2 clusters to one Fe4S4 cluster has only recently been reported [25]. BolA-like proteins, more precisely BolA1 and BolA3, were also suggested to interact with Grx5 in the assembly of Fe4S4 and possibly Fe2S2 clusters, as summarized, e.g., in [22]. Both human BolA1 and BolA3, interact with apo- and holo-Grx5 to form hetero-clusters with different affinities as shown in in vivo and in vitro studies [116,117]. NMR, EPR, CD, and UV/vis spectroscopy were utilized to characterize and identify differences in the nature of the clusters bound in the BolA1-Grx5 and BolA3-Grx5 hetero-complexes [118].
The loss of Grx5 disrupts FeS assembly on target proteins and leads to mitochondrial iron overload [19,114]. In Schizosaccharomyces pombe, Grx5 depletion also led to a decrease in mitochondrial DNA [119]. Additionally, in S. cerevisiae, an iron-dependent increased rRNA degradation was observed upon Grx5 depletion due to iron overload [120]. In zebrafish, a lack of Grx5 led to the activation of IRP1 and blocked heme biosynthesis [121]. The first step in this pathway is catalyzed by aminolaevulinate synthase 2 (ALAS2). The over-expression of ALAS2 RNA without the iron response element regulated by IRP1 rescued the zebrafish embryos, while the expression of ALAS2, including the iron response element, did not [121]. Human patients with decreased levels of Grx5 develop iron overload and sideroblastic-like microcytic anemia [82,109].
The mechanisms of cluster transfer in the mitochondrial FeS cluster machinery, as well as to target proteins, remain to be revealed. Over the years, many studies have been published proposing cluster transfer between proteins that are clearly involved in the mitochondrial FeS cluster synthesis pathway, but they have relied solely on in vitro data (e.g., [115]). As mentioned above, these sorts of in vitro studies are restricted by thermodynamics and do not take physiological conditions nor enzymatic catalysis into account. An example of how this leads in an unavailing direction can be found for CSYC-type Grx2. Also located in the mitochondria, Grx2 complexes an FeS cluster [16]. In contrast to Grx5 depletion, the loss of Grx2 does not impair ISC biogenesis or transfer but leads to defects, e.g., in brain and heart development [103,106]. In vivo Grx2 and Grx5 display completely different functions in redox regulation and iron homeostasis, respectively. However, it was published that in vitro human Grx2 transferred its FeS cluster to human ferredoxin (Fdx1) (see Table 2 and Figure 5) with an apparent second-order rate constant of 1160 ± 200 M−1 min−1 [122]. An essential reaction that takes more than 60 min is far away from being physiological and would be inconsonant with the human lifespan.
Table 2.
FeS cluster transfer reactions analyzed in vitro. Abbreviations: A.v.: Azotobacter vinelandii, H.s.: Homo sapiens, P.: Populus tremodus, S.c.: Saccharomyces cerevisiae, S.p.: Schizosaccharomyces pombe, Syn.: Synechocystis sp.
| Donor | Acceptor | Additional Factors | Transfer Rate (M−1 min−1) | Method | Assay Time (min) | Ref. |
|---|---|---|---|---|---|---|
| [Fe2S2](GS)4 | S.c. Grx3 | 1360 ± 110 1600 ± 450 2153 ± 281 |
CD | 30 | [41] | |
| [Fe2S2](GS)4 | H.s. BolA1 H.s. Grx5 | DTT | 60,000 ± 1200 | CD | 30 | [123] |
| [Fe2S2](GS)4 | H.s. BolA3 H.s. Grx5 | DTT | 28,000 ± 2800 | CD | 30 | [124] |
| [Fe2S2](GS)4 | H.s. BolA3 S.c. Grx3 | DTT | 29,000 ± 3000 | CD | 30 | [124] |
| H.s. Grx2 | H.s. Fdx1 | GSH | 1160 ± 200 | CD | 60 | [122] |
| H.s. Grx3 | H.s. Ciapin1 | UV-Vis | [125] | |||
| H.s. Grx3 | H.s. Ciapin1 | BolA2 | CD, UV-Vis | [56] | ||
| H.s. Grx5 | H.s. IscU | DTT, GSH, H.s. HSPA9, HSC20, ATP, MgCl2, | 7500 ± 2300 | CD | 60 | [115] |
| H.s. Grx5 | H.s. IscU D37A | DTT, GSH | 3500 ± 500 | CD | 58 | [115] |
| H.s. Grx5 | H.s. Nfu1 | DTT, GSH | 950 ± 450 | CD | 118 | [115] |
| H.s. Grx5 | H.s. Nfu1 | DTT, GSH, BolA3 | CD, UV-Vis, NMR | [126] | ||
| H.s. Grx5 | H.s. Fdx1 | DTT, GSH | 2000 ± 700 | CD | 120 | [115] |
| H.s. Grx5 | H.s. Fdx2 | DTT, GSH | 650 ± 250 | CD | 120 | [115] |
| H.s. Grx5 | H.s. ISCA1/ISCA2 | DTT, GSH | NMR | 9–48 h | [127] | |
| H.s. Grx5 | H.s. ISCA2 | DTT, GSH | NMR | 9–48 h | [127] | |
| H.s. Grx5 | H.s. ISCA2 C79S | DTT, GSH | NMR | 9–48 h | [127] | |
| H.s. ISCA1 | H.s. BolA1, H.s. Grx5 | DTT, GSH | CD | 60 | [123] | |
| H.s. ISCA2 | H.s. BolA1, H.s. Grx5 | DTT, GSH | CD | 60 | [123] | |
| H.s. ISCU | H.s. BolA1, H.s. Grx5 | DTT, GSH | 3600 ± 400 | CD | 60 | [123] |
| H.s. ISCU | H.s. BolA3, S.c. Grx3 | DTT, GSH | 4600 ± 870 | CD | 60 | [124] |
| H.s. ISCU | H.s. BolA3, H.s. Grx5 | DTT, GSH | 14,000 ± 1000 | CD | 60 | [124] |
| H.s. ISCU | H.s. Grx5 | DTT, GSH | 10,300 ± 1800 | CD | 10 | [115] |
| H.s. ISCU | S.c. Grx3 | GSH | 3370 ± 200 | CD | 60 | [128] |
| H.s. Nfu | H.s. Grx5 | DTT, GSH | 35,100 ± 2000 | CD | 60 | [129] |
| H.s. Nfu | H.s. Grx2 | GSH | 2000 ± 150 | CD | 60 | [122] |
| H.s. Nfu | S.c. Grx3 | GSH | 36,200 ± 7700 | CD | 60 | [128] |
| H.s. Nfu | S.c. Grx3 | DTT, GSH, H.s. HSPA9, HSC20, ATP, MgCl2 | 34,400 ± 4500 | CD | 60 | [129] |
| H.s. Nfu1 | H.s. BolA3, S.c. Grx3 | DTT, GSH | CD | 60 | [124] | |
| H.s. Nfu1 | H.s. BolA3, H.s. Grx5 | DTT, GSH | CD | 60 | [124] | |
| H.s. BolA1 H.s. Grx5 | H.s. Fdx1 | DTT, GSH | CD | 60 | [123] | |
| H.s. BolA1 H.s. Grx5 | H.s. Fdx2 | DTT, GSH | CD | 60 | [123] | |
| H.s. BolA1 H.s. Grx5 | H.s. ISCA1 | DTT, GSH | CD | 60 | [123] | |
| H.s. BolA1 H.s. Grx5 | H.s. ISCA2 | DTT, GSH | CD | 60 | [123] | |
| H.s. BolA3 S.c. Grx3 | H.s. Fdx1 | DTT, GSH | 1800 ± 170 | CD | 60 | [124] |
| H.s. BolA3 S.c. Grx3 | H.s. Fdx2 | DTT, GSH | 2600 ± 540 | CD | 60 | [124] |
| H.s. BolA3 S.c. Grx3 | H.s. Nfu1 | DTT, GSH | CD | 60 | [124] | |
| H.s. BolA3 H.s. Grx5 | H.s. Fdx1 | DTT, GSH | 1400 ± 140 | CD | 60 | [124] |
| H.s. BolA3 H.s. Grx5 | H.s. Fdx2 | DTT, GSH | 2800 ± 380 | CD | 60 | [124] |
| H.s. BolA3 H.s. Grx5 | H.s. Nfu1 | DTT, GSH | CD | 60 | [124] | |
| S.c. Grx3 | H.s. Fdx1 | GSH | 2100 ± 500 | CD | 60 | [122] |
| S.c. Grx3 | H.s. Fdx2 | GSH | 695 ± 138 | CD | 240 | [122] |
| S.c. Grx3 | A.v. IscA | ≥50,000 | CD | 10 | [130] | |
| S.p. Isa1 | S.c. Grx3 | GSH | 6200 ± 1900 | CD | 60 | [122] |
| A.v. Grx5 | A.v. Fdx | DTT | 2100 | CD | 160 | [131] |
| A.v. Grx5 | A.v. IscA | 22,000 | CD | 10 | [130] | |
| A.v. IscA | S.c. Fra2-Grx3 | 15,000 | CD | 120 | [130] | |
| A.v. IscU | A.v. Grx5 | GSH | 30 | CD | 180 | [131] |
| A.v. IscU | A.v. Grx5 | A.v. HscA, A.v. HcsB, MgCl2, ATP, KCl | 20,000 | CD | 60 | [131] |
| A.t. GrxS14 | A.v. IscA | ≥50,000 | CD | 10 | [130] | |
| A.t. GrxS14 | A.t. SufA1 | ≥50,000 | CD | 10 | [130] | |
| A.t. GrxS15 | A.t. (mito)Fdx1 | Native PAGE | [132] | |||
| P. GrxS14 | Syn. Fdx | 20,000 | CD | ~60 | [74] |
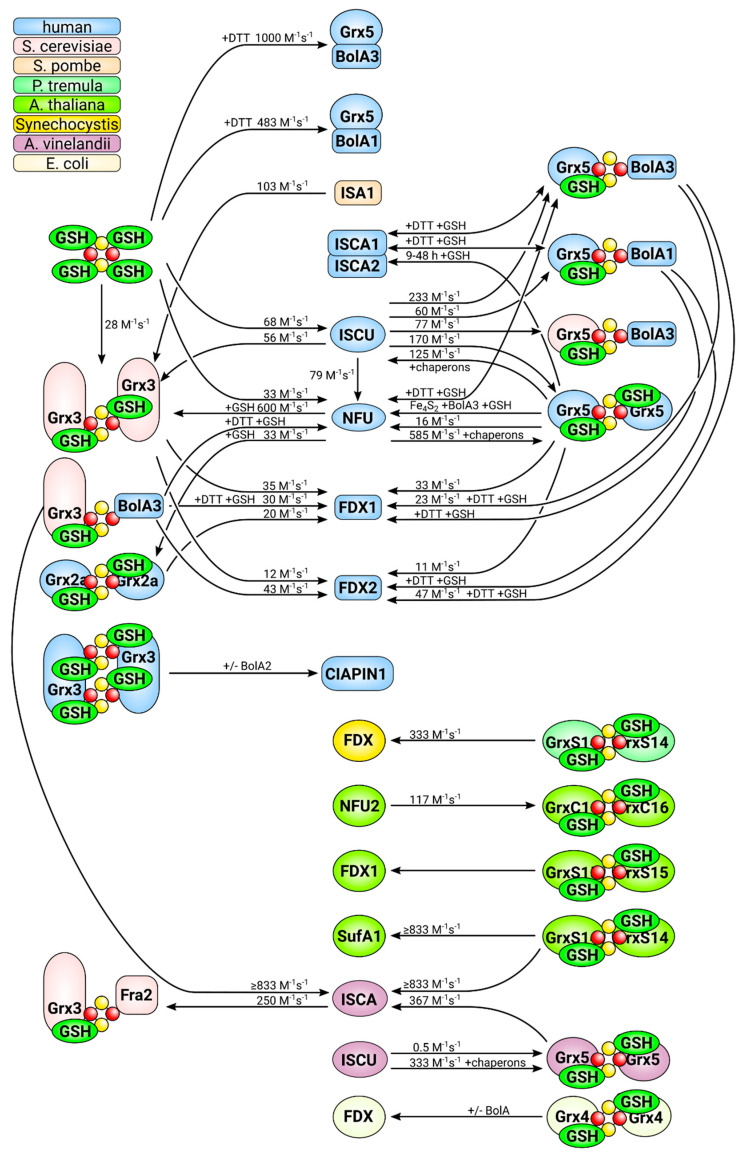
Figure 5.
