Abstract
Chronic inflammation caused by infections has been suggested to be one of the most important cause of cancers. It has recently been shown that there is correlation between intestinal bacteria and cancer development including metastasis. As over 700 bacterial species exist in an oral cavity, it has been concerning that bacterial infection may cause oral cancer. However, the role of bacteria regarding tumorigenesis of oral cancer remains unclear. Several papers have shown that Fusobacterium species deriving the oral cavities, especially, play a crucial role for the development of colorectal and esophageal cancer. F. nucleatum is a well-known oral bacterium involved in formation of typical dental plaque on human teeth and causing periodontal diseases. The greatest characteristic of F. nucleatum is its ability to adhere to various bacteria and host cells. Interestingly, F. nucleatum is frequently detected in oral cancer tissues. Moreover, detection of F. nucleatum is correlated with the clinical stage of oral cancer. Although the detailed mechanism is still unclear, Fusobacterium species have been suggested to be associated with cell adhesion, tumorigenesis, epithelial-to-mesenchymal transition, inflammasomes, cell cycle, etc. in oral cancer. In this review, we introduce the reports focused on the association of Fusobacterium species with cancer development and progression including oral, esophageal, and colon cancers.
Keywords: Fusobacterium nucleatum, oral cancer, cancer development and progression
1. Introduction
Oral cancer, predominantly oral squamous cell carcinoma (OSCC), is a significant health problem and is regarded as the main cause of death from oral diseases in many countries. Traditional risk factors of oral cancer include alcohol abuse, tobacco and tobacco-derivate chewing, and oral virus infections. Other factors include infections, exposure to ionizing radiation, and environmental pollutants [1]. Thus, various causes of cancer are known to be closely involved in lifestyle choices, such as smoking, drinking, and diet.
Chronic inflammation caused by infections has been suggested to be one of the most important cause of cancers [2]. Indeed, infection of various viruses, bacteria, and parasites, such as Hepatitis B virus (HBV), Hepatitis B virus (HCV), Epstein–Barr virus (EBV), human papilloma virus (HPV), human herpes virus 8 (HHV8), human thymus-derived-cell leukemia/lymphoma virus-1 (HTLV-1), human immunodeficiency virus (HIV), Helicobacter pylori, Schistosomiasis, and liver flukes are well-known causes of cancer [2]. Recently, commensal bacteria are also involved in carcinogenesis. A huge number of different commensal bacteria naturally colonize in the human body in a relatively stable equilibrium. Microbial-immune network correlates gut bacteria with the whole-body health, and the failure of immune homeostasis manifests significant impact on various diseases, which might result in cancer [3,4,5]. Indeed, some commensal bacteria including Peptostreptococcus anaerobius [6], enterotoxigenic Bacteriodes fragiles [7], and Escherichia coli [8] are involved in carcinogenesis of colorectal cancer (CRC).
In the oral cavity, bacteria, fungi, viruses, and archaea naturally colonize in different habitats including the teeth, gingival sulcus, tongue, cheeks, hard and soft palates, and tonsils. The oral microbiota refers to a highly varied and complicated ecosystem of these organisms. Over 700 bacterial species are endemic to the oral cavity, and indigenous oral flora act to prevent the settlement of foreign bacteria. Some bacteria of the oral cavity are harmful and can cause serious disease, while many of the oral bacteria are in fact beneficial in preventing diseases. Thus, the oral cavity is inhabited by complex multispecies bacterial communities that usually exist in a balanced immunoinflammatory state with the host [9]. It is now established that many chronic inflammatory conditions are caused by an imbalance between host–microbiota interactions, resulting in a dysbiotic community, deregulated immune responses, and eventually disease outcomes [10]. Oral commensal bacteria play a critical role in the development of oral diseases, including periodontal disease and tooth loss, and maintenance of a normal oral physiological environment [11,12]. Moreover, oral commensal bacteria are known to be involved in the pathogenesis and development of systematic diseases, such as pneumonia, cardiovascular diseases, diabetes, dementia, etc. It has been of concern that oral commensal bacteria may be involved in the pathogenesis of OSCC [13,14]. However, it remains unclear the role of bacteria regarding carcinogenesis of OSCC, even though a lot of bacteria inhabit in the oral cavity. Interestingly, it recently has been shown that one of oral commensal bacteria, Fusobacterium species, especially, play a crucial role for the development of CRC [15,16,17]. As Fusobacterium species are commensal bacteria in the oral cavity, the cumulative evidences of Fusobacterium species in CRC make us hypothesize that Fusobacterium species may be involved in the pathogenesis and development of OSCC. In this review, we introduce the reports focused on the association of Fusobacterium species with cancer development and progression.
2. Fusobacterium Species
The genus Fusobacterium are Gram-negative, non-spore forming, non-motile, pleomorphic, and obligate anaerobic bacilli, which inhabit the human oral cavity, oropharynx, upper respiratory, gastrointestinal, and female genitourinary tracts as part of the normal flora [18]. Nine species including F. nucleatum (subspecies nucleatum, polymorphum, vincentii, animalis, fusiforme, and canifelium), F. necrophorum (subspecies necrophorum and funduliforme), F. ulcerans, F. gonidiaformans, F. mortiferum, F. naviforme, F. necrogenes, F. russii, and F. varium cause human infections of the head and neck, chest, lung, liver, and abdomen [19]. F. nucleatum is a well-known oral bacterium that forms typical dental plaque on human teeth and is involved in periodontal diseases [20]. The greatest characteristic of F. nucleatum is to adhere to various bacteria and cells. F. nucleatum is a central species in physical interactions between Gram-positive and Gram-negative species that are likely to be important for biofilm formation, and it is considered as a bridge for the attachment of commensals that colonize the tooth and epithelial surface with true pathogens [21,22]. F. nucleatum has two types of substance—fimbriae and non-fimbrial adhesin—for attaching to other bacteria and cells. These substances contribute to colonization and also bacterial pathogenesis and infection. Fusobacterium adhesion A (FadA), a fimbrial adhesin protein, was recently shown to be required for bacterial attachment and invasion of gingival epithelial and endothelial cells [23]. FadA has two forms: pre-FadA and mature FadA (mFadA; 111 amino acids). The pre-FadA (129 amino acids) is a non-secreted protein and is associated with the inner membrane. The mFadA is a secreted protein and is easily dissociated from bacteria. Mixtures of pre-FadA and mFadA form high-molecular-weight aggregates, which are required for attachment and invasion of host cells [24]. FadA is highly conserved among oral fusobacteria, such as F. nucleatum, F. periodonticum and F. simiae, whereas it is absent in non-oral fusobacterial species, including F. gonidiaformans, F. mortiferum, F. naviforme, F. russii, and F. ulcerans [23].
