Abstract
Background: The outbreak of Corona Virus Disease 2019 (COVID-19) might affect the psychological health of population, especially medical workers. We aimed to investigate the impact of the COVID-19 pandemic on emotional and cognitive responses and behavioral coping among Chinese residents. Methods: An online investigation was run from 5 February to 25 February 2020, which recruited a total of 616 Chinese residents. Self-designed questionnaires were used to collect demographic information, epidemic knowledge and prevention of COVID-19 and characteristics of medical workers. The emotional and cognitive responses were assessed via the Symptom Check List-30 (SCL-30) and Yale–Brown Obsessive Compulsive Scale (Y-BOCS). Behavioral coping was assessed via Simplified Coping Style Questionnaire (SCSQ). Results: In total, 131 (21.3%) medical workers and 485 (78.7%) members of the general public completed the structured online survey. The structural equation models showed that emotional response interacted with cognitive response, and both emotional response and cognitive response affected the behavioral coping. Multivariate regression showed that positive coping enhanced emotional and cognitive responses, while negative coping reduced emotional and cognitive responses. The emotional response (depression, anxiety and photic anxiety) scores of the participants were higher than the norm (all p < 0.001); in particular, the panic scores of members of the general public were higher than those of medical workers (p < 0.05), as well as the cognitive response (paranoia and compulsion). Both positive and negative coping scores of the participants were lower than the norm (p < 0.001), and the general public had higher negative coping than medical workers (p < 0.05). Conclusion: During the preliminary stage of COVID-19, our study confirmed the significance of emotional and cognitive responses, which were associated with behavioral coping and significantly influenced the medical workers and the general public’s cognition and level of public health emergency preparedness. These results emphasize the importance of psychological health at times of widespread crisis.
Keywords: Corona Virus Disease 2019, emotion, cognition, behavioral coping
1. Introduction
In December 2019, Corona Virus Disease 2019 (COVID-19) was first reported and became an outbreak in Wuhan, the capital city of Hubei Province, China [1,2]. The disease, which was caused by coronavirus SARS-CoV-2, rapidly spread throughout China and become a global health emergency [3]. On March 11, 2020, the World Health Organization (WHO) declared COVID-19 a pandemic.
The psychological health of people, especially medical workers, has been greatly challenged during the immediate wake of the viral pandemic. People have high levels of stress due to there being no firm estimate of how long the pandemic will last and how long their lives will be disrupted or whether they will be infected [4]. Moreover, the lack of sufficient knowledge about COVID-19, various channels of opaque information, various rumors, fear of infection, and prolonged isolation and confinement, might seriously affect their psychological health. Being isolated, working in high-risk positions, and having contact with infected people are common causes of psychological burden among medical workers [5,6].
According to psychology, public health emergencies are a negative pressure source, with characteristics of suddenness, menace, extensiveness and infectivity, and people’s life and health have been greatly threatened [7,8]. Public health emergencies, such as COVID-19, can cause depression, anxiety, photic anxiety and other psychological responses, and lead to the emergence of stress disorder, post-traumatic stress disorder and other psychological disorders [4,9]. These psychological barriers of negative emotion can occur even in people not at high risk of getting sick, in the face of a virus with which the general public may be unfamiliar [10].
A precondition for carrying out effective emergency intervention is to evaluate and analyze the psychological state of the people affected by the emergency and to understand the characteristics of the emotional and cognitive responses of different groups in time, so as to take efficient and comprehensive actions in a timely fashion to protect the psychological health of people, especially medical workers [9].
Therefore, with reference to the ‘Corona Virus Disease 2019 Guidelines for Public Psychological Self-help and Counseling’ [11] and the ‘Compilation of Psychological Responses Questionnaire to Public Health Emergency’ [12], this study was mainly carried out in terms of three aspects—emotional response, cognitive response, and behavioral coping—with the aim of evaluating the psychological health status and behavioral coping of medical workers and the general public under the COVID-19 pandemic, and exploring the impact of public health emergencies on psychological health, so as to provide a basis from which relevant departments can carry out precise prevention and control strategies for the public. A structural equation model (SEM) was established to verify the hypothetical associations among emotional and cognitive responses and behavioral coping. The hypotheses were that emotional response interacted with cognitive response, and the psychological dimensions of emotional and cognitive responses affected behavioral coping.
2. Materials and Methods
2.1. Participants
This is a cross-sectional study performed via an online investigation run from February 5 to February 25, 2020. We recruited Chinese residents faced with the COVID-19 pandemic, including medical workers and members of the general public, to participate in this investigation. The research project was approved by the human ethics committee of the Mental Health Center of Shantou University in accordance with the Declaration of Helsinki. All participants provided written informed consent and received a small gift as compensation for their involvement.
Data were collected through Wenjuanxing (http://www.wjx.cn, Changsha Ranxing Information Technology Co., LTD, Changsha, China) with an anonymous, self-rated questionnaire that was distributed to network platforms. All participants were informed of the contents of the study and advised of their privacy and confidentiality commitments when volunteering. Each IP address was accessed to respond once. The answering time of each questionnaire was automatically monitored in the network background, and to guarantee the validity and feasibility of the questionnaire, questionnaires answered in less than 100 s were regarded as invalid.
2.2. Questionnaires
The questionnaire includes two parts: basic demographic information and psychological health assessment, including emotional response, cognitive response and behavioral coping.
