Abstract
(1) This review aims to evaluate the effectiveness of treatments with virtual reality systems (VRSs) on the functional autonomy of older adults versus conventional treatment. (3) Methods: Systematic review and meta-analysis. An electronic data search was carried out, following the PRISMA statement, up to February 2020. We combined results from clinical trials using VRSs for the improvement of basic and instrumental activities of daily living. The guidelines of the Cochrane Handbook for Systematic Reviews of Interventions were followed for calculations and risk of bias. The Grading of Recommendations Assessment, Development and Evaluation (GRADE) was used to assess the quality of evidence. (4) Results: The final analysis included 23 studies with a population of 1595 participants. A moderate, but clinically significant, effect was found for basic activities of daily living (BADLs), (Standard Medium Deviation, SMD 0.61; 95% CI: −0.15–1.37; P < 0.001). A small effect was found for instrumental ADLs (Instrumental Activities of daily living, IADLs) (SMD −0.34; 95% CI: −0.82–0.15; P < 0.001). Functional ambulation was the BADL which improved the most (SMD −0.63; 95% CI: −0.86, −0.40; P < 0.001). (5) Conclusion: The use of VRSs is an innovative and feasible technique to support and improve the functional autonomy of community-dwelling older adults. Due to the very low quality of the evidence for our main outcomes, the effects of a VRS on the BADLs and IADLs are uncertain. Clinical trials of a higher methodological quality are necessary to increase the level of knowledge of its actual effectiveness.
Keywords: virtual reality, functional autonomy, rehabilitation, exergame
1. Introduction
The morphological and functional changes associated with aging can have a negative impact on the performance of activities of daily living (ADLs). It has been estimated that 20–25% of community-dwelling people over 75 may experience limitations in their capacity to perform ADLs [1,2]. This dependency is a predictor of frailty and institutionalization [3,4]. In a recent study, the American Occupational Therapy Association (AOTA) supported the need to build a friendly environment and to implement prevention programs which include physical, social and leisure activities for older persons with a high and stable intrinsic capacity [3].
In the last decade, there has been a growing interest in the use of virtual reality systems (VRSs) to implement programs for supporting the functional ability of older adults through physical exercise [5,6,7], cognitive [8,9] and social interventions [10]. VRSs allow for the re-creation and control of virtual everyday environments, and for the planning of safe, ecological and motivating treatment activities. Unlike the real world, the virtual world can be adapted and adjusted to the capacities and needs of each person, and thus it provides great flexibility of experiences and virtual tasks, which include the sequences of functional movements necessary to achieve autonomy in real-life activity. The analysis and control of all the activity’s virtual elements by the occupational therapist enable virtual achievements which could not be attained in real life, due to either disability or to environment restrictions. These achievements increase motivation, commitment and adherence to the rehabilitation process.
The possibility of generating exercises that can be repeated over time, selecting the frequency and intensity, enables compliance with the principles of motor learning and neuroplasticity, as well as the generalization of this learning [11]. A new performance context is therefore created, with which the person identifies and gets involved. Thus, they manage to carry out actions which are not always possible in their original setting and which can help to improve their occupational performance [12]. These characteristics make virtual reality-based technology an appropriate rehabilitation technique for different people.
Various reviews have been published in recent years about the effectiveness of VRSs for older adults. These have shown positive effects on physical functioning [6,13,14] and cognitive functioning [15,16]. However, no previous review has analyzed the effects of VRSs on autonomy in the performance of activities of daily living in older adults. In addition, many of the previous reviews have focused on older populations with neurological disorders, excluding older adults without disabilities. Thus, the preventive potential of VRSs is still not known.
The aim of this systematic review and meta-analysis is to critically evaluate the effectiveness of VRSs for improving the functional autonomy of older populations and for preventing disability. These findings can be useful for future research and intervention projects aiming at preventing disability and promoting the occupational performance of older adults.
2. Materials and Methods
The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement was employed to carry out this review [17]. The Grading of Recommendations Assessment, Development and Evaluation was also used [18].
2.1. Search
Six databases were searched electronically (Web of Science, OT Seeker, Guideline National Clearing House, databases of the Spanish National Research Council (CSIC), Scopus and Cochrane), up to February 2020. No date, study design, language or age limits were set in order to increase the sensitivity of the search. The electronic search was completed with a hand search of the bibliographical references of the studies included. The search terms were developed by a methodology consultant from the Institute of Health Sciences (ICS, Spain). See Appendix A for key search terms.
The inclusion criteria were the following: (1) studies with older adults over 60 years of age who performed activities of daily living independently, (2) studies which used VRSs in order to improve the performance of ADLs [19], (3) studies whose outcome measures included the assessment of ADLs, (4) studies considered as peer-reviewed scientific literature (Level I, Level II or Level III) [20] and (5) studies with a simple majority in the 25 items of the CONSORT checklist [21].
The studies excluded were those with participants under the age of 60 with neurological or osteoarticular disorders which severely affected functional independence, studies which did not use VRSs directly and studies which did not report on changes in occupational performance.
2.2. Review, Selection and Data Extraction
Two independent reviewers selected the studies. Discrepancies were resolved by a third reviewer. The data extraction protocol was based on the PRISMA items [17] and the Cochrane Handbook for Systematic Reviews of Interventions. The form included information regarding methodological characteristics, participants, healthcare resource, intervention, results on functional ability and conclusions. Study authors were contacted to retrieve unreported data.
2.3. Summary Measures and Statistical Analysis
Various outcome measures were used. Objective measures were included which evaluated ADLs in an overall way (Barthel Index [22], Functional Independence Measure (FIM) [23], Late Life Function and Disability Instrument (LLF&DI) [24] and the Instrumental Activities of Daily Living Scale [25]). Quantitative assessment tools were also included which assessed specific ADLs, such as ambulation or transfers (Functional Gait Assessment (FGA) [26], Timed Up and Go (TUG) [27], Four Step Square Test (FSST) [28], 6-min walk test (6MWT) [29], 8-foot up and go [30] and Five Sit to Stand [31]). The effect magnitude was measured using Hedges’s adjusted g standardized mean difference (SMD), with its confidence interval at 95% (95% CI). The total effect size, weighted by the sample size of the studies, was calculated using the inverse variance method and a random effects model. Its 95% CI and its statistical significance were calculated using the Z-test. The effect size was interpreted using Cohen’s criteria for pooled estimates [32]; SMD > 0.20, small; SMD > 0.50, medium; and SMD > 0.8, large effect.
2.4. Assessment of Level of Evidence of the Set of Studies
The GRADE system [18] was used, considering eight factors to reduce or increase the level of evidence. The factors for downgrading the level were (1) risk of bias; (2) inconsistency; (3) indirect evidence; (4) imprecision by the calculation of the optimal information size (OIS); (5) publication bias. The factors considered for upgrading the level of evidence were (1) large effect size (SMD ˃ 0.8); (2) dose–response effect; (3) control for confounding factors in the individual studies.
2.5. Risk of Bias Assessment in Individual Studies
The risk of bias of each article was assessed independently by two reviewers using the items included in Review Manager (RevMan), version 5.3. (The Nordic Cochrane Centre, The Cochrane Collaboration: Copenhagen, Denmark, 2014). Based on five “risk of bias” items, we determined that studies at:
a low risk of bias were those in which all items were assigned a low risk of bias;
an unclear risk of bias were studies in which one or more items were found to be at an unclear risk of bias; and
a high risk of bias were studies in which one or more items were found to be at a high risk of bias.
2.6. Heterogeneity
The I2 statistic was calculated, which was interpreted as absent (0), low (25), moderate (50) or high (75 or higher).
2.7. Publication Bias
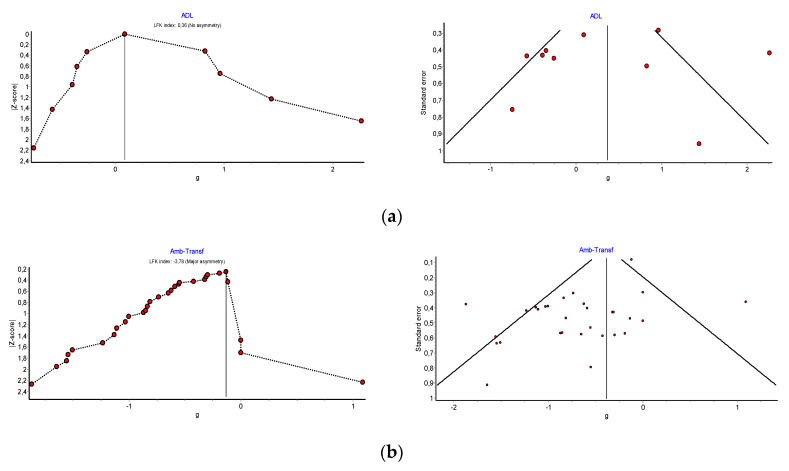
Publication bias was assessed using a funnel plot created with RevMan, complemented with a DOI plot created with METAXL. Egger’s method, Begg’s test with Epidat 3.1 and the Luis Furuya-Kanamori (LFK) index were used. An LFK index ≤ 1 was considered as no asymmetry, ˃1 ≤2 as minor asymmetry and ˃2 as major asymmetry.