Two distinct types of adherence protein have been found in fusobacteria and classified based on their inhibition mode using either D-galactose or L-arginine [25]. Adherence to predominantly Gram-negative late-colonizing bacteria, including Porphyromonas gingivalis, Tannerella forsythia, and Treponema denticola, is associated with galactose-inhibiting (lectin-like) interactions, while adherence to mainly Gram-positive early colonizing species is associated with arginine-inhibiting (nonlectin-like) interactions. Three components, a 40–42 kDa major outer membrane porin protein (FomA), and 39.5-kDa and 30-kDa polypeptides, have been suggested as possible adhesins involved in the lectin-like interbacterial co-aggregation of F. nucleatum [26,27,28]. These adherent factors of Fusobacterium play important roles in tumor progression as discussed in the next section.
3. F. nucleatum and Cancer
3.1. F. nucleatum in Colorectal Cancer
Elevated F. nucleatum levels were significantly detected in colon tissue of colon cancer patients compared with healthy people and F. nucleatum inhabited on colorectal tissues in a half of colon cancer cases [29,30], suggesting that F. nucleatum may be involved in CRC development. Moreover, F. nucleatum colonies in primary CRC tissues were also identified in the metastatic liver tissues [31]. Komiya et al. reported that F. nucleatum was detected in both CRC and oral saliva samples, 75% of which was the same strain [32]. Cumulative clinical evidences suggested that the enrichment of F. nucleatum might be related to CRC metastasis [29,31,33,34,35]. Moreover, F. nucleatum was associated with CRC recurrence and resistance to chemotherapy by activating the autophagy pathway [36]. Thus, F. nucleatum that may be derived from oral cavity is frequently detected in CRC samples and is suggested to be involved in malignant behaviors of CRC.
As described above, several reports show the association of F. nucleatum with carcinogenesis or metastasis of CRC. Kostic et al. reported that intake of F. nucleatum to ApcMIN/+ mice, which causes gastrointestinal cancer, promoted small and large intestinal tumorigenesis [37]. Moreover, F. nucleatum was enriched in tumor tissues compared with Streptococcus species [37]. Importantly, abundance of Fusobacterium was frequently detected in the stool of patients as well as in the adenomas and CRC tissues [37]. In the intestinal tumor microenvironment, F. nucleatum selectively expanded myeloid-derived immune cells but not lymphoid immune cells, leading to tumor progression [37]. Moreover, F. nucleatum promotes metastasis of CRC by modulating KRT7-AS/KRT7 [38].
The outer membrane proteins of F. nucleatum, such as FadA and Fibroblast activation protein 2 (Fap2) have been focused as CRC pathogen. E-cadherin acts as a tumor suppressor by modulating β-catenin pathway [39,40]. Loss or heterogeneous expression of E-cadherin correlated with advanced stages and poor prognosis of CRC patients [41]. Rubinstein et al. demonstrated that F. nucleatum attached and invaded into CRC cells via the FadA-mediated interaction with E-cadherin [15]. Moreover, FadA promotes E-cadherin-mediated CRC tumor growth in xenograft mice via NF-κB activation, producing proinflammatory cytokines such as IL-6, IL-8, and IL-18 and upregulation of Wnt signaling gene (Wnt-7a, -7b, and -9a), Myc, and Cyclin D1 [15]. Interestingly, patients with adenoma and adenocarcinoma in colon had elevated FadA gene expression 10–100 times higher compared to normal individuals [15].
Fap2 also plays a critical function in the development of CRC. Fap2, a 390-KDa protein encoded by the Fap2 gene of F. nucleatum. Fap2 is suggested to be a galactose-sensitive hemagglutinin and adhesin that is likely to play a role in the virulence of fusobacteria [42]. Fap2 inhibits the immune cells, such as T cells and NK cells for killing the CRC cells via a immunoreceptor, TIGIT [16]. Moreover, acetylgalactosamine (Gal-GalNAc) is recognized by fusobacterial Fap2, which functions as a Gal-Gal-NAc lectin [17]. Intravenously injected F. nucleatum localized to mouse CRC tissues in a Fap2-dependent manner, suggesting that fusobacteria use a hematogenous route to reach colon adenocarcinomas via interaction between Fap2 and Gal-GalNAc [17]. Interestingly, Gal-GalNAc is highly expressed in adenocarcinomas including ovary, stomach, colon and lung [43,44]. Although it is still unclear the role of GalNAc in OSCC, N-acetylgalactosaminyltransferase 3 (GalNAc-T3), which regulates the critical initial steps of mucin-type O-glycosylation, may play a role in the pathogenesis of recurrence of early stage of OSCC [45]. These observations suggest that Fap2 of Fusobacterium may modulate tumor progression by binding to Gal-GalNAc on cancer cells.