2.2.1. Demographic Data
Demographic data included basic demographic characteristics, acquisition and cognition of preventive knowledge, factors affecting mood, basic information and pressure source of medical workers.
2.2.2. Psychological Health Assessment
Three scales were used to assess the psychological health status and coping styles of participants. The Symptom Checklist-30 scale (SCL-30) [13] and the Yale–Brown Obsessive Compulsive Scale (Y-BOCS) [14] were used to evaluate the emotional response and cognitive response. The Simplified Coping Style Questionnaire (SCSQ) [15] was used to evaluate behavioral coping.
SCL-90-R [16], which was developed in its initial version by Derogatis LR [17] and will be revised soon, includes a wide range of psychiatric symptomatology. This survey addresses emotional response (depression, anxiety and photic anxiety) and cognitive response (paranoia and compulsion). Depression, anxiety, photic anxiety and paranoia were selected from SCL-90-R to constitute SCL-30. The SCL-30 scale, a 30-item self-reported scale with items rated on a 5-point Likert scale, was used to select the dimensions of evaluating emotion during a public health emergency, including depression, anxiety, photic anxiety, paranoia, with the scores categorized as follows: no (0), mild (1), moderate (2), severe (3), or pretty severe (4).
The Y-BOCS includes two subscales, corresponding to obsessive thinking and compulsive behavior, respectively. The scale covers the core attributes of obsessive symptoms and can comprehensively evaluate the severity of obsessive symptoms. The severity was assessed via symptomatic distress, frequency, conflict, and self-resistance. The subscales were revised by psychologist on the basis of pandemic of COVID-19, with the scores categorized as follows: complete control (0), a majority of control (1), moderate control (2), poor control (3), or lost control (4). A total score of 6–15 indicates mild compulsion, 16–25 indicates moderate compulsion, and more than 25 indicates severe compulsion.
The SCSQ was synthesized by coping styles cognitive theories and combined with the Chinese characteristics. SCSQ included 20 evaluation points, and was used to evaluate population positive coping and negative coping during an emergency, with the scores categorized as follows: not adopt (0), occasionally (1), sometimes (2), usually (3). The positive coping dimension consisted of items 1–12, which mainly reflect the characteristics of positive coping. The negative coping dimension consisted of items 13–20, which mainly reflect the characteristics of negative coping.
2.3. Statistical Analysis
Statistical analyses were performed with IBM SPSS Statistics 26.0 (IBM Corp., Armonk, NY, USA) and GraphPad prism 8 (GraphPad Software Inc., San Diego, CA, USA). Descriptive analyses were used for demographic data. The results were expressed as the percentage value for categorical data and mean ± standard deviation for continuous data. Chi-square tests were used to compare the data for different categorical variables. All tests were two-sided and p < 0.05 was considered statistically significant. Reliability factor analysis was performed using IBM SPSS Statistic 26.0 for the reliability of the scale, and confirmatory factor analysis was performed with Amos22.0 (IBM Corp., Armonk, NY, USA) for the validity of the scale. A structural equation model (SEM) was constructed via Amos22.0 to explore the relationship among emotional response, cognitive response and behavioral coping. Multivariate stepwise regression analyses were performed using stepwise variable selection to further analyze the association among emotional and cognitive responses and behavioral coping.
3. Results
3.1. Demographic Characteristics of the Participants
A total of 616 participants, including 131 (21.3%) medical workers and 485 (78.7%) members of the general public, completed the online survey. Table 1 presents the demographic characteristics of the participants. More females (63.8%) participated in this survey, and 57.8% of the participants were aged from 19 to 35 years. The participants had relatively high educational levels, with more than half of participants (71.6%) having an educational level of undergraduate or higher. The majority of participants (97.1%) did not have a contact history of COVID-19.
Table 1.
Demographic characteristics of the participants.
| Variables | Number (n = 616) | Percentage (%) |
|---|---|---|
| Gender | ||
| Male | 223 | 36.2 |
| Female | 393 | 63.8 |
| Age (years) | ||
| 0–18 | 55 | 8.8 |
| 19–35 | 356 | 57.8 |
| 36–59 | 188 | 30.5 |
| ≥ 60 | 17 | 2.8 |
| Educational level | ||
| Secondary school or less | 57 | 9.2 |
| Junior college | 118 | 19.1 |
| Undergraduate | 280 | 45.5 |
| Postgraduate or more | 161 | 26.1 |
| Occupation | ||
| Health workers | 131 | 21.3 |
| Educational and cultural workers | 59 | 9.6 |
| Students with medical background | 90 | 14.6 |
| Students without medical background | 66 | 10.7 |
| Civil servant/Career preparation | 64 | 10.4 |
| Company employee | 92 | 14.9 |
| Service industry | 17 | 2.8 |
| Self-employment venture | 19 | 3.1 |
| Worker/Farmer | 13 | 2.1 |
| Full-time housewife | 6 | 1.0 |
| Retired | 14 | 2.3 |
| Others | 45 | 7.3 |
| COVID-19 contact history | ||
| No | 598 | 97.1 |
| Contact history of epidemic focus | 4 | 0.6 |
| Suspected or confirmed COVID-19 patients living around | 14 | 2.3 |
3.2. Acquisition and Cognition of Preventive Knowledge of COVID-19
The main methods of acquisition of information among medical workers and the general public were official news and broadcasts, chat software, and timely messages from the APP, with statistical significance between the two groups (p = 0.005). Additionally, awareness of preventive measures was statistically significant (p = 0.029) among the two groups, such as wearing a mask, avoiding gathering together, washing hands, disinfecting furniture, and maintaining healthy habits. Factors affecting mood were mainly limited to going outside, going to work early, and the impact on the original schedule, with statistical significance (p < 0.001) being exhibited between the two groups (Table 2).
