Abstract
Objectives:
To determine the rates of emergency department (ED) visits and inpatient hospitalizations for genitourinary (GU) complications after spinal cord injury (SCI) using a national sample; to examine which patient and facility factors are associated with inhospital mortality; and to estimate direct medical costs of GU complications after SCI.
Design:
Retrospective cross-sectional and cost analysis of the 2006 to 2015 National Inpatient Sample and National Emergency Department Sample from the Healthcare Cost and Utilization Project.
Participants:
SCI-related encounters using various International Classification of Disease, Ninth Edition, Clinical Modification diagnosis codes. The inpatient sample included 1,796,624 hospitalizations, and the ED sample included 618,118 treat-and-release visits.
Main Outcome Measures:
The exposure included a GU complication, identified by International Classification of Disease, Ninth Edition, Clinical Modification codes 590–599. The outcomes then included an ED visit or hospitalization, death prior to discharge, and direct medical costs estimated from reported hospital charges.
Results:
For the inpatient sample, we observed a 2.5% annual increase (95% confidence interval [CI], 1.8–3.2) in the proportion of SCI-related hospitalizations with any GU complication from 2006 to 2011, and a lesser rate of increase of 0.9% (95% CI, 0.4–1.4) each year from 2011 to 2015. Age, level of injury, and payer source were correlated to inhospital mortality. The costs of GU-related health care use exceeded $4 billion over the study period.
Conclusions:
This study shows the rates and economic burden of health care use associated with GU complications in persons with SCI in the United States. The need to develop strategies to effectively deliver health care to the SCI population for these conditions remains great.
Keywords: Neurogenic bladder, Rehabilitation, Spinal cord injury
Spinal cord injury (SCI) affects approximately 54 people per 1 million in the United States, or about 17,700 new SCI cases each year. There are currently an estimated 288,000 people living with an SCI in the United States.1 Neurogenic bladder is a common secondary condition after SCI, and the associated pathophysio-logical changes render persons with SCI susceptible to urinary tract infections (UTI) and other genitourinary (GU) complications.2 It has been well documented that GU complications are the most common reasons for health care utilization among patients with SCI.3,4 Previous studies have highlighted the morbidity and mortality of GU complications in the SCI population.5
Gaps in knowledge about the full scope of GU complications after SCI remain. Many previous studies obtained data from either the SCI Model Systems Database or the Veterans Health Administration (VHA). The SCI Model Systems Database is a network of 13 SCI centers across the country, sponsored by the National Institute on Disability, Independent Living, and Rehabilitation Research, Administration for Community Living, U.S. Department of Health and Human Services. However, only a subset of persons with SCI are treated at a Model Systems facility. The VHA dedicates an entire system of care to people with SCI, but represents a subpopulation restricted to veterans. There are inherent racial, ethnic, sex, and psychosocial differences in veterans that seek care with the VHA as compared to even the general veteran population.6–8 We do not have clear understanding how the rates of health care encounters associated with GU complications are changing over time among patients with SCI, nor the economic burden of these encounters. We also lack data on patient or facility factors that may be associated with the rate of health care use associated with GU complications, and the subsequent mortality. The objective of this study is to provide a comprehensive view of the burden (including costs) of inpatient and emergency department (ED) health care encounters associated with GU complications among a nationally-representative group of patients with SCI in the United States. We conducted a retrospective analysis of inpatient hospitalization and treat-and-release ED visits using 10 years of data from the National Inpatient Sample (NIS) and Nationwide Emergency Department Sample (NEDS), both developed for the Healthcare Cost and Utilization Project (HCUP) that is sponsored by the Agency for Healthcare Research and Quality. Both the NIS and NEDS are the largest all-payer, publicly available databases of inpatient hospitalization stays and hospital-based ED visits, respectively, in the United States. These HCUP databases will provide the appropriate data to address these gaps.
Methods
Design, settings, participants
Briefly, the NIS contains clinical (eg, diagnoses, procedures, length of stay, inhospital death) and nonclinical (eg, sociodemo-graphics) data from more than 7 million hospitalizations annually (35 million when weighted), and approximates a 20% stratified sample of all United States nonfederal, nonrehabilitation, short-term community hospitals.9,10 Prior to 2012, participating hospitals were stratified by bed size, ownership, teaching status, urban or rural location, and United States census region, and a 2-stage cluster sampling design first selected hospitals as the primary sampling units, and subsequently included all inpatient hospitalizations from the selected hospitals in the final annually-compiled NIS database.9,10 Beginning in 2012, the NIS sampling strategy was modified to select 20% of hospitalizations from all participating hospitals. Our analysis incorporates information provided in HCUP-supplied NIS-Trends files to ensure that sampling weights and data elements were defined consistently over time despite the change in sampling design.
The NEDS contains similar patient and facility-level information as the NIS, and is commonly used to create national and regional estimates of ED care. Unweighted, the NEDS contains data from approximately 31 million ED visits each year; weighted, it estimates roughly 143 million ED visits.11 Both databases provide discharge-level data without identifiers permitting the linkage of encounters for the same patient; therefore, analyses of the NIS and NEDS result in per-encounter (inpatient admission or ED visit), as opposed to per-patient, results.
