Abstract
Memantine (3,5-dimethyladamantan-1-amine) is an orally active, noncompetitive N-methyl-D-aspartate receptor (NMDAR) antagonist approved for treatment of moderate-to-severe Alzheimer’s disease (AD), a neurodegenerative condition characterized by a progressive cognitive decline. Unfortunately, memantine as well as the other class of drugs licensed for AD treatment acting as acetylcholinesterase inhibitors (AChEIs), provide only symptomatic relief. Thus, the urgent need in AD drug development is for disease-modifying therapies that may require approaching targets from more than one path at once or multiple targets simultaneously. Indeed, increasing evidence suggests that the modulation of a single neurotransmitter system represents a reductive approach to face the complexity of AD. Memantine is viewed as a privileged NMDAR-directed structure, and therefore, represents the driving motif in the design of a variety of multi-target directed ligands (MTDLs). In this review, we present selected examples of small molecules recently designed as MTDLs to contrast AD, by combining in a single entity the amantadine core of memantine with the pharmacophoric features of known neuroprotectants, such as antioxidant agents, AChEIs and Aβ-aggregation inhibitors.
Keywords: memantine, Alzheimer’s disease, multi target directed ligand, hybrid structures
1. Introduction
Alzheimer’s disease (AD) is a chronic neurodegenerative condition that slowly destroys nerve cells, leading to a progressive cognitive decline. As for major chronic diseases, a pluralism of causative features is thought to be implicated, resulting in complex networks of perturbation. The mechanistic understanding of synaptic damage might offer a valuable key for developing future therapeutic strategies to tackle AD progression. In this context, excitotoxicity is emerging as a pivotal event. Caused by excessive or prolonged glutamate exposure, this pathological condition alters neurons to death.
N-methyl-D-aspartate (NMDA) receptors (NMDAR) are ionotropic glutamate receptors primarily involved in synaptic plasticity underlying learning and memory. However, they are also prime actors of excitotoxic damage occurring during chronic neurodegenerative injuries [1]. Increasing consensus indicates that functional properties of NMDAR are governed by their localization, with synaptic NMDAR (sNMDAR) contributing to cell plasticity and neurotrophic processes, while extrasynaptic NMDAR (eNMDAR) triggering apoptotic signalling pathways [2]. This effect accounts for the difficulties encountered in the design of safe and effective cures acting on NMDARs, and contemporary suggests that a selective targeting of the eNMDARs represents a promising approach to treat neurodegenerative conditions [3].
Memantine is an uncompetitive NMDAR antagonist approved to treat moderate-severe AD patients. It acts as an open-channel blocker with a relatively rapid off-rate from the channel [4]. Due to these peculiar kinetics, memantine mainly enters the channel in conditions of excessive and prolonged glutamate exposure, preferentially acting on extrasynaptic/tonically-activated NMDAR over synaptic/phasically-activated NMDAR [5,6]. This peculiar profile, which allows memantine to contrast excitotoxicity while preserving glutamatergic synaptic functioning, possibly accounts for the clinical tolerability of the drug [7]. Unfortunately, however, memantine offers only palliative benefits to patients. Possibly, the explanation for this issue might be the complex neurotransmitters dysfunction characterizing AD, which suggests the modulation of a single neurotransmitter system to be inadequate to face the disease. Increasing evidence indicates a mutual feedback connection between the glutamatergic and the cholinergic systems, which both possess strong implications in cognitive functions [8]. Furthermore, the failure of calcium homeostatic balance deriving from NMDAR overactivation as well as metal dyshomeostasis (Fe, Zn, Cu) [9,10] orchestrates several pathologic features, including oxidative damage [11,12], neuroinflammation and protein misfolding and aggregation [13,14], all contributing to the neurotoxicity mediated by excitotoxic damage. Indeed, the presence of neuritic plaques constituted mainly by insoluble Aβ-peptide (Aβ) in the brain parenchyma, is one of the hallmarks required for AD diagnosis.