FeS cluster transfer reactions analyzed in vitro to date. This figure summarizes all in vitro cluster transfer reactions analyzed and described in the literature. The directions of the reactions are indicated by arrows. The origin of the different proteins used in the analyses, i.e., the species that encodes the respective protein, is color coded, as displayed in the top left corner. For details and references, see Table 2.
2.2.3. Multi-Domain Glutaredoxins, Glutaredoxin 3
Multi-domain Grxs are unique to eukaryotic cells. They consist of an N-terminal, normally redox inactive, and a Trx domain followed by one to three CGFS-type Grx domains, each of which can complex the GSH co-ligated Fe2S2 cluster in dimeric complexes. The yeast Saccharomyces cerevisiae expresses two closely related multi-domain Grxs containing a single CGFS-type Grx domain each, Grx3 and Grx4. Two major functions, both central for iron metabolism, were characterized for these proteins: (1) Grx3 and Grx4 have a central role in intra-cellular iron trafficking and sensing. The depletion of Grx3/4 specifically impaired all iron-requiring reactions in the cytosol, mitochondria, and nucleus, including the synthesis of FeS clusters, heme, and di-iron centers, such as in RNR (see Figure 1). The cells failed to insert iron into target proteins, as well as to deliver iron to mitochondria. Iron was simply not bio-available in the absence of the proteins [51] and (2) the availability of iron to form the FeS-bridged holo-complexes of Grx3 and 4 is used as sensor for the iron state of fungal cells. Extensive analyses of S. cerevisiae and S. pombe have uncovered unique mechanisms that control iron metabolism in different fungi, summarized recently in [11]. The common thread in these regulatory mechanisms are the multi-domain CGFS-type Grxs that interact, often together with BolA-type proteins (see below), with transcription factors dependent on the iron state of the cell, thus controlling the transcription of proteins and enzymes that take part in, or control, iron metabolism. For detailed discussion on this topic, see for instance [10,11,133,134].
Vertebrate-specific Grx3, also known as protein kinase C-interacting cousin of thioredoxin (PICOT), TXNL-2, and HUSSY-22, contains two C-terminal CGFS-type Grx domains [66,135,136]. Grx3 is ubiquitously expressed [80,137], the protein can complex two Fe2S2 clusters at the interfaces between the two CGFS-type Grx domains in a homo-dimeric holo-complex, and it binds iron in vivo [80]. The depletion of Grx3 in zebrafish embryos primarily affected hemoglobin maturation. The loss of Grx3 function did not affect globin biosynthesis, and instead heme did not mature [52]. This was likely caused by the loss of an essential FeS cluster in the enzyme ferrochelatase that catalyzes the final step in heme maturation, iron insertion [138]. Gene silencing of Grx3 in cells of human origin (HeLa cells) induced a phenotype resembling an iron starvation phenotype despite the sufficient bio-available iron. The protein levels of several cytosolic FeS proteins were altered, for instance, IRP1 and glutamine phosphoribosylpyrophosphate amidotransferase (GPAT). The protein levels of ferritin were decreased and the levels of the transferrin receptor increased, indicating the activation of IRP1. Apparently, the Grx3-depleted cells were unable to use iron efficiently, indicating a central role for Grx3 in iron metabolism [52] similar to the one described in yeast [51], i.e., a function in cellular iron trafficking. The molecular base of this function and how it relates to the observed defects in FeS protein maturation in the cytosol of eukaryotic cells is still unknown.
Human Grx3 was initially identified as an interaction partner of protein kinase C θ and is associated with various signaling pathways that lead to the activation of cells [136]. Grx3 is essential during development, the loss of Grx3 in mice resulted in embryonic death between E12.5 and E14.5, without apparent defects in organogenesis [139]. Grx3−/− embryos did not exhibit obvious histological abnormalities, however, the embryos were reported to be of smaller body size and developed hemorrhages in the head [139,140]. It is noteworthy that the time point of embryonic death, E12.5, also marks the onset of definitive erythropoiesis in the fetal liver [141,142] and, from this point on, erythropoesis is the major iron-consuming process. Grx3 can protect from cardiac hypertrophy in animal models. Grx3 protein levels were increased in these models and heterozygous Grx3+/− mice were more vulnerable to developing cardiac hypertrophy, in contrast to wildtype mice [139,140]. Disturbances in iron metabolism have also been linked to cardiac pathologies. For instance, in Friedreich’s ataxia patients, the (partial) loss of the FeS cluster biogenesis protein frataxin (Figure 1) causes mitochondrial iron overload and defects in mitochondrial FeS maturation, summarized in [23,143]. These defects frequently cause cardiomyopathy and cardiac hypertrophy [144]. To date, however, it is unclear whether the role of Grx3 in cardiac hypertrophy is connected to its role in iron metabolism.
2.3. Grxs and BolA-Like Proteins
Both genetic and biochemical evidence link BolA-like proteins to iron metabolism and to CGFS-type Grxs in particular [10,145]. It was hypothesized that both proteins interact in the transfer of FeS clusters to targeting complexes or recipient proteins. This is supported by a number of in vitro and structural studies [118]. Unlike the CGFS-type Grxs, BolA-like proteins from different species show a high degree of heterogeneity and a low degree of conservation, including some of the residues that were suggested to take part in the ligation of FeS clusters in both homo- and hetero-dimeric holo-complexes.
In S. cerevisiae, the regulation of iron metabolism by the transcription factors activator of iron transcription protein (Aft) 1 and Aft2 depends on the Grx3/Grx4 siblings and the proteins Fe repressor of activation (Fra) 1 and Fra2, for summaries, see [10,11]. Fra2 is BolA-like protein also known as BolA2. The Fe2S2 cluster in the hetero-dimeric complex between Grx3/4 and Fra2 is complexed by the Grx3/4 active site CGFS cysteinyl residue, a Fra2 histidyl residue, one GSH, and another ligand that is not a histidyl residue and remains elusive [146,147]. The conserved His103 residue is not required for hetero-dimer formation and cluster binding in vitro, but influences cluster stability [146]. In vitro studies described a cluster transfer between Grx3-Bol2 and Aft2, involving a ligand exchange mechanism and a specific protein–protein interaction that requires Aft2 Cys187 [148,149]. Cluster binding appeared to be more stable in the hetero-dimeric complex compared to Grx3/4 homo-dimers, although removal of this cluster did not disrupt the Grx3-Fra2 hetero-dimer, raising the question of whether it functions as an FeS scaffold or iron sensing protein [147]. In the proposed iron sensing mechanism in S. pombe, an FeS cluster is transferred from the transcription factor iron-sensing transcription factor 1 (Fep1) to Grx4-Fra2 in response to iron starvation, thereby activating gene expression to increase the intra-cellular iron pool [150].
The holo-complex of the human multi-domain CGFS-type Grx3 bridges two Fe2S2 clusters with four GSHs and its two conserved CGFS motifs [80]. In 2012, Li et al. demonstrated that human Grx3 forms a heterotrimeric complex with human BolA2 in vitro, and this was confirmed by Banci et al. [53,56]. As in yeast, cysteinyl and histidyl residues of Grx3 and BolA2, respectively, were proposed to be involved in cluster coordination [53,56]. In contrast to yeast, however, in vivo data supporting this interaction and a physiological role of this hetero-trimeric complex remain to be presented. In vitro data suggested more stable Fe2S2 clusters in the hetero-trimeric compared to the Grx3 homo-dimeric complexes, as observed in yeast. Nevertheless, a role of the BolA2-Grx3 complex in Fe2S2 cluster transfer in the cytosolic FeS protein maturation pathway was proposed [56]. Cluster transfer from homo-dimeric Grx3 to CIAPIN1 (also named anamorsin, see Figure 1 and Figure 5) was demonstrated, the specific interactions between the two were proposed as key mechanisms in anamorsin maturation [125]. However, the hetero-complex with BolA2 was also reported to be able to transfer both bridging Fe2S2 clusters to CIAPIN1/anamorsin in vitro, and thus a function as an FeS cluster transfer component in the cytosolic FeS protein biogenesis was suggested [56]. The siRNA-mediated silencing of Grx3 induces an iron starvation phenotype in HeLa cells [52]. However, the silencing of BolA2 expression not only failed to induce a similar phenotype, but the co-silencing of Grx3 and BolA2 rescued the iron starvation phenotype to some degree (unpublished own data). These results imply an antagonistic rather than joint function of cytosolic Grx3 and BolA2. This fragmentary puzzle of information and results remains to be solved.
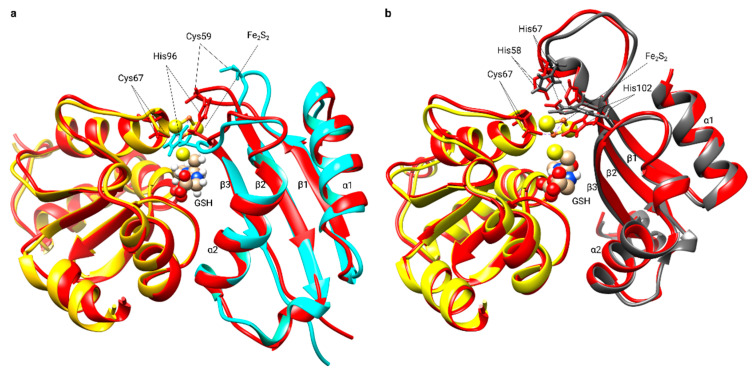
Mitochondria of eukaryotic cells usually harbor the CGFS-type Grx5 and two BolA-like proteins, BolA1 and BolA3, both of which can form hetero FeS-bridged complexes with Grx5. Uzarska et al. demonstrated that human apo-Grx5 and BolA1 or BolA3 also specifically interact in chemical shift assays [114]. This interaction involves the location surrounding the invariant histidyl residue in the BolAs and the GSH-binding site in Grx5 [117]. Complex holo-models suggest that Grx5-BolA3 undergo significant structural rearrangement upon dimer formation and FeS cluster binding (Figure 6) [118]. In the loop connecting β-strand 1 and 2 of BolA3, the Cys 59 residue moves towards the invariant C-terminal His 96 and coordinates the Fe2S2 together with the active site and GSH thiols of Grx5. The complex with BolA1, on the other hand, seems to not involve structural re-arrangements and has a different orientation [118] (Figure 6).