3. Results
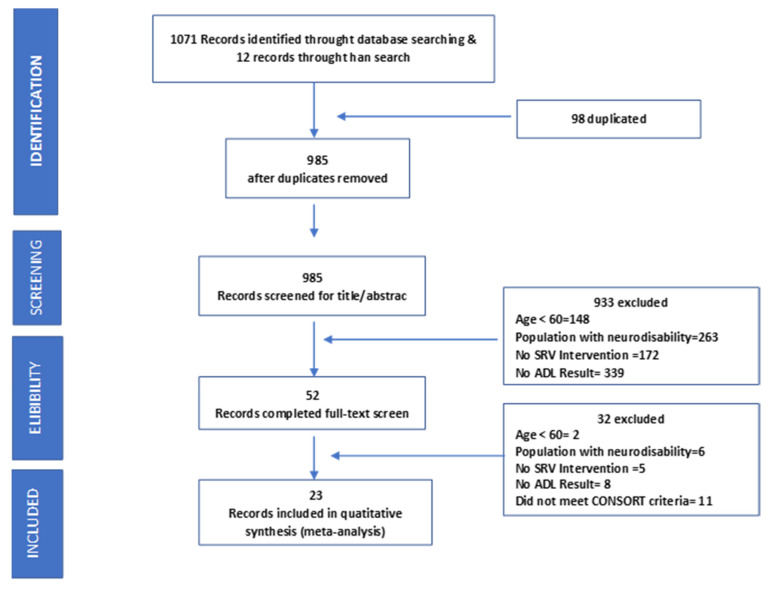
In total, 1083 articles were identified. After removing duplicates, 985 records were screened, with 52 manuscripts selected for complete reading. The full text review included 23 studies applying VRSs to improve the functional ability of independently living older adults over 60 years of age. Figure 1 shows the flow chart of this selection. The total number of participants was 1595, with an age range of 60–96 years.
Figure 1.
PRISMA flow diagram of search strategy and results.
3.1. Characteristics of Included Studies
The included studies were published within the last nine years (2011–2020). That indicates that the use of VRSs is a very recent research area. The aim of these studies was to analyze the effect of VRSs on two areas of occupation and IAVDs; functional ambulation, the capacity to make transfers, cognitive function, physical condition and quality of life. Data about design, sample size, characteristics of the population, type of intervention and assessed outcomes are shown in Appendix B.
Five studies evaluated the overall impact of VRSs on BADLs [33,34,35,36,37] and three studies examined IADLs [38,39,40]. We also identified six studies which assessed the effectiveness of VRSs on the capacity to make transfers and twenty-one studies which reported on their effectiveness in improving functional ambulation.
The studies were randomized and quasi-randomized clinical trials. Eighteen studies were Level I (randomized controlled trials) and five studies were Level II (two groups, nonrandomized studies). The control groups received interventions consisting of physical exercise sessions (six studies) and health education (three studies). The remaining fourteen studies did not design any intervention for the control group. Only five studies carried out a follow-up after the intervention [38,39,41,42,43].
3.2. Intervention with VRS
The use of VRSs was the main intervention technique. Seven studies used VRSs specifically designed for rehabilitation [34,39,42,44,45,46,47]. The rest of the studies used virtual reality active video games (Nintendo® Wii, XBox®, Sony® PlayStation and Xavi Sport®). No study used head-mounted displays. Appendix C shows the devices and exergames used in each article. The duration of the interventions was from 1 to 24 weeks, with sessions between 20 and 50 min.
3.3. Effectiveness of VRSs on Activities of Daily Living
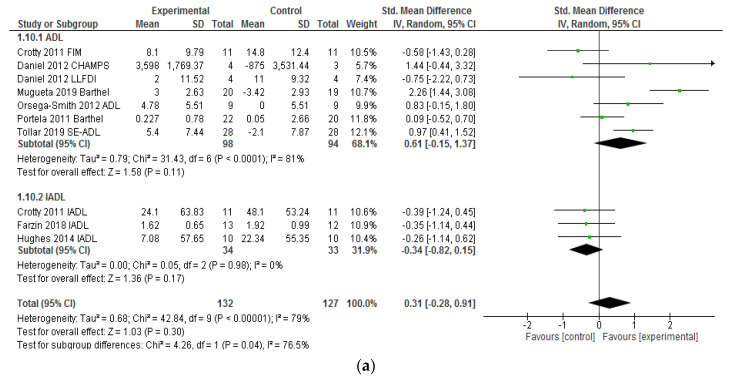
Eight studies provided sufficient data to report on the effectiveness of VRSs in improving the performance of activities of daily living. As Figure 2a shows, the effect size of VRSs in improving the performance of BADLs is moderate but significant; the total SMD was 0.61 (95% CI: −0.15; 1.37). Four of the studies which assessed effectiveness on BADLs obtained a large effect (d > 0.8) [33,34,35,37] and two studies found a medium effect [33,38]. However, the effectiveness of VRSs was smaller for the three studies which assessed IADLs [38,39,40]. The total SMD was −0.34 (95% CI: −0.82; 0.15) and the effect found was small (Figure 2a). This indicates that the interventions with VRSs had a small non-significant effect (p = 0.3) for improving the performance of IADs compared to the control group.
Figure 2.
(a) Forest Plot illustrating effectiveness of VRSs on the activities of daily living (BADL and IADL). (b) Forest Plot illustrating effectiveness of VRSs on the transfer and functional ambulation.
3.4. Effectiveness of VRSs on Functional Ambulation and Transfers
Thirty-two outcomes from twenty-two studies provided sufficient data to analyze the effectiveness of VRS in the improvement of functional ambulation in older adults. The total SMD was −0.63 (95% CI: −0.86, −0.40, p = 0.001). This indicates that the interventions with VRSs had moderate, but significant effects (Figure 2a). The group of participants which received treatment sessions with a VRS increased their level of performance in ambulation compared to the control group that received traditional physical exercise.
Six outcomes of transfer ability from six studies were analyzed. The effect size of the treatment programs with VRSs on the ability to make transfers from sitting to standing and vice versa was small, with an SMD of −0.23 (95% CI: −0.71, −0.25; P < 0.001). Only two studies obtained a large effect [24,35], whereas the rest obtained a low effectiveness. Figure 2b shows the SMD for each study, as well as the total SMD.
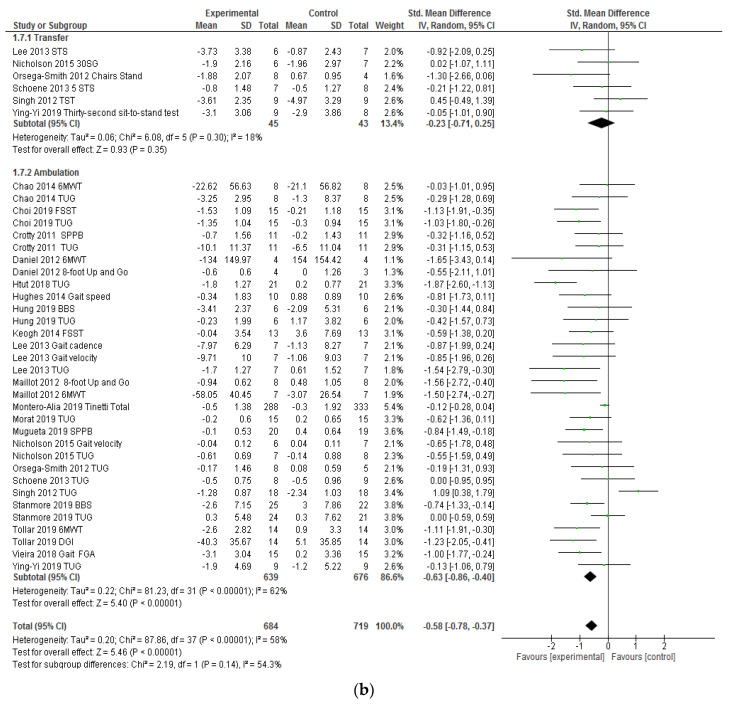
3.5. Risk of Bias of the Individual Studies
Figure 3 shows the risk of bias assessment for each study. The risk of bias was moderate for the studies which addressed the effectiveness of VRSs in the performance of ADLs. Only one study did not do random sequence generation, and seven out of eight studies lacked clarification about the allocation concealment. Five studies (62%) did not blind outcome assessors and the incomplete outcome data bias was low.