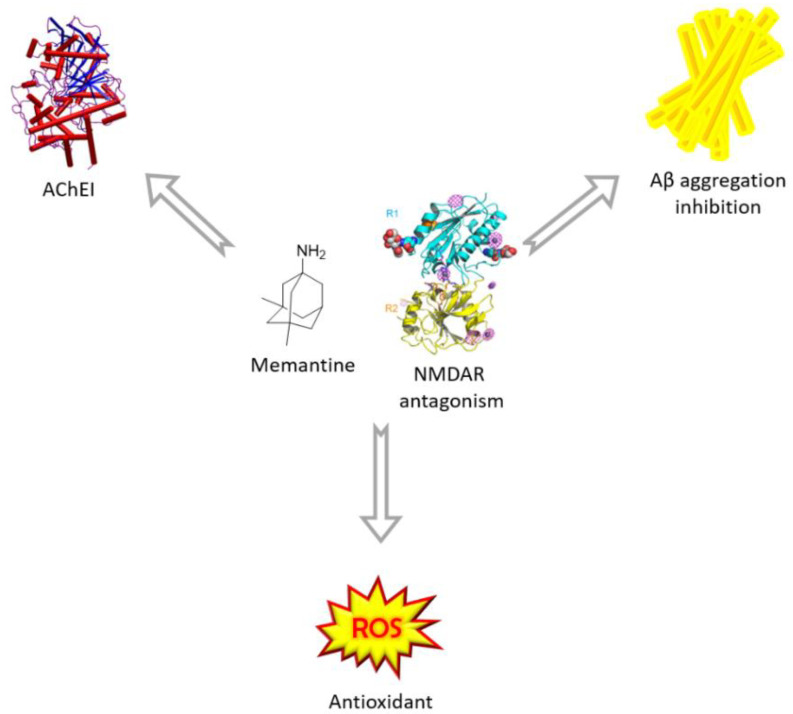
On this basis, research efforts have recently focused on the identification of therapeutic tools that could target glutamatergic hyperactivation and excitotoxicity-related mechanisms, triggering a synergistic response [15]. Thus, Multi Target Directed Ligands (MTDLs), i.e., single molecules acting on different targets simultaneously, are emerging at a rapid pace as a valuable opportunity to restore the complex interplay among multiple NMDAR-mediated alterations [16,17]. In this context, memantine is viewed as a privileged NMDAR-directed structure, and therefore, represents the driving motif in the design of a variety of multifunctional compounds. In the search for a disease-modifying drug for AD, the MTDL approach has been applied by different research groups to obtain hybrid compounds able to hit simultaneously different pathways implicated in AD [18]. In this review, we present selected examples of small molecules designed by merging in a single entity the amantadine core of memantine with the chemical features of known neuroprotectants performing through different mechanism of action, such as antioxidant and anti-aggregating activity or AChE and monoaminoxidase inhibition (Figure 1).
Figure 1.
Conjugation strategies exploiting memantine’s NMDAR antagonism to tackle AD.
2. Memantine and Cholinesterase Inhibitor Hybrids
To date, only two classes of drugs are licensed for the treatment of AD: AChEIs for mild to-moderate disease and memantine for moderate and severe disease. AChEIs prevent cholinesterase enzymes (ChEs) from degrading acetylcholine (ACh), in order to increase the synaptic concentration and the duration of action of the neurotransmitter [19].
Among the various theories that try to explain the characteristic etiopathological cascade of AD, one of the most investigated is the cholinergic hypothesis. Indeed, cholinergic loss is one of the driving impairments since the early symptoms of the disease, unavoidably leading to the characteristic cognitive decline [20]. Actually, the standard-of-care treatment for AD is the combination of cholinesterase’s inhibitors, with the aim to potentiate the cholinergic transmission, and memantine [16]. AChEIs currently used in AD therapy, such as Rivastigmine, Donepezil and Galantamine, are able to stabilize cognitive decline for 3 to 6 months, but do not halt or slow down the progression of the disease [19,21]. Also, some Donepezil-based derivatives prevent the formation of amyloid plaques, since a connection has been demonstrated between AChE activity and plaque formation [22]. Indeed, Aβ peptide interacts with the peripheric anionic site (PAS) of human AChE (hAChE), that operates as a nucleation site enhancing Aβ aggregation [23].
Moreover, throughout AD progression there is a reduction of AChE levels and an increase of those of a nonspecific cholinesterase, butyrylcholinesterase (BChE); thus, targeting the latter could result in higher therapeutic efficacy [20]. Recently, some novel compounds bearing a carbamate moiety have proved to selectively bind to BChE and to act as neuroprotectors in vivo, pointing out a potential advantage for a disease-modifying therapy [24].
Following the polypharmacological approach and the clinical relevance of both memantine and AChEIs, several MTDLs have been developed by joining memantine to pharmacophores, inhibiting ChE with the aim to synergistically and more effectively tackle the AD pathological cascade. Herein there are reported a series of these hybrids divided by their ChEI core.
