Abstract
Objective
Guidelines do not specify how cutoffs for high disease activity differ between the Disease Activity Score 28‐joint count indices DAS28–erythrocyte sedimentation rate (ESR) and DAS28–C‐reactive protein (CRP). Studies that compare DAS28‐CRP and DAS28‐ESR depend on data from clinical trials, registries, or practices with multiple providers. Existing studies use data from patients who received immunosuppressive therapy. This study compared the DAS28‐ESR and DAS28‐CRP values from immunosuppressive treatment–naïve patients in a single physician practice.
Methods
A retrospective electronic medical chart review was conducted for new diagnoses of rheumatoid arthritis (RA; International Classification of Diseases [ICD]‐9 714), based on the American College of Rheumatology/European League against Rheumatology 2010 RA classification criteria. The number of patients with high disease activity (>5.1) was compared using ESR and CRP data to calculate the proportion of discordance. A receiver operator curve and Youden index was used to calculate the DAS28‐CRP high disease activity cutoff estimation that corresponds with DAS28‐ESR of more than 5.1.
Results
There were 171 patients included in this study. The baseline mean DAS28‐ESR was higher than the baseline mean DAS‐28 CRP: 5.1 ± 1.2 versus 4.1 ± 1.0 (P < 0.001); 48.5% of patients met criteria for high disease activity (score >5.1) compared with only 14.6% when measured by DAS28‐CRP. Discordance was 33.9%. κ coefficient was only .307. Receiver operator curve and Youden index analysis suggested that the cutoff point for high disease activity of DAS28‐CRP greater than 4.1, which corresponds to DAS28‐ESR greater than 5.1. Similarly, DAS28‐ESR posttreatment scores were significantly higher than DAS28‐CRP. When measured by DAS28‐ESR, patients in remission had higher scores as measured by DAS28‐ESR (1.81) than DAS28‐CRP (1.45).
Conclusion
There is a difference between DAS28‐ESR and DAS28‐CRP, even when calculated for immunosuppressive treatment–naïve patients. DAS28‐CRP is significantly lower than DAS28‐ESR.
INTRODUCTION
Disease activity of rheumatoid arthritis (RA) is usually assessed by using Disease Activity Score 28‐joint count (DAS28) (1, 2). DAS28 scores range from 0 to 9.4 and are calculated using tender joints, swollen joints, general health, and a laboratory measure of acute inflammation (3). DAS28 can be characterized using erythrocyte sedimentation rate (ESR) or C‐reactive protein (CRP). Despite the routine use of disease activity scores in guiding treatment, existing guidelines do not specify how cutoffs for high disease activity differ between DAS28‐ESR and DAS28‐CRP (4). Thus, stakeholders, such as individual providers, health systems, and payers, often use these values synonymously when determining the need for therapeutic regimens.
Previous studies have shown that DAS28‐CRP values are lower than the corresponding DAS28‐ESR values (5, 6, 7, 8, 9, 10, 11, 12, 13). Despite these reports, it is still common for practitioners and payors to assess the cutoff points as being similar. Many pharmaceutical companies use DAS28‐CRP in their clinical trials without altering cutoffs for high disease activity, moderate disease activity, low disease activity (LDA), and remission. Most existing studies that compare DAS28‐CRP and DAS28‐ESR are drawn largely on data from clinical trials, registries, or practices with multiple providers as evaluators. Because of the variation between independent providers and separate institutions, existing data must be validated by and compared with data from a single provider. Furthermore, many patients in these studies have been treated with immunosuppressive treatment. Immunosuppressive medications have the ability to alter ESR or CRP disproportionately or to reduce one of these values without controlling disease activity. For example, interleukin (IL)‐6 inhibitors can reduce CRP dramatically without controlling disease in all patients (14). Thus, existing data must be validated by and compared with data that control for 1) interobserver discrepancy and 2) confounding effects of concomitant immunosuppressive medications. The purpose of our study was to compare the DAS28‐ESR and DAS28‐CRP values from immunosuppressive treatment–naïve patients in a single‐physician practice at a single institution.