Figure 3.
Risk of bias ADL studies, Risk of bias functional mobility studies.
The risk of bias for functional mobility and transfers was high (Figure 3). In functional ambulation, four studies had a high risk of bias for random sequence generation [35,48,49,50], none of the studies could blind participants, only six blinded outcome assessors [37,38,41,47,51,52] and only one had a low risk of bias for allocation concealment. On the other hand, loss to follow-up was significant in only one study (Keogh et al., 2014).
3.6. Heterogeneity
The studies which assessed the overall performance of ADLs (I2 = 79%) and transfers (I2 = 77%; chi-squared p = 0.0007) showed a high heterogeneity. In the studies which analyzed functional ambulation, heterogeneity was moderate, with I2 = 55% (chi-squared p = 0.004). The forest plots (Figure 2a,b) show a significant variability between the studies which favored the experimental intervention.
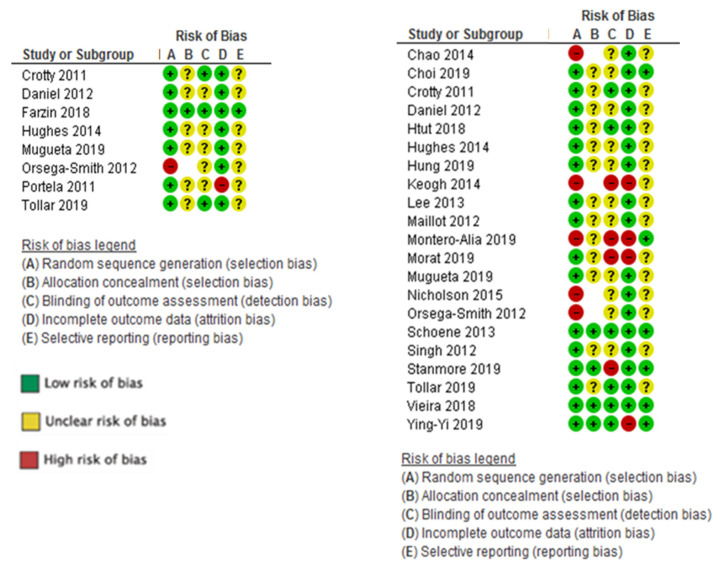
3.7. Publication Bias
The funnel plot and the DOI plot (Figure 4) show signs of publication bias. Both plots present asymmetry, mainly in those studies with fewer participants but a greater impact on functional performance. The LFK index showed minor asymmetry both for ambulation (LFK = 3.78) and for transfers (LFK = 0.36). The statistical significance of Begg’s test for ambulation was p = 0.0235 and that of Egger’s test was p = 0.0057. The statistical significance of Begg’s test for transfers was p = 0.13 and that of Egger’s test was p = 0.11.
Figure 4.
(a) Publication Bias: LFK Index and Doi Plot ADL Studies, (b) Publication Bias: LFK Index and Doi Plot Functional Mobility Studies.
3.8. GRADE Quality of Evidence
The quality of evidence was low to very low for studies which used VRSs to optimize ADL performance, and moderate to low for studies using VRSs to improve functional mobility. Appendix D specifies the reasons for decreasing the level in each of the study groups.
4. Discussion
This systematic review and meta-analysis examined the effectiveness and the quality of evidence of VRSs to support the functional autonomy of non-disabled older adults. Although there are still few studies that have analyzed the effectiveness of intervention programs based on virtual reality on older persons’ occupational performance, the results are encouraging. Seventy-three percent of studies showed significant improvement in the functional ability of this population group. However, the GRADE grading of recommendation was low to very low due to the risk of bias, inconsistency and imprecision of the analyzed data. Therefore, these studies should be treated with caution.
Additionally, clear signs of publication bias were found in studies which assessed functional mobility (LFK: −3.3). A detailed analysis showed that the studies with fewer participants had better results. This indicates the possibility that there might be unpublished studies which did not show significant effects of VRSs.
In most studies, the intervention with VRS was applied through commercial exergames or active video games; only seven studies used VRSs specifically designed for rehabilitation. This may be due to the accessibility and low cost of active game consoles. Moreover, commercial exergames offer a virtual re-creation of environments and challenges that are highly immersive, appealing and enjoyable for the user, thus increasing commitment to the task. In line with other reviews [53,54], our results suggest that the use of commercial virtual reality consoles, such as the Nintendo Wii®, PlayStation® and Xbox Kinect®, can be beneficial and feasible in improving the functional autonomy of older persons.
We found that the use of VRSs is more effective and has greater evidence in the field of occupation corresponding to BADLs and ambulation than in the performance of IADLs. The reason for these results may be that IADLs are more complex activities, both in their treatment and their assessment, because they depend largely on the social and environmental context [55]. These factors are not addressed in the intervention programs based on VRSs. In this regard, recent reviews [56,57] conclude that improvement in physical performance does not always translate into improvement in IADLs. Nevertheless, we found a direct link between an increase in physical functional test scores (TUG, 6MWT) and the performance of basic activities. We assume, from these results, that intervention with VRSs could help older persons to live independently and safely in their own home and could facilitate productive aging.
This review and meta-analysis has several strengths. Its methodology did not set a time or language limit on the publications and made use of a wide range of databases in order to increase the sensitivity of the search. It also included articles of high methodological quality: 78% of the studies were Level I and the remaining 22% were Level II articles.
However, the articles included had a number of important methodological limitations: the sample size, the risk of bias and the post-intervention follow-up. Only two studies had more than 100 participants, and sixteen studies had fewer than 50 participants. Regarding the risk of bias, none of the studies could blind participants and only seven studies blinded assessors. The lack of post-intervention follow-up made it impossible to know the long-term and preventive effect of VRSs on the functional ability of older persons.
5. Conclusions
As a conclusion, our findings suggest that the use of VRSs is an innovative and feasible technique to support and improve the functional autonomy of community-dwelling older adults. However, clinical trials of a higher methodological quality are necessary to increase the level of knowledge of its actual effectiveness.
Appendix A
Table A1.
Key search terms.