Figure 6.
Structural rearrangements in Grx5 and BolA upon dimer formation. (a) Superimposition of the backbone structure of human apo-Grx5 [PDB:2WUL] (yellow) and human BolA3 [PDB: 2NCL] (cyan) with the Fe2S2 BolA3-Grx5 complex backbone structure (red). (b) Superimposition of the backbone structure of human apo-Grx5 [PDB:2WUL] (yellow) and human BolA1 [PDB:5LCI] (dark gray) with the Fe2S2 BolA1-Grx5 complex backbone structure (red). The GSH molecule and the Fe2S2 cluster are represented as balls and sticks. The invariant C-terminal His (His 96 in BolA3 and His 102 in BolA1), His 67 in BolA1, Cys 59 in BolA3, and Cys 67 in human Grx5 residues are shown.
In vivo and in vitro studies suggest specialized functions of yeast mitochondrial Bol1 and Bol3 in the same pathway, i.e., FeS protein maturation in mitochondria. The over-expression of Grx5 increases the BolA1 level but there is no effect on BolA3 [116]. BolA1 interacts with Grx5 via the Fe2S2 cluster, whereas BolA3 interacts with Nfu1 in the Fe4S4 cluster assembly, although the detailed mechanisms remain unsolved [116,117]. Yeast cells lacking BolA1 and BolA3 show defects in Fe4S4 enzymes, e.g., aconitase and lipoic acid synthase [116,151]. The interaction of the two human mitochondrial BolA-like proteins, BolA1 and BolA3, and Grx5 was characterized by a number of in vitro techniques [117]. Conserved histidyl residues (His102 in BolA1 and His96 in BolA3) and other potential cluster ligands, e.g., histidyl and cysteinyl residues in BolA1 and BolA3, respectively, are involved in hetero-dimeric cluster formation [10,117]. A reduced Rieske-type Fe2S2 cluster is coordinated by Grx5 and BolA1 with high affinity, whereas the oxidized, Fdx-like cluster of Grx5 and BolA3 is labile and BolA3 preferably interacts with Nfu1 [117,118]. Based solely on in vitro studies, Sen et al. concluded the contrary—a significant BolA3-Grx5 interaction and a weak BolA3-Nfu1 interaction [124]. Two BolA3-Grx5 hetero-complexes can transfer their Fe2S2 clusters to Nfu1 to form a Fe4S4 cluster in FeS protein maturation [126]. A role in cluster trafficking was ruled out for BolA1-Grx5 because of its structurally buried cluster and the lack of transfer efficiency to common Fe2S2 cluster acceptors, such as ferredoxins [123]. Patients with mutations in the Grx5 or the BolA3 gene suffer from variations of nonketotic hyperglycinemia with decreased lipoylation, likely caused by interruption of the cluster transfer pathway to the FeS protein lipoate synthase [110]. The physiological role of BolA1 and BolA3 in complex with Grx5 remains elusive. For more comprehensive summaries of the topic, we refer to [10,54,111].
2.4. FeS Cluster Transfer Reactions
CGFS-type Grxs and BolA-like proteins have been suggested to cooperate in the transfer of FeS clusters to target proteins and targeting protein complexes [53]. A number of studies, summarized in Table 2 and Figure 5, have addressed such transfer reactions in vitro, mostly utilizing differences in the absorption or circular dichroism of the holo-complexes of target and recipient proteins. In brief, the combined in vitro data on these cluster transfer reactions can be summarized as follows: it appears that Fe2S2 clusters can be transferred between most proteins that have the ability to ligate them, independent of the physiological significance of these interactions and phylogenetics. The reactions are reversible and seem to primarily follow thermodynamic constrains. So far, evidence for the requirement of any form of catalysis has only been demonstrated for the transfer of the Fe2S2 cluster built in the initial scaffold ISCU to the Grx5 homolog of Azotobacter vinelandii in the form of the HscA/HscB chaperone system [131]. The rate constants, especially of the reactions regarded as physiologically significant, are generally low, in the range of 0.1–1.7·101 M−1 s−1. Astonishingly, some of the highest rate constants have been reported for cluster transfer reactions between proteins that cannot be considered physiologically meaningful, e.g., from human Nfu (mitochondrial) to S. cerevisiae Grx3 (cytosolic) with 6·102 M−1 s−1 [122], or from S. cerevisiae Grx3 to Azotobacter vinelandii ISCA at ≥8.3·102 M−1 s−1 [130]. In vitro, human Grx2, a CSYC-type Grx, can transfer its cluster to Fdx1 with similar (low) rates as CGFS-type Grx5, i.e., 1.9·101 M−1 s−1 and 3.3·101 M−1 s−1, respectively, summarized in Table 2 and Figure 5. In vivo, however, due to its different quaternary structure, the ubiquitously expressed [77] mitochondrial Fe2S2-Grx2a cannot compensate for the iron deficiency phenotype caused by Fe2S2-Grx5 depletion or loss, in neither zebrafish [82] nor in humans [82,109]. With respect to the role of the BolA-like proteins, no in vitro study so far has demonstrated that these proteins are strictly required for the transfer of FeS clusters from Grxs to any other protein or vice versa, nor that their presence would enhance the rate constants of the transfer reaction. To date, in vitro studies have not provided conclusive evidence on the nature of the efficiency, nor the specificity in cluster transfer reactions observed in vivo.
3. Other Glutathione-Iron Complexes
Dinitrosyl-iron complexes (DINICs) are the derivative of nitric oxide (NO), iron, and other ligands. They play a crucial role in stabilization, storage, and NO bio-activity [152]. The electron paramagnetic resonance (EPR) signal at g = 2.03 is a characteristic feature of DINICs and was identified in vivo in animal tissues and other organisms [153]. In general, DINICs are formed by the attachment of anionic ligands to an Fe(NO)2 nucleus. One common ligand of these centers is the thiolate of glutathione (GS−). Depending on the number of iron-nitrosyl nuclei attached to the ligand(s), both mono- and bi-nuclear DINICs are formed [154]. Under physiological conditions, mononuclear thiol-ligated DINICs appear to be in equilibrium with binuclear DINICs of the Roussin’s red salt thioether type [155]. FeS proteins may be the major source of protein-bound DINICs as demonstrated in E. coli when ·NO directly reacts with the FeS clusters [156]. ·NO may also react with superoxide (O2−), yielding peroxynitrite (ONOO−) that can react with proteins, inducing carbonylation and nitration [61]. In a recent study, we provided evidence that FeS-Grx2 can inhibit ONOO− formation in cells by the reaction of its GSH co-ligated FeS cluster with ·NO, yielding glutathionyl-DINICs [88]. Such glutathionyl-DINICs may biologically be the most significant form. For instance, they may play an important role in protein S-nitrosylation (S-NO).
Various studies and reviews have reported the formation of S-NOs in vivo, see for instance [157,158,159,160]. It is often described as the product of the reaction of the ·NO radical with thiol groups. However, this reaction as such cannot take place unless one electron is removed, e.g., by a metal/enzyme catalyst [161].
| NO + R-SH → R-S-NO + e− | (1) |
Glutathionyl-DINICs can release nitrosonium ions (NO+) that can react with GSH to form GS-NO [162]. This NO+ moiety can be transferred to other thiols by a nucleophilic attack on the electrophilic nitrogen atom of GS-NO—a process known as protein trans-nitrosylation [163].
| GS-NO + R′-SH → GSH + R′-S-NO | (2) |
The thiol peroxidases peroxiredoxin 1 (Prx1) is S-nitrosylated in mammalian cells [164]. This reaction is mediated by glutathionyl-DINICs and involves the reactive peroxidatic cysteinyl residue in the active site of Prx1. The reaction affects the reactivity of the protein and thus its enzymatic and signaling functions [165].
DINICs complexed with glutathione may also be of interest for therapeutic applications [153]. They might serve also as ·NO donors to regulate the muscle tonus around the vasculature [152] and have already been successfully tested as hypotensive drugs in clinical trials [166]. The stability of DINICs can be increased through their interaction with proteins [153]. For example, cysteinyl residues in serum albumin can modulate and prolong the vasodilating activity of glutathionyl-DINICs [152]. It is noteworthy that these DINICs do not seem to affect the cellular glutathione levels, nor cellular proliferation [167]. They are not toxic to HeLa cells [168] and they increase the viability of fibroblasts and rat caridiomyocytes [167,169]. Glutathionyl-DINICs were also reported to accelerate skin wound healing, to inhibit apoptosis, and to suppress endometriosis [9,170]. In heart infarction models, treatment reduced the size of the infarction zone and inhibited platelet aggregation [171,172]. In summary, treatment with glutahionyl-DINICS may develop into new therapeutic strategies.
4. Conclusions and Outlook
The past decade has seen some remarkable progress in our understanding of the role of GSH and Grxs in iron metabolism, particularly with respect to the synthesis and maturation of FeS proteins. Promising steps have been made towards re-building functional FeS transfer and targeting complexes in vitro. We have reached a molecular understanding of the factors that determine the GSH-dependent oxidoreductase and FeS scaffold functions of Grxs. With the unraveling of the yeast Grx3/4-Fra2-mediated regulation of iron homeostasis in yeast, we have been presented with the first well-characterized physiological function of a Grx-BolA hetero-complex. However, a number of urgent open questions remain to be answered. They include, without claiming completeness:
What is the role of GSH in the export of FeS precursors from mitochondria to the cytosolic FeS assembly machinery? What compound is exported and what is the source of iron for cytosolic FeS maturation?
Outside the well-established yeast Aft regulon, what are the physiological roles of the CGFS-type Grx interactions with BolA-like proteins? Are these interactions essential for mitochondrial and/or cytosolic FeS maturation and transfer reactions? Do (more) of these complexes function in iron sensing?
What is the mechanism of cluster transfer between Grxs and recipient proteins? What are the factors that ensure both the specificity and efficiency of the reactions in vivo that we are apparently missing in vitro to date?
Author Contributions
T.D., H.M.F., J.L.M., G.M., and L.C.H. wrote and revised the text. All authors have read and agreed to the published version of the manuscript.
Funding
This work was supported by grants from the Deutsche Forschungsgemeinschaft (LI 984/3-2, LI 984/4-1, and GRK1947-A1. We acknowledge support for the Article Processing Charge from the DFG (German Research Foundation, 393148499) and the Open Access Publication Fund of the University of Greifswald.
Conflicts of Interest
The authors declare no conflict of interest.