Table 2.
Acquisition and awareness of preventive knowledge between medical workers and the general public.
| Variables | Medical Workers (n = 131) |
Public (n = 485) |
p-Value |
|---|---|---|---|
| Main access of information | 0.005 | ||
| Official news and broadcasts | 114 (87.0) | 412(84.9) | |
| Short message service | 58 (44.3) | 252(52.0) | |
| Chat software | 68 (51.9) | 325(67.0) | |
| Timely message from APP | 85 (64.9) | 347(71.5) | |
| Video Clips from APP | 19 (14.5) | 114(23.5) | |
| Internet searching | 59 (45.0) | 217(44.7) | |
| Others | 7 (5.3) | 23(4.7) | |
| Awareness of COVID-19 transmission | 0.35 | ||
| Droplet transmission | 131(100.0) | 482(99.4) | |
| Contact transmission | 123(93.9) | 428(88.2) | |
| Fecal–oral transmission | 99(75.6) | 373(76.9) | |
| Household articles transmission | 85(64.9) | 337(69.5) | |
| Others | 8(6.1) | 35(7.2) | |
| Awareness of preventive measures | 0.029 | ||
| Wear a mask | 129(98.5) | 484(99.8) | |
| Avoid gathering together | 126(96.2) | 481(99.2) | |
| Wash hands and disinfect furniture | 128(97.7) | 477(98.4) | |
| Exercise | 109(83.2) | 427(88.0) | |
| Raise the room temperature | 19(14.5) | 84(17.3) | |
| Healthy living habits | 121(92.4) | 432(89.1) | |
| Vinegar vapors | 8(6.1) | 45(9.3) | |
| Factors affecting mood | <0.001 | ||
| Limited going outside | 55(42.0) | 361(74.4) | |
| Going to work early | 42(32.1) | 59(12.2) | |
| Impact on the original schedule | 60(45.8) | 235(48.5) | |
| Poor preventive awareness of families | 25(19.1) | 110(22.7) | |
| Unable to reunite with families | 43(32.8) | 80(16.5) | |
| Information explosion and rumors | 67(51.1) | 237(48.9) | |
| Suspected cases around residence | 35(26.7) | 97(20.0) | |
| Others | 8(6.1) | 29(6.0) |
3.3. General Characteristics of Medical Workers and Their Pressure Sources
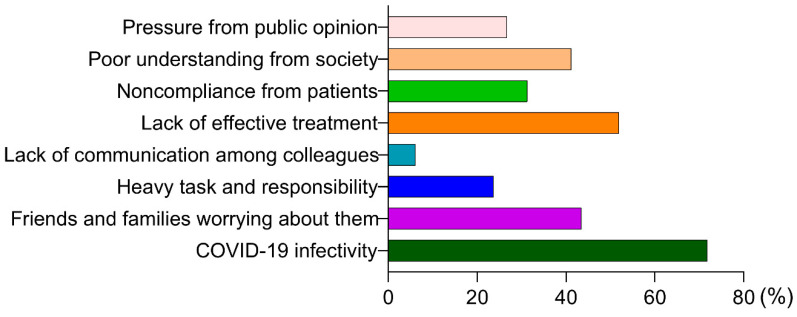
A total of 131 medical workers participated in the survey, including 46 (35.1%) clinical doctors, 20 (15.3%) public health physicians and 30 (22.9%) nurses. 36.6% of the medical workers worked in the designated hospital for COVID-19, and 40.5% worked in the general hospital. A total of 46.6% worked in clinical departments, 8.4% worked in epidemic prevention or infection control and 15.3% worked in the auxiliary department (Table 3). Their top three pressure sources were, in turn, the highly contagious nature of COVID-19, the lack of effective treatment, and their relatives and friends worrying about them (Figure 1).
Table 3.
General characteristics of participating medical workers (n = 131).
| Characteristics | Number | Percentage (%) |
|---|---|---|
| Work units | ||
| Designated hospital for COVID-19 patients | 48 | 36.6 |
| General hospital | 53 | 40.5 |
| Disease prevention and control department | 7 | 5.3 |
| Community health service center | 10 | 7.6 |
| Others | 13 | 10.0 |
| Concrete post | ||
| Clinician | 46 | 35.1 |
| Public health physician | 20 | 15.3 |
| Nurse | 30 | 22.9 |
| Administrative staff | 12 | 9.2 |
| Others | 23 | 17.6 |
| Work department | ||
| Clinical department | 61 | 46.6 |
| Radiology department | 4 | 3.1 |
| Clinical Test Lab | 5 | 3.8 |
| Epidemic prevention or infection control department | 11 | 8.4 |
| Auxiliary department | 20 | 15.3 |
| Others | 30 | 22.9 |
| Seniority | ||
| <5 years | 53 | 40.5 |
| 5–10 years | 34 | 26.0 |
| 10–20 years | 29 | 22.1 |
| 20 years | 15 | 11.5 |
Figure 1.