| Category | Key Search Terms |
|---|---|
| Population | Aging, elderly, geriatr *, gerontology, late life, older adults, oldest, seniors, old age. |
| Intervention: VRT | (“Wii *” OR “gaming technology” OR “active videogame” OR nintendo OR “video game*” OR exergam* OR Wii OR kinect OR Xbox OR “Play Station” OR “Xavi Sports”) OR (“virtual reality” OR virtual-reality tecnhology OR “Virtual navigation” OR “Virtual environment” OR “Simulated reality” OR “virtual rehabilitation” OR vr-based OR “virtually simulated” OR “use-computer interface”) |
| Outcome | Activities of daily living, daily living activities, daily self-care activities, adl, daily life activity *, functional Independence, physical functional performance, transfer, bathing, grooming, eating, feeding, functional mobility, walking, walking capacity, ambulation, gait, mobility, showering, toilet hygiene, toileting, personal hygiene, self-care, self-feeding, |
| Study and trial designs | clinical trial, controlled clinical trial, double blind, evidence-based, evidence synthesis, feasibility study, health technology assessment, intervention, longitudinal, multicenter study, pilot, random allocation, randomized controlled trials, standard of care, treatment outcome, validation study |
Appendix B
| Characteristics of Included Studies (N = 23) | |||||||||||
| Author | Evidence Level Design | Participants | Intervention | Follow-ups | Result | ||||||
| n | Age (yrs) Mean (SD) Range |
Sex | Inclusion Criteria | Placement | Experimental Group | Control Group |
Outcome Measures | Results | |||
| Chao 2014 [48] |
Level II | n = 32 EC = 16 CC = 16 |
85 (79–91) |
67 % Female | >65 years; independent walking; able to read and speak English; able to follow instructions | Assisted living Buffalo (EEUU) |
SAHA + Nintendo Wii Fit 4 weeks 2 times/week |
Health educational session | BBS; TUG SMWT; GDS FES; SF8 |
No follow-up | The experimental group improved gait speed, reduced depressive symptoms and increased confidence in activities of daily living. The control group did not show improvement in any result. |
| Choi 2019 [58] |
Level I RCT |
n = 57 EC = 28 CC = 29 |
69–85 | 84% Female | >65 years; < 26 MCA; able to communicate | Welfare center, Korea | VPK Exercise 6 weeks 2 times/week |
Home exercise program: flexion, curl-ups, sideways leg lifts, prone leg lifts and supine leg lifts. | BBS; FSST; TUG; OLST; MCA; ACT | No follow-up | VPK improves physical and cognitive functions. VKP exercise induces significant increases in postural control and muscular strength. |
| Crotty 2011 [38] |
Level I RCT |
n = 44 EC = 22 CC = 22 |
84 (80–88) |
79% Female |
>65 years; <150 kilos; independent walking; MEC: 21–30; good level of vision | Acute care hospital, Australia |
Nintendo Wii 2 weeks 5 times/week |
Strength, balance, aerobic exercises | TUG; BBS; SPPB; FIM; AIDL | 4 weeks after intervention | Wii is feasible for providing treatment to elderly patients. It can improve mobility and balance in comparison with traditional approaches. |
| Daniel 2012 [33] |
Level I RCT |
n = 23 EC = 16 CC = 7 |
76 (55–86) |
57% Female |
>65 years; 1–2 of the characteristics of frailty | Senior centers and residential living centers Texas, US |
Nintendo Wii Fit 15 weeks 3 times/week |
Traditional senior fitness program | Senior fitness test; body weight; BES, CHAMPS; LLFDI SF-36. | No follow-up | Both groups improved scores in ABC and CHAMPS scales. The experimental group increased caloric expenditure. |
| Farzin 2018 [39] | Level I ECA |
N = 25 | 55 (51–59) |
68% Female | >55 years; absence of a) history of neurological impairments, b) psychiatric disorders, c) learning disabilities, d) cerebrovascular disease | Older Adult University Program Kuala Lumpur, Malaysia |
Virtual Week Board Game 6 weeks 1 time/week |
Usual routine activities | GAS; IADL; PRMQ; PMT | 4 and 12 weeks after the intervention | VWB training improved performance and activities of daily living and reduce depression and anxiety levels. |
| Htut [51] | Level I RCT |
n = 84 EC:VR = 21 EC:BE = 21 EC:PE = 21 CC = 21 |
75 (70–80) |
37% female | 65–85 years MEC > 23 BI = 100 |
Residential aged-care Yangon, Myanmar | Xbox Kinect Cognitive Stimulation Balance exercise 8 weeks 3 times/week |
Without intervention | TUG; 5 TST FES; MoCA BBS |
No follow-up | VR group improved both physical and cognition performance, while BE was effective in enhancing cognition. VR and BE may help fall concern in older persons. |
| Hughes 2014 [40] |
Level II | n = 20 EC = 10 CC = 10 |
77.4 (72–83) |
70% Female | MYHAT Cognitive Classification | Community-dwelling adults Pittsburgh, US |
Nintendo Wii Sports 24 weeks 1 time/week |
Without intervention | CAMCI; CRSQ AIVD GAIT: 6 m |
No follow-up | The experimental group improved in overall cognition, perceived cognitive ability and gait speed. |
| Hung 2019 [42] |
Level I RCT |
n = 24 EC = 12 CC = 12 |
68 (66–72) |
57% female | >60 years; medical diagnoses of diabetes; independently ambulatory; MEC > 24 |
Community-dwelling adults Taipei, China |
Xavi Sport VR 6 weeks 3 times/week |
Without intervention | TUG; BBS UST; MFES |
6 weeks after the intervention | VR showed positive effects on functional balance. BBS, UTS and TUG test scores significantly improved after intervention. |
| Keogh 2014 [49] |
Level II Quasi-experimental |
n = 34 EC = 19 CC = 15 |
83 (75–91) |
55% Female |
>65 years; walk 10 min without aid; cognitive capacity to understand instructions | Residential aged-care Gold Coast, Australia | Nintendo Wii Sports 8 weeks |
Usual routine activities | FSST RAPA WhOQOL-BREF semistructured group Interview |
No follow-up | The intervention group showed a statistically significant improvement in strength in upper limbs, levels of physical and psychological activity and quality of life after participating in virtual reality programs with Wii. |
| Lee 2013 |
Level I RCT |
n = 64 EC = 32 CC = 32 |
74 (69–79) |
71% Female |
>65 years; diagnosis of type 2 DM; able to communicate |
Community-dwelling adults Seoul, Korea |
Sony PlayStation and EyeToy 10 weeks 2 times/week |
Health education on diabetes management | BBS TUG STS Gait Rite FES |
No follow-up | VR can be used to prevent falls and improve the quality of walking. |
| Maillot 2012 [7] |
Level I RCT |
n = 32 EC = 16 CC = 16 |
71 (65–78) |
84% Female | Recommendation to Canadian Health Network. Never play video games and living a sedentary lifestyle |
Community-dwelling adults Paris, France |
Nintendo Wii Sports 14 weeks |
Without intervention | MAQ; GDS MMSE, SFT, TNT, ST, MRT, SST |
No follow-up | Improvement in the VRTI group in cognitive and physical tests. There were no differences in visuospatial function. |
| Montero 2019 [43] |
Level II Quasi-random |
n = 977 EC:508 EE:469 |
75 (72–78) |
59% female | <70 years; able to walk independently (with or without walking aids) |
Community-dwelling adults Cataluña, Spain |
Exergame Wii Fit with Wii Balance Board |
Usual routine activities | Tinetti Test Short FES-I UST |
9 weeks after intervention | Found no effect of balance training usie on balance or falls. A reduced fear of falling was found at 3 months, but no longer at 1 year. The authors think this may be a chance finding. |
| Morat 2019 [46] | n = 45 VOL = 15 VOL + US = 15 Cc = 15 |
69 (64–74) |
62% female | <60 years; healthy | Community-dwelling adults Cologne, Germany |
Dvidat, Senso Dvidat Senso+ Postoromed 8 weeks 3 times/week |
Without intervention | TUG, Y-balance test, motor dual-task | No follow-up | Exergames under stable and unstable conditions are a feasible training tool with high adherence rates to improve functional balance and calf strength. Exergames, especially under unstable conditions, improve factors that are relevant for fall prevention, such as balance, functional mobility and strength. | |
| Mugueta 2019 [34] |
Level I RCT |
n = 40 EC = 20 CC = 20 |
84 (77–91) |