Today, there are several therapeutic approaches available with which to modify gut microbiota on CRC management. To alter the composition and the activity of gut microbiota, several therapeutic methods, such as fecal microbiota transplantation and administration of prebiotics, probiotics, and synbiotics, are available for CRC patients [46]. In addition to these methods, oral hygiene managements for reducing the amount of F. nucleatum may contribute to the prevention of CRC.
3.2. F. nucleatum in Esophageal Cancer
The involvement of F. nucleatum in the development of esophageal cancer has also been reported. Yamamura et al. reported that DNA levels of F. nucleatum in esophageal cancer tissues were higher than those in pared adjacent non-tumor tissues [47]. Moreover, esophageal squamous cell carcinoma (ESCC) tissues contained more Fusobacterium (3.2% vs. 1.3%) and less Streptococcus (12.0% vs. 30.2%), compared to the non-tumor tissues [48]. Importantly, higher DNA levels of F. nucleatum in ESCC patients were significantly associated with cancer-specific survival [47], predicted poor recurrence-free survival, and poor response to neoadjuvant chemotherapy [49]. In addition, C-C Motif Chemokine Ligand 20 (CCL20), which plays crucial roles in cell proliferation and migration, is significantly upregulated in F. nucleatum-positive esophageal cancer tissues [47]. Thus, F. nucleatum is involved in the development of colorectal and esophageal cancers.
3.3. Fusobacterium Species and Oral Cancer
There are many reports showing that Fusobacterium were detected in OSCC tissues [50,51]. The ratio between aerobes and anaerobes within the biofilms on the surfaces of OSCC tissues was approximately 1:2, whereas that in the healthy control was 2:1, indicating that OSCC surfaces provide an important reservoir for anaerobic bacteria [52]. F. nucleatum subsp. polymorphum was the most significantly overrepresented species in OSCC compared to the control group with deep-epithelium swabs [53]. Perera et al. also reported that the Fusobacterium was enriched in OSCC biopsy compared to fibroepithelial polyp as a control [54]. Moreover, significantly greater bacterial diversity was observed in the swab of OSCC sites than that of normal sites [55]. Thus, distribution of bacteria including Fusobacterium in OSCC tissues may be distinct from that in healthy oral mucosal tissues. Yang et al. reported that F. periodonticum and several bacteria in oral rinse samples were associated with OSCC, and they progressively increased in abundance from stage I to stage IV [56].
Fusobacterium can invade into epithelial cells. Compared to P. gingivalis, wild-type F. nucleatum 12,230 remarkably adheres and invades into human gingival epithelial cells (HGECs) [57]. Interestingly, the spontaneous mutant of F. nucleatum was unable to invade into HGECs, suggesting the requirement for bacterial components to their invasion [40]. Moreover, glucose inhibition assay shows that lectin-like interactions are involved in the attachment of F. nucleatum to OSCC cells [57]. Furthermore, infection of F. nucleatum in human epithelial cells promotes cellular migration, possibly via stimulation of Etk/BMX, S6 kinase p70, and RhoA kinase and increases the production of MMP-13 (collagenase 3) via the activation of mitogen-activated protein kinase p38 [58]. However, the detailed mechanisms of adhesion of Fusobacterium in OSCC cells and F. nucleatum-mediated invasion of OSCC cells is still unclear. Nevertheless, the fact that F. nucleatum is abundant in the oral cavity of OSCC patients seems to be important in the tumorigenesis and/or the progression of oral cancer.
Several reports show the involvement of F. nucleatum in tumorigenesis and development of OSCC. Gallimidi et al. demonstrated that chronic intake of P. gingivalis and F. nucleatum promoted tumor progression in a 4-nitroquinoline-1-oxide (4NQO)-induced mouse tongue cancer model [59]. The infected group showed larger and more invasive tumors with increased expression of cyclin D1, IL-6, and phospho-STAT3. Moreover, co-culture with P. gingivalis and F. nucleatum upregulated IL-6 expression in OSCC cells, whereas these effects was not caused by F. nucleatum alone [59]. These findings suggest that exposure of oral epithelial cells to P. gingivalis/F. nucleatum triggers TLR signaling, resulting in IL-6 production that activates STAT3 which in turn induces important effectors driving growth and invasiveness of OSCC cells, such as cyclin D1.
It is known that epithelial-to-mesenchymal transition (EMT) in cancer cells is associated with invasion, metastasis, stemness, and resistance of therapy [60]. Recently, F. nucleatum promotes cell migration and EMT by upregulating mesenchymal markers, including N-cadherin, Vimentin, and SNAI1 in noncancerous human immortalized oral epithelial cells and OSCC cell lines [61]. As EMT is important event of tumor progression and malignant behaviors, it is worth investigating whether F. nucleatum is involved in EMT in OSCC cells. Recently, it has been reported that partial-EMT (p-EMT) that partially combines epithelial and mesenchymal features, is involved in tumor progression and metastasis [62,63]. We previously reported that SERPINE1, ITGA5, TGFBI, P4HA2, CDH13, and LAMC2 can be a prognostic marker among p-EMT genes [64]. In our preliminary finding, co-culture with F. nucleatum promoted invasion of OSCC cells with upregulation of p-EMT genes [65]. We are now investigating the detailed mechanism of F. nucleatum–driven p-EMT in OSCC.