The pressure sources of medical workers.
3.4. Association among Emotional and Cognitive Responses and Behavioral Coping
3.4.1. Reliability and Validity of Emotional and Cognitive Response Subscales
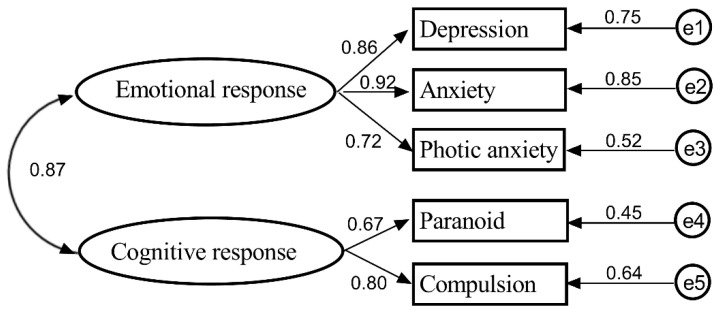
IBM SPSS Statistic 26.0 was used to analyze the reliability of the emotional and cognitive responses subscale. The Cronbach’s α coefficient of the emotional response subscale was 0.813, the Cronbach’s α coefficient of the cognitive response subscale was 0.820, and the Cronbach’s α coefficient of the coping style questionnaire was 0.871. Amos 22.0 was used to analyze the validity α of the emotional response subscale and the cognitive response subscale. Parameter estimation was computed by the maximum likelihood estimate. In addition, standard regression weights of the emotional response subscale and cognitive response subscale are shown in Figure 2. General standard regression weight is required > 0.7. The Cronbach’s α and standard regression weight describe the explanatory power of latent variables for the measured variables.
Figure 2.
Confirmatory factor analysis of emotional and cognitive response scales.
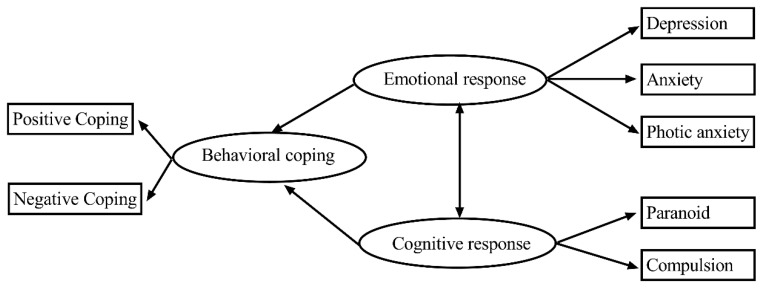
3.4.2. SEM of Emotional and Cognitive Responses and Behavioral Coping
We established an SEM of the associations among emotional response, cognitive response and behavioral coping. Firstly, emotional response as a respective factor for psychological health, including depression, anxiety and photic anxiety, was analyzed in the previous step. Secondly, cognitive response consisted of paranoia and obsessive compulsion. The third area was the simplified coping style of the population regarding whether their coping was positive or negative during the pandemic (Figure 3). The Chi-square test of model fit yielded a value (CMIN) of 116.74, with degrees of freedom = 18, p < 0.001, RMSEA = 0.022, CFI = 0.947, IFI= 0.947 and TLI = 0.907, indicating a good fit. The results showed that emotional response interacted with cognitive response. In addition, the psychological dimensions of emotional response and cognitive response affected behavioral coping. The results are shown in Figure 3 and Table 4.
Figure 3.
SEM of emotional and cognitive responses and behavioral coping.
Table 4.
Direct and indirect effects in SEM.
| Direct or Indirect Effects Pathway | Estimate | Standard Error | C.R. | p-Value |
|---|---|---|---|---|
| Depression←Emotion | 13.723 | 1.410 | 12.033 | <0.001 |
| Anxiety←Emotion | 4.349 | 0.532 | 8.168 | <0.001 |
| Photic anxiety←Emotion | 8.3885 | 0.530 | 15.817 | <0.001 |
| Paranoia←Cognition | 4.799 | 0.286 | 16.787 | <0.001 |
| Compulsion←Cognition | 23.275 | 1.448 | 16.077 | <0.001 |
| Positive←Behavior | 0.499 | 0.043 | 11.721 | <0.001 |
| Negative←Behavior | −0.123 | 0.073 | −1.678 | 0.093 |
| Behavior←Emotion | 35.019 | 2.793 | 12.537 | <0.001 |
| Behavior←Cognition | 2.779 | 0.345 | 8.067 | <0.001 |
3.4.3. Multivariate Stepwise Regression among Emotional and Cognitive Responses and Behavioral Coping
Multivariate stepwise regression was used to analyze the association among emotional and cognitive responses and behavioral coping. The emotional and cognitive response scales’ total scores were regarded as dependent variables, and behavioral coping, including positive coping and negative coping, was regarded as an independent variable. The results showed that both positive coping (β= −0.21) and negative coping (β = 0.53) were significantly associated with emotional and cognitive responses (R2 = 0.177, F = 111.34, p < 0.001), and positive coping enhanced emotional and cognitive responses, while negative coping reduced emotional and cognitive responses (Table 5).
Table 5.