Each encounter in the NIS and NEDS contains a principal diagnosis code field, and several secondary diagnosis code fields (up to 29 beginning in 2014), documented using International Classification of Diseases, Ninth Edition, Clinical Modification codes. Encounters for patients who are not pregnant and 18 to 80 years of age with SCI were identified using any principal or secondary diagnosis code in the following ranges: (1) fracture of vertebral column with SCI (806.xx); (2) SCI without evidence of spinal bone injury (952.xx); (3) quadriplegia and quadraparesis (344.0x); (4) paraplegia (344.1); and (5) cauda equina syndrome (344.6x). To enhance the clinical utility of these data, specific diagnosis codes reflective of injury level or the resulting paralysis in a hierarchical fashion, resulting in 4 mutually-exclusive groups: (1) cervical, quadriplegia; (2) thoracic, lumbar, sacral, paraplegia; (3) cauda equina; and (4) other SCI. We then identified encounters with an associated GU complication by scanning for the presence of diagnosis codes in the 590.00 to 599.9 code range. We analyzed GU complications both as a whole (1 or more diagnosis code in this range), as well as specific GU complications: (1) infections of kidney (590.xx); (2) hydronephrosis (591); (3) calculus of kidney and ureter (592.xx); (4) other disorders of kidney and ureter (593.xx); (5) calculus of lower urinary tract (594.xx); (6) cystitis (595.xx); (7) other disorders of bladder (596.xx); (8) urethritis not sexually transmitted and urethral syndrome (597.xx); (9) urethral stricture (598.xx); and (10) other disorders of urethra and urinary tract (599.xx, which includes UTI). We then included other patient characteristics— age, sex, race or ethnicity (only available in the NIS), and payer source— as well as hospital region, size, and type.
Despite being compiled using separate sampling strategies, the NIS and NEDS have potentially overlapping samples. The NEDS includes both treat-and-release ED visits and ED visits that subsequently result in inpatient admission, the latter is part of the sampling frame for the NIS. Therefore, in the absence of patient identifiers, to ensure a comprehensive but nonoverlapping analytic database using both NIS and NEDS data, we selected from the NEDS only ED visits that resulted in the patient being treated and released or in which the patient died in the ED. Those ED visits in which the patient was admitted to the same hospital, transferred to another hospital, or in which the destination was unknown were excluded due to the possibility of also being captured in the NIS.
Our primary study outcomes were the frequency and temporal trends in rates of GU complications, and the impact of GU complications (when documented as the principal diagnosis versus a secondary diagnosis) on inhospital mortality, length of stay, and the direct costs of medical care from the provider perspective. We estimated costs from total encounter-level charges reported in the HCUP databases. Unadjusted charges can be a misleading reflection of cost because the markup from the cost for the hospital to provide services to what is ultimately charged can vary substantially across hospitals, among different departments or service units within the same hospital, and over time.12 Therefore, to obtain a more accurate estimate of actual cost, we adjusted total charges per year and hospital-specific cost-to-charge ratio (CCR) obtained from HCUP. When a specific CCR was not available for a hospital, we used a group-average CCR for that hospital based on other hospitals with similar characteristics (location, bed size, ownership, teaching status). We then accounted for inflation by adjusting estimates to 2015 dollars using the medical care component of the Consumer Price Index.13 It is important to note that HCUP does not supply or publish CCR data for the NEDS and the lack of hospital identifiers prevents linking to inpatient CCR for the same hospital. Therefore, in a process described by Peterson et al,14 we first calculated the average inpatient CCR from hospitals with SCI hospitalizations. We then calculated the mean CCR across hospitals by year, region, urban or rural designation, and teaching status, and applied those inpatient SCI-related CCRs to ED visits occurring at hospitals with the same characteristics.
Analysis
We used descriptive statistics including frequencies, percentages, and rates to assess characteristics of inpatient hospitalizations and treat-and-release ED visits among patients 18 to 80 years of age with SCI, stratified by type of encounter and neurologic level of injury. Log-binomial regression was used to estimate prevalence ratios and 95% confidence intervals (CIs) representing the association between various patient and hospital characteristics and the likelihood of (1) GU complications and (2) inhospital mortality. We developed separate models for inpatient and treat-and-release ED encounters, with covariate selection based on the literature, data availability, and empirical bivariate analyses. Then, we estimated the average annual direct medical costs of care of inpatient hospitalizations and treat-and-release ED visits among patients 18 to 80 years with SCI, stratified by type of encounter and presence of any GU complications.
Joinpoint regression was used to estimate and characterize temporal trends in the annual proportion of inpatient hospitalizations and treat-and-release ED visits for SCI that were associated with 1 or more GU complications. Joinpoint regression is a statistical approach that is effective in identifying changes in the rates of events over time. It does so by first fitting annual rate data to a straight line, assuming no joinpoints and that a single trend best reflects rates from 2006 to 2015.15 Then, in an iterative fashion, joinpoints are one-at-a-time added to the model, and a Monte Carlo permutation test is used to determine whether each joinpoint improves model fit; if so, the joinpoint is incorporated. When an optimal number of joinpoints is specified in the final model, each corresponds to a statistically significant change (increase or decrease) in the temporal trend, and how the rate changes within that time interval is described using the annual percent change.