Inflammasomes are multiprotein complexes that regulate immune processes in response to infections and tissue damage. Inflammasomes mediate the processing of the two most important inflammatory cytokines, pro-interleukin-1β (IL-1β), and pro-IL-18 to their active forms. The inflammasome is formed by the apoptosis-associated speck-like protein containing a CARD (ASC), procaspase-1, and a sensor protein, which is either a NOD-like receptor (NLR) or an absent in melanoma 2 (AIM2)-like receptor. IL-1β plays a pro-tumorigenic role and enhances the aggressiveness of OSCC [66]. Aral et al. reported that F. nucleatum infection in OSCC cells promotes AIM2 inflammasome expression [67]. In addition, F. nucleatum potentially upregulated IL-1β expression, but downregulated POP1 which controls NLRP3 inflammasome activation by targeting ASC. Especially in the oral cavity, it is reported that the presence of nanoparticles released from dental metal alloy activates NLRP3 inflammasome in human oral keratinocytes, resulting in the development of potentially malignant oral disorders [68]. As TRIM16, which enhances IL-1β production, is also upregulated by F. nucleatum, F. nucleatum may play a role by dysregulating inflammasomes and their modulators in OSCC.
Bacterial infection influences genomic stability and integrity by causing DNA damage, which increases the possibility of tumor initiation and development. Recently, it has been reported that F. nucleatum infection in OSCC cells causes DNA damage via Ku70/p53 pathway [69]. Although Ku70 is involved in the non-homologous end joining (NHEJ) pathway of DNA repair via binding to DNA double-strand break ends, the detailed mechanism of the association between F. nucleatum infection and Ku70 is still unclear.
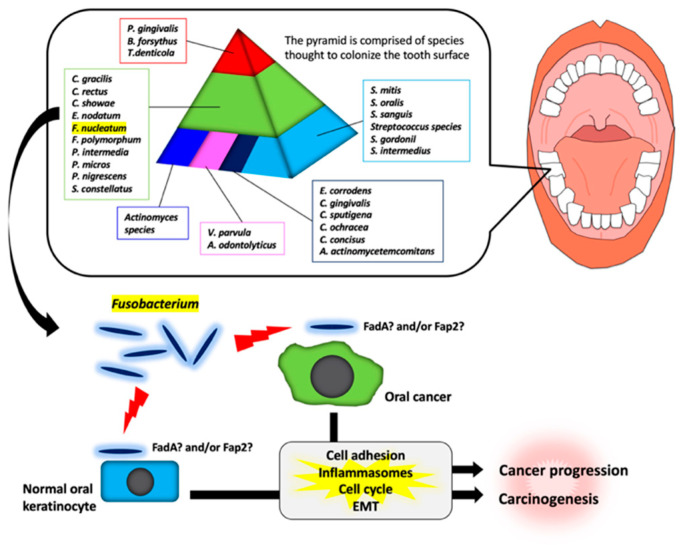
It has been shown that there are specific associations among bacteria within dental plaque by cluster analysis using subgingival plaque samples [70,71]. As shown in Figure 1, various bacteria exist as shown in the pyramid. F. nucleatum is in the middle of pyramid. Among the species in the middle of pyramid, F. nucleatum is dominant in the dental biofilm at a later stage of plaque formation. As described above, Fusobacterium infection affects the tumorigenesis and development of OSCC through various responses (Figure 1). However, the target molecules of Fusobacterium are still unknown. Further studies will be required for clarifying the evidence of Fusobacterium involvement in tumorigenesis and development of OSCC.
Figure 1.
Schematic model for the involvement of Fusobacterium species in oral carcinogenesis and cancer progression. In a dental plaque, various bacteria exist as shown in the pyramid. The base of the pyramid is comprised of species thought to colonize the tooth surface and proliferate at an early stage. Then, complex species in the middle of pyramid becomes numerically more dominant later and is thought to bridge the early colonizers. Finally, the complex species in the top of the pyramid numerically more dominant at late stages in plaque development. Among them, Fusobacterium species may adhere with oral keratinocyte or oral cancer cells via interaction between FadA/Fap2 and E-cadherin. This interaction may induce carcinogenesis and cancer progression.
4. Conclusions
F. nucleatum is well known oral commensal bacterium that forms typical dental plaque on human teeth is involved periodontal diseases. The involvement of F. nucleatum in carcinogenesis and the development of CRC has attracted attention in the field of CRC research. Importantly, the enrichment of F. nucleatum is frequently observed in OSCC tissues compared to healthy oral mucosal tissues. However, the roles of F. nucleatum in OSCC are still unclear. It is also necessary to investigate whether the mechanism of F. nucleatum in OSCC overlaps with that in CRC. We suggest that oral hygiene managements for reducing the amount of F. nucleatum may contribute to the prevention of OSCC and CRC. Moreover, various commensal bacteria exist in the oral cavity. Therefore, it is interesting to examine the relationship between F. nucleatum and other bacteria in the tumorigenesis and development of OSCC.
Acknowledgments
We thank Yoichiro Miyake (Tokushima Bunri University) for excellent suggestions.
Author Contributions
N.F., N.K., and Y.K. wrote the manuscript; K.Y., K.O., and T.Y. edited the manuscript, with contributions from all authors. All authors have read and agreed to the published version of the manuscript.
Funding
This work was supported by grants to N. Fujiwara from JSPS KAKENHI (19K19315) and Y. Kudo from JSPS KAKENHI (19H03853 and 19K22718).
Conflicts of Interest
The authors declare no conflict of interest.