Multivariate stepwise regression among emotional and cognitive responses and behavioral coping.
| Model | B | Beta | t | p-Value | 95%CI |
|---|---|---|---|---|---|
| Constant | 11.68 | — | 7.77 | <0.001 | (8.73, 14.64) |
| Positive | −4.85 | −0.21 | −4.15 | <0.001 | (−7.15, −2.55) |
| Negative | 15.05 | 0.53 | 10.71 | <0.001 | (12.29, 17.81) |
F = 111.34, p < 0.001, R2 = 0.177.
3.4.4. Comparison of the Scales’ Scores between Medical Workers and the General Public
In emotional response, the depression, anxiety and photic anxiety scores among medical workers and the general public were higher than the norm (all p < 0.001), and the photic anxiety score of the general public was higher than that of medical workers (p < 0.05). As to cognitive response, the paranoia score among medical workers and the general public was higher than the norm (p < 0.05), and the compulsion sore of the general public was higher than that of medical workers (p < 0.05) (Table 6). Both positive coping and negative coping scores among medical workers and the general public were lower than the norm (both p < 0.001), while the negative coping sores of the general public were higher than those of medical workers (p < 0.05) (Table 7).
Table 6.
Comparison of emotional and cognitive responses sores between participants and norm.
| Response | Dimensions | Norm | Medical Workers | Public | F | p-Value |
|---|---|---|---|---|---|---|
| Emotion | Depression | 1.50 ± 0.59 | 4.42 ± 6.16 | 4.89 ± 7.20 | 68.22 | <0.001 |
| Anxiety | 1.39 ± 0.43 | 2.85 ± 4.96 | 2.91 ± 5.03 | 27.65 | <0.001 | |
| Photic anxiety | 1.23 ± 0.41 | 2.69 ± 4.01 | 3.35 ± 3.98 * | 78.02 | <0.001 | |
| Cognition | Paranoia | 1.43 ± 0.57 | 1.56 ± 2.48 | 1.79 ± 2.83 | 4.44 | 0.01 |
| Compulsion | 6~10 (Mild) | 6.22 ± 6.25 | 7.36 ± 7.01 * | 54.40 | <0.001 |
F-value is statistic of ANOVA test among the norm, medical workers and general public groups; * Comparison between medical workers and the general public, p < 0.05.
Table 7.
Comparison of behavioral coping sores between participants and norm.
| Behavioral Coping | Norm | Medical Workers | Public | F | p-Value |
|---|---|---|---|---|---|
| Positive | 1.78 ± 0.52 | 1.35 ± 0.91 | 1.48 ± 0.88 | 32.97 | <0.001 |
| Negative | 1.59 ± 0.66 | 0.78 ± 0.73 | 1.06 ± 0.73 * | 118.89 | <0.001 |
F-value is statistic of ANOVA test among the norm, medical workers and general public groups; * Comparison between medical workers and the general public, p < 0.05.
4. Discussion
This is the first investigation of emotional and cognitive responses and behavioral coping in the wake of the coronavirus epidemic in China that explores psychological health in cases of public health emergency. To conduct a comprehensive analysis, we used multiple scales to evaluate the emotional and cognitive responses and behavioral coping of the Chinese population, especially medical workers.
When cities are struck by various disasters, the characteristics of psychological health problems that arise can differ in different periods [18,19]. After an emergency, people suffering from impacts on their psychological health often outnumber people who are physically injured, and psychological health impacts may last longer [20]. The viral pandemic, as a huge negative pressure source, poses great challenges to the psychological health of people, especially medical workers [21]. Although the majority of Chinese residents did not have a contact history of COVID-19 in this survey, complex emotions can occur even in people not at high risk of getting sick, in the face of a virus with which the general public may be unfamiliar [22].
People received information via various channels. Distinguishing real news from rumors undoubtedly increases the psychological burden of the public. Medical workers tend to be able to distinguish real news and rumors because of their expert knowledge. The Preventive Guidelines for People at Different Risks of SARS-CoV-2 Infection [23] were promulgated on time, and the public were generally aware of the transmission of COVID-19, but were still puzzled as to how to prevent it. Thus, acquisition and awareness of preventive knowledge among medical workers and the general public were of statistical significance, probably because medical workers have professional knowledge and occupational skills [24,25].
In terms of the SEM in this study, emotional response interacted with cognitive response, and the psychological dimensions of emotional response and cognitive response affected behavioral coping. The results of multivariate stepwise regression showed that positive coping may enhance psychological health, while negative coping may reduce psychological health. Both positive and negative coping had significant predictive power for emotional and cognitive responses. The study [5] confirmed that people mainly transformed their assessment of stress events and adopted corresponding coping strategies to adjust their emotional and cognitive responses. The relationship between individual coping styles and psychosomatic health has become an important content of psychological research [26,27,28]. The circumstances of pressure sources are evaluated to judge whether it burden or exceed the individual coping skills or not. This study found that mild psychological health disturbances accounted for a large proportion. People with mild psychological disturbances may be more likely to adopt coping styles and learn the necessary skills, so as to adapt in productive ways and cope with different challenges. Previous retrospective studies [6,29,30] have shown that the coping ways and necessary skills were protective for psychological health.
The results showed that the emotional and cognitive response scores increased, while behavioral coping scores decreased in both the general public and among medical workers. In addition, the scores of each psychological dimension and the coping dimension of the general public were higher than those of medical workers, among which the differences in compulsion and negative coping were statistically significant. During the pandemic, both medical workers and the general public’s psychological health were affected, and medical workers have a better emotional and cognitive responses and coping styles to public health emergencies than the general public. Medical workers with professional knowledge in relative exposure patterns and transmission of various infectious diseases could acquire some degree of comfort and control over their situations [24].