Statistical analyses were performed with SAS version 9.4,a Stata MP 13.1,b and the Joinpoint Regression Program, version 4.1.1.3.c This study was deemed exempt by the Baylor College of Medicine Institutional Review Board, as data in the NIS and NEDS are deidentified and publicly available, thus not meeting the definition of human subject research.
Results
Our analysis included nearly 1.8 million hospitalizations and over 618,000 treat-and-release ED visits among people with SCI during the 10-year study period. Table 1 shows basic sociodemographic information for the patients with SCI in the inpatient and ED samples, respectively, as well as the rates of GU complication during the encounter, stratified by neurologic level of injury. Most inpatient encounters were for male patients (57%–70%) and patients who were non-Hispanic white (54%–64%). Patients hospitalized tended to be slightly older than patients treated and released from the ED, and there were statistically significant differences in the mean age among those classified to the “other SCI” group in both samples (P<.01). Medicare was the most common payer source for every group except the “other SCI” group, where private insurance was more common (P<.01). Overall, the most common principal diagnoses associated with inpatient SCI-related hospitalizations were septicemia (13.4%), rehabilitation care (6.8%), and UTIs (6.7%). For SCI-related ED visits, the most common diagnoses were UTI (16.7%), genitourinary symptoms and ill-defined conditions (4.7%), and complication of a medical device, implant, or graft (4.7%); (data not shown). A GU complication was documented as the primary diagnosis in 8.2% and 18.7% of all SCI-related inpatient hospitalizations and ED visits, respectively. However, a GU complication among all linked diagnoses other than primary occurred in more than half of inpatient and more than one-third of ED visits. “Other disorders of the urinary tract” (which include UTIs) were the most prevalent GU complication subtype across all neurologic levels.
Table 1.
Characteristics of inpatient hospitalizations and treat-and-release emergency department visits among patients with spinal cord injury, 2006–2015
| Characteristic | Inpatient Hospitalizations | Treat-and-Release ED Visits | ||||||
|---|---|---|---|---|---|---|---|---|
| Cervical, Quadriplegia (n=690,742) | Thoracic, Lumbar, Sacral, Paraplegia (n=967,273) | Cauda Equina (n=130,988) | Other (n=7621) | Cervical, Quadriplegia (n=197,147) | Thoracic, Lumbar, Sacral, Paraplegia (n=398,424) | Cauda Equina (n=14,004) | Other (n=8543) | |
| Age (y), mean ± SD | 51±33 | 52±34 | 54±35 | 49±38 | 46±31 | 45±31 | 47±34 | 44±33 |
| Ethnicity, (%) | ||||||||
| Non-Hispanic white | 54.6 | 54.0 | 63.8 | 55.2 | * | * | * | * |
| Non-Hispanic black | 18.5 | 20.6 | 10.5 | 15.3 | * | * | * | * |
| Hispanic | 7.9 | 8.8 | 8.0 | 10.5 | * | * | * | * |
| Other | 5.2 | 4.5 | 5.0 | 4.5 | * | * | * | * |
| Sex, (%) male | 70.3 | 66.3 | 56.6 | 69.2 | 75.1 | 72.1 | 50.6 | 64.7 |
| Payer source, (%) | ||||||||
| Medicare | 51.2 | 52.8 | 39.5 | 30.6 | 52.5 | 46.0 | 34.6 | 21.6 |
| Medicaid | 20.8 | 22.1 | 13.7 | 14.2 | 26.2 | 32.2 | 22.7 | 18.0 |
| Private | 20.7 | 18.4 | 34.8 | 32.9 | 14.6 | 13.4 | 24.7 | 33.7 |
| Other | 7.3 | 6.7 | 12.1 | 22.4 | 6.7 | 8.4 | 17.9 | 26.7 |
| Any GU complication, principal diagnosis, (%) | 7.7 | 9.3 | 3.3 | 3.0 | 18.6 | 19.4 | 9.8 | 5.3 |
| Any GU complication, any diagnosis, (%) | 52.7 | 56.6 | 25.4 | 20.9 | 34.5 | 34.3 | 17.5 | 10.1 |
| Specific GU complications, rate per 1000†, ‡ | ||||||||
| Infection of kidney | 6.6 | 13.0 | 5.3 | 3.7 | 6.3 | 11.1 | 8.6 | 6.4 |
| Hydronephrosis | <1.0 | <1.0 | <1.0 | <1.0 | <1.0 | <1.0 | <1.0 | <1.0 |
| Kidney/ureter stone | 7.0 | 5.7 | 1.9 | <1.0 | 3.1 | 2.8 | 5 | 1.5 |
| Other disorder of kidney or ureter | <1.0 | <1.0 | <1.0 | <1.0 | <1.0 | <1.0 | <1.0 | <1.0 |
| Lower urinary tract stone | 1.1 | 1.0 | <1.0 | 1.3 | <1.0 | <1.0 | <1.0 | <1.0 |
| Cystitis | 2.3 | 2.8 | 1.5 | <1.0 | 7.9 | 10.1 | 3.6 | 3.0 |
| Other disorder of bladder | 4.8 | 5.4 | 0.7 | 3.2 | 5.6 | 4.4 | 3.0 | <1.0 |
| Urethritis, not STI | <1.0 | <1.0 | <1.0 | <1.0 | <1.0 | <1.0 | <1.0 | <1.0 |
| Urethral stricture | <1.0 | <1.0 | <1.0 | <1.0 | <1.0 | <1.0 | <1.0 | <1.0 |
| Other disorders of urinary tract | 53.9 | 63.4 | 21.2 | 19.9 | 16.1 | 16.4 | 7.6 | 4.2 |
Abbreviation: STI, sexually transmitted infection.