60% female | >65 years; >90 MBI; <10 SPPB; no physical exercise |
Elderly day centers Bilbao, Spain |
Exergame FRED, Kinect 6 weeks 3 times/week |
Without intervention | BI; SPPB EuroQol |
No follow-up | FRED Exergame reduced frailty risk: 14.7% less than control group No difference in EuroQol or BI. |
| Nicholson 2015 [50] |
Level II Two groups, nonrandomized studies |
n = 43 EC = 21 CC = 22 |
74 (69–79) |
76% Female | >65 years; not involved in balance exercises for the last 3 months; independent walking; adequate visual capacity; without progressive or terminal illness, acute illness or unstable chronic illness | Community-dwelling adults. Sunshine Coast, Australia |
Nintendo Wii Fit 6 weeks 3 times/week without supervision |
Without intervention | TUG; FES STS; PACES; FR |
No follow-up | The experimental group improved in all variables but only left lateral reach showed statistical significance. |
| Orsega-Smith 2012 [35] |
Level I RCT |
n = 30 EC = 20 CC = 9 |
71 (66–83) |
92% Female |
>63 years | Community-dwelling Older Adults | Nintendo Wii Fit: balance and yoga 4 weeks 8 weeks |
Without intervention | ABC/FES; ADL BBS; TUG; CS |
No follow-up | The experimental group improved transfers, balance and ADLs. The control group did not show any changes. |
| Portela [36] | Level I RCT |
n = 65 EC = 23 CC = 42 |
79 (78–80) |
61% Female |
>65 years; good level of vision and hearing; stand for 2 min without upper limb support | Community-dwelling Older Adults | Nintendo Wii 12 weeks 1 time/week |
Traditional senior fitness program | BI; BBS; MMSE SF36 |
No follow-up | The supervised use of Wii had an impact on physical improvement. The unsupervised use of Wii had a positive impact on vitality and mental health. |
| Schoene 2013 [47] |
Level I RCT |
n = 37 EC = 15 CC = 17 |
77.5 (73–82) |
- | Walking independently 20 m; independent for ADLs |
Independent-living units Sydney, Australia |
Exergame DDR Stepmania 8 weeks 2 times/week |
Usual routine activities | CSRT RT/CRST MT; 5STS; TUG TRIAL MAKING FES; PPA; AST |
No follow-up | VR is safe and can be applied at home. It improves physical and cognitive parameters for fall prevention. |
| Singh 2013 [44] |
Level I RCT |
n = 38 EC = 16 CC = 16 |
62.5 (58–69) |
100% Female |
>65 years; independent walking | Senior citizens’ club Kuala Lumpur, Malaysia | Wii Balance Board 6 weeks |
Traditional senior fitness balance program | OPI; TST; TUG | No follow-up | VR improves agility, balance and functional mobility. There was no significant difference between groups. |
| Stanmore 2019 [45] |
Level I RCT |
n = 106 EC = 56 CC = 50 |
78 (58–96) |
78 % Female | >55 years; mental capacity; able to speak English; able to watch television from 2 m distance; able to use VR |
Assisted living facilities Manchester and Glasgow, UK |
Exergame FAME OTAGO 12 weeks |
Physical exercise | BBS; FES TUG; GDS |
No follow-up | VR exergame improved balance, pain and fear of falling and are a cost-effective fall prevention strategy in assisted living facilities. |
| Tollar 2019 [37] |
Level I RCT |
n = 83 EC-CYC = 27 EC-EXE = 28 CC = 28 |
69.6 (66–72) |
53% Female | >60 years; >24 MMSE; >40 BDI; mobility difficulty | Hospital Somogy, Hungary |
Xbox or bicycle ergometer 5 weeks 5 times/week |
Usual routine activities | 6MWT; SE-ADL; DGI; MAP; SF-36; WOMAC | No follow-up | Xbox and cycling improved general health-related QoL and walking capacity. Xbox improved the SE-ADL (7.3%) |
| Gomes 2019 [41] | Level I RCT |
n = 30 EC = 15 CC = 15 |
84 (78–90) |
93% female | >60 years; able to walk independently; normal or corrected visual acuity; good hearing; no previous experience with VR |
Sao Paulo Brazil Hospital |
Nintendo Wii Fit 7 weeks 2 times/week |
Advice regarding the importance of physical activity | FGA; MoCA; FES | 4 weeks after intervention | VR Wii-Fit was feasible, acceptable and safe for frail older adults and improved their postural control and gait. There were no effects on cognition, mood or fear of falling. |
| Liao 2019 [52] | Level I ECA |
n = 52 EC = 27 Cc = 25 |
81 (73–89) |
>65 and <95 years; the presence of at least one of the 5 frailty characteristics defined by Fried |
Daycare centers Taiwan |
Kinect: Tano, LongGood 12 weeks 3 times/week |
Combined exercise: Resistance, aerobic and balance | IPAQ: IMC; TUG; grip strength; FES | No follow-up | Kinect-based exergaming is at least as beneficial as combined exercise in the prefrail and frail elderly. | |
| ABC: Activity-specific Balance Confidence; ACT: Arm Curl Test; ADL: Activities of Daily Living; AIDL: Activity Instrumental Daily Living; AST: Alternate Step Test; BBS: Balance Berg Scale; BE: Brain Exercise; BI: Barthel Index; BDI: Beck Depression Inventory; CAMCI: Computer Assessment of Mild Cognitive Impairment; CHAMPS: Community Healthy Activities Model Program for Seniors questionnaire CSRQ: Cognitive Self-Report Questionnaire; CRST-RT: Choice Stepping Reaction Time; CS: Chair Stand; FES: Falls Efficacy Scale; DGI: Dynamic Gait Index: FGA: Functional Gait Assessment; FIM: Functional Independence Measure; FPA: Foot Placement Accuracy; FR: Functional Reach; FSST: Four Square Step Test; GAS: Geriatric Anxiety Scale; GDS: Geriatric Depression Scale; IADL: Instrumental Activities of Daily Living scale; Level I: randomized controlled trials; Level II: two groups, nonrandomized studies (e.g., cohort, case–control); MAQ: Modifiable Activity Questionnaire; MBI: Modified Barthel Index; MCA: Montreal Cognitive Assessment; MEC: Mini-Examen Cognoscitivo; DM: Diabetes Mellitus; MAP: Mean Arterial Pressure; MCA: Montreal Cognitive Assessment; MFES: Modified Falls Efficacy Scale; MMSE = Mini Mental State Examination; MoCA: Montreal Cognitive Assessment; MRT: Matrix Reasoning Test; MT: Movement Time; OLST: One-Leg Stance Test; OPI: Overall Performance Index; PPA: Physiological Profile Assessment score; PACES: Physical Activity Enjoyment Scale; PE: Physical Exercise; PMT: Prospective Memory Tasks; PRMQ: Prospective Retrospective Memory Questionnaire; RAPA: Rapid Assessment Physical Activity scale; RCT: Randomized Clinical Trial; SFT: Senior Fitness Test; SF8: Short Form 8; SF36: Short Form 36; ST: Stroop Test; SE-ADL: Schwab–England Activities of Daily Living scale; SF-36: Short Form 36 Health Survey; SMWT: Six-Minute Walk Test; SPPB: Shot Physical Performance Battery; SST: Spatial Span Test TMT: Trail Making Test; TST: Ten Step Test; TUG: Timed Up and Go; UST: Unipedal Stance Test; VR: Virtual Reality; WHOQL-BREF: World Health Organization Quality of Life; WOMAC: McMaster Universities Osteoarthritis Index; VPK: Virtual Kayak Paddling; 5STS = Five Times Sit-to-Stand; 6MWT: 6-min Walk Test. | |||||||||||
Appendix C
Table A2.
Virtual Reality Types, Video Game Consoles and Exergames of Included Studies.
| Author | Virtual Reality Type | Videogame Console and Technical Assistance | Exergame |
|---|---|---|---|
| Chao, 2014 [48] | Active Video Game | Nintendo Wii + Balance Board Walker was placed around the balance board |
Wii Fit: Jogging; LungE; Penguin slide Table tilt; Chair; Deep breathing |
| Choi, 2019 [58] | Specific Virtual Reality | Virtual kayak paddling + a projected video | Kayaking |
| Crotty, 2011 [38] | Active Video Game | Nintendo Wii + Balance Board Chair around the balance board |
Wii Fit |
| Daniel, 2012 [33] | Active Video Game | Nintendo Wii + weighty vest | Wii Sport, tennis, boxing, boling |
| Farzin, 2019 [39] | Specific Virtual Reality | Virtual Week (VW) Board Game | VW includes 8 to 10 PM tasks (four regular, four irregular and two stop clock tasks) which allow for exercising almost all types of everyday PM tasks (e.g., self-care, medication adherence, keeping social appointments) |
| Htut, 2018 [51] | Active Video Game | X-Box 360 + Kinect | Light Raise, Virtual Smash Stack ’em Up, One Ball Roll, Pin Push, Super Saber, Target Kick, Play Paddle Panic, Body Bally, Bamp Bash |