People have high levels of stress due to there being no definite estimate of how the long pandemic will last and how long our lives will be disrupted, or whether we will be infected. Additionally, long-term limitations of going out, impact on original schedule, lack of social interaction and mixed information have an influence on people’s psychological health [19,31]. In this study, the causes of psychological burden on medical workers were the infectivity of COVID-19, the lack of effective treatment, the initially insufficient understanding of the virus, and poor support from society and patients. For medical workers, their life status of daily fighting against COVID-19 shows that they have to be able to cope with psychological pressure and are at risk of allostatic load [32]. In pandemic situations, such exposure is known to be mentally injurious [33,34]. Not only does the direct exposure of the work circumstances affect the psychological health of medical workers, but the infection of close relatives generated psychological trauma or fear when the public health emergency hit [5].
Studies [35,36,37] have shown that there is a positive correlation between psychological health and occupational stress. Excessive occupational stress will aggravate anxiety, panic and other adverse psychological emotions of medical workers, as well as somatic symptoms such as insomnia and digestive tract abnormalities, causing negative effects on their work. In the meantime, these impacts reinforce occupational stress in turn. Subsequently, with training on the Novel Coronavirus Infection Pneumonia Diagnosis and Treatment Plan for all medical workers [38], with continuously updated guidelines on how to deal with COVID-19 patients [39], with rest in shifts for medical workers, and with rapid supply of medical protective items, the stress of medical workers has been relieved to some degree and supporting their perseverance. Therefore, relevant departments and institutions should carry out targeted psychological guidance and intervention in the population, especially for medical workers during the pandemic, as well as for reconstruction after the pandemic. Medical workers should be given more social support and understanding, so as to protect the solid “defense line” during infectious disease outbreaks.
Limitations and strengths. The present study has several limitations. First, this study was based on an online survey. The use of clinical interviews is encouraged to draw a more comprehensive assessment of the problem in future studies. Second, this study just reflects people’s psychological health at a particular phase of the COVID-19 pandemic, and a longitudinal approach might help research the development of allostatic overload and changes in post-traumatic psychological health. Despite these limitations, multiple dimensions were considered in this study to analyze people’s psychological characteristics during the pandemic. In addition, an SEM was established to evaluate the associations among the emotional response, cognitive response and behavioral coping of Chinese residents. In the future, somatic symptoms, such as insomnia, nausea, vomiting, anorexia, and frequent urination, could also appear during public health emergencies in addition to emotional responses and cognitive responses. Somatic symptoms can be considered as another subscale to interact with emotional response and cognitive response, and the SEM can thus be further refined to explore the influence on the pandemic of COVID-19. Research in post-traumatic psychological health, dynamic observation and psychological intervention should be performed to obtain more epidemiological data and more specific clues for the intervention of psychological health.
5. Conclusions
During the preliminary stage of COVID-19, our study confirmed the significance of emotional response and cognitive response, which are associated with behavioral coping and significantly influenced the medical workers and the general public’s cognition and level of public health emergency preparedness. It is necessary to recognize psychological health needs as an important component of response to sudden city-scale crisis scenarios.
Acknowledgments
The authors wish to thank all the volunteers who participated in this project.
Author Contributions
Conceptualization, K.W. and Z.C.; methodology, S.Z. and A.H.; software, Z.C.; formal analysis, Z.C.; investigation, S.Z. and X.Z. and A.H. and Z.Q.; resources, Y.H.; data curation, Z.C. and Z.Q.; writing—original draft preparation, Z.C.; writing—review and editing, Y.H. and K.W.; visualization, S.Z.; project administration, Z.Q. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Conflicts of Interest
The authors declare no conflict of interest.