References
- 1.Deponte M. The Incomplete Glutathione Puzzle: Just Guessing at Numbers and Figures? Antioxid. Redox Signal. 2017;27:1130–1161. doi: 10.1089/ars.2017.7123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Berndt C., Lillig C.H., Flohé L. Redox regulation by glutathione needs enzymes. Front. Pharmacol. 2014;5:168. doi: 10.3389/fphar.2014.00168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Handy D.E., Lubos E., Yang Y., Galbraith J.D., Kelly N., Zhang Y.Y., Leopold J.A., Loscalzo J. Glutathione peroxidase-1 regulates mitochondrial function to modulate redox-dependent cellular responses. J. Biol. Chem. 2009;284:11913–11921. doi: 10.1074/jbc.M900392200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sakai O., Uchida T., Imai H., Ueta T. Glutathione peroxidase 4 plays an important role in oxidative homeostasis and wound repair in corneal epithelial cells. FEBS Open Bio. 2016;6:1238–1247. doi: 10.1002/2211-5463.12141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Yang W.S., Stockwell B.R. Ferroptosis: Death by Lipid Peroxidation. Trends Cell Biol. 2016;26:165–176. doi: 10.1016/j.tcb.2015.10.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cao J.Y., Dixon S.J. Mechanisms of ferroptosis. Cell. Mol. Life Sci. 2016;73:2195–2209. doi: 10.1007/s00018-016-2194-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ingold I., Berndt C., Schmitt S., Doll S., Poschmann G., Buday K., Roveri A., Peng X., Freitas F.P., Seibt T., et al. Selenium Utilization by GPX4 Is Required to Prevent Hydroperoxide-Induced Ferroptosis. Cell. 2018;172:409–422. doi: 10.1016/j.cell.2017.11.048. [DOI] [PubMed] [Google Scholar]
- 8.Kumar C., Igbaria A., D’autreaux B., Planson A.G., Junot C., Godat E., Bachhawat A.K., Delaunay-Moisan A., Toledano M.B. Glutathione revisited: A vital function in iron metabolism and ancillary role in thiol-redox control. EMBO J. 2011;30:2044–2056. doi: 10.1038/emboj.2011.105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Berndt C., Lillig C.H. Glutathione, Glutaredoxins, and Iron. Antioxid. Redox Signal. 2017;27:1235–1251. doi: 10.1089/ars.2017.7132. [DOI] [PubMed] [Google Scholar]
- 10.Li H., Outten C.E. Monothiol CGFS glutaredoxins and BolA-like proteins: [2Fe-2S] binding partners in iron homeostasis. Biochemistry. 2012;51:4377–4389. doi: 10.1021/bi300393z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gupta M., Outten C.E. Iron-sulfur cluster signaling: The common thread in fungal iron regulation. Curr. Opin. Chem. Biol. 2020;55:189–201. doi: 10.1016/j.cbpa.2020.02.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rouhier N., Couturier J., Johnson M.K., Jacquot J.-P. Glutaredoxins: Roles in iron homeostasis. Trends Biochem. Sci. 2010;35:43–52. doi: 10.1016/j.tibs.2009.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sugiura Y., Tanaka H. Iron-sulfide chelates of some sulfur-containing peptides as model complex of non-heme iron proteins. Biochem. Biophys. Res. Commun. 1972;46:335–340. doi: 10.1016/S0006-291X(72)80143-8. [DOI] [PubMed] [Google Scholar]
- 14.Kispal G., Csere P., Guiard B., Lill R. The ABC transporter Atm1p is required for mitochondrial iron homeostasis. FEBS Lett. 1997;418:346–350. doi: 10.1016/S0014-5793(97)01414-2. [DOI] [PubMed] [Google Scholar]
- 15.Sipos K., Lange H., Fekete Z., Ullmann P., Lill R., Kispal G. Maturation of cytosolic iron-sulfur proteins requires glutathione. J. Biol. Chem. 2002;277:26944–26949. doi: 10.1074/jbc.M200677200. [DOI] [PubMed] [Google Scholar]
- 16.Lillig C.H., Berndt C., Vergnolle O., Lönn M.E., Hudemann C., Bill E., Holmgren A. Characterization of human glutaredoxin 2 as iron-sulfur protein: A possible role as redox sensor. Proc. Natl. Acad. Sci. USA. 2005;102:8168–8173. doi: 10.1073/pnas.0500735102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Beinert H., Holm R.H., Münck E. Iron-sulfur clusters: Nature’s modular, multipurpose structures. Science. 1997;277:653–659. doi: 10.1126/science.277.5326.653. [DOI] [PubMed] [Google Scholar]
- 18.Johnson D.C., Dean D.R., Smith A.D., Johnson M.K. Structure, function, and formation of biological iron-sulfur clusters. Annu. Rev. Biochem. 2005;74:247–281. doi: 10.1146/annurev.biochem.74.082803.133518. [DOI] [PubMed] [Google Scholar]
- 19.Lill R., Hoffmann B., Molik S., Pierik A.J., Rietzschel N., Stehling O., Uzarska M.A., Webert H., Wilbrecht C., Mühlenhoff U. The role of mitochondria in cellular iron–sulfur protein biogenesis and iron metabolism. Biochim. Biophys. Acta BBA-Mol. Cell Res. 2012;1823:1491–1508. doi: 10.1016/j.bbamcr.2012.05.009. [DOI] [PubMed] [Google Scholar]
- 20.Gerber J., Neumann K., Prohl C., Mühlenhoff U., Lill R. The Yeast Scaffold Proteins Isu1p and Isu2p Are Required inside Mitochondria for Maturation of Cytosolic Fe/S Proteins. Mol. Cell. Biol. 2004;24:4848–4857. doi: 10.1128/MCB.24.11.4848-4857.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Balk J., Schaedler T.A. Iron cofactor assembly in plants. Annu. Rev. Plant Biol. 2014;65:125–153. doi: 10.1146/annurev-arplant-050213-035759. [DOI] [PubMed] [Google Scholar]
- 22.Braymer J.J., Lill R. Iron-sulfur cluster biogenesis and trafficking in mitochondria. J. Biol. Chem. 2017;292:12754–12763. doi: 10.1074/jbc.R117.787101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sheftel A., Stehling O., Lill R. Iron-sulfur proteins in health and disease. Trends Endocrinol. Metab. 2010;21:302–314. doi: 10.1016/j.tem.2009.12.006. [DOI] [PubMed] [Google Scholar]
- 24.Sheftel A.D., Wilbrecht C., Stehling O., Niggemeyer B., Elsässer H.P., Mühlenhoff U., Lill R. The human mitochondrial ISCA1, ISCA2, and IBA57 proteins are required for [4Fe-4S] protein maturation. Mol. Biol. Cell. 2012;23:1157–1166. doi: 10.1091/mbc.e11-09-0772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Weiler B.D., Brück M.-C., Kothe I., Bill E., Lill R., Mühlenhoff U. Mitochondrial [4Fe-4S] protein assembly involves reductive [2Fe-2S] cluster fusion on ISCA1–ISCA2 by electron flow from ferredoxin FDX2. Proc. Natl. Acad. Sci. USA. 2020 doi: 10.1073/pnas.2003982117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Sheftel A.D., Stehling O., Pierik A.J., Netz D.J., Kerscher S., Elsässer H.P., Wittig I., Balk J., Brandt U., Lill R. Human ind1, an iron-sulfur cluster assembly factor for respiratory complex I. Mol. Cell. Biol. 2009;29:6059–6073. doi: 10.1128/MCB.00817-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Braymer J.J., Stümpfig M., Thelen S., Mühlenhoff U., Lill R. Depletion of thiol reducing capacity impairs cytosolic but not mitochondrial iron-sulfur protein assembly machineries. Biochim. Biophys. Acta Mol.-Cell Res. 2019;1866:240–251. doi: 10.1016/j.bbamcr.2018.11.003. [DOI] [PubMed] [Google Scholar]
- 28.Danielson S.R., Held J.M., Oo M., Riley R., Gibson B.W., Andersen J.K. Quantitative mapping of reversible mitochondrial Complex I cysteine oxidation in a Parkinson disease mouse model. J. Biol. Chem. 2011;286:7601–7608. doi: 10.1074/jbc.M110.190108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Balijepalli S., Boyd M.R., Ravindranath V. Inhibition of mitochondrial complex I by haloperidol: The role of thiol oxidation. Neuropharmacology. 1999;38:567–577. doi: 10.1016/S0028-3908(98)00215-9. [DOI] [PubMed] [Google Scholar]
- 30.Chinta S.J., Andersen J.K. Redox imbalance in Parkinson’s disease. Biochim. Biophys. Acta BBA-Gen. Subj. 2008;1780:1362–1367. doi: 10.1016/j.bbagen.2008.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Mailloux R.J., Willmore W.G. S-glutathionylation reactions in mitochondrial function and disease. Front. Cell Dev. Biol. 2014;2:68. doi: 10.3389/fcell.2014.00068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kispal G., Csere P., Prohl C., Lill R. The mitochondrial proteins Atm1p and Nfs1p are essential for biogenesis of cytosolic Fe/S proteins. EMBO J. 1999;18:3981–3989. doi: 10.1093/emboj/18.14.3981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Srinivasan V., Pierik A.J., Lill R. Crystal structures of nucleotide-free and glutathione-bound mitochondrial ABC transporter Atm1. Science. 2014;343:1137–1140. doi: 10.1126/science.1246729. [DOI] [PubMed] [Google Scholar]
- 34.Lill R., Srinivasan V., Mühlenhoff U. The role of mitochondria in cytosolic-nuclear iron–sulfur protein biogenesis and in cellular iron regulation. Curr. Opin. Microbiol. 2014;22:111–119. doi: 10.1016/j.mib.2014.09.015. [DOI] [PubMed] [Google Scholar]
- 35.Schaedler T.A., Faust B., Shintre C.A., Carpenter E.P., Srinivasan V., van Veen H.W., Balk J. Structures and functions of mitochondrial ABC transporters. Biochem. Soc. Trans. 2015;43:943–951. doi: 10.1042/BST20150118. [DOI] [PubMed] [Google Scholar]
- 36.Bekri S., Kispal G., Lange H., Fitzsimons E., Tolmie J., Lill R., Bishop D.F. Human ABC7 transporter: Gene structure and mutation causing X-linked sideroblastic anemia with ataxia with disruption of cytosolic iron-sulfur protein maturation. Blood. 2000;96:3256–3264. doi: 10.1182/blood.V96.9.3256. [DOI] [PubMed] [Google Scholar]
- 37.D’Hooghe M., Selleslag D., Mortier G., Van Coster R., Vermeersch P., Billiet J., Bekri S. X-linked sideroblastic anemia and ataxia: A new family with identification of a fourth ABCB7 gene mutation. Eur. J. Paediatr. Neurol. 2012;16:730–735. doi: 10.1016/j.ejpn.2012.02.003. [DOI] [PubMed] [Google Scholar]