METHODS
We conducted a retrospective electronic chart review for new diagnoses of RA (ICD‐9 714) from January 1, 2005, to September 1, 2018, at our institution. Patients were included if they were 1) given a new diagnosis of RA or 2) were treated with 10 mg or less of prednisone after diagnosis. Patients were excluded if 1) they had previously or were receiving treatment with a disease‐modifying antirheumatic drug or steroid upon study enrollment, 2) they received a disease‐modifying antirheumatic drug or more than 10 mg of prednisone after diagnosis, or 3) if their electronic medical record did not contain the data necessary to calculate both ESR and CRP disease activity scores. Disease severity was calculated using the DAS28‐ESR and DAS28‐CRP at baseline (immunosuppressive naïve) and again following treatment with 10 mg or less of prednisone.
SPSS 25.0 for Windows (IBM, Armonk, NY) was used for analysis. Descriptive statistics for baseline DAS28‐ESR and DAS28‐CRP were compared using a paired t test, with P < .05 considered significant.
DAS28‐CRP and DAS28‐ESR were compared according to the cutoff value for baseline high disease activity (>5.1) using sensitivity, specificity, κ coefficients, and proportion of discordance. A receiver operator characteristic (ROC) curve and Youden index were used to calculate the DAS28‐CRP high disease activity optimal cut‐point value corresponding to DAS28‐ESR of more than 5.1. DAS28‐ESR and DAS28‐CRP posttreatment scores were analyzed using paired t test. Agreement between DAS28‐ESR and DAS28‐CRP posttreatment scores were compared using Bland‐Altman statistics and plots. This study has been approved by the institutional review boards of Trinity Health of Minot, ND and the University of North Dakota.
RESULTS
A total of 171 patients newly diagnosed with RA were included in the study from the 1386 screened patients. All patients in this study were immunosuppressive treatment–naïve upon study enrollment (n = 171). All posttreatment values were recorded from enrolled patients who were treated with 10 mg or less of prednisone. Overall, 91.8% of patients were white, 65.5% female, and mean age was 55.1 ± 15.9 years. The seropositive rate was 66.1 percent. At baseline, the mean DAS28‐ESR was higher than the mean DAS‐28 CRP, 5.1 ± 1.2 versus 4.1 ± 1.0 (P < .001) (Table 1).
Table 1.
Baseline characteristics of patients
| Demographics | |
|---|---|
| Number of patients, n | 171 |
| Age, mean ± SD days | 55.1 ± 15.9 |
| Gender, female, n (%) | 112 (65.5) |
| Race [n (%)] | |
| White | 157 (91.8) |
| Other | 14 (8.2) |
| RF positivity (n [%]) | 91 (53.2) |
| Anti‐CCP positivity (n [%]) | 84 (49.1) |
| Seropositive patients (both RF and anti‐CPP positivity) (n [%]) | 113 (66.1) |
| DAS28‐ESR | 5.1 ± 1.2 |
| DAS28‐CRP | 4.1 ± 1.0 |
Abbreviation: CCP, cyclic citrullinated peptide; CRP, C‐reactive protein; DAS, Disease Activity Score; ESR, erythrocyte sedimentation rate; RF, rheumatoid factor.
Agreement comparison of DAS28‐ESR and DAS28‐CRP is summarized in Table 2. At baseline, more patients met high disease activity criteria (>5.1) for DAS28‐ESR than for DAS28‐CRP: 48.5% versus 14.6% (Table 3). Discordance between these two parameters was 33.9%, which corresponds to minimal or fair level of agreement between DAS28‐CRP more than 5.1 and DAS28‐ESR more than 5.1 (κ coefficient = .307), with high sensitivity and low specificity. ROC curve and Youden index analysis showed that the cutoff point estimation of high disease activity using DAS28‐ESR greater than 5.1 corresponded to a DAS28‐CRP score of 4.06 (area under the ROC curve = 0.93, P = .000) (Figure 1).