References
- 1.Yu N., Li W., Kang Q., Xiong Z., Wang S., Lin X., Liu Y., Xiao J., Liu H., Deng D., et al. Clinical features and obstetric and neonatal outcomes of pregnant patients with COVID-19 in Wuhan, China: A retrospective, single-centre, descriptive study. Lancet Infect. Dis. 2020;20:559–564. doi: 10.1016/S1473-3099(20)30176-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Du Z., Wang L., Cauchemez S., Xu X., Wang X., Cowling B.J., Meyers L.A. Risk for Transportation of Coronavirus Disease from Wuhan to Other Cities in China. Emerg. Infect. Dis. 2020;26:1049–1052. doi: 10.3201/eid2605.200146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hou C., Chen J., Zhou Y., Hua L., Yuan J., He S., Guo Y., Zhang S., Jia Q., Zhao C., et al. The effectiveness of the quarantine of Wuhan city against the Corona Virus Disease 2019 (COVID-19): Well-mixed SEIR model analysis. J. Med. Virol. 2020;92:841–848. doi: 10.1002/jmv.25827. [DOI] [PubMed] [Google Scholar]
- 4.Lima C.K.T., Carvalho P.M.M., Lima I., Nunes J., Saraiva J.S., de Souza R.I., da Silva C.G.L., Neto M.L.R. The emotional impact of Coronavirus 2019-nCoV (new Coronavirus disease) Psychiatry Res. 2020;287:112915. doi: 10.1016/j.psychres.2020.112915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wu P., Fang Y., Guan Z., Fan B., Kong J., Yao Z., Liu X., Fuller C.J., Susser E., Lu J., et al. The psychological impact of the SARS epidemic on hospital employees in China: Exposure, risk perception, and altruistic acceptance of risk. Can. J. Psychiatry. 2009;54:302–311. doi: 10.1177/070674370905400504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Maunder R.G., Lancee W.J., Balderson K.E., Bennett J.P., Borgundvaag B., Evans S., Fernandes C.M., Goldbloom D.S., Gupta M., Hunter J.J., et al. Long-term psychological and occupational effects of providing hospital healthcare during SARS outbreak. Emerg. Infect. Dis. 2006;12:1924–1932. doi: 10.3201/eid1212.060584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sui H., Song Y., Yang C., Wang C., Ni S. Investigation on the Influence of the Public Health Emergency on Populace Psychology in China. Chin. J. Soc. Med. 2007;34:161–163. [Google Scholar]
- 8.He Y., Liu N. Methodology of emergency medical logistics for public health emergencies. Transport. Res. Part E Log. Transport. Rev. 2015;79:178–200. doi: 10.1016/j.tre.2015.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kang L., Ma S., Chen M., Yang J., Wang Y., Li R., Yao L., Bai H., Cai Z., Xiang Yang B., et al. Impact on mental health and perceptions of psychological care among medical and nursing staff in Wuhan during the 2019 novel coronavirus disease outbreak: A cross-sectional study. Brain Behav. Immun. 2020 doi: 10.1016/j.bbi.2020.03.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Montemurro N. The emotional impact of COVID-19: From medical staff to common people. Brain Behav. Immun. 2020 doi: 10.1016/j.bbi.2020.03.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ma X., Xie B., Wang G., Zhao X. Corona Virus Disease 2019 Guidelines for Public Psychological Self-help and Counseling. [(accessed on 31 January 2020)];2020 Available online: https://mp.weixin.qq.com/s/yPuw8qelwN-iH4CqTRxcVg.
- 12.Tang Z., Wei B., Su L., Yu M., Wang X., Tan Y. Development of Psychological Reaction Scales to Public Health Emergencies. Mod. Prev. Med. 2007;21:4050–4053. [Google Scholar]
- 13.Martínez-Pampliega A., Herrero-Fernández D., Martín S., Cormenzana S. Psychometrics of the SCL-90-R and Development and Testing of Brief Versions SCL-45 and SCL-9 in Infertile Couples. Nurs. Res. 2019;68:e1–e10. doi: 10.1097/NNR.0000000000000363. [DOI] [PubMed] [Google Scholar]
- 14.Kim S.W., Dysken M.W., Kuskowski M. The Yale-Brown Obsessive-Compulsive Scale: A reliability and validity study. Psychiatry Res. 1990;34:99–106. doi: 10.1016/0165-1781(90)90061-9. [DOI] [PubMed] [Google Scholar]
- 15.Jie Y. Reliability and validity preliminary study of Simplified Coping Style Questionnaire. Chin. J. Clin. Psychol. 1998;6:53–54. [Google Scholar]
- 16.Wang Z.Y. Symptom Check List (SCL-90) Shanghai Jingshen Yixue. 1984;2:68–70. [Google Scholar]
- 17.Derogatis L.R. SCL-90 R-(Revised) Version Manual-I. [(accessed on 3 February 2020)]; Available online: https://www.pearsonassessments.com/store/usassessments/en/Store/Professional-Assessments/Personality-%26-Biopsychosocial/Symptom-Checklist-90-Revised/p/100000645.html.
- 18.Shioyama A., Uemoto M., Shinfuku N., Ide H., Seki W., Mori S., Inoue S., Natsuno R., Asakawa K., Osabe H. The mental health of school children after the Great Hanshin-Awaji Earthquake: II. Longitudinal analysis. Seishin Shinkeigaku Zasshi. 2000;102:481–497. [PubMed] [Google Scholar]
- 19.Ohto H., Yasumura S., Maeda M., Kainuma H., Fujimori K., Nollet K.E. From Devastation to Recovery and Revival in the Aftermath of Fukushima’s Nuclear Power Plants Accident. Asia Pac. J. Public Health. 2017;29:10S–17S. doi: 10.1177/1010539516675700. [DOI] [PubMed] [Google Scholar]
- 20.Allsopp K., Brewin C.R., Barrett A., Williams R., Hind D., Chitsabesan P., French P. Responding to mental health needs after terror attacks. BMJ. 2019;366:l4828. doi: 10.1136/bmj.l4828. [DOI] [PubMed] [Google Scholar]