2.1. Tacrine-Adamantanes Hybrids
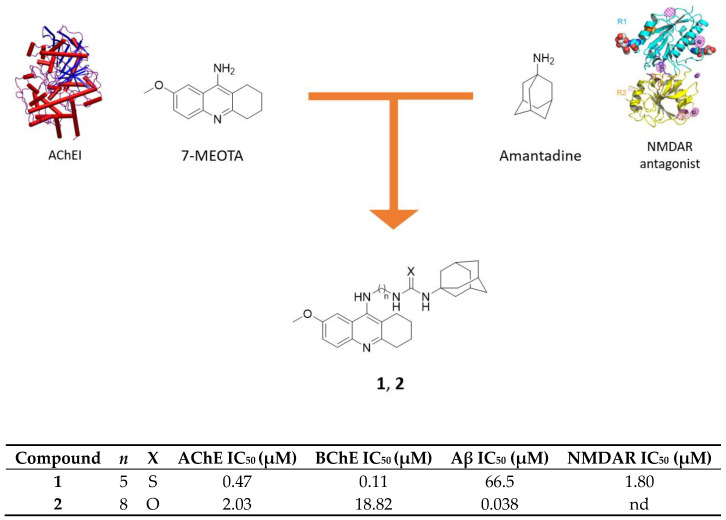
Tacrine (THA) is a non-competitive reversible AChEI active in the central nervous system (CNS) and slightly selective for BChE [25]. It was the first AChEI drug approved by FDA to combat AD, but it was withdrawn from the market due to its hepatoxicity [26]. Its derivatives 7-methoxytacrine (7-MEOTA) and 6-chlorotacrine (6-Cl-THA) are potent anti-ChE compounds with lower side effects [27,28]. An interesting strategy to obtain a multimodal profile towards ChE and NMDAR is to combine tacrine scaffold with the adamantane core through tethers of different length. In this view, hybrids of 7-MEOTA and amantadine, linked by methylene-thiourea or methylene-urea tethers, were designed and synthesized. The new compounds showed micromolar to submicromolar activities towards hAChE and human BChE (hBChE), NMDA receptor and Aβ1-40 aggregation (Figure 2) [29,30].
Figure 2.
Drug design and biological activities of 7-MEOTA-amantadine hybrids 1 and 2.
These hybrids act as competitive inhibitors of hAChE and hBChE with thioureas displaying higher selectivity for the latter; this may be beneficial, since it has been demonstrated that the levels of this enzyme increase in the course of AD (Figure 2) [20]. They have lower IC50 values for both enzymes than reference 7-MEOTA (10.50 μM for hAChE and 21 μM for hBChE), with the hybrids bearing a five-carbon linker that are the most potent in both series, suggesting that this is the optimal distance for target interaction [29,30]. Furthermore, the urea derivative 2 showed the highest inhibition of Aβ1-40 aggregation, while the thiourea 1 inhibits NMDAR with a similar IC50 value as memantine (1.80 μM vs. 1 μM) and the same efficacy as open channel blocker, but with slower kinetics, which may suggest why it preferentially binds to eNMDAR [31]. In fact, selectivity for eNMDARs is highly desirable due to their involvement in glutamate-mediated excitotoxicity and it is achieved through use-dependent inhibitors with a slow onset of action [32]. In addition to these activities, most of the compounds tested displayed weak-to-moderate activity towards BACE-1 enzyme, which, alongside inhibitory activity on Aβ1-40 aggregation previously showed, proves their potential antiamyloid properties.
Molecular modelling studies performed on compounds 1 and 2 showed how the 7-MEOTA moiety binds to the catalytic anionic site (CAS) while the amantadine core binds to the PAS of both cholinesterases. In hAChE, the 7-MEOTA scaffold creates π-π interactions within the cation-π site, while the methoxy group stabilizes the complex through hydrogen bonding. The alkyl chain contributes to stabilize the molecule-enzyme complex through the interaction of phenyl groups of amino acid residues located in the middle of the gorge, whereas the amantadine moiety establishes π-aliphatic interactions and several Van der Waals interactions at the edge of the gorge in the PAS. In the hBChE, the interactions are similar, with the nitrogen atom of the three-fused ring structure and the secondary amino group that create further hydrogen bonding. Based on the results obtained from docking studies, assumptions were made also to understand the ability of these hybrids to counteract Aβ1-40 aggregation; it was supposed that the three-ring structure of 7-MEOTA establishes π-π interactions with the hydrophobic regions of Aβ, while the adamantane cage is involved in non-aromatic interactions. Most urea derivatives studied here are superior than their thiourea counterparts in inhibiting amyloid fibrillization, probably due to the urea moiety that creates stronger hydrogen bonds.