Table 2.
Agreement comparison of DAS28‐CRP > 5.1 and DAS28‐ESR > 5.1 at baseline
| DAS28‐CRP > 5.1 | DAS28‐ESR > 5.1 | Proportion of Discordance | Sensitivity (%) | Specificity (%) | K Coefficient | |
|---|---|---|---|---|---|---|
| All 171 | 25/171 (14.6) | 83/171 (48.5) | 58/171 (33.9) | 100 | 60.3 | 0.31 |
Sensitivity, specificity, and κ based on DAS28‐CRP score greater than 5.1 as the standard.
Abbreviation: DAS28‐CRP, Disease Activity Score in 28 joints calculated with C‐reactive protein; DAS28‐ESR, Disease Activity Score in 28 joints calculated with erythrocyte sedimentation rate.
Table 3.
Means and mean difference between posttreatment DAS28‐CRP and DAS28‐ESR by gender, age, and severity
| Characteristic | DAS28‐ESR | DAS28‐CRP |
Mean Difference (95% CI; n) |
P value |
|---|---|---|---|---|
| Overall | 2.70 | 2.04 | 0.66 (0.56‐0.76; 151) | .000 |
| Gender | ||||
| Male | 2.67 | 2.17 | 0.51 (0.35‐0.68; 51) | .000 |
| Female | 2.71 | 1.98 | 0.73 (0.60‐0.86; 100) | .000 |
| Age | ||||
| ≤50 years | 2.78 | 2.11 | 0.67 (0.50‐0.83; 58) | .000 |
| >50 years | 2.65 | 2.00 | 0.65 (0.52‐0.78; 93) | .000 |
| Severity | ||||
| Remission (<2.6) | 1.81 | 1.45 | 0.36 (0.22‐0.50; 79) | .000 |
| LDA (2.6 to ≤3.2) | 2.80 | 1.79 | 1.01 (0.85‐1.18; 25) | .000 a |
| MDA (3.2 to ≤5.1) | 3.91 | 2.96 | 0.95 (0.95‐0.80; 41) | .000 |
| HDA (>5.1) | 5.73 | 4.66 | 1.07 (0.96‐1.17; 6) | .000 a |
Abbreviations: CI, confidence interval; CRP, C‐reactive protein; DAS28, Disease Activity Scores 28‐joint count; ESR, erythrocyte sedimentation rate; HDA, high disease activity; LDA, low disease activity; MDA, medium disease activity; n, number of paired scores.
Low samples.
Figure 1.
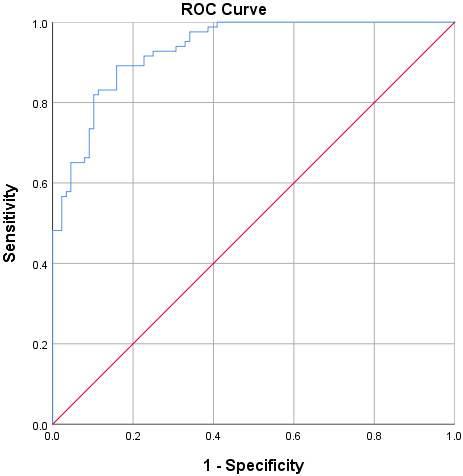
Receiver Operating Characteristic Curve for Discriminating between the American College of Rheumatology DAS28‐ESR High Disease Activity Cut‐off (>5.1) and DAS28‐CRP at Baseline among RA Patients at a Midwestern Hospital.
Paired posttreatment DAS28‐ESR and DASCRP‐28 scores were available for 151 patients. These values were derived from patients who had been treated with 10 mg or less of prednisone after study enrollment. The DAS28‐CRP was, on average, 0.66 points higher than the corresponding DAS28‐ESR for the whole cohort (P = 0.000, Table 3). Bland‐Altman plot illustrates how DAS28‐ESR scores are higher at remission through high disease activity levels (Figure 2). When stratifying by gender, age, and severity, DAS28‐CRP was significantly lower in all subcategories than the corresponding DAS28‐ESR score. The mean DAS28‐CRP score in patients in remission was significantly lower—by 0.36 points—than the corresponding DAS28‐ESR score.