- 38.Schaedler T.A., Thornton J.D., Kruse I., Schwarzländer M., Meyer A.J., van Veen H.W., Balk J. A conserved mitochondrial ATP-binding cassette transporter exports glutathione polysulfide for cytosolic metal cofactor assembly. J. Biol. Chem. 2014;289:23264–23274. doi: 10.1074/jbc.M114.553438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Li J., Cowan J.A. Glutathione-coordinated [2Fe-2S] cluster: A viable physiological substrate for mitochondrial ABCB7 transport. Chem. Commun. Camb. Engl. 2015;51:2253–2255. doi: 10.1039/C4CC09175B. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Pearson S.A., Wachnowsky C., Cowan J.A. Defining the mechanism of the mitochondrial Atm1p [2Fe–2S] cluster exporter. Metallomics. 2020;12:902–915. doi: 10.1039/C9MT00286C. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Fidai I., Wachnowsky C., Cowan J.A. Glutathione-complexed [2Fe-2S] clusters function in Fe-S cluster storage and trafficking. J. Biol. Inorg. Chem. JBIC Publ. Soc. Biol. Inorg. Chem. 2016;21:887–901. doi: 10.1007/s00775-016-1387-2. [DOI] [PubMed] [Google Scholar]
- 42.Lill R. Function and biogenesis of iron-sulphur proteins. Nature. 2009;460:831–838. doi: 10.1038/nature08301. [DOI] [PubMed] [Google Scholar]
- 43.Webert H., Freibert S.A., Gallo A., Heidenreich T., Linne U., Amlacher S., Hurt E., Mühlenhoff U., Banci L., Lill R. Functional reconstitution of mitochondrial Fe/S cluster synthesis on Isu1 reveals the involvement of ferredoxin. Nat. Commun. 2014;5:1–12. doi: 10.1038/ncomms6013. [DOI] [PubMed] [Google Scholar]
- 44.Vernis L., Facca C., Delagoutte E., Soler N., Chanet R., Guiard B., Faye G., Baldacci G. A newly identified essential complex, Dre2-Tah18, controls mitochondria integrity and cell death after oxidative stress in yeast. PLoS ONE. 2009;4:e4376. doi: 10.1371/journal.pone.0004376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Netz D.J., Stümpfig M., Doré C., Mühlenhoff U., Pierik A.J., Lill R. Tah18 transfers electrons to Dre2 in cytosolic iron-sulfur protein biogenesis. Nat. Chem. Biol. 2010;6:758–765. doi: 10.1038/nchembio.432. [DOI] [PubMed] [Google Scholar]
- 46.Banci L., Bertini I., Calderone V., Ciofi-Baffoni S., Giachetti A., Jaiswal D., Mikolajczyk M., Piccioli M., Winkelmann J. Molecular view of an electron transfer process essential for iron–sulfur protein biogenesis. Proc. Natl. Acad. Sci. USA. 2013;110:7136–7141. doi: 10.1073/pnas.1302378110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Balk J., Pierik A.J., Netz D.J., Mühlenhoff U., Lill R. The hydrogenase-like Nar1p is essential for maturation of cytosolic and nuclear iron-sulphur proteins. EMBO J. 2004;23:2105–2115. doi: 10.1038/sj.emboj.7600216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Balk J., Aguilar Netz D.J., Tepper K., Pierik A.J., Lill R. The essential WD40 protein Cia1 is involved in a late step of cytosolic and nuclear iron-sulfur protein assembly. Mol. Cell. Biol. 2005;25:10833–10841. doi: 10.1128/MCB.25.24.10833-10841.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Song D., Lee F.S. A role for IOP1 in mammalian cytosolic iron-sulfur protein biogenesis. J. Biol. Chem. 2008;283:9231–9238. doi: 10.1074/jbc.M708077200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Netz D.J., Pierik A.J., Stümpfig M., Bill E., Sharma A.K., Pallesen L.J., Walden W.E., Lill R. A bridging [4Fe-4S] cluster and nucleotide binding are essential for function of the Cfd1-Nbp35 complex as a scaffold in iron-sulfur protein maturation. J. Biol. Chem. 2012;287:12365–12378. doi: 10.1074/jbc.M111.328914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Mühlenhoff U., Molik S., Godoy J.R., Uzarska M.A., Richter N., Seubert A., Zhang Y., Stubbe J., Pierrel F., Herrero E., et al. Cytosolic monothiol glutaredoxins function in intracellular iron sensing and trafficking via their bound iron-sulfur cluster. Cell Metab. 2010;12:373–385. doi: 10.1016/j.cmet.2010.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Haunhorst P., Hanschmann E.M., Bräutigam L., Stehling O., Hoffmann B., Mühlenhoff U., Lill R., Berndt C., Lillig C.H. Crucial function of vertebrate glutaredoxin 3 (PICOT) in iron homeostasis and hemoglobin maturation. Mol. Biol. Cell. 2013;24:1895–1903. doi: 10.1091/mbc.e12-09-0648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Li H., Mapolelo D.T., Randeniya S., Johnson M.K., Outten C.E. Human Glutaredoxin 3 Forms [2Fe-2S]-Bridged Complexes with Human BolA2. Biochemistry. 2012;51:1687–1696. doi: 10.1021/bi2019089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Dhalleine T., Rouhier N., Couturier J. Putative roles of glutaredoxin-BolA holo-heterodimers in plants. Plant Signal. Behav. 2014;9:e28564. doi: 10.4161/psb.28564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Roret T., Tsan P., Couturier J., Zhang B., Johnson M.K., Rouhier N., Didierjean C. Structural and spectroscopic insights into BolA-glutaredoxin complexes. J. Biol. Chem. 2014;289:24588–24598. doi: 10.1074/jbc.M114.572701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Banci L., Camponeschi F., Ciofi-Baffoni S., Muzzioli R. Elucidating the Molecular Function of Human BOLA2 in GRX3-Dependent Anamorsin Maturation Pathway. J. Am. Chem. Soc. 2015;137:16133–16143. doi: 10.1021/jacs.5b10592. [DOI] [PubMed] [Google Scholar]
- 57.Seki M., Takeda Y., Iwai K., Tanaka K. IOP1 protein is an external component of the human cytosolic iron-sulfur cluster assembly (CIA) machinery and functions in the MMS19 protein-dependent CIA pathway. J. Biol. Chem. 2013;288:16680–16689. doi: 10.1074/jbc.M112.416602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Stehling O., Vashisht A.A., Mascarenhas J., Jonsson Z.O., Sharma T., Netz D.J., Pierik A.J., Wohlschlegel J.A., Lill R. MMS19 assembles iron-sulfur proteins required for DNA metabolism and genomic integrity. Science. 2012;337:195–199. doi: 10.1126/science.1219723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Urzica E., Pierik A.J., Mühlenhoff U., Lill R. Crucial role of conserved cysteine residues in the assembly of two iron-sulfur clusters on the CIA protein Nar1. Biochemistry. 2009;48:4946–4958. doi: 10.1021/bi900312x. [DOI] [PubMed] [Google Scholar]
- 60.Gari K., León Ortiz A.M., Borel V., Flynn H., Skehel J.M., Boulton S.J. MMS19 links cytoplasmic iron-sulfur cluster assembly to DNA metabolism. Science. 2012;337:243–245. doi: 10.1126/science.1219664. [DOI] [PubMed] [Google Scholar]
- 61.Hanschmann E.-M., Godoy J.R., Berndt C., Hudemann C., Lillig C.H. Thioredoxins, glutaredoxins, and peroxiredoxins—Molecular mechanisms and health significance: From cofactors to antioxidants to redox signaling. Antioxid. Redox Signal. 2013;19:1539–1605. doi: 10.1089/ars.2012.4599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Holmgren A. Glutathione-dependent synthesis of deoxyribonucleotides. Characterization of the enzymatic mechanism of Escherichia coli glutaredoxin. J. Biol. Chem. 1979;254:3672–3678. [PubMed] [Google Scholar]
- 63.Mieyal J.J., Gallogly M.M., Qanungo S., Sabens E.A., Shelton M.D. Molecular mechanisms and clinical implications of reversible protein S-glutathionylation. Antioxid. Redox Signal. 2008;10:1941–1988. doi: 10.1089/ars.2008.2089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Gallogly M.M., Mieyal J.J. Mechanisms of reversible protein glutathionylation in redox signaling and oxidative stress. Curr. Opin. Pharmacol. 2007;7:381–391. doi: 10.1016/j.coph.2007.06.003. [DOI] [PubMed] [Google Scholar]
- 65.Sabens Liedhegner E.A., Gao X.-H., Mieyal J.J. Mechanisms of altered redox regulation in neurodegenerative diseases-focus on s-glutathionylation. Antioxid. Redox Signal. 2012;16:543–566. doi: 10.1089/ars.2011.4119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Lillig C.H., Berndt C., Holmgren A. Glutaredoxin systems. Biochim. Biophys. Acta. 2008;1780:1304–1317. doi: 10.1016/j.bbagen.2008.06.003. [DOI] [PubMed] [Google Scholar]
- 67.Holmgren A., Johansson C., Berndt C., Lönn M.E., Hudemann C., Lillig C.H. Thiol redox control via thioredoxin and glutaredoxin systems. Biochem. Soc. Trans. 2005;33:1375–1377. doi: 10.1042/BST0331375. [DOI] [PubMed] [Google Scholar]
- 68.Tamarit J., Belli G., Cabiscol E., Herrero E., Ros J. Biochemical characterization of yeast mitochondrial Grx5 monothiol glutaredoxin. J. Biol. Chem. 2003;278:25745–25751. doi: 10.1074/jbc.M303477200. [DOI] [PubMed] [Google Scholar]
- 69.Sagemark J., Elgán T.H., Bürglin T.R., Johansson C., Holmgren A., Berndt K.D. Redox properties and evolution of human glutaredoxins. Proteins. 2007;68:879–892. doi: 10.1002/prot.21416. [DOI] [PubMed] [Google Scholar]
- 70.Gallogly M.M., Starke D.W., Leonberg A.K., Ospina S.M.E., Mieyal J.J. Kinetic and mechanistic characterization and versatile catalytic properties of mammalian glutaredoxin 2: Implications for intracellular roles. Biochemistry. 2008;47:11144–11157. doi: 10.1021/bi800966v. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Mesecke N., Spang A., Deponte M., Herrmann J.M. A novel group of glutaredoxins in the cis-Golgi critical for oxidative stress resistance. Mol. Biol. Cell. 2008;19:2673–2680. doi: 10.1091/mbc.e07-09-0896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Ströher E., Millar A.H. The biological roles of glutaredoxins. Biochem. J. 2012;446:333–348. doi: 10.1042/BJ20112131. [DOI] [PubMed] [Google Scholar]
- 73.Rodríguez-Manzaneque M.T., Tamarit J., Bellí G., Ros J., Herrero E. Grx5 is a mitochondrial glutaredoxin required for the activity of iron/sulfur enzymes. Mol. Biol. Cell. 2002;13:1109–1121. doi: 10.1091/mbc.01-10-0517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Bandyopadhyay S., Gama F., Molina-Navarro M.M., Gualberto J.M., Claxton R., Naik S.G., Huynh B.H., Herrero E., Jacquot J.P., Johnson M.K., et al. Chloroplast monothiol glutaredoxins as scaffold proteins for the assembly and delivery of [2Fe–2S] clusters. EMBO J. 2008;27:1122–1133. doi: 10.1038/emboj.2008.50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Gravina S.A., Mieyal J.J. Thioltransferase is a specific glutathionyl mixed disulfide oxidoreductase. Biochemistry. 1993;32:3368–3376. doi: 10.1021/bi00064a021. [DOI] [PubMed] [Google Scholar]