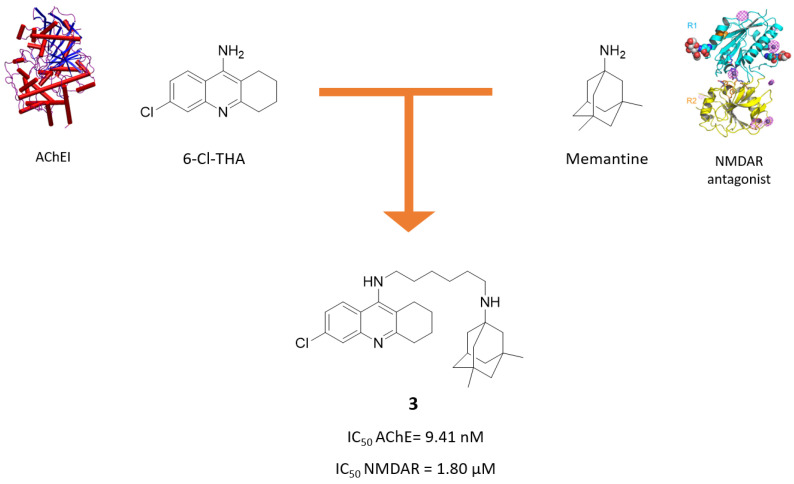
Following a similar strategy, Kaniakova, M. and coworkers designed and synthesized the 6-Cl-THA-memantine hybrid 3 (Figure 3) [33]. The esamethylene linker was chosen based on the optimal spacer previously found in a series of galantamine-memantine hybrids, which will be discussed later.
Figure 3.
Drug design and biological activities of 6-chlorotacrine-memantine hybrid 3.
Compound 3 demonstrated to act in a multimodal fashion, with a good activity towards AChE and NMDAR, as well as a higher neuroprotection ability than memantine after microinjection of NMDA into the dorsal rat hippocampus. In particular, 3 turned out to be more potent than parent compound 6-Cl-THA in inhibiting AChE (IC50 = 9.41 nM vs. 20 nM), but less potent than memantine in blocking NMDAR (IC50 = 1.80 μM vs. 0.79 μM). Like memantine, it targets the GluN1/N2B subunit, acting as an open channel blocker. Due to its promising pharmacological properties, its ability to cross the blood-brain barrier (BBB) was predicted using the PAMPA assay and its cytotoxic effect in CHO-K1 mammalian cells was assessed. Results suggest that it has a high probability of passing the BBB (Pe = 9.20 × 10−6 cm s−1), but is more cytotoxic than 6-Cl-THA (IC50 = 5.93 μM vs. 70.7 μM).
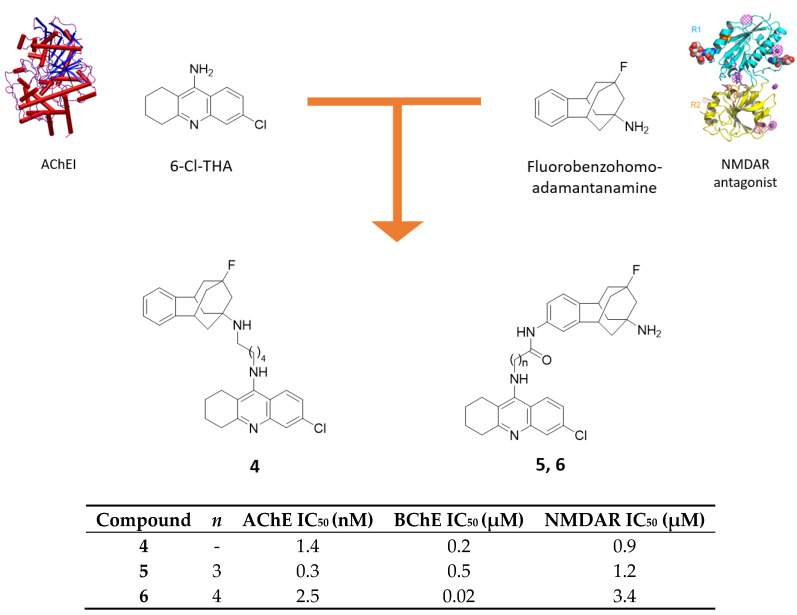
Beside adamantylamine scaffold, its benzofused analogs have been extensively studied as NMDAR antagonists, with fluorobenzohomoadamantanamine being more potent than memantine and amantadine [34]. Due to its promising activity, Perez-Areales and coworkers combined this scaffold with 6-Cl-THA moiety through different linker lengths and in different linkage position to evaluate the potential pharmacological value of hybrids formed in this way (Figure 4) [35].