Figure 2.
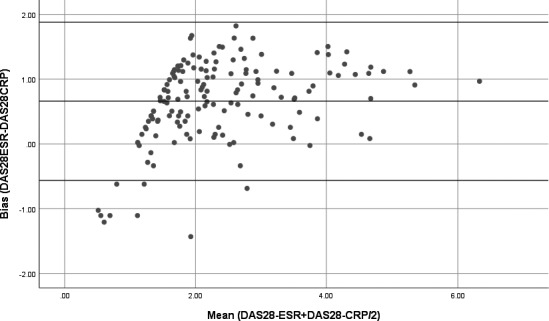
Bland–Altman plot analysis of the post‐treatment disease activity using DAS28‐ESR and DAS28‐CRP in RA patients. The middle line indicates the bias (mean difference), the upper and lower lines represent the limits of agreement.
DISCUSSION
Outcomes in RA are closely related to disease activity (1). Thus, disease activity scores are used routinely in guiding individual treatment and in assessing the efficacy of therapies in clinical trials. Multiple studies in the last decade have demonstrated that DAS28‐CRP is lower than DAS28‐ESR (5, 6, 7, 8, 9, 10, 11, 12, 13). For example, one study found that a high disease activity cutoff for DAS28‐ESR of 5.1 correlated with a DAS28‐CRP score of 4.6 (5). However, existing guidelines do not specify how cutoffs for high disease activity differ between DAS28‐ESR and DAS28‐CRP (15). Variables such as age and gender are known to impact the discrepancy between ESR and CRP calculations (16, 17). Despite the growing body of literature on the discrepancy between these DAS28‐ESR and DAS28‐CRP, many stakeholders continue to use ESR and CRP values synonymously when determining the need and viability of therapeutic regimens.
Our study has confirmed what has been found in different populations in a single‐physician practice (5, 6, 7, 8, 9, 10, 11, 12, 13). We found that the DAS28‐CRP values are lower than the corresponding DAS28‐ESR values both at baseline high disease activity and posttreatment. The mean DAS28‐CRP score was 0.93 points less than the mean DAS28‐ESR score at baseline high disease activity. Although 48.5 percent of patients in this study (at baseline) met criteria for severe disease activity (>5.1) according to DAS28‐ESR, only 14.6 percent met severe disease activity according to DAS28‐CRP. The κ coefficient revealed only minimal agreement between severe disease activity as determined by DAS28‐ESR and DAS28‐CRP, rather than the good or moderate agreement found in previous studies (5, 7, 8). The cutoff point estimation of high disease activity using a DAS28‐ESR score greater than 5.1 corresponds to a DAS28‐CRP score of 4.06. The change in direction of bias on the Bland‐Altman plot below 2.00 is likely due to the lower limits of normal for ESR and CRP. Underestimating high disease activity in a treat‐to‐target paradigm of care could lead to less aggressive treatment in patients who would warrant aggressive management of their disease.
We found similar discrepancies in posttreatment DAS28‐ESR and DAS28‐CRP scores among those in remission, low disease activity, and moderate disease activity. For patients who achieved remission (<2.6) after treatment, the mean DAS28‐ESR was 1.81 and DAS28‐CRP was 1.45 (P < .001). Overestimating LDA and remission is particularly problematic if the practitioner is using DAS28 in a treat‐to‐target approach. If DAS28‐CRP levels overestimate remission and LDA, it is possible that patients who still have active disease are not being treated accordingly.