- 76.Zahedi Avval F., Holmgren A. Molecular mechanisms of thioredoxin and glutaredoxin as hydrogen donors for Mammalian s phase ribonucleotide reductase. J. Biol. Chem. 2009;284:8233–8240. doi: 10.1074/jbc.M809338200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Lönn M.E., Hudemann C., Berndt C., Cherkasov V., Capani F., Holmgren A., Lillig C.H. Expression Pattern of Human Glutaredoxin 2 Isoforms: Identification and Characterization of Two Testis/Cancer Cell-Specific Isoforms. Antioxid. Redox Signal. 2008;10:547–558. doi: 10.1089/ars.2007.1821. [DOI] [PubMed] [Google Scholar]
- 78.Johansson C., Lillig C.H., Holmgren A. Human Mitochondrial Glutaredoxin Reduces S-Glutathionylated Proteins with High Affinity Accepting Electrons from Either Glutathione or Thioredoxin Reductase. J. Biol. Chem. 2004;279:7537–7543. doi: 10.1074/jbc.M312719200. [DOI] [PubMed] [Google Scholar]
- 79.Lundberg M., Johansson C., Chandra J., Enoksson M., Jacobsson G., Ljung J., Johansson M., Holmgren A. Cloning and expression of a novel human glutaredoxin (Grx2) with mitochondrial and nuclear isoforms. J. Biol. Chem. 2001;276:26269–26275. doi: 10.1074/jbc.M011605200. [DOI] [PubMed] [Google Scholar]
- 80.Haunhorst P., Berndt C., Eitner S., Godoy J.R., Lillig C.H. Characterization of the human monothiol glutaredoxin 3 (PICOT) as iron-sulfur protein. Biochem. Biophys. Res. Commun. 2010;394:372–376. doi: 10.1016/j.bbrc.2010.03.016. [DOI] [PubMed] [Google Scholar]
- 81.Johansson C., Roos A.K., Montano S.J., Sengupta R., Filippakopoulos P., Guo K., Von Delft F., Holmgren A., Oppermann U., Kavanagh K.L. The crystal structure of human GLRX5: Iron-sulfur cluster co-ordination, tetrameric assembly and monomer activity. Biochem. J. 2011;433:303–311. doi: 10.1042/BJ20101286. [DOI] [PubMed] [Google Scholar]
- 82.Camaschella C., Campanella A., De Falco L., Boschetto L., Merlini R., Silvestri L., Levi S., Iolascon A. The human counterpart of zebrafish shiraz shows sideroblastic-like microcytic anemia and iron overload. Blood. 2007;110:1353–1358. doi: 10.1182/blood-2007-02-072520. [DOI] [PubMed] [Google Scholar]
- 83.Feng Y., Zhong N., Rouhier N., Hase T., Kusunoki M., Jacquot J.P., Jin C., Xia B. Structural insight into poplar glutaredoxin C1 with a bridging iron-sulfur cluster at the active site. Biochemistry. 2006;45:7998–8008. doi: 10.1021/bi060444t. [DOI] [PubMed] [Google Scholar]
- 84.Rouhier N., Unno H., Bandyopadhyay S., Masip L., Kim S.K., Hirasawa M., Gualberto J.M., Lattard V., Kusunoki M., Knaff D.B., et al. Functional, structural, and spectroscopic characterization of a glutathione-ligated [2Fe-2S] cluster in poplar glutaredoxin C1. Proc. Natl. Acad. Sci. USA. 2007;104:7379–7384. doi: 10.1073/pnas.0702268104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Berndt C., Hudemann C., Hanschmann E.-M., Axelsson R., Holmgren A., Lillig C.H. How does iron-sulfur cluster coordination regulate the activity of human glutaredoxin 2? Antioxid. Redox Signal. 2007;9:151–157. doi: 10.1089/ars.2007.9.151. [DOI] [PubMed] [Google Scholar]
- 86.Johansson C., Kavanagh K.L., Gileadi O., Oppermann U. Reversible sequestration of active site cysteines in a 2Fe-2S-bridged dimer provides a mechanism for glutaredoxin 2 regulation in human mitochondria. J. Biol. Chem. 2007;282:3077–3082. doi: 10.1074/jbc.M608179200. [DOI] [PubMed] [Google Scholar]
- 87.Iwema T., Picciocchi A., Traore D.A.K., Ferrer J.-L., Chauvat F., Jacquamet L. Structural Basis for Delivery of the Intact [Fe2S2] Cluster by Monothiol Glutaredoxin. Biochemistry. 2009;48:6041–6043. doi: 10.1021/bi900440m. [DOI] [PubMed] [Google Scholar]
- 88.Lepka K., Volbracht K., Bill E., Schneider R., Rios N., Hildebrandt T., Ingwersen J., Prozorovski T., Lillig C.H., van Horssen J., et al. Iron-sulfur glutaredoxin 2 protects oligodendrocytes against damage induced by nitric oxide release from activated microglia. Glia. 2017;65:1521–1534. doi: 10.1002/glia.23178. [DOI] [PubMed] [Google Scholar]
- 89.Couturier J., Przybyla-Toscano J., Roret T., Didierjean C., Rouhier N. The roles of glutaredoxins ligating Fe–S clusters: Sensing, transfer or repair functions? Biochim. Biophys. Acta BBA-Mol. Cell Res. 2015;1853:1513–1527. doi: 10.1016/j.bbamcr.2014.09.018. [DOI] [PubMed] [Google Scholar]
- 90.Li L., Cheng N., Hirschi K.D., Wang X. Structure of Arabidopsis chloroplastic monothiol glutaredoxin AtGRXcp. Acta Crystallogr. D Biol. Crystallogr. 2010;66:725–732. doi: 10.1107/S0907444910013119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Wang L., Li Y., Jacquot J.-P., Rouhier N., Xia B. Characterization of poplar GrxS14 in different structural forms. Protein Cell. 2014;5:329–333. doi: 10.1007/s13238-014-0042-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Trnka D., Engelke A.D., Gellert M., Moseler A., Hossain M.F., Lindenberg T.T., Pedroletti L., Odermatt B., de Souza J.V., Bronowska A.K., et al. Molecular basis for the distinct functions of redox-active and FeS-transfering glutaredoxins. Nat. Commun. 2020;11:3445. doi: 10.1038/s41467-020-17323-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Liedgens L., Zimmermann J., Wäschenbach L., Geissel F., Laporte H., Gohlke H., Morgan B., Deponte M. Quantitative assessment of the determinant structural differences between redox-active and inactive glutaredoxins. Nat. Commun. 2020;11:1725. doi: 10.1038/s41467-020-15441-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Gladyshev V.N., Liu A., Novoselov S.V., Krysan K., Sun Q.A., Kryukov V.M., Kryukov G.V., Lou M.F. Identification and characterization of a new mammalian glutaredoxin (thioltransferase), Grx2. J. Biol. Chem. 2001;276:30374–30380. doi: 10.1074/jbc.M100020200. [DOI] [PubMed] [Google Scholar]
- 95.Beer S.M., Taylor E.R., Brown S.E., Dahm C.C., Costa N.J., Runswick M.J., Murphy M.P. Glutaredoxin 2 catalyzes the reversible oxidation and glutathionylation of mitochondrial membrane thiol proteins: Implications for mitochondrial redox regulation and antioxidant DEFENSE. J. Biol. Chem. 2004;279:47939–47951. doi: 10.1074/jbc.M408011200. [DOI] [PubMed] [Google Scholar]
- 96.Hudemann C., Lönn M.E., Godoy J.R., Avval F.Z., Capani F., Holmgren A., Lillig C.H. Identification, expression pattern, and characterization of mouse glutaredoxin 2 isoforms. Antioxid. Redox Signal. 2009;11:1–14. doi: 10.1089/ars.2008.2068. [DOI] [PubMed] [Google Scholar]
- 97.Scalcon V., Tonolo F., Folda A., Bindoli A., Rigobello M.P. Dimers of glutaredoxin 2 as mitochondrial redox sensors in selenite-induced oxidative stress. Metallomics. 2019;11:1241–1251. doi: 10.1039/C9MT00090A. [DOI] [PubMed] [Google Scholar]
- 98.Wu H., Xing K., Lou M.F. Glutaredoxin 2 prevents H2O2-induced cell apoptosis by protecting complex I activity in the mitochondria. Biochim. Biophys. Acta. 2010;1797:1705–1715. doi: 10.1016/j.bbabio.2010.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Diotte N.M., Xiong Y., Gao J., Chua B.H.L., Ho Y.-S. Attenuation of doxorubicin-induced cardiac injury by mitochondrial glutaredoxin 2. Biochim. Biophys. Acta. 2009;1793:427–438. doi: 10.1016/j.bbamcr.2008.10.014. [DOI] [PubMed] [Google Scholar]
- 100.Enoksson M., Fernandes A.P., Prast S., Lillig C.H., Holmgren A., Orrenius S. Overexpression of glutaredoxin 2 attenuates apoptosis by preventing cytochrome c release. Biochem. Biophys. Res. Commun. 2005;327:774–779. doi: 10.1016/j.bbrc.2004.12.067. [DOI] [PubMed] [Google Scholar]
- 101.Kanaan G.N., Ichim B., Gharibeh L., Maharsy W., Patten D.A., Xuan J.Y., Reunov A., Marshall P., Veinot J., Menzies K., et al. Glutaredoxin-2 controls cardiac mitochondrial dynamics and energetics in mice, and protects against human cardiac pathologies. Redox Biol. 2018;14:509–521. doi: 10.1016/j.redox.2017.10.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Young A., Gardiner D., Kuksal N., Gill R., O’Brien M., Mailloux R.J. Deletion of the Glutaredoxin-2 Gene Protects Mice from Diet-Induced Weight Gain, Which Correlates with Increased Mitochondrial Respiration and Proton Leaks in Skeletal Muscle. Antioxid. Redox Signal. 2019;31:1272–1288. doi: 10.1089/ars.2018.7715. [DOI] [PubMed] [Google Scholar]
- 103.Bräutigam L., Schütte L.D., Godoy J.R., Prozorovski T., Gellert M., Hauptmann G., Holmgren A., Lillig C.H., Berndt C. Vertebrate-specific glutaredoxin is essential for brain development. Proc. Natl. Acad. Sci. USA. 2011;108:20532–20537. doi: 10.1073/pnas.1110085108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Bräutigam L., Jensen L.D.E., Poschmann G., Nyström S., Bannenberg S., Dreij K., Lepka K., Prozorovski T., Montano S.J., Aktas O., et al. Glutaredoxin regulates vascular development by reversible glutathionylation of sirtuin 1. Proc. Natl. Acad. Sci. USA. 2013;110:20057–20062. doi: 10.1073/pnas.1313753110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Berndt C., Lillig C.H., Holmgren A. Thiol-based mechanisms of the thioredoxin and glutaredoxin systems: Implications for diseases in the cardiovascular system. Am. J. Physiol. Heart Circ. Physiol. 2007;292:H1227–H1236. doi: 10.1152/ajpheart.01162.2006. [DOI] [PubMed] [Google Scholar]