References
- 1.Anand P., Kunnumakkara A.B., Sundaram C., Harikumar K.B., Tharakan S.T., Lai O.S., Sung B., Aggarwal B.B. Cancer is a preventable disease that requires major lifestyle changes. Pharm. Res. 2008;25:2097–2116. doi: 10.1007/s11095-008-9661-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kuper H., Adami H.O., Trichopoulos D. Infections as a major preventable cause of human cancer. J. Intern. Med. 2000;248:171–183. doi: 10.1046/j.1365-2796.2000.00742.x. [DOI] [PubMed] [Google Scholar]
- 3.Blumberg R., Powrie F. Microbiota, disease, and back to health: A metastable journey. Sci. Transl. Med. 2012;4:rv7. doi: 10.1126/scitranslmed.3004184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Erdman S.E., Poutahidis T. Gut bacteria and cancer. Biochim. Biophys. Acta (BBA)-Rev. Cancer. 2015;1856:86–90. doi: 10.1016/j.bbcan.2015.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Erdman S.E., Rao V.P., Olipitz W., Taylor C.L., Jackson E.A., Levkovich T., Lee C.W., Horwitz B.H., Fox J.G., Ge Z., et al. Unifying roles for regulatory T cells and inflammation in cancer. Int. J. Cancer. 2010;126:1651–1665. doi: 10.1002/ijc.24923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tsoi H., Chu E.S.H., Zhang X., Sheng J., Nakatsu G., Ng S.C., Chan A.W.H., Chan F.K.L., Sung J.J.Y., Yu J. Peptostreptococcus anaerobius induces intracellular cholesterol biosynthesis in colon cells to induce proliferation and causes dysplasia in mice. Gastroenterology. 2017;152:1419–1433.e5. doi: 10.1053/j.gastro.2017.01.009. [DOI] [PubMed] [Google Scholar]
- 7.Thiele Orberg E., Fan H., Tam A.J., Dejea C.M., Destefano Shields C.E., Wu S., Chung L., Finard B.B., Wu X., Fathi P., et al. The myeloid immune signature of enterotoxigenic Bacteroides fragilis-induced murine colon tumorigenesis. Mucosal Immunol. 2017;10:421–433. doi: 10.1038/mi.2016.53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zhang S., Fu J., Dogan B., Scherl E.J., Simpson K.W. 5-Aminosalicylic acid downregulates the growth and virulence of Escherichia coli associated with IBD and colorectal cancer, and upregulates host anti-inflammatory activity. J. Antibiot. 2018;71:950–961. doi: 10.1038/s41429-018-0081-8. [DOI] [PubMed] [Google Scholar]
- 9.Hajishengallis G., Lamont R.J. Beyond the red complex and into more complexity: The polymicrobial synergy and dysbiosis (PSD) model of periodontal disease etiology. Mol. Oral Microbiol. 2012;27:409–419. doi: 10.1111/j.2041-1014.2012.00663.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mohammed H., Varoni E.M., Cochis A., Cordaro M., Gallenzi P., Patini R., Staderini E., Lajolo C., Rimondini L., Rocchetti V. Oral Dysbiosis in Pancreatic Cancer and Liver Cirrhosis: A Review of the Literature. Biomedicines. 2018;6:115. doi: 10.3390/biomedicines6040115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Abiko Y., Sato T., Mayanagi G., Takahashi N. Profiling of subgingival plaque biofilm microflora from periodontally healthy subjects and from subjects with periodontitis using quantitative real-time PCR. J. Periodontal Res. 2010;45:389–395. doi: 10.1111/j.1600-0765.2009.01250.x. [DOI] [PubMed] [Google Scholar]
- 12.Preza D., Olsen I., Willumsen T., Boches S.K., Cotton S.L., Grinde B., Paster B.J. Microarray analysis of the microflora of root caries in elderly. Eur. J. Clin. Microbiol. Infect Dis. 2009;28:509–517. doi: 10.1007/s10096-008-0662-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zhang L., Liu Y., Zheng H.J., Zhang C.P. The Oral Microbiota May Have Influence on Oral Cancer. Front. Cell Infect. Microbiol. 2020;9:476. doi: 10.3389/fcimb.2019.00476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kudo Y., Tada H., Fujiwara N., Tada Y., Tsunematsu T., Miyake Y., Ishimaru N. Oral environment and cancer. Genes Environ. 2016;38:13. doi: 10.1186/s41021-016-0042-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rubinstein M.R., Wang X., Liu W., Hao Y., Cai G., Han Y.W. Fusobacterium nucleatum promotes colorectal carcinogenesis by modulating E-cadherin/beta-catenin signaling via its FadA adhesin. Cell Host Microbe. 2013;14:195–206. doi: 10.1016/j.chom.2013.07.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gur C., Ibrahim Y., Isaacson B., Yamin R., Abed J., Gamliel M., Enk J., Bar-On Y., Stanietsky-Kaynan N., Coppenhagen-Glazer S., et al. Binding of the Fap2 protein of Fusobacterium nucleatum to human inhibitory receptor TIGIT protects tumors from immune cell attack. Immunity. 2015;42:344–355. doi: 10.1016/j.immuni.2015.01.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Abed J., Emgard J.E., Zamir G., Faroja M., Almogy G., Grenov A., Sol A., Naor R., Pikarsky E., Atlan K.A., et al. Fap2 Mediates Fusobacterium nucleatum Colorectal Adenocarcinoma Enrichment by Binding to Tumor-Expressed Gal-GalNAc. Cell Host Microbe. 2016;20:215–225. doi: 10.1016/j.chom.2016.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Long S., Prober C., Fischer M. Principles and Practice of Pediatric Infectious Diseases. 5th ed. Elsevier; Amsterdam, The Netherlands: 2017. pp. 1015–1017. [Google Scholar]