Our results demonstrate a large discrepancy between these two scores that are frequently used interchangeably. Although existing studies have focused on proposing different cutoffs, future research should focus on making adjustments to the formulas themselves. Adjustments to DAS28‐ESR and DAS28‐CRP formulas could include reweighting variables or performing adjustments to CRP values to help balance the two formulas.
This study has two unique contributions to the literature on this subject. First, this was a single‐center study with one observer for consistency. Second, values were calculated in treatment‐naïve patients without the confounding effects of concomitant medications (such as an IL‐6 inhibitor, which reduces CRP dramatically but does not control disease activity in all patients) (14). Our approach reduces the potential for error, and strongly suggests that DAS28‐CRP underestimates disease severity when compared with DAS28‐ESR. Future guidelines should carefully differentiate between DAS28‐ESR and DAS28‐CRP indices.
The patients included in this study were racially homogenous (91.8% white) and may not accurately represent the broader population of patients with RA. The single‐site nature of this study may limit the generalizability of our findings. This study did not supply data on the body mass index or comorbidities of the patients in the study. Some comorbidities, such as obesity or renal disease, may impact the difference between DAS28‐ESR and DAS28‐CRP. One unresolved dilemma for the treat‐to‐target approach becomes the following: are DAS28 cutoff points specified for ESR or CRP calculations? With current data, it is impossible to know which measure is “correct.” If the DAS28 cutoff points are best used for DAS28‐ESR, then DAS28‐CRP greatly overestimates LDA and remission. If DAS28 cutoff points are best used with DAS28‐CRP, then DAS28‐ESR greatly underestimates LDA and remission. Future studies should investigate whether CRP or ESR data better correlate to clinical severity.
In conclusion, DAS28‐ESR and DAS28‐CRP cutoffs for high disease activity, LDA, and remission are not the same. DAS28‐CRP is significantly lower than DAS28‐ESR. At the high end of disease activity, DAS28‐CRP may underestimate disease activity. At the low end of disease activity, DAS28‐CRP may overestimate the number of patients in LDA or remission.
AUTHOR CONTRIBUTIONS
All authors were involved in the preparation or critical revision of this article. All authors approved the final version to be published.
Study conception and design
Diri, Greenmyer, Stacy, Beal, Sahmoun.
Acquisition of data
Greenmyer, Stacy.
Analysis and interpretation of data
Diri, Greenmyer, Beal, Sahmoun.
No potential conflicts of interest relevant to this article were reported.
REFERENCES
- 1. Listing J, Kekow J, Manger B, Burmester GR, Pattloch D, Zink A, et al. Mortality in rheumatoid arthritis: the impact of disease activity, treatment with glucocorticoids, TNAα inhibitors and rituximab. Ann Rheumatic Dis 2015;74:415–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Prevoo ML, van’t Hof MA, Kuper HH, van Leeuwen MA, van de Putte LB, van Riel PL. Modified disease activity scores that include twenty‐eight‐joint counts. Development and validation in a prospective longitudinal study of patients with rheumatoid arthritis. Arthritis Rheum 1995;38:44–8. [DOI] [PubMed] [Google Scholar]
- 3. Fransen J, van Riel PL. The Disease Activity Score and the EULAR response criteria. Clin Exp Rheumatol 2005;23 Suppl 39:93–9. [PubMed] [Google Scholar]
- 4. Singh JA, Saag KG, Bridges SL Jr, Akl EA, Bannuru RR, Sullivan MC, et al. 2015 American College of Rheumatology Guideline for the Treatment of Rheumatoid Arthritis. Arthritis Care Res (Hoboken) 2015;68:1–26. [DOI] [PubMed] [Google Scholar]