- 106.Berndt C., Poschmann G., Stühler K., Holmgren A., Bräutigam L. Zebrafish heart development is regulated via glutaredoxin 2 dependent migration and survival of neural crest cells. Redox Biol. 2014;2:673–678. doi: 10.1016/j.redox.2014.04.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Gellert M., Richter E., Mostertz J., Kantz L., Masur K., Hanschmann E.M., Ribback S., Kroeger N., Schaeffeler E., Winter S., et al. The cytosolic isoform of glutaredoxin 2 promotes cell migration and invasion. Biochim. Biophys. Acta BBA-Gen. Subj. 2020;1864:129599. doi: 10.1016/j.bbagen.2020.129599. [DOI] [PubMed] [Google Scholar]
- 108.Schütte L.D., Baumeister S., Weis B., Hudemann C., Hanschmann E.-M., Lillig C.H. Identification of potential protein dithiol-disulfide substrates of mammalian Grx2. Biochim. Biophys. Acta. 2013;1830:4999–5005. doi: 10.1016/j.bbagen.2013.07.009. [DOI] [PubMed] [Google Scholar]
- 109.Ye H., Jeong S.Y., Ghosh M.C., Kovtunovych G., Silvestri L., Ortillo D., Uchida N., Tisdale J., Camaschella C., Rouault T.A. Glutaredoxin 5 deficiency causes sideroblastic anemia by specifically impairing heme biosynthesis and depleting cytosolic iron in human erythroblasts. J. Clin. Investig. 2010;120:1749–1761. doi: 10.1172/JCI40372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Baker P.R., Friederich M.W., Swanson M.A., Shaikh T., Bhattacharya K., Scharer G.H., Aicher J., Creadon-Swindell G., Geiger E., MacLean K.N., et al. Variant non ketotic hyperglycinemia is caused by mutations in LIAS, BOLA3 and the novel gene GLRX5. Brain J. Neurol. 2014;137:366–379. doi: 10.1093/brain/awt328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Ciofi-Baffoni S., Nasta V., Banci L. Protein networks in the maturation of human iron–sulfur proteins. Metallomics. 2018;10:49–72. doi: 10.1039/C7MT00269F. [DOI] [PubMed] [Google Scholar]
- 112.Das D., Patra S., Bridwell-Rabb J., Barondeau D.P. Mechanism of frataxin “bypass” in human iron-sulfur cluster biosynthesis with implications for Friedreich’s ataxia. J. Biol. Chem. 2019;294:9276–9284. doi: 10.1074/jbc.RA119.007716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Bonomi F., Iametti S., Morleo A., Ta D., Vickery L.E. Facilitated transfer of IscU-[2Fe2S] clusters by chaperone-mediated ligand exchange. Biochemistry. 2011;50:9641–9650. doi: 10.1021/bi201123z. [DOI] [PubMed] [Google Scholar]
- 114.Uzarska M.A., Dutkiewicz R., Freibert S.-A., Lill R., Mühlenhoff U. The mitochondrial Hsp70 chaperone Ssq1 facilitates Fe/S cluster transfer from Isu1 to Grx5 by complex formation. Mol. Biol. Cell. 2013;24:1830–1841. doi: 10.1091/mbc.e12-09-0644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Olive J.A., Cowan J.A. Role of the HSPA9/HSC20 chaperone pair in promoting directional human iron-sulfur cluster exchange involving monothiol glutaredoxin 5. J. Inorg. Biochem. 2018;184:100–107. doi: 10.1016/j.jinorgbio.2018.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Melber A., Na U., Vashisht A., Weiler B.D., Lill R., Wohlschlegel J.A., Winge D.R. Role of Nfu1 and Bol3 in iron-sulfur cluster transfer to mitochondrial clients. Elife. 2016;5:e15991. doi: 10.7554/eLife.15991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Uzarska M.A., Nasta V., Weiler B.D., Spantgar F., Ciofi-Baffoni S., Saviello M.R., Gonnelli L., Mühlenhoff U., Banci L., Lill R. Mitochondrial Bol1 and Bol3 function as assembly factors for specific iron-sulfur proteins. Elife. 2016;5:e16673. doi: 10.7554/eLife.16673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Nasta V., Giachetti A., Ciofi-Baffoni S., Banci L. Structural insights into the molecular function of human [2Fe-2S] BOLA1-GRX5 and [2Fe-2S] BOLA3-GRX5 complexes. Biochim. Biophys. Acta Gen. Subj. 2017;1861:2119–2131. doi: 10.1016/j.bbagen.2017.05.005. [DOI] [PubMed] [Google Scholar]
- 119.Kim K.-D., Chung W.-H., Kim H.-J., Lee K.-C., Roe J.-H. Monothiol glutaredoxin Grx5 interacts with Fe-S scaffold proteins Isa1 and Isa2 and supports Fe-S assembly and DNA integrity in mitochondria of fission yeast. Biochem. Biophys. Res. Commun. 2010;392:467–472. doi: 10.1016/j.bbrc.2010.01.051. [DOI] [PubMed] [Google Scholar]
- 120.Zinskie J.A., Ghosh A., Trainor B.M., Shedlovskiy D., Pestov D.G., Shcherbik N. Iron-dependent cleavage of ribosomal RNA during oxidative stress in the yeast Saccharomyces cerevisiae. J. Biol. Chem. 2018;293:14237–14248. doi: 10.1074/jbc.RA118.004174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Wingert R.A., Galloway J.L., Barut B., Foott H., Fraenkel P., Axe J.L., Weber G.J., Dooley K., Davidson A.J., Schmidt B., et al. Deficiency of glutaredoxin 5 reveals Fe-S clusters are required for vertebrate haem synthesis. Nature. 2005;436:1035–1039. doi: 10.1038/nature03887. [DOI] [PubMed] [Google Scholar]
- 122.Fidai I., Wachnowsky C., Cowan J.A. Mapping cellular Fe-S cluster uptake and exchange reactions-divergent pathways for iron-sulfur cluster delivery to human ferredoxins. Met. Integr. Biometal. Sci. 2016;8:1283–1293. doi: 10.1039/C6MT00193A. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Sen S., Hendricks A.L., Cowan J.A. Cluster exchange reactivity of [2Fe-2S]-bridged heterodimeric BOLA1-GLRX5. FEBS J. 2020 doi: 10.1111/febs.15452. [DOI] [PubMed] [Google Scholar]
- 124.Sen S., Rao B., Wachnowsky C., Cowan J.A. Cluster exchange reactivity of [2Fe-2S] cluster-bridged complexes of BOLA3 with monothiol glutaredoxins. Met. Integr. Biometal. Sci. 2018;10:1282–1290. doi: 10.1039/C8MT00128F. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Banci L., Ciofi-Baffoni S., Gajda K., Muzzioli R., Peruzzini R., Winkelmann J. N-terminal domains mediate [2Fe-2S] cluster transfer from glutaredoxin-3 to anamorsin. Nat. Chem. Biol. 2015;11:772–778. doi: 10.1038/nchembio.1892. [DOI] [PubMed] [Google Scholar]
- 126.Nasta V., Suraci D., Gourdoupis S., Ciofi-Baffoni S., Banci L. A pathway for assembling [4Fe-4S]2+ clusters in mitochondrial iron-sulfur protein biogenesis. FEBS J. 2020;287:2312–2327. doi: 10.1111/febs.15140. [DOI] [PubMed] [Google Scholar]
- 127.Brancaccio D., Gallo A., Piccioli M., Novellino E., Ciofi-Baffoni S., Banci L. [4Fe-4S] Cluster Assembly in Mitochondria and Its Impairment by Copper. J. Am. Chem. Soc. 2017;139:719–730. doi: 10.1021/jacs.6b09567. [DOI] [PubMed] [Google Scholar]
- 128.Wachnowsky C., Fidai I., Cowan J.A. Cytosolic iron-sulfur cluster transfer-a proposed kinetic pathway for reconstitution of glutaredoxin 3. FEBS Lett. 2016;590:4531–4540. doi: 10.1002/1873-3468.12491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Wachnowsky C., Liu Y., Yoon T., Cowan J.A. Regulation of human Nfu activity in Fe-S cluster delivery-characterization of the interaction between Nfu and the HSPA9/Hsc20 chaperone complex. FEBS J. 2018;285:391–410. doi: 10.1111/febs.14353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Mapolelo D.T., Zhang B., Randeniya S., Albetel A.N., Li H., Couturier J., Outten C.E., Rouhier N., Johnson M.K. Monothiol glutaredoxins and A-type proteins: Partners in Fe-S cluster trafficking. Dalton Trans. Camb. Engl. 2003. 2013;42:3107–3115. doi: 10.1039/c2dt32263c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Shakamuri P., Zhang B., Johnson M.K. Monothiol glutaredoxins function in storing and transporting [Fe2S2] clusters assembled on IscU scaffold proteins. J. Am. Chem. Soc. 2012;134:15213–15216. doi: 10.1021/ja306061x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Moseler A., Aller I., Wagner S., Nietzel T., Przybyla-Toscano J., Mühlenhoff U., Lill R., Berndt C., Rouhier N., Schwarzländer M., et al. The mitochondrial monothiol glutaredoxin S15 is essential for iron-sulfur protein maturation in Arabidopsis thaliana. Proc. Natl. Acad. Sci. USA. 2015;112:13735–13740. doi: 10.1073/pnas.1510835112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Outten C.E., Albetel A.-N. Iron sensing and regulation in Saccharomyces cerevisiae: Ironing out the mechanistic details. Curr. Opin. Microbiol. 2013;16:662–668. doi: 10.1016/j.mib.2013.07.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Mühlenhoff U., Hoffmann B., Richter N., Rietzschel N., Spantgar F., Stehling O., Uzarska M.A., Lill R. Compartmentalization of iron between mitochondria and the cytosol and its regulation. Eur. J. Cell Biol. 2015;94:292–308. doi: 10.1016/j.ejcb.2015.05.003. [DOI] [PubMed] [Google Scholar]
- 135.Stanchi F., Bertocco E., Toppo S., Dioguardi R., Simionati B., Cannata N., Zimbello R., Lanfranchi G., Valle G. Characterization of 16 novel human genes showing high similarity to yeast sequences. Yeast Chichester Engl. 2001;18:69–80. doi: 10.1002/1097-0061(200101)18:1<69::AID-YEA647>3.0.CO;2-H. [DOI] [PubMed] [Google Scholar]
- 136.Witte S., Villalba M., Bi K., Liu Y., Isakov N., Altman A. Inhibition of the c-Jun N-terminal kinase/AP-1 and NF-kappaB pathways by PICOT, a novel protein kinase C-interacting protein with a thioredoxin homology domain. J. Biol. Chem. 2000;275:1902–1909. doi: 10.1074/jbc.275.3.1902. [DOI] [PubMed] [Google Scholar]
- 137.Godoy J.R., Funke M., Ackermann W., Haunhorst P., Oesteritz S., Capani F., Elsässer H.P., Lillig C.H. Redox atlas of the mouse. Immunohistochemical detection of glutaredoxin-, peroxiredoxin-, and thioredoxin-family proteins in various tissues of the laboratory mouse. Biochim. Biophys. Acta. 2011;1810:2–92. doi: 10.1016/j.bbagen.2010.05.006. [DOI] [PubMed] [Google Scholar]
- 138.Lange H., Mühlenhoff U., Denzel M., Kispal G., Lill R. The heme synthesis defect of mutants impaired in mitochondrial iron-sulfur protein biogenesis is caused by reversible inhibition of ferrochelatase. J. Biol. Chem. 2004;279:29101–29108. doi: 10.1074/jbc.M403721200. [DOI] [PubMed] [Google Scholar]