- 19.Citron D.M. Update on the taxonomy and clinical aspects of the genus fusobacterium. Clin. Infect Dis. 2002;35(Suppl. S1):S22–S27. doi: 10.1086/341916. [DOI] [PubMed] [Google Scholar]
- 20.Patini R., Staderini E., Lajolo C., Lopetuso L., Mohammed H., Rimondini L., Rocchetti V., Franceschi F., Cordaro M., Gallenzi P. Relationship between oral microbiota and periodontal disease: A systematic review. Eur. Rev. Med. Pharmacol. Sci. 2018;22:5775–5788. doi: 10.26355/eurrev_201809_15903. [DOI] [PubMed] [Google Scholar]
- 21.Kolenbrander P.E., Andersen R.N., Blehert D.S., Egland P.G., Foster J.S., Palmer R.J., Jr. Communication among oral bacteria. Microbiol. Mol. Biol. Rev. 2002;66:486–505. doi: 10.1128/MMBR.66.3.486-505.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kolenbrander P.E. Oral microbial communities: Biofilms, interactions, and genetic systems. Ann. Rev. Microbiol. 2000;54:413–437. doi: 10.1146/annurev.micro.54.1.413. [DOI] [PubMed] [Google Scholar]
- 23.Han Y.W., Ikegami A., Rajanna C., Kawsar H.I., Zhou Y., Li M., Sojar H.T., Genco R.J., Kuramitsu H.K., Deng C.X. Identification and characterization of a novel adhesin unique to oral fusobacteria. J. Bacteriol. 2005;187:5330–5340. doi: 10.1128/JB.187.15.5330-5340.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Xu M., Yamada M., Li M., Liu H., Chen S.G., Han Y.W. FadA from Fusobacterium nucleatum utilizes both secreted and nonsecreted forms for functional oligomerization for attachment and invasion of host cells. J. Biol. Chem. 2007;282:25000–25009. doi: 10.1074/jbc.M611567200. [DOI] [PubMed] [Google Scholar]
- 25.Amano A. Bacterial adhesins to host components in periodontitis. Periodontol. 2000. 2010;52:12–37. doi: 10.1111/j.1600-0757.2009.00307.x. [DOI] [PubMed] [Google Scholar]
- 26.Kaufman J., DiRienzo J.M. Isolation of a corncob (coaggregation) receptor polypeptide from Fusobacterium nucleatum. Infect. Immun. 1989;57:331–337. doi: 10.1128/IAI.57.2.331-337.1989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kinder S.A., Holt S.C. Localization of the Fusobacterium nucleatum T18 adhesin activity mediating coaggregation with Porphyromonas gingivalis T22. J. Bacteriol. 1993;175:840–850. doi: 10.1128/JB.175.3.840-850.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Shaniztki B., Hurwitz D., Smorodinsky N., Ganeshkumar N., Weiss E.I. Identification of a Fusobacterium nucleatum PK1594 galactose-binding adhesin which mediates coaggregation with periopathogenic bacteria and hemagglutination. Infect. Immun. 1997;65:5231–5237. doi: 10.1128/IAI.65.12.5231-5237.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Castellarin M., Warren R.L., Freeman J.D., Dreolini L., Krzywinski M., Strauss J., Barnes R., Watson P., Allen-Vercoe E., Moore R.A., et al. Fusobacterium nucleatum infection is prevalent in human colorectal carcinoma. Genome Res. 2012;22:299–306. doi: 10.1101/gr.126516.111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kostic A.D., Gevers D., Pedamallu C.S., Michaud M., Duke F., Earl A.M., Ojesina A.I., Jung J., Bass A.J., Tabernero J., et al. Genomic analysis identifies association of Fusobacterium with colorectal carcinoma. Genome Res. 2012;22:292–298. doi: 10.1101/gr.126573.111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bullman S., Pedamallu C.S., Sicinska E., Clancy T.E., Zhang X., Cai D., Neuberg D., Huang K., Guevara F., Nelson T., et al. Analysis of Fusobacterium persistence and antibiotic response in colorectal cancer. Science. 2017;358:1443–1448. doi: 10.1126/science.aal5240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Komiya Y., Shimomura Y., Higurashi T., Sugi Y., Arimoto J., Umezawa S., Uchiyama S., Matsumoto M., Nakajima A. Patients with colorectal cancer have identical strains of Fusobacterium nucleatum in their colorectal cancer and oral cavity. Gut. 2019;68:1335–1337. doi: 10.1136/gutjnl-2018-316661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Yang Y., Weng W., Peng J., Hong L., Yang L., Toiyama Y., Gao R., Liu M., Yin M., Pan C., et al. Fusobacterium nucleatum increases proliferation of colorectal cancer cells and tumor development in mice by activating toll-like receptor 4 signaling to nuclear factor-kappab, and up-regulating expression of MicroRNA-21. Gastroenterology. 2017;152:851–866.e24. doi: 10.1053/j.gastro.2016.11.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Li Y.Y., Ge Q.X., Cao J., Zhou Y.J., Du Y.L., Shen B., Wan Y.J., Nie Y.Q. Association of Fusobacterium nucleatum infection with colorectal cancer in Chinese patients. World J. Gastroenterol. 