| Hughes, 2014 [40] | Active Video Game | Nintendo Wii | Wii Sports: bowling, golf, tennis, and baseball Wii Play: Wii Resort Boom Blox |
| Hung, 2019 [42] | Active Video Game | Xavi Sport + stepping mat | Set-up, stepping exercise, hamster game, drumming game |
| Keogh, 2014 [49] | Active Video Game | Nintendo Wii | Wii Sports: bowling, golf, tennis, baseball, boxing |
| Lee, 2013 [59] | Active Video Game | Play Station + EyeToy | Wishi Washi: window washing, Keep Ups, Bowling, Bubble Pop, Boot Camp, Kung Foo |
| Maillot, 2012 [7] | Active Video Game | Nintendo Wii | Wii Fit Wii Sport: tennis |
| Montero, 2019 [43] | Active Video Game | Nintendo Wii | Not specified |
| Morat, 2019 [46] | Specific Virtual Reality | Dividat Senso Swing and Posturomed | Targets, Divided, Simon, Flexi, Snake, Tetris, Habitats, Birds, Hexagon |
| Mugueta, 2019 [34] | Specific Virtual Reality | FRED + Kinect | FRED entails several scenarios, with each one representing one or more steps in a simplified process to enable txakoli to be produced |
| Nicholson, 2015 [50] | Active Video Game | Nintendo Wii + Balance Board | Soccer heading, penguin slide, ski slalom, ski jump, table tilt, snowball fight, perfect 10, and tightrope walking |
| Orsega Smith, 2012 [35] | Active Video Game | Nintendo Wii + Balance Board | Wii Fit: Balance Games: Penguin Slide,’ ‘Table Tilt,’ ‘Ski Slalom,’ ‘Balance Bubble’, Hula Hood, Snowboard Slalom; Wii Fit: Yoga: deep breathing, half-moon, palm tree |
| Portela [36] | Active Video Game | Nintendo Wii | Wii Sport |
| Schoene, 2013 [47] | Active Video Game: Stepmania | Television + step pad + computer unit | Open-source modified DDR game Stepmania: pressure sensitive panels which represent stepping direction and additional cognitive load (“bomb” for dodge) |
| Singh, 2013 [44] | Active Video Game | Nintendo Wii+ Balance Board | Ski Slalom, Table Tilt, Penguin Slide, Soccer Heading, Tight Rope Walk, Perfect 10, Tilt City |
| Stanmore, 2019 [45] | Specific Virtual Reality | MIRA Exergames + Kinect | Side Taps: Atlantis, Catch, Izzy the Bee, Move, Follow; Jugger, Firefly, Catch, Follow, Move; Sit to Stand: Powerhouse Bid, Atlantis, Izzy the Bee; Squats: Izzy the Bee, Atlantis, Catch, Move, Follow; Hip Frontal Flexion: Animals, Atlantis, Airplane, Catch, Follow, Colour Clouds, Move, Piano; Elbow Flexion: Grab, Catch, Follow, Atlantis, Izzy the Bee, Move, Firefly, Piano, Jugger; Full Body Turn: Animals, Catch, Firefly, Colour Clouds, Follow, Jugger, Basketball, Move; General–Shoulder: Atlantis, Catch, Firefly, Follow, Izzy the Bee, Jugger, Move; Hip Abduction: Atlantis, Catch, Izzy the Bee, Move, Follow, Fireflies, Jugger, Seasons; Knee Flexion: Grab, Catch, Follow, Atlantis, Izzy the Bee, Move, Firefly, Jugger; Shoulder Abduction: Atlantis, Follow, Catch, Izzy the Bee, Move, Firefly, Jugger, Follow, Memory scape |
| Tollar, 2019 [37] | Specific Virtual Reality | Exer Program designed to improve postural control, gait mobility, gait stability, turning and balance + Kinect |
Space Pop trains spatial orientation through target reaching with arms, legs and whole body and Just Dance prompts users to generate and combine movement sequences |
| Gomes, 2018 [41] | Active Video Game | Nintendo + Balance Board | Wii Fit Plus: Table Tilt, Rhythm, Parade, Obstacle Course, Single Leg Extension, Tilt City, Basic Step, Penguin Heading Soccer, Basic Run, Torso Twist |
| Liao, 2019 [52] | Active Video Game | Tano and LongGood software packages + Kinect | Tai-chi exercise, resistance and aerobic exercises, balance game |
Appendix D
Table A3.
Grading of Recommendations Assessment, Development and Evaluation (GRADE): Evidence Profile: SRV vs. control on functional autonomy: ADL.
| Evidence Profile: SRV vs. Control on Functional Capacity: ADL | Evidence Profile: SRV vs. Control on Functional Mobility | ||||
|---|---|---|---|---|---|
| N° of studies: 8 (10 comparisons) Type of studies: RCT Intervention: Virtual Reality Systems on ADL Control: TPE, ADL, programs of health education or non-intervention N° of patients: 212 |
N° of studies: 22 (38 comparisons) Type of studies: RCT Intervention: Virtual Reality Systems Control: physical exercise, programs of health education or non-intervention N° of patients: 1097 |
||||
| GRADE Factor | Importance | Explanations | GRADE Factor | Importance | Explanations |
| Limitations in study design or execution (risk of bias) | Moderate ↓1 level |
Downgrading for risk of bias was not considered because most information is from studies at moderate risk of bias Moderate risk of bias Rate down one level |
Limitations in study design or execution (risk of bias) | Moderate ↓1 level |
Downgrading for risk of bias was not considered because most information is from studies at moderate risk of bias. Moderate risk of bias Rate down one level |
| Inconsistency results | Serious ↓1 level |
Downgrading for inconsistency was considered because I2 = 79%. | Inconsistency results | No serious inconsistency | Downgrading for inconsistency was not considered because I2 = 58% |
| Indirectness evidence | No serious indirectness | In none of the studies were there substantial differences between the population, intervention or outcomes measured in the studies and those established in the systematic review. | Indirectness evidence | No serious indirectness | In none of the studies were there substantial differences between the population, intervention or outcomes measured in the studies and those established in the systematic review. |
| Imprecision | Moderated ↓1 level |
The OIS was calculated, the resulting OIS being 276 participants with MDS = 0.3. The number of patients included in the meta-analysis is 212, moderately lower to the OIS. Downgrading for imprecision was considered. |
Imprecision | No serious imprecision | The OIS was calculated, the resulting OIS being 276 participants with MDS = 0.3. The number of patients included in the meta-analysis is 1097, far superior to OIS. Downgrading for imprecision was not considered. |
| Publication bias | Not serious | Downgrading for publication bias was not considered because the DOI plot shows no asymmetry with LFK = 0.36. |
Publication bias | Serious ↓1 level |
Downgrading for publication bias was considered because the DOI plot shows marked asymmetry with LFK = 3.3 (major asymmetry). |
| Magnitude of effect | Moderated ↓1 level |
SMD = │0.31 │ Upgrading for large magnitude of effect was not considered. |
Magnitude of effect | Not serious | SMD =│0.58│ Upgrading for large magnitude of effect was not considered. |
| Dose-response gradient | Not considered. | Dose–response gradient | Not considered. | ||
| No plausible confounders | Not considered because studies in this meta-analysis are not observational. | No plausible confounders | Not considered because studies in this meta-analysis are not observational. | ||
| Quality rating | Very low quality: we are moderately confident in the effect estimate; the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different (GRADE Working Group grades of evidence) | Quality rating | Moderate–low quality: we are moderately confident in the effect estimate; the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different (GRADE Working Group grades of evidence) | ||
Abbreviations: ADL: Activities of Daily Living; LFK: LFK Index; MCID: Minimum Clinically Important Difference; RCT: Randomized Controlled Trial; OIS: Optimal Information Size. VRS: Virtual Reality System.
Author Contributions
Conceptualization: A.-I.C.-S.; formal analysis, A.S.-F. and A.-I.C.-S.; Investigation: A.-I.C.-S. and B.P.-L.; Methodology: J.-J.C.-Á.; Project administration: B.P.-L. and A.M.-M.; Supervision, A.-I.C.-S.; Visualization: A.-I.C.-S. and M.R.-H.; Writing—original draft: A.-I.C.-S. and J.-J.C.-Á.; Writing—review and editing: A.-I.C.-S. and M.R.-H. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Conflicts of Interest
The authors declare no conflict of interest.