Figure 4.
Drug design and biological activities of 6-chlorotacrine-benzohomoadamantane hybrids 4–6.
The resulting hybrids are better inhibitors of hAChE than 6-Cl-THA (IC50 = 0.3–2.5 nM vs. 14.5 nM). In particular, with a primary amino group attached to the adamantane moiety, the activity is augmented, with compound 5 being the most potent; the importance of the unsubstituted amino group is prominent in the inhibition of hBChE, for which hybrid 6 has the lowest IC50 value. However, only few of the tested hybrids turned out to be more potent than 6-Cl-THA (0.5 μM) in inhibiting hBChE.
Compounds 4 and 5 resulted as the most potent against NMDARs. Unlike in memantine, where the methylation of the amino group leads to a reduced activity, here the monomethylation of the bridgehead amino group in the polycyclic scaffold is tolerated and both compounds are about 2-fold more potent than benzohomoadamantanamine (IC50 = 0.9 and 1.2 μM vs. 1.9 μM). Particularly, in nitrogen-connected series, the hybrid with the longer linker has the best activity, while in the benzo-attached series, the opposite pattern is observed. Apart from the discussed targets, the compounds showed negligible inhibitory efficacy on BACE-1 enzyme and on Aβ42 and tau aggregation. Finally, PAMPA assay for brain permeation predictions was carried out with the results showing a more efficient BBB permeation for derivatives bearing a substituted amino group in the benzofused core (4), probably due to their higher lipophilicity. These studies show that hybrid molecules bearing an aminoadamantane moiety bound to THA or one of its derivatives exert their action in various pathways involved in AD in low-micromolar or nanomolar ranges [35]. In many cases, the spacer plays an important role in modulating the activity: the proper spacers’ length and nature is fundamental to the optimal interaction of pharmacophores to their respective binding sites.
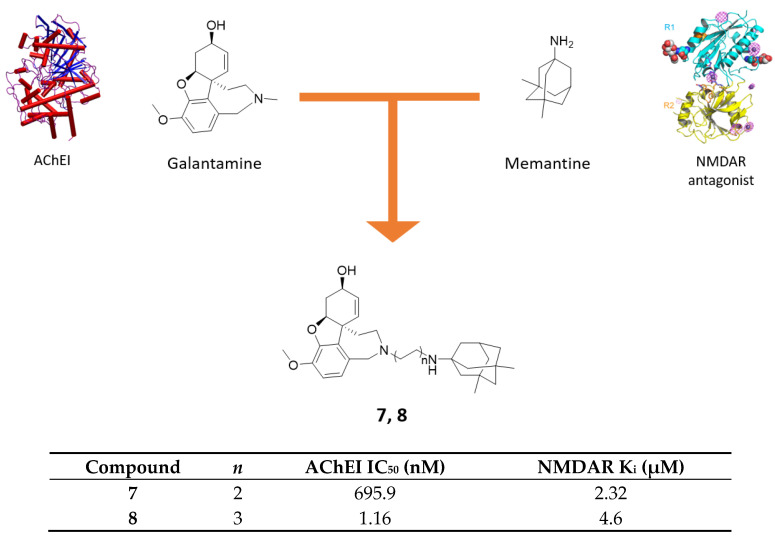
2.2. Galantamine-Memantine Hybrids
Galantamine is an alkaloid-derived AChEI approved since 2001 for the treatment of mild-to-moderate forms of AD. Furthermore, galantamine associates AChEI efficacy to potentiation of NMDAR transmission mediated by protein kinase C (PKC) and to the ability of allosterically modulated α-subunit of nicotinic receptors [36,37]. Particularly, through the modulation of α7-nAChR on presynaptic glutamatergic neurons, it can enhance the beneficial effect of NMDAR’s synaptic activation, potentiating at the same time memantine’s neuroprotective effect [38]. These premises were further assessed in an in vitro validation assay where inactive dose of memantine and galantamine produced full neuroprotective efficacy, confirming promising experimental efficacy of their combination therapy [39]. In this context, after a computationally-driven SAR campaign, a series of galantamine-memantine conjugates, connected through the nitrogen atom of both, were developed, demonstrating to exert both NMDAR antagonism and AChE inhibition with high and well-balanced potencies [40]. It is important to note that for AChE inhibition, it is fundamental to identify the proper linker length between the two moieties, allowing interaction both to AChE’s CAS and PAS. In fact, 4-methylene linker of 7 prevented it from properly interacting with the PAS (identified with Trp286), thereby reducing its affinity when compared to derivatives with longer alkyl chains (e.g., 8, Figure 5). Concurrently, for NMDAR antagonism, alkyl substituents on memantine’s nitrogen are allowed. In terms of AChEI activity, different lengths of the alkyl linker or N-methyl substitutions on memantine moiety are well tolerated, whereas spacer with heteroatoms and switching amine function of memantine into amide greatly affected AChEI profile. Regarding NMDAR, only alkyl or alkylamino linkers were allowed, whereas all other modifications were detrimental for NMDAR affinity.