2016;22:3227–3233. doi: 10.3748/wjg.v22.i11.3227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Yan X., Liu L., Li H., Qin H., Sun Z. Clinical significance of Fusobacterium nucleatum, epithelial-mesenchymal transition, and cancer stem cell markers in stage III/IV colorectal cancer patients. Onco Targets Ther. 2017;10:5031–5046. doi: 10.2147/OTT.S145949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Yu T., Guo F., Yu Y., Sun T., Ma D., Han J., Qian Y., Kryczek I., Sun D., Nagarsheth N., et al. Fusobacterium nucleatum promotes chemoresistance to colorectal cancer by modulating autophagy. Cell. 2017;170:548–563.e16. doi: 10.1016/j.cell.2017.07.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kostic A.D., Chun E., Robertson L., Glickman J.N., Gallini C.A., Michaud M., Clancy T.E., Chung D.C., Lochhead P., Hold G.L., et al. Fusobacterium nucleatum potentiates intestinal tumorigenesis and modulates the tumor-immune microenvironment. Cell Host Microbe. 2013;14:207–215. doi: 10.1016/j.chom.2013.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Chen S., Su T., Zhang Y., Lee A., He J., Ge Q., Wang L., Si J., Zhuo W., Wang L. Fusobacterium nucleatum promotes colorectal cancer metastasis by modulating KRT7-AS/KRT7. Gut Microbes. 2020;11:511–525. doi: 10.1080/19490976.2019.1695494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Bryant D.M., Stow J.L. The ins and outs of E-cadherin trafficking. Trends Cell Biol. 2004;14:427–434. doi: 10.1016/j.tcb.2004.07.007. [DOI] [PubMed] [Google Scholar]
- 40.Peifer M., Polakis P. Wnt signaling in oncogenesis and embryogenesis—A look outside the nucleus. Science. 2000;287:1606–1609. doi: 10.1126/science.287.5458.1606. [DOI] [PubMed] [Google Scholar]
- 41.Dorudi S., Sheffield J.P., Poulsom R., Northover J.M., Hart I.R. E-cadherin expression in colorectal cancer. An immunocytochemical and in situ hybridization study. Am. J. Pathol. 1993;142:981–986. [PMC free article] [PubMed] [Google Scholar]
- 42.Coppenhagen-Glazer S., Sol A., Abed J., Naor R., Zhang X., Han Y.W., Bachrach G. Fap2 of Fusobacterium nucleatum is a galactose-inhibitable adhesin involved in coaggregation, cell adhesion, and preterm birth. Infect. Immun. 2015;83:1104–1113. doi: 10.1128/IAI.02838-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Yang G.Y., Shamsuddin A.M. Gal-GalNAc: A biomarker of colon carcinogenesis. Histol. Histopathol. 1996;11:801–806. [PubMed] [Google Scholar]
- 44.Abed J., Maalouf N., Parhi L., Chaushu S., Mandelboim O., Bachrach G. Tumor Targeting by Fusobacterium nucleatum: A Pilot Study and Future Perspectives. Front. Cell Infect. Microbiol. 2017;7:295. doi: 10.3389/fcimb.2017.00295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Harada Y., Izumi H., Noguchi H., Kuma A., Kawatsu Y., Kimura T., Kitada S., Uramoto H., Wang K.Y., Sasaguri Y., et al. Strong expression of polypeptide N-acetylgalactosaminyltransferase 3 independently predicts shortened disease-free survival in patients with early stage oral squamous cell carcinoma. Tumour Biol. 2016;37:1357–1368. doi: 10.1007/s13277-015-3928-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Kaźmierczak-Siedlecka K., Daca A., Fic M., van de Wetering T., Folwarski M., Makarewicz W. Therapeutic methods of gut microbiota modification in colorectal cancer management—Fecal microbiota transplantation, prebiotics, probiotics, and synbiotics. Gut Microbes. 2020;11:1518–1530. doi: 10.1080/19490976.2020.1764309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Baba H. Human Microbiome Fusobacterium Nucleatum in Esophageal Cancer Tissue Is Associated with Prognosis. Clin. Cancer Res. 2016;22:5574–5581. doi: 10.1158/1078-0432.CCR-16-1786. [DOI] [PubMed] [Google Scholar]
- 48.Shao D., Vogtmann E., Liu A., Qin J., Chen W., Abnet C.C., Wei W. Microbial characterization of esophageal squamous cell carcinoma and gastric cardia adenocarcinoma from a high-risk region of China. Cancer. 2019;125:3993–4002. doi: 10.1002/cncr.32403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Yamamura K., Baba Y., Nakagawa S., Mima K., Miyake K., Nakamura K., Sawayama H., Kinoshita K., Ishimoto T., Iwatsuki M., et al. Intratumoral Fusobacterium Nucleatum Levels Predict Therapeutic Response to Neoadjuvant Chemotherapy in Esophageal Squamous Cell Carcinoma. Clin. Cancer Res. 2019;25:6170–6179. doi: 10.1158/1078-0432.CCR-19-0318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Nagy K.N., Sonkodi I., Szoke I., Nagy E., Newman H.N. The microflora associated with human oral carcinomas. Oral Oncol. 1998;34:304–308. doi: 10.1016/S1368-8375(98)80012-2. [DOI] [PubMed] [Google Scholar]
- 51.Schmidt B.L., Kuczynski J., Bhattacharya A., Huey B., Corby P.M., Queiroz E.L., Nightingale K., Kerr A.R., DeLacure M.D., Veeramachaneni R., et al. Changes in abundance of oral microbiota associated with oral cancer. PLoS ONE. 2014;9:e98741. doi: 10.1371/journal.pone.0098741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Bolz J., Dosa E., Schubert J., Eckert A.W. Bacterial colonization of microbial biofilms in oral squamous cell carcinoma. Clin. Oral Investig. 2014;18:409–414. doi: 10.1007/s00784-013-1007-2. [DOI] [PubMed] [Google Scholar]