Patient race/ethnicity is not available in the NEDS, from which information on treat-and-release ED visits was extracted.
Hospitalizations for patients with more than 1 specific type of GU complication diagnosed were counted in each GU subgroup.
Subgroups with a complication rate of less than 1 per 1000 hospitalizations were expressed as <1.0.
Figure 1 shows temporal trends in rates of inpatient hospitalizations and treat-and-release ED visits with GU complications as the principal diagnosis, and separately as any diagnosis. Figure 1A shows the proportion of hospitalizations for which the GU complication was listed as the principal diagnosis decreased 2.7% each year between 2006 and 2012, and decreased 6.5% each year from 2012 to 2015. There was a small, consistent 1.5% annual increase in the GU complication rate among ED visits, but no temporal changes in the proportion of SCI-related ED visits for which the GU complication was the principal diagnosis. For encounters where a GU complication is listed as any diagnosis (fig 1B), however, we observed a 2.5% annual increase (95% CI, 1.8–3.2) in the proportion of SCI-related hospitalizations with any GU complication from 2006 to 2011, and a lesser rate of increase of 0.9% (95% CI, 0.4–1.4) each year from 2011 to 2015.
Fig 1.
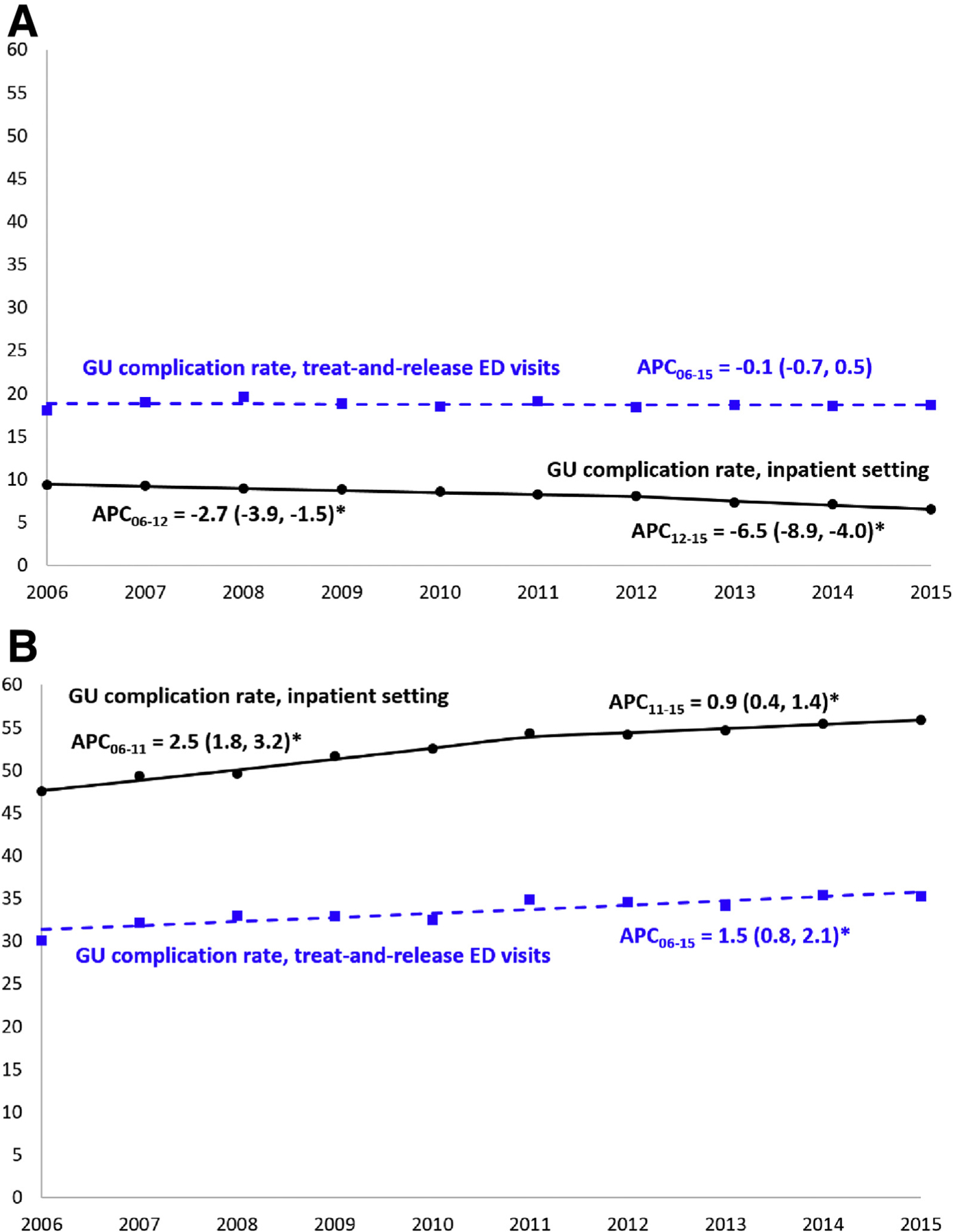
Temporal trends in the proportion of inpatient hospitalizations and treat-and-release ED visits associated with GU complications among patients with SCI, 2006 to 2015. NOTE. The Y-axis represents the proportion (%) of encounters for SCIs that had an indication of 1or more GU complications. APC is expressed as the point estimate and 95% CI. The top panel (A) represents consideration of GU complications only when documented as a principal diagnosis; the bottom panel (B) considers GU complications when documented as any diagnosis made during the medical encounter. Abbreviation: APC, annual percent change. *Statistically significant finding.