References
- 1.Iwarsson S., Horstmann V., Sonn U. Assessment of dependence in daily activities combined with a self-rating of difficulty. J. Rehabil. Med. 2009;41:150–156. doi: 10.2340/16501977-0298. [DOI] [PubMed] [Google Scholar]
- 2.Yang Y. Characterising Long Term Care Needs among Chinese Older Adults with Cognitive Impairment or ADL Limitations. J. Cross Cult. Gerontol. 2019;35:35–47. doi: 10.1007/s10823-019-09382-8. [DOI] [PubMed] [Google Scholar]
- 3.Liu C.-J.C. Functional Ability in the Changing Demographic Landscape: Evidence and Opportunities for Occupational Therapy. Am. J. Occup. 2018;72:7204170010p1–7204170010p5. doi: 10.5014/ajot.2018.724002. [DOI] [PubMed] [Google Scholar]
- 4.Vermeulen J., Neyens J.C.L., van Rossum E., Spreeuwenberg M.D., de Witte L.P. Predicting ADL disability in community-dwelling elderly people using physical frailty indicators: A systematic review. BMC Geriatr. 2011;11:33. doi: 10.1186/1471-2318-11-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Costa M.T.S., Vieira L.P., de Oliveira Barbosa E., Oliveira L.M., Maillot P., Vaghetti C.A.O., Giovani Carta M., Machado S., Gatica-Rojas V., Monteiro-Junior R.S. Virtual Reality-Based Exercise with Exergames as Medicine in Different Contexts: A Short Review. Clin. Pract. Epidemiol. Ment. Health. 2019;15:15–20. doi: 10.2174/1745017901915010015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Skjæret N., Nawaz A., Morat T., Schoene D., Helbostad J.L., Vereijken B. Exercise and rehabilitation delivered through exergames in older adults: An integrative review of technologies, safety and efficacy. Int. J. Med. Inform. 2016;85:1–16. doi: 10.1016/j.ijmedinf.2015.10.008. [DOI] [PubMed] [Google Scholar]
- 7.Maillot P., Perrot A., Hartley A. Effects of interactive physical-activity video-game training on physical and cognitive function in older adults. Psychol. Aging. 2012;27:589–600. doi: 10.1037/a0026268. [DOI] [PubMed] [Google Scholar]
- 8.Belchior P., Yam A., Thomas K.R., Bavelier D., Ball K.K., Mann W.C., Marsiske M. Computer and Videogame Interventions for Older Adults’ Cognitive and Everyday Functioning. Games Health J. 2019;8:129–143. doi: 10.1089/g4h.2017.0092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Faria A.L., Andrade A., Soares L.I., Badia S.B. Benefits of virtual reality based cognitive rehabilitation through simulated activities of daily living: A randomized controlled trial with stroke patients. J. Neuroeng. Rehabil. 2016;13:96. doi: 10.1186/s12984-016-0204-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Li J., Erdt M., Chen L., Cao Y., Lee S.-Q., Theng Y.-L. The Social Effects of Exergames on Older Adults: Systematic Review and Metric Analysis. J. Med. Int. Res. 2018;20:e10486. doi: 10.2196/10486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Levin M.F. Can virtual reality offer enriched environments for rehabilitation? Expert Rev. Neurother. 2011;11:153–155. doi: 10.1586/ern.10.201. [DOI] [PubMed] [Google Scholar]
- 12.Contreras K., Cubillos R., Hernández Ó., Reveco C., Santis N. Rehabilitación virtual en la intervención de terapia ocupacional. Rev. Chil. Ter. Ocup. 2014;14:197–209. doi: 10.5354/0719-5346.2014.35722. [DOI] [Google Scholar]
- 13.Choi S.D., Guo L., Kang D., Xiong S. Exergame technology and interactive interventions for elderly fall prevention: A systematic literature review. Appl. Ergon. 2017;65:570–581. doi: 10.1016/j.apergo.2016.10.013. [DOI] [PubMed] [Google Scholar]
- 14.Neri S.G., Cardoso J.R., Cruz L., Lima R.M., de Oliveira R.J., Iversen M.D., Carregaro R.L. Do virtual reality games improve mobility skills and balance measurements in community-dwelling older adults? Systematic review and meta-analysis. Clin. Rehabil. 2017;31:1292–1304. doi: 10.1177/0269215517694677. [DOI] [PubMed] [Google Scholar]
- 15.Bonnechère B., Jansen B., Omelina L., Van Sint Jan S. The use of commercial video games in rehabilitation: A systematic review. Int. J. Rehabil. Res. 2016;39:277–290. doi: 10.1097/MRR.0000000000000190. [DOI] [PubMed] [Google Scholar]
- 16.D’Cunha N.M., Nguyen D., Naumovski N., McKune A.J., Kellett J., Georgousopoulou E.N., Frost J., Isbel S. A Mini-Review of Virtual Reality-Based Interventions to Promote Well-Being for People Living with Dementia and Mild Cognitive Impairment. Gerontology. 2019;65:430–440. doi: 10.1159/000500040. [DOI] [PubMed] [Google Scholar]
- 17.Moher D., Liberati A., Tetzlaff J., Altman D.G. PRISMA Group Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009;6:e1000097. doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Guyatt G., Oxman A.D., Akl E.A., Kunz R., Vist G., Brozek J., Norris S., Falck-Ytter Y., Glasziou P., DeBeer H., et al. GRADE guidelines: 1. Introduction-GRADE evidence profiles and summary of findings tables. J. Clin. Epidemiol. 2011;64:383–394. doi: 10.1016/j.jclinepi.2010.04.026. [DOI] [PubMed] [Google Scholar]
- 19.American Occupational Therapy Association Occupational Therapy practice framework: Domain and Process (3rd Edition) Am. J. Occup. Ther. 2017;68:S1. doi: 10.5014/ajot.2014.682006. [DOI] [Google Scholar]
- 20.Sackett D.L., Rosenberg W.M., Gray J.A., Haynes R.B., Richardson W.S. Evidence based medicine: What it is and what it isn’t. BMJ. 1996;312:71–72. doi: 10.1136/bmj.312.7023.71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Cobos-Carbó A., Augustovski F. Declaración CONSORT 2010: Actualización de la lista de comprobación para informar ensayos clínicos aleatorizados de grupos paralelos. Med. Clín. 2011;137:213–215. doi: 10.1016/j.medcli.2010.09.034. [DOI] [PubMed] [Google Scholar]
- 22.Cid-Ruzafa J., Damián-Moreno J. Valoración de la discapacidad física: El indice de Barthel. Rev. Esp. Salud Pública. 1997;71:127–137. doi: 10.1590/S1135-57271997000200004. [DOI] [PubMed] [Google Scholar]
- 23.Martínez-Martín P., Fernández-Mayoralas G., Frades-Payo B., Rojo-Pérez F., Petidier R., Rodríguez-Rodríguez V., Forjaz M.J., Prieto-Flores M.E., Pedro Cuesta J. de Validación de la Escala de Independencia Funcional. Gac. Sanit. 2009;23:49–54. doi: 10.1016/j.gaceta.2008.06.007. [DOI] [PubMed] [Google Scholar]
- 24.Sayers S.P., Jette A.M., Haley S.M., Heeren T.C., Guralnik J.M., Fielding R.A. Validation of the Late-Life Function and Disability Instrument. J. Am. Geriatr. Soc. 2004;52:1554–1559. doi: 10.1111/j.1532-5415.2004.52422.x. [DOI] [PubMed] [Google Scholar]
- 25.Graf C. The Lawton Instrumental Activities of Daily Living (IADL) Scale. 2. Med. Surg. Nurses. 2008;108:59. [PubMed] [Google Scholar]
- 26.Wrisley D.M., Marchetti G.F., Kuharsky D.K., Whitney S.L. Reliability, internal consistency, and validity of data obtained with the functional gait assessment. Phys. Ther. 2004;84:906–918. doi: 10.1093/ptj/84.10.906. [DOI] [PubMed] [Google Scholar]
- 27.Podsiadlo D., Richardson S. The timed “Up & Go”: A test of basic functional mobility for frail elderly persons. J. Am. Geriatr. Soc. 1991;39:142–148. doi: 10.1111/j.1532-5415.1991.tb01616.x. [DOI] [PubMed] [Google Scholar]
- 28.Dite W., Temple V.A. A clinical test of stepping and change of direction to identify multiple falling older adults. Arch. Phys. Med. Rehabil. 2002;83:1566–1571. doi: 10.1053/apmr.2002.35469. [DOI] [PubMed] [Google Scholar]
- 29.ATS Committee on Proficiency Standards for Clinical Pulmonary Function Laboratories ATS statement: Guidelines for the six-minute walk test. Am. J. Respir. Crit. Care Med. 2002;166:111–117. doi: 10.1164/ajrccm.166.1.at1102. [DOI] [PubMed] [Google Scholar]
- 30.Rikli R.E., Jones C.J. Development and validation of criterion-referenced clinically relevant fitness standards for maintaining physical independence in later years. Gerontologist. 2013;53:255–267. doi: 10.1093/geront/gns071. [DOI] [PubMed] [Google Scholar]
- 31.Bohannon R.W. Daily sit-to-stands performed by adults: A systematic review. J. Phys. Sci. 2015;27:939–942. doi: 10.1589/jpts.27.939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Cohen J. Statistical Power Analysis for the Behavioral Sciences. 2nd ed. L. Erlbaum Associates; Hillsdale, NJ, USA: 1988. [Google Scholar]
- 33.Daniel K. Wii-hab for pre-frail older adults. Rehabil. Nurs. 2012;37:195–201. doi: 10.1002/rnj.25. [DOI] [PubMed] [Google Scholar]