- 5. Fleischmann RM, van der Heijde D, Gardiner PV, Szumski A, Marshall L, Bananis E. DAS28‐CRP and DAS28‐ESR cut offs for high disease activity in rheumatoid arthritis are not interchangeable. RMD Open 2017;3:e000382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Matsui T, Kuga Y, Kaneko A, Nishino J, Eto Y, Chiba N, et al. Disease Activity Score 28 (DAS 28) using C‐reactive protein underestimates disease activity and overestimates EULAR response criteria compared with DAS28 using erythrocyte sedimentation rate in a large observational cohort of rheumatoid arthritis patients in Japan. Ann Rheum Dis 2007;66:1221–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Son KM, Kim SY, Lee SH, Yang CM, Seo YI, Kim HA. Comparison of the disease activity score using the erythrocyte sedimentation rate and C‐reactive protein levels in Koreans with rheumatoid arthritis. Int J Rheum Dis 2016;19:1278–83. [DOI] [PubMed] [Google Scholar]
- 8. Sengul I, Akcay‐Yalbuzdag S, Ince B, Goksel‐Karatepe A, Kaya T. Comparison of the Das28‐CRP and DAS28‐ESR in patients with rheumatoid arthritis. Int J Rheum Dis 2015;18:640–5. [DOI] [PubMed] [Google Scholar]
- 9. Inoue E, Ymanaka H, Hara M, Tomatsu T, Kamatani N. Comparison of Disease Activity Score (DAS)28‐erythrocyte sedimentation rate and DAS28‐C‐reactive protein threshold values. Ann Rheum Dis 2007;66:407–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Tamhane A, Redden DT, McGwin G Jr, Brown EE, Westfall AO, Reynolds RJ IV, et al. Comparison of the Disease Activity Score using erythrocyte sedimentation rate and C‐reactive protein in African‐Americans with rheumatoid arthritis. J Rheumatol 2013;40:1812–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Das Chagas Medeiros MM, de Oliveria B, de Cerqueira J, de Souza Quixada R, de Oliveira I. Correlation of rheumatoid arthritis indexes (Disease Activity Score 28 measured with ESR and CRP, Simplified Disease Activity Index and Clinical Disease Activity Index) and agreement of disease activity states with various cut‐off points in a northeastern Brazilian population. Rev Bras. Rheumatol 2015;55:477–84. [DOI] [PubMed] [Google Scholar]
- 12. Castrejón I, Ortiz AM, García‐Vicuña R, Lopez‐Bote JP, Humbría A, Caromona L, et al. Are the C‐reactive protein values and erythrocyte sedimentation rate equivalent when estimating the 28‐joint disease activity score in rheumatoid arthritis? [Comparative study]. Clin Exp Rheumatol 2008;26:769–75. [PubMed] [Google Scholar]
- 13. Park SY, Lee H, Cho SK, Choi CB, Sung YK, Bae SC. Evaluation of disease activity indices in Korean patients with rheumatoid arthritis. Rheumatol Int 2011;32:545–9. [DOI] [PubMed] [Google Scholar]
- 14. Ogata A, Kato Y, Higa S, Yoshizaki K. IL‐6 inhibitor for the treatment of rheumatoid arthritis: a comprehensive review. Mod Rheumatol 2019;29:258–67. [DOI] [PubMed] [Google Scholar]
- 15. Sheehy C, Evans V, Hasthorpe H, Mukhtyar C. Revising DAS28 scores for remission in rheumatoid arthritis. Clin Rheumatol 2014;33:269–72. [DOI] [PubMed] [Google Scholar]
- 16. Hensor EM, Emery P, Bingham SJ, Conaghan PG; YEAR Consortium . Discrepancies in categorizing rheumatoid arthritis patients by DAS‐28(ESR) and DAS‐28(CRP): can they be reduced? [Research support]. Rheumatology (Oxford) 2010;49:1521–9. [DOI] [PubMed] [Google Scholar]
- 17. Hamann PD, Shaddick G, Hyrich K, Green A, McHugh N, Pauling JD. BSRBR‐RA Contributors Group. Gender stratified adjustment of the DAS28‐CRP improves inter‐score agreement with the DAS28‐ESR in rheumatoid arthritis. Rheumatology (Oxford) 2019;58:831–5. [DOI] [PMC free article] [PubMed] [Google Scholar]