- 139.Cha H., Kim J.M., Oh J.G., Jeong M.H., Park C.S., Park J., Jeong H.J., Park B.K., Lee Y.H., Jeong D., et al. PICOT is a critical regulator of cardiac hypertrophy and cardiomyocyte contractility. J. Mol. Cell. Cardiol. 2008;45:796–803. doi: 10.1016/j.yjmcc.2008.09.124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Jeong D., Cha H., Kim E., Kang M., Yang D.K., Kim J.M., Yoon P.O., Oh J.G., Bernecker O.Y., Sakata S. PICOT inhibits cardiac hypertrophy and enhances ventricular function and cardiomyocyte contractility. Circ. Res. 2006;99:307–314. doi: 10.1161/01.RES.0000234780.06115.2c. [DOI] [PubMed] [Google Scholar]
- 141.Steiner R., Vogel H. On the kinetics of erythroid cell differentiation in fetal mice. I. Microspectrophotometric determination of the hemoglobin content in erythroid cells during gestation. J. Cell. Physiol. 1973;81:323–338. doi: 10.1002/jcp.1040810305. [DOI] [PubMed] [Google Scholar]
- 142.Brotherton T.W., Chui D.H., Gauldie J., Patterson M. Hemoglobin ontogeny during normal mouse fetal development. Proc. Natl. Acad. Sci. USA. 1979;76:2853–2857. doi: 10.1073/pnas.76.6.2853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Ye H., Rouault T.A. Human iron-sulfur cluster assembly, cellular iron homeostasis, and disease. Biochemistry. 2010;49:4945–4956. doi: 10.1021/bi1004798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Rajagopalan B., Francis J.M., Cooke F., Korlipara L.P., Blamire A.M., Schapira A.H., Madan J., Neubauer S., Cooper J.M. Analysis of the factors influencing the cardiac phenotype in Friedreich’s ataxia. Mov. Disord. 2010;25:846–852. doi: 10.1002/mds.22864. [DOI] [PubMed] [Google Scholar]
- 145.Huynen M.A., Spronk C.A.E.M., Gabaldón T., Snel B. Combining data from genomes, Y2H and 3D structure indicates that BolA is a reductase interacting with a glutaredoxin. FEBS Lett. 2005;579:591–596. doi: 10.1016/j.febslet.2004.11.111. [DOI] [PubMed] [Google Scholar]
- 146.Li H., Mapolelo D.T., Dingra N.N., Keller G., Riggs-Gelasco P.J., Winge D.R., Johnson M.K., Outten C.E. Histidine 103 in Fra2 is an iron-sulfur cluster ligand in the [2Fe-2S] Fra2-Grx3 complex and is required for in vivo iron signaling in yeast. J. Biol. Chem. 2011;286:867–876. doi: 10.1074/jbc.M110.184176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Li H., Mapolelo D.T., Dingra N.N., Naik S.G., Lees N.S., Hoffman B.M., Riggs-Gelasco P.J., Huynh B.H., Johnson M.K., Outten C.E. The Yeast Iron Regulatory Proteins Grx3/4 and Fra2 Form Heterodimeric Complexes Containing a [2Fe-2S] Cluster with Cysteinyl and Histidyl Ligation. Biochemistry. 2009;48:9569–9581. doi: 10.1021/bi901182w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Poor C.B., Wegner S.V., Li H., Dlouhy A.C., Schuermann J.P., Sanishvili R., Hinshaw J.R., Riggs-Gelasco P.J., Outten C.E., He C. Molecular mechanism and structure of the Saccharomyces cerevisiae iron regulator Aft2. Proc. Natl. Acad. Sci. USA. 2014;111:4043–4048. doi: 10.1073/pnas.1318869111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Li H., Outten C.E. The conserved CDC motif in the yeast iron regulator Aft2 mediates iron–sulfur cluster exchange and protein–protein interactions with Grx3 and Bol2. JBIC J. Biol. Inorg. Chem. 2019;24:809–815. doi: 10.1007/s00775-019-01705-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Encinar del Dedo J., Gabrielli N., Carmona M., Ayté J., Hidalgo E. A Cascade of Iron-Containing Proteins Governs the Genetic Iron Starvation Response to Promote Iron Uptake and Inhibit Iron Storage in Fission Yeast. PLoS Genet. 2015;11:e1005106. doi: 10.1371/journal.pgen.1005106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Lill R., Freibert S.-A. Mechanisms of Mitochondrial Iron-Sulfur Protein Biogenesis. Annu. Rev. Biochem. 2020;89:471–499. doi: 10.1146/annurev-biochem-013118-111540. [DOI] [PubMed] [Google Scholar]
- 152.Liu T., Zhang M., Terry M.H., Schroeder H., Wilson S.M., Power G.G., Li Q., Tipple T.E., Borchardt D., Blood A.B. Hemodynamic Effects of Glutathione-Liganded Binuclear Dinitrosyl Iron Complex: Evidence for Nitroxyl Generation and Modulation by Plasma Albumin. Mol. Pharmacol. 2018;93:427–437. doi: 10.1124/mol.117.110957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Vanin A.F. Dinitrosyl iron complexes with thiolate ligands: Physico-chemistry, biochemistry and physiology. Nitric Oxide Biol. Chem. 2009;21:1–13. doi: 10.1016/j.niox.2009.03.005. [DOI] [PubMed] [Google Scholar]
- 154.Borodulin R.R., Dereven’kov I.A., Burbaev D.S., Makarov S.V., Mikoyan V.D., Serezhenkov V.A., Kubrina L.N., Ivanovic-Burmazovic I., Vanin A.F. Redox activities of mono- and binuclear forms of low-molecular and protein-bound dinitrosyl iron complexes with thiol-containing ligands. Nitric Oxide Biol. Chem. 2014;40:100–109. doi: 10.1016/j.niox.2014.06.005. [DOI] [PubMed] [Google Scholar]
- 155.Vanin A.F. Dinitrosyl iron complexes with thiol-containing ligands as a “working form” of endogenous nitric oxide. Nitric Oxide. 2016;54:15–29. doi: 10.1016/j.niox.2016.01.006. [DOI] [PubMed] [Google Scholar]
- 156.Landry A.P., Duan X., Huang H., Ding H. Iron-sulfur proteins are the major source of protein-bound dinitrosyl iron complexes formed in Escherichia coli cells under nitric oxide stress. Free Radic. Biol. Med. 2011;50:1582–1590. doi: 10.1016/j.freeradbiomed.2011.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Foster M.W., Hess D.T., Stamler J.S. Protein S-nitrosylation in health and disease: A current perspective. Trends Mol. Med. 2009;15:391–404. doi: 10.1016/j.molmed.2009.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Chen S.C., Huang B., Liu Y.C., Shyu K.G., Lin P.Y., Wang D.L. Acute hypoxia enhances proteins’ S-nitrosylation in endothelial cells. Biochem. Biophys. Res. Commun. 2008;377:1274–1278. doi: 10.1016/j.bbrc.2008.10.144. [DOI] [PubMed] [Google Scholar]
- 159.Murray C.I., Uhrigshardt H., O’Meally R.N., Cole R.N., Van Eyk J.E. Identification and quantification of S-nitrosylation by cysteine reactive tandem mass tag switch assay. Mol. Cell. Proteom. MCP. 2012;11:M111.013441. doi: 10.1074/mcp.M111.013441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Qu Z., Greenlief C.M., Gu Z. Quantitative Proteomic Approaches for Analysis of Protein S-Nitrosylation. J. Proteome Res. 2016;15:1–14. doi: 10.1021/acs.jproteome.5b00857. [DOI] [PubMed] [Google Scholar]
- 161.Anand P., Stamler J.S. Enzymatic mechanisms regulating protein S-nitrosylation: Implications in health and disease. J. Mol. Med. Berl. Ger. 2012;90:233–244. doi: 10.1007/s00109-012-0878-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Borodulin R.R., Kubrina L.N., Mikoyan V.D., Poltorakov A.P., Shvydkiy V.O., Burbaev D.S., Serezhenkov V.A., Yakhontova E.R., Vanin A.F. Dinitrosyl iron complexes with glutathione as NO and NO+ donors. Nitric Oxide. 2013;29:4–16. doi: 10.1016/j.niox.2012.11.001. [DOI] [PubMed] [Google Scholar]
- 163.Heinrich T.A., da Silva R.S., Miranda K.M., Switzer C.H., Wink D.A., Fukuto J.M. Biological nitric oxide signalling: Chemistry and terminology. Br. J. Pharmacol. 2013;169:1417–1429. doi: 10.1111/bph.12217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Martínez-Ruiz A., Lamas S. Detection and proteomic identification of S-nitrosylated proteins in endothelial cells. Arch. Biochem. Biophys. 2004;423:192–199. doi: 10.1016/j.abb.2003.12.006. [DOI] [PubMed] [Google Scholar]
- 165.Truzzi D.R., Alves S.V., Netto L.E.S., Augusto O. The Peroxidatic Thiol of Peroxiredoxin 1 is Nitrosated by Nitrosoglutathione but Coordinates to the Dinitrosyl Iron Complex of Glutathione. Antioxidants. 2020;9:276. doi: 10.3390/antiox9040276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Chazov E.I., Rodnenkov O.V., Zorin A.V., Lakomkin V.L., Gramovich V.V., Vyborov O.N., Dragnev A.G., Timoshin A.A., Buryachkovskaya L.I., Abramov A.A., et al. Hypotensive effect of Oxacom® containing a dinitrosyl iron complex with glutathione: Animal studies and clinical trials on healthy volunteers. Nitric Oxide. 2012;26:148–156. doi: 10.1016/j.niox.2012.01.008. [DOI] [PubMed] [Google Scholar]
- 167.Akentieva N.P., Sanina N.A., Gizatullin A.R., Shkondina N.I., Prikhodchenko T.R., Shram S.I., Zhelev N., Aldoshin S.M. Cytoprotective Effects of Dinitrosyl Iron Complexes on Viability of Human Fibroblasts and Cardiomyocytes. Front. Pharmacol. 2019;10:1277. doi: 10.3389/fphar.2019.01277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Giliano N.Y., Konevega L.V., Noskin L.A., Serezhenkov V.A., Poltorakov A.P., Vanin A.F. Dinitrosyl iron complexes with thiol-containing ligands and apoptosis: Studies with HeLa cell cultures. Nitric Oxide Biol. Chem. 2011;24:151–159. doi: 10.1016/j.niox.2011.02.005. [DOI] [PubMed] [Google Scholar]
- 169.Hou J., He H., Huang S., Qian M., Wang J., Tan X., Han G., Song Y., Xu Z., Liu Y. A mitochondria-targeted nitric oxide donor triggered by superoxide radical to alleviate myocardial ischemia/reperfusion injury. Chem. Commun. 2019;55:1205–1208. doi: 10.1039/C8CC07304J. [DOI] [PubMed] [Google Scholar]
- 170.Burgova E.N., Tkachev N.A., Adamyan L.V., Mikoyan V.D., Paklina O.V., Stepanyan A.A., Vanin A.F. Dinitrosyl iron complexes with glutathione suppress experimental endometriosis in rats. Eur. J. Pharmacol. 2014;727:140–147. doi: 10.1016/j.ejphar.2014.01.002. [DOI] [PubMed] [Google Scholar]
- 171.Pisarenko O.I., Serebryakova L.I., Tskitishvili O.V., Studneva I.M., Vanin A.F., Chazov E.I. Cardioprotective efficacy of dinitrosyl iron complex with L-cysteine in rats in vivo. Biol. Bull. 2008;35:95–98. doi: 10.1134/S1062359008010147. [DOI] [PubMed] [Google Scholar]
- 172.Mordvintsev P.I., Rudneva V.G., Vanin A.F., Shimkevich L.L., Khodorov B.I. Inhibition of platelet aggregation by dinitrosyl iron complexes with low molecular weight ligands. Biokhimiia Mosc. Russ. 1986;51:1851–1857. [PubMed] [Google Scholar]