Table 2 shows the results of the log-binomial regression analysis exploring the associations of patient and hospital characteristics to mortality prior to discharge in the inpatient and ED setting. Persons with cervical injuries or quadriplegia, compared to those with paraplegia or lower level injuries were 72% (95% CI, 1.65–1.78) more likely to die during an inpatient admission, and twice as likely to die (prevalence ratio=1.98; 95% CI, 1.67–2.35) during an ED visit. Age was directly associated with inhospital mortality, with persons with SCI age 55 to 80 years being more than twice as likely to die as those aged 18 to 24 years. Those with “other” payer source, which included the uninsured and underinsured, were 25% more likely to die during an inpatient admission (95% CI, 1.17–1.35), and 67% more likely to die during an ED visit (95% CI, 1.24–2.25) than those with private insurance.
Table 2.
Associations between patient and hospital characteristics, and mortality prior to discharge, among patients with SCI, 2006–2015
| Mortality Prior to Discharge | ||
|---|---|---|
| Inpatient Hospitalizations Adjusted PR, 95% CI | Treat-and-Release ED Visits Adjusted PR, 95% CI | |
| Injury type | ||
| Cervical/quadriplegia | 1.72 (1.65–1.78) | 1.98 (1.67–2.35) |
| Thoracic, lumbar, sacral/paraplegia | 1.00 | 1.00 |
| Cauda equina | 0.50 (0.45–0.56) | 0.56 (0.26–1.21) |
| Sex | ||
| Male | 1.00 | 1.00 |
| Female | 1.04 (1.00–1.07) | 1.09 (0.91–1.31) |
| Age | ||
| 18–24 | 1.00 | 1.00 |
| 25–34 | 0.81 (0.71–0.92) | 0.65 (0.44–0.97) |
| 35–44 | 1.01 (0.90–1.14) | 0.68 (0.46–1.01) |
| 45–54 | 1.46 (1.32–1.63) | 1.08 (0.75–1.56) |
| 55–80 | 2.72 (2.46–3.01) | 2.15 (1.50–3.10) |
| Race/ethnicity | ||
| Non-Hispanic white | 1.00 | NA |
| Non-Hispanic black | 0.89 (0.85–0.94) | NA |
| Hispanic | 1.00 (0.94–1.07) | NA |
| Other | 1.19 (1.10–1.29) | NA |
| Missing | 1.06 (0.98–1.14) | NA |
| Median household Income | ||
| Lowest | 1.09 (1.03–1.16) | 0.89 (0.67–1.18) |
| 2nd | 1.09 (1.03–1.16) | 1.12 (0.86–1.46) |
| 3rd | 1.05 (0.99, 1.11) | 1.05 (0.81–1.37) |
| Highest | 1.00 | 1.00 |
| Primary payer | ||
| Medicare | 0.90 (0.86–0.95) | 0.86 (0.67–1.09) |
| Medicaid | 0.91 (0.85–0.97) | 0.66 (0.49–0.90) |
| Private | 1.00 | 1.00 |
| Other | 1.25 (1.17–1.35) | 1.67 (1.24–2.25) |
| Timing of discharge | ||
| Weekday | 1.00 | 1.00 |
| Weekend | 1.23 (1.18–1.28) | 1.31 (1.09–1.57) |
| ED services during encounter | ||
| ED-related | 1.33 (1.27–1.39) | NA |
| Not ED-related | 1.00 | NA |
| Hospital Census Region | ||
| Northeast | 1.00 | 1.00 |
| Midwest | 0.78 (0.72–0.85) | 0.85 (0.62–1.16) |
| South | 0.99 (0.93–1.06) | 1.17 (0.89–1.55) |
| West | 0.96 (0.89–1.04) | 0.76 (0.57–1.02) |
| Hospital type | ||
| Rural | 0.72 (0.67–0.78) | 0.99 (0.75–1.32) |
| Urban, nonteaching | 0.88 (0.84–0.93) | 1.07 (0.88–1.30) |
| Urban, teaching | 1.00 | 1.00 |
| Hospital bed size | ||
| Small | 0.85 (0.79–0.92) | NA |
| Medium | 0.92 (0.87–0.97) | NA |
| Large | 1.00 | NA |
Abbreviations: NA, not applicable; PR, prevalence ratio.