- 53.Al-Hebshi N.N., Nasher A.T., Maryoud M.Y., Homeida H.E., Chen T., Idris A.M., Johnson N.W. Inflammatory bacteriome featuring Fusobacterium nucleatum and Pseudomonas aeruginosa identified in association with oral squamous cell carcinoma. Sci. Rep. 2017;7:1834. doi: 10.1038/s41598-017-02079-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Perera M., Al-Hebshi N.N., Perera I., Ipe D., Ulett G.C., Speicher D.J., Chen T., Johnson N.W. Inflammatory Bacteriome and Oral Squamous Cell Carcinoma. J. Dent. Res. 2018;97:725–732. doi: 10.1177/0022034518767118. [DOI] [PubMed] [Google Scholar]
- 55.Zhao H., Chu M., Huang Z., Yang X., Ran S., Hu B., Zhang C., Liang J. Variations in oral microbiota associated with oral cancer. Sci. Rep. 2017;7:11773. doi: 10.1038/s41598-017-11779-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Yang C.Y., Yeh Y.M., Yu H.Y., Chin C.Y., Hsu C.W., Liu H., Huang P.J., Hu S.N., Liao C.T., Chang K.P., et al. Oral Microbiota Community Dynamics Associated With Oral Squamous Cell Carcinoma Staging. Front. Microbiol. 2018;9:862. doi: 10.3389/fmicb.2018.00862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Han Y.W., Shi W., Huang G.T., Kinder Haake S., Park N.H., Kuramitsu H., Genco R.J. Interactions between periodontal bacteria and human oral epithelial cells: Fusobacterium nucleatum adheres to and invades epithelial cells. Infect. Immun. 2000;68:3140–3146. doi: 10.1128/IAI.68.6.3140-3146.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Uitto V.J., Baillie D., Wu Q., Gendron R., Grenier D., Putnins E.E., Kanervo A., Firth J.D. Fusobacterium nucleatum increases collagenase 3 production and migration of epithelial cells. Infect. Immun. 2005;73:1171–1179. doi: 10.1128/IAI.73.2.1171-1179.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Binder Gallimidi A., Fischman S., Revach B., Bulvik R., Maliutina A., Rubinstein A.M., Nussbaum G., Elkin M. Periodontal pathogens Porphyromonas gingivalis and Fusobacterium nucleatum promote tumor progression in an oral-specific chemical carcinogenesis model. Oncotarget. 2015;6:22613–22623. doi: 10.18632/oncotarget.4209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Nieto M.A., Huang R.Y., Jackson R.A., Thiery J.P. Emt: 2016. Cell. 2016;166:21–45. doi: 10.1016/j.cell.2016.06.028. [DOI] [PubMed] [Google Scholar]
- 61.Zhang S., Li C., Liu J., Geng F., Shi X., Li Q., Lu Z., Pan Y. Fusobacterium nucleatum promotes epithelial-mesenchymal transiton through regulation of the lncRNA MIR4435-2HG/miR-296-5p/Akt2/SNAI1 signaling pathway. FEBS J. 2020 doi: 10.1111/febs.15233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Bednarz-Knoll N., Alix-Panabieres C., Pantel K. Plasticity of disseminating cancer cells in patients with epithelial malignancies. Cancer Metastasis Rev. 2012;31:673–687. doi: 10.1007/s10555-012-9370-z. [DOI] [PubMed] [Google Scholar]
- 63.Saitoh M. Involvement of partial EMT in cancer progression. J. Biochem. 2018;164:257–264. doi: 10.1093/jb/mvy047. [DOI] [PubMed] [Google Scholar]
- 64.Kisoda S., Shao W., Fujiwara N., Mouri Y., Tsunematsu T., Jin S., Arakaki R., Ishimaru N., Kudo Y. Prognostic value of partial EMT-related genes in head and neck squamous cell carcinoma by a bioinformatic analysis. Oral Dis. 2020 doi: 10.1111/odi.13351. [DOI] [PubMed] [Google Scholar]
- 65.Fujiwara N., Shao W., Yoshida K., Arakaki R., Ozaki K., Ishimaru N., Kudo Y. The effects of Fusobacterium nucleatum in oral cancer cells; Proceedings of the 38th Japan Society for Molecular Pathology; Hyogo, Japan. 19 July 2019. [Google Scholar]
- 66.Lee C.H., Chang J.S., Syu S.H., Wong T.S., Chan J.Y., Tang Y.C., Yang Z.P., Yang W.C., Chen C.T., Lu S.C., et al. IL-1beta promotes malignant transformation and tumor aggressiveness in oral cancer. J. Cell Physiol. 2015;230:875–884. doi: 10.1002/jcp.24816. [DOI] [PubMed] [Google Scholar]
- 67.Aral K., Milward M.R., Gupta D., Cooper P.R. Effects of Porphyromonas gingivalis and Fusobacterium nucleatum on inflammasomes and their regulators in H400 cells. Mol. Oral Microbiol. 2020;35:158–167. doi: 10.1111/omi.12302. [DOI] [PubMed] [Google Scholar]
- 68.Sasabe E., Tomomura A., Kitamura N., Yamamoto T. Metal nanoparticles-induced activation of NLRP3 inflammasome in human oral keratinocytes is a possible mechanism of oral lichenoid lesions. Toxicol. In Vitro. 2020;62:104663. doi: 10.1016/j.tiv.2019.104663. [DOI] [PubMed] [Google Scholar]
- 69.Geng F., Zhang Y., Lu Z., Zhang S., Pan Y. Fusobacterium nucleatum Caused DNA Damage and Promoted Cell Proliferation by the Ku70/p53 Pathway in Oral Cancer Cells. DNA Cell Biol. 2020;39:144–151. doi: 10.1089/dna.2019.5064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Socransky S.S., Haffajee A.D., Cugini M.A., Smith C., Kent R.L., Jr. Microbial complexes in subgingival plaque. J. Clin. Periodontol. 1998;25:134–144. doi: 10.1111/j.1600-051X.1998.tb02419.x. [DOI] [PubMed] [Google Scholar]
- 71.Socransky S.S., Haffajee A.D. Dental biofilms: Difficult therapeutic targets. Periodontol. 2000. 2002;28:12–55. doi: 10.1034/j.1600-0757.2002.280102.x. [DOI] [PubMed] [Google Scholar]