Figure 5.
Drug design and biological activities of memantine-galantamine hybrids 7 and 8.
Derivative 8 stood out as the best of the series regarding the AChEI/NMDAR profile as well as efficient NR2B binder (NMDAR with 2B subunit, peculiar of eNMDARs involved in glutamatergic overexcitation) and valid neuroprotective agent after insult by NMDA in SHSY-5Y cells (IC50 = 0.28 nM, Figure 5) [40]. Compound 7 was selected for further in vivo biological evaluation as a result of best compromise between well-balanced pharmacological potencies and physico-chemical properties (Figure 5) [41]. Due to a suboptimal pharmacokinetic profile, it was tested intracerebroventricularly in AD mouse model through osmotic minipump. After 7 days treatment at 7.5 µg/day, compound 7 was able to completely revert the induced neurotoxicity in vivo in terms of behavioral readouts (e.g., neuroprotective effect for short-term memory) and biochemical analysis (e.g., strong reduction of all neurodegenerative-related, apoptotic and synaptic plasticity biomarker) [41]. More recently, preliminary in vivo studies were conducted with compound 7 by transdermal iontophoresis delivery, looking to maintain the same pharmacological effects with a more patient-friendly administration. For now, compound 7 has proved to be delivered consistently to the brain through iontophoresis but further preclinical studies and pharmacokinetic-pharmacodynamic optimization are needed to prove its biological effects with this new innovative delivery system [42].
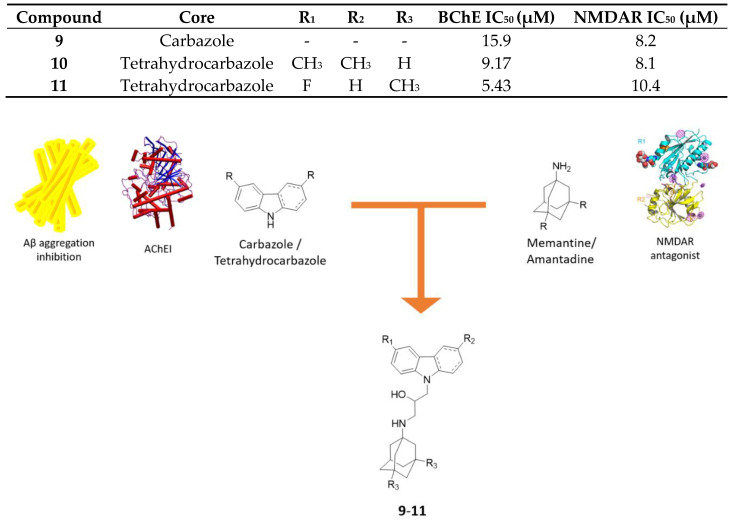
2.3. Aminoadamantane-Carbazole/Tetrahydrocarbazole Hybrids
It has been reported that some carbazole derivatives are potential AD-modifying compounds, i.e., N-alkyl carbazoles are able to favor the formation of soluble form of Aβ, through different mechanisms [43] and are also able to block apoptosis, thus exerting a neuroprotective effect [44]. Moreover, recent studies suggested that some carbazole-based compounds are valuable anti-AD drug candidates, since they are able to inhibit both AChE and BChE activity [45] as well as AChE- and self-induced Aβ aggregation [46]. These findings support the rationale to develop novel hybrids with a multimodal profile by adding to biological properties of the carbazole core the neuroprotection