Figure 2 shows the average annual direct medical costs of care of inpatient hospitalizations and treat-and-release ED visits among patients 18 to 80 years of age with SCI in the United States, stratified by type of encounter and presence of any GU complications. Overall, annual costs associated with SCI hospitalizations and ED visits were approximately $4.3 billion, with 60.6% and 37.2% coming from inpatient hospitalizations in which the admission source was the ED or another location, respectively, and 2.2% resulting from treat-and-release ED visits. Approximately half of all SCI-related costs nationally were associated with encounters during which a GU complication was present.
Fig 2.
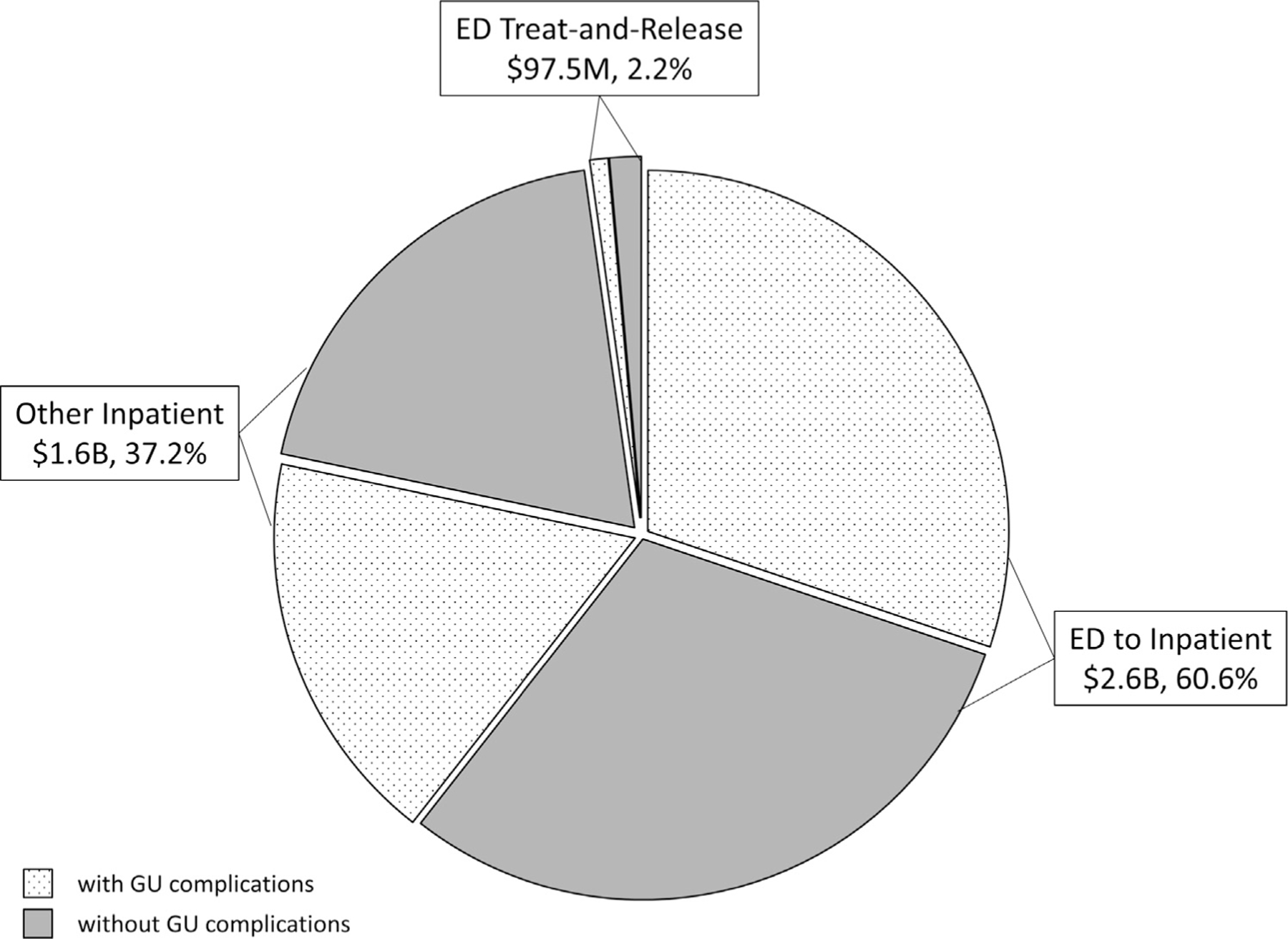
Average annual direct medical costs of care of inpatient hospitalizations and treat-and-release ED visits among patients 18 to 80 years of age with SCI, stratified by type of encounter and presence of any GU complications. NOTE. Costs are expressed as millions (M) or billions (B) of 2015 United States dollars.