- 34.Mugueta-Aguinaga I., Garcia-Zapirain B. FRED: Exergame to Prevent Dependence and Functional Deterioration Associated with Ageing. A Pilot Three-Week Randomized Controlled Clinical Trial. Int. J. Environ. Res. Public Health. 2017;14:1439. doi: 10.3390/ijerph14121439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Orsega-Smith E., Davis J., Slavish K., Gimbutas L. Wii Fit Balance Intervention in Community-Dwelling Older Adults. Games Health J. 2012;1:431–435. doi: 10.1089/g4h.2012.0043. [DOI] [PubMed] [Google Scholar]
- 36.Portela F.R., Correia R.J.C., Fonseca J.A., Andrade J.M. Wiitherapy on seniors—Effects on physical and metal domains; Proceedings of the 2011 IEEE 1st International Conference on Serious Games and Applications for Health (SeGAH); Braga, Portugal. 16–18 November 2011; pp. 1–5. [Google Scholar]
- 37.Tollár J., Nagy F., Moizs M., Tóth B.E., Sanders L.M.J., Hortobágyi T. Diverse Exercises Similarly Reduce Older Adults’ Mobility Limitations. Med. Sci. Sports Exerc. 2019;51:1809–1816. doi: 10.1249/MSS.0000000000002001. [DOI] [PubMed] [Google Scholar]
- 38.Crotty M., Laver K., Quinn S., Ratcliffe J., George S., Whitehead C., Davies O. Is use of the Nintendo Wii Fit in physiotherapy as effective as conventional physiotherapy training for hospitalised older adults?; Proceedings of the 2011 International Conference on Virtual Rehabilitation; Zurich, Switzerland. 27–29 June 2011; pp. 1–2. [Google Scholar]
- 39.Farzin A., Ibrahim R., Madon Z., Basri H. The Efficiency of a Multicomponent Training for Prospective Memory Among Healthy Older Adults: A Single-Blind, Randomized Controlled Within-Participants Cross-Over Trial. Am. J. Phys. Med. Rehabil. 2018;97:628–635. doi: 10.1097/PHM.0000000000000931. [DOI] [PubMed] [Google Scholar]
- 40.Hughes K.J., Salmon N., Galvin R., Casey B., Clifford A.M. Interventions to improve adherence to exercise therapy for falls prevention in community-dwelling older adults: Systematic review and meta-analysis. Age Ageing. 2019;48:185–195. doi: 10.1093/ageing/afy164. [DOI] [PubMed] [Google Scholar]
- 41.Gomes G.C.V., Bacha J.M.R., do Socorro Simões M., Lin S.M., Viveiro L.A.P., Varise E.M., Filho W.J., Pompeu J.E. Feasibility, safety, acceptability, and functional outcomes of playing Nintendo Wii Fit PlusTM for frail elderly: Study protocol for a feasibility trial. Pilot Feasibility Stud. 2017;3:41. doi: 10.1186/s40814-017-0184-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Hung E.S.-W., Chen S.-C., Chang F.-C., Shiao Y., Peng C.-W., Lai C.-H. Effects of Interactive Video Game-Based Exercise on Balance in Diabetic Patients with Peripheral Neuropathy: An Open-Level, Crossover Pilot Study. Evid. Based Complement. Altern. Med. 2019;2019:4540709. doi: 10.1155/2019/4540709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Montero-Alía P., Miralles-Basseda R., López-Jiménez T., Muñoz-Ortiz L., Jiménez-González M., Prat-Rovira J., Albarrán-Sánchez J.L., Manresa-Domínguez J.M., Andreu-Concha C.M., Rodríguez-Pérez M.C., et al. Controlled trial of balance training using a video game console in community-dwelling older adults. Age Ageing. 2019;48:506–512. doi: 10.1093/ageing/afz047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Singh D.K.A., Rajaratnam B.S., Palaniswamy V., Raman V.P., Bong P.S., Pearson H. Effects of balance-focused interactive games compared to therapeutic balance classes for older women. Climacteric. 2012;16:141–146. doi: 10.3109/13697137.2012.664832. [DOI] [PubMed] [Google Scholar]
- 45.Stanmore E.K., Mavroeidi A., de Jong L.D., Skelton D.A., Sutton C.J., Benedetto V., Munford L.A., Meekes W., Bell V., Todd C. The effectiveness and cost-effectiveness of strength and balance Exergames to reduce falls risk for people aged 55 years and older in UK assisted living facilities: A multi-centre, cluster randomised controlled trial. BMC Med. 2019;17:49. doi: 10.1186/s12916-019-1278-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Morat M., Bakker J., Hammes V., Morat T., Giannouli E., Zijlstra W., Donath L. Effects of stepping exergames under stable versus unstable conditions on balance and strength in healthy community-dwelling older adults: A three-armed randomized controlled trial. Exp. Gerontol. 2019;127:110719. doi: 10.1016/j.exger.2019.110719. [DOI] [PubMed] [Google Scholar]
- 47.Schoene D., Lord S.R., Delbaere K., Severino C., Davies T.A., Smith S.T. A Randomized Controlled Pilot Study of Home-Based Step Training in Older People Using Videogame Technology. PLoS ONE. 2013;8:e57734. doi: 10.1371/journal.pone.0057734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Chao Y.-Y., Scherer Y.K., Montgomery C.A., Wu Y.-W., Lucke K.T. Physical and psychosocial effects of Wii Fit exergames use in assisted living residents: A pilot study. Clin. Nurs. Res. 2015;24:589–603. doi: 10.1177/1054773814562880. [DOI] [PubMed] [Google Scholar]
- 49.Keogh J.W.L., Power N., Wooller L., Lucas P., Whatman C. Physical and psychosocial function in residential aged-care elders: Effect of Nintendo Wii Sports games. J. Aging Phys. Act. 2014;22:235–244. doi: 10.1123/japa.2012-0272. [DOI] [PubMed] [Google Scholar]
- 50.Nicholson V.P., McKean M., Lowe J., Fawcett C., Burkett B. Six weeks of unsupervised Nintendo Wii Fit gaming is effective at improving balance in independent older adults. J. Aging Phys. Act. 2015;23:153–158. doi: 10.1123/JAPA.2013-0148. [DOI] [PubMed] [Google Scholar]
- 51.Htut T.Z.C., Hiengkaew V., Jalayondeja C., Vongsirinavarat M. Effects of physical, virtual reality-based, and brain exercise on physical, cognition, and preference in older persons: A randomized controlled trial. Eur. Rev. Aging Phys. Act. 2018;15:1–12. doi: 10.1186/s11556-018-0199-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Liao Y.-Y., Chen I.-H., Lin Y.-J., Chen Y., Hsu W.-C. Effects of Virtual Reality-Based Physical and Cognitive Training on Executive Function and Dual-Task Gait Performance in Older Adults With Mild Cognitive Impairment: A Randomized Control Trial. Front. Aging Neurosci. 2019;11:162. doi: 10.3389/fnagi.2019.00162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Pacheco T.B.F., de Medeiros C.S.P., de Oliveira V.H.B., Vieira E.R., de Cavalcanti F.A.C. Effectiveness of exergames for improving mobility and balance in older adults: A systematic review and meta-analysis. Syst. Rev. 2020;9:163. doi: 10.1186/s13643-020-01421-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Bevilacqua R., Maranesi E., Riccardi G.R., Donna V.D., Pelliccioni P., Luzi R., Lattanzio F., Pelliccioni G. Non-Immersive Virtual Reality for Rehabilitation of the Older People: A Systematic Review into Efficacy and Effectiveness. J. Clin. Med. 2019;8:1882. doi: 10.3390/jcm8111882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Tomioka K., Kurumatani N., Saeki K. The differential effects of type and frequency of social participation on IADL declines of older people. PLoS ONE. 2018;13:e0207426. doi: 10.1371/journal.pone.0207426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Hunter E.G., Kearney P.J. Occupational Therapy Interventions to Improve Performance of Instrumental Activities of Daily Living for Community-Dwelling Older Adults: A Systematic Review. Am. J. Occup. 2018;72:7204190050p1–7204190050p9. doi: 10.5014/ajot.2018.031062. [DOI] [PubMed] [Google Scholar]
- 57.Orellano E., Colón W.I., Arbesman M. Effect of occupation- and activity-based interventions on instrumental activities of daily living performance among community-dwelling older adults: A systematic review. Am. J. Occup. 2012;66:292–300. doi: 10.5014/ajot.2012.003053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.The Effects of Virtual Kayak Paddling Exercise on Postural Balance, Muscle Performance, and Cognitive Function in Older Adults with Mild Cognitive-PubMed-NCBI. [(accessed on 27 December 2019)]; doi: 10.1123/japa.2018-0020. Available online: https://www.ncbi.nlm.nih.gov/pubmed/?term=The+Effects+of+Virtual+Kayak+Paddling+Exercise+on+Postural+Balance%2C+Muscle+Performance%2C+and+Cognitive+Function+in+Older+Adults+with+Mild+Cognitive+Impairment%3A+A+Randomized+Controlled+Trial. [DOI] [PubMed]
- 59.Lee S., Shin S. Effectiveness of virtual reality using video gaming technology in elderly adults with diabetes mellitus. Diabetes Technol. Ther. 2013;15:489–496. doi: 10.1089/dia.2013.0050. [DOI] [PubMed] [Google Scholar]