- 21.Huang Y., He M., Li A., Lin Y., Zhang X., Wu K. Personality, Behavior Characteristics, and Life Quality Impact of Children with Dyslexia. Int. J. Environ. Res. Public Health. 2020;17:1415. doi: 10.3390/ijerph17041415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Zhang Y., Ma Z.F. Impact of the COVID-19 Pandemic on Mental Health and Quality of Life among Local Residents in Liaoning Province, China: A Cross-Sectional Study. Int. J. Environ. Res. Public Health. 2020;17:2381. doi: 10.3390/ijerph17072381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.National Health Commission of the People’s Republic of China Preventive Guidelines for People at Different Risks of SARS-CoV-2 Infection. [(accessed on 31 January 2020)]; Available online: http://www.nhc.gov.cn/jkj/s7916/202001/a3a261dabfcf4c3fa365d4eb07ddab34.shtml. (In Chinese)
- 24.Chowell G., Abdirizak F., Lee S., Lee J., Jung E., Nishiura H., Viboud C. Transmission characteristics of MERS and SARS in the healthcare setting: A comparative study. BMC Med. 2015;13:210. doi: 10.1186/s12916-015-0450-0. (In Chinese) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hawryluck L., Gold W.L., Robinson S., Pogorski S., Galea S., Styra R. SARS control and psychological effects of quarantine, Toronto, Canada. Emerg. Infect. Dis. 2004;10:1206–1212. doi: 10.3201/eid1007.030703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Davey G.C., Tallis F., Hodgson S. The relationship between information-seeking and information-avoiding coping styles and the reporting of psychological and physical symptoms. J. Psychosom. Res. 1993;37:333–344. doi: 10.1016/0022-3999(93)90135-3. [DOI] [PubMed] [Google Scholar]
- 27.Ruchkin V.V., Eisemann M., Hagglof B. Coping styles and psychosomatic problems: Are they related? Psychopathology. 2000;33:235–239. doi: 10.1159/000029151. [DOI] [PubMed] [Google Scholar]
- 28.Lau Y., Wang Y., Kwong D.H., Wang Y. Testing direct and moderating effects of coping styles on the relationship between perceived stress and antenatal anxiety symptoms. J. Psychosom. Obstet. Gynaecol. 2015;36:29–35. doi: 10.3109/0167482X.2014.992410. [DOI] [PubMed] [Google Scholar]
- 29.Takamoto M., Aikawa A. The effect of coping and appraisal for coping on mental health and later coping. Shinrigaku kenkyu Jpn. J. Psychol. 2013;83:566–575. doi: 10.4992/jjpsy.83.566. [DOI] [PubMed] [Google Scholar]
- 30.Sharma M., Fine S.L., Brennan R.T., Betancourt T.S. Coping and mental health outcomes among Sierra Leonean war-affected youth: Results from a longitudinal study. Dev. Psychopathol. 2017;29:11–23. doi: 10.1017/S0954579416001073. [DOI] [PubMed] [Google Scholar]
- 31.Triguero-Mas M., Donaire-Gonzalez D., Seto E., Valentin A., Martinez D., Smith G., Hurst G., Carrasco-Turigas G., Masterson D., van den Berg M., et al. Natural outdoor environments and mental health: Stress as a possible mechanism. Environ. Res. 2017;159:629–638. doi: 10.1016/j.envres.2017.08.048. [DOI] [PubMed] [Google Scholar]
- 32.Fava G.A., McEwen B.S., Guidi J., Gostoli S., Offidani E., Sonino N. Clinical characterization of allostatic overload. Psychoneuroendocrinology. 2019;108:94–101. doi: 10.1016/j.psyneuen.2019.05.028. [DOI] [PubMed] [Google Scholar]
- 33.McAlonan G.M., Lee A.M., Cheung V., Cheung C., Tsang K.W., Sham P.C., Chua S.E., Wong J.G. Immediate and sustained psychological impact of an emerging infectious disease outbreak on health care workers. Can. J. Psychiatry. 2007;52:241–247. doi: 10.1177/070674370705200406. [DOI] [PubMed] [Google Scholar]
- 34.Nickell L.A., Crighton E.J., Tracy C.S., Al-Enazy H., Bolaji Y., Hanjrah S., Hussain A., Makhlouf S., Upshur R.E. Psychosocial effects of SARS on hospital staff: Survey of a large tertiary care institution. CMAJ. 2004;170:793–798. doi: 10.1503/cmaj.1031077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Sawhney G., Jennings K.S., Britt T.W., Sliter M.T. Occupational stress and mental health symptoms: Examining the moderating effect of work recovery strategies in firefighters. J. Occup. Health Psychol. 2018;23:443–456. doi: 10.1037/ocp0000091. [DOI] [PubMed] [Google Scholar]
- 36.Labrague L.J., McEnroe-Petitte D.M., Leocadio M.C., Van Bogaert P., Cummings G.G. Stress and ways of coping among nurse managers: An integrative review. J. Clin. Nurs. 2018;27:1346–1359. doi: 10.1111/jocn.14165. [DOI] [PubMed] [Google Scholar]
- 37.Song K.W., Choi W.S., Jee H.J., Yuh C.S., Kim Y.K., Kim L., Lee H.J., Cho C.H. Correlation of occupational stress with depression, anxiety, and sleep in Korean dentists: Cross-sectional study. BMC Psychiatry. 2017;17:398. doi: 10.1186/s12888-017-1568-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.SINAnews (Internet) Beijing: In January, Hubei Had More than 3000 Medical Infections, and the Wuhan Health and Medical Committee Reported “None” for Half a Month. [(accessed on 6 March 2020)]; Available online: https://news.sina.com.cn/o/2020-03-06/dociimxyqvz8395569.shtml.
- 39.National Health Commission An Announcement of Issuing the Novel Coronavirus Infection Pneumonia Diagnosis and Treatment Plan (Trial Version 7) [(accessed on 3 March 2020)]; Available online: http://www.nhc.gov.cn/yzygj/s7653p/202003/46c9294a7dfe4cef80dc7f5912eb1989.shtml.