Discussion
In the HCUP database we found that infections (including UTIs) and other GU complications are the most common reasons people with SCI present to the ED and are hospitalized. The demographically representative person with SCI for our cohort is a non-Hispanic white man in his 40s to 50s, with Medicare as the primary payer source. GU complications as a primary diagnosis are more common in ED visits than inpatient visits, but as any diagnosis are more common in persons with SCI that are hospitalized as compared to those seen in the ED. As a primary diagnosis, the rates of GU complications among persons with SCI presenting for care are minimally decreasing, but the rates of GU complications as any diagnosis are increasing at a significant rate. Age, neurologic level of injury, and payer source significantly influence mortality during encounters associated with GU complications. ED-to-inpatient encounters among persons with SCI account for most of health care costs, with encounters associated with GU complications accounting for nearly half of the total costs.
Our findings confirm GU infections and other GU complications are the most common reasons for ED and inpatient health care use in persons with SCI, which has been seen in previous studies.3,4 Our demographic distribution varies in some respects from the most recent SCI Model System data; our sample is older, less predominantly male (but still male majority), and paraplegia is more common.1 The ethnic distribution for the inpatient sample is similar to what is seen in the SCI Model Systems Database, however. The demographic findings of Skelton et al16 in a veteran cohort with SCI found a sample older and more predominantly male than the cohort of the current study, but with similar ethnic breakdowns. Therefore, age and sex differ in the broad, national sample of the current study, but the ethnic breakdown is similar in all the studies. GU complication as a primary diagnosis could be a rough estimate of incidence of these conditions, while a GU complication as any diagnosis roughly estimates the prevalence. It makes sense, then, that the prevalence of a person having a GU complication is high, because persons with SCI are living longer. The incidence of GU conditions in SCI is essentially static, however, likely related to the recent focus on minimizing the incidence, diagnosis, and subsequent treatment of GU complications such as catheter-associated UTI.17–19 Interestingly, the decrease in the rates of GU complications listed as the principal diagnosis for inpatient hospitalizations around 2011 to 2012 correlates closely to the implementation of nationwide initiatives to reduce the rates of catheter-associated UTI, and the hospital reimbursement penalties that came along with them.20,21 It is relatively intuitive that age and more rostral neurogenic level of injury would be significantly associated with mortality during a health care encounter for persons with SCI, as well as the fact that ED-to-inpatient encounters are the most costly, given the multiple settings and providers involved in this type of care transition.
Study limitations
These strengths of this study include the large, nationwide sample size and length of study. However, there are inherent drawbacks to using a large administrative database. The accuracy of coding cannot be confirmed via chart review. More detailed info on level of injury was unavailable, thus the neurogenic level of injury groups created were relatively heterogeneous. There was no information about patient signs and symptoms available to confirm the diagnosis of GU complications, nor was there the ability to confirm how the patient managed their bladder (ie, spontaneous void, indwelling catheter, intermittent catheterization, etc) which some studies have shown may influence the rates of GU complications after SCI. Last, the national databases used in this study are cross-sectional and lack patient identifiers that would facilitate investigation of readmissions, repeat ED encounters, or other longer-term outcomes among patients with SCI.
Conclusion
In conclusion, the economic burden of health care encounters associated with GU complications is staggering, indicating that interventions to reduce GU complications remain a high value target to decrease costs and improve quality. Future directions include reducing the burden of GU complications for patients and payers by impalementation of SCI-specific best practices to prevent GU infections and other GU complications, including improving the diagnostic accuracy of UTI (as opposed to chronic asymptomatic colonization).
Acknowledgments
Supported by the Health Resources and Services Administration (grant no. 1 D34HP31024-01-00) (Skelton, Salemi, Akpati, Silva, Dongarwar, Salihu); the Veterans Affairs Health Services Research and Development Service (grant no. CDA2 IK2 HX002484-01) (Skelton); and the Center for Innovations in Quality, Effectiveness and Safety (grant no. CIN 13-413) (Skelton and Trautner). The content is solely the responsibility of the authors and does not necessarily represent the official views of Baylor College of Medicine.
List of abbreviations:
- CCR
cost-to-charge ratio
- CI
confidence interval
- ED
emergency department
- GU
genitourinary
- HCUP
Healthcare Cost and Utilization Project
- NEDS
National Emergency Department Sample
- NIS
National Inpatient Sample
- SCI
spinal cord injury
- UTI
urinary tract infection
- VHA
Veterans Health Administration
Footnotes
Suppliersa
SAS 9.4; SAS Institute, Inc.
Stata/MP 13.1; StataCorp LP.
Joinpoint Regression Program version 4.1.1.3; National Cancer Institute.
Disclosures: none.
Presented as abstracts to the Baylor College of Medicine Center of Excellence in Health Equity, Training, and Research, June 19, 2018, Houston, TX; and to the Veterans Affairs Health Services Research and Development Service, July 12, 2018, Salt Lake City, UT.
References
- 1.National Spinal Cord Injury Statistical Center. Spinal cord injury facts and figures at a glance. Available at: https://www.nscisc.uab.edu/Public/Facts%20and%20Figures%20-%202018.pdf. Accessed September 19, 2018. [PubMed] [Google Scholar]
- 2.McKibben MJ, Seed P, Ross SS, Borawski KM. Urinary tract infection and neurogenic bladder. Urol Clin North Am 2015;42:527–36. [DOI] [PubMed] [Google Scholar]
- 3.Skelton F, Hoffman JM, Reyes M, Burns SP. Examining health-care utilization in the first year following spinal cord injury. J Spinal Cord Med 2015;38:690–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cardenas DD, Hoffman JM, Kirshblum S, McKinley W. Etiology and incidence of rehospitalization after traumatic spinal cord injury: a multicenter analysis. Arch Phys Med Rehabil 2004;85:1757–63. [DOI] [PubMed] [Google Scholar]
- 5.Fitzpatrick MA, Suda KJ, Safdar N, et al. Unique risks and clinical outcomes associated with extended-spectrum b-lactamase enterobacteriaceae in veterans with spinal cord injury or disorder: a case-case-control study. Infect Control Hosp Epidemiol 2016;37:768–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Washington DL, Villa V, Brown A, Damron-Rodriguez J, Harada N. Racial/ethnic variations in veterans’ ambulatory care use. Am J Public Health 2005;95:2231–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Washington DL, Yano EM, Simon B, Sun S. To use or not to use. What influences why women veterans choose VA health care. J Gen Intern Med 2006;21:S11–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Long JA, Polsky D, Metlay JP. Changes in veterans’ use of outpatient care from 1992 to 2000. Am J Public Health 2005;95:2246–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cost Healthcare and Project Utilization (HCUP). Introduction to the HCUP Nationwide Inpatient Sample (NIS) 2011. Available at: https://www.hcup-us.ahrq.gov/db/nation/nis/NIS_Introduction_2011.jsp. Accessed September 19, 2018.
- 10.Houchens R, Elixhauser A. Final report on calculating Nationwide Inpatient Sample (NIS) variances for data years 2011 and earlier. Available at: https://www.hcup-us.ahrq.gov/reports/methods/2003_02.pdf. Accessed September 19, 2018.
- 11.Cost Healthcare and Project Utilization (HCUP). Overview of Nationwide Emergency Department Sample (NEDS). Available at: https://www.hcup-us.ahrq.gov/nedsoverview.jsp. Accessed September 19, 2018. [Google Scholar]
- 12.Salemi JL, Comins MM, Chandler K, et al. A practical approach for calculating reliable cost estimates from observational data: application to cost analyses in maternal and child health. Appl Health Econ Health Policy 2013;11:343–57. [DOI] [PubMed] [Google Scholar]
- 13.United States Department of Labor. Consumer Price Index: all urban consumers—(CPI-U). Available at: https://www.bls.gov/cpi/. Accessed October 17, 2018. [Google Scholar]
- 14.Peterson C, Xu L, Florence C, Parks SE. Annual cost of U.S. hospital visits for pediatric abusive head trauma. Child Maltreat 2015; 20:162–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kim HJ, Fay MP, Feuer EJ, Midthune DN. Permutation tests for joinpoint regression with applications to cancer rates. Stat Med 2000; 19:335–51. [DOI] [PubMed] [Google Scholar]
- 16.Skelton F, Grigoryan L, Holmes SA, Poon IO, Trautner B. Routine urine testing at the spinal cord injury annual evaluation leads to unnecessary antibiotic use: a pilot study and future directions. Arch Phys Med Rehabil 2018;99:219–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Trautner BW, Bhimani RD, Amspoker AB, et al. Development and validation of an algorithm to recalibrate mental models and reduce diagnostic errors associated with catheter-associated bacteriuria. BMC Med Inform Decis Mak 2013;13:48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Trautner BW, Grigoryan L, Petersen NJ, et al. Effectiveness of an antimicrobial stewardship approach for urinary catheter-associated asymptomatic bacteriuria. JAMA Intern Med 2015;175:1120–7. [DOI] [PubMed] [Google Scholar]
- 19.Saint S, Greene MT, Krein SL, et al. A program to prevent catheter-associated urinary tract infection in acute care. N Engl J Med 2016; 374:2111–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Saint S, Meddings JA, Calfee D, Kowalski CP, Krein SL. Catheter-associated urinary tract infection and the Medicare rule changes. Ann Intern Med 2009;150:877–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.National Quality Forum. National Healthcare Safety Network (NHSN) catheter-associated urinary tract infection (CAUTI) outcome measure. Available at: http://www.qualityforum.org/QPS/MeasureDetails.aspx?standardID=1121&print=0&entityTypeID=1. Accessed October 17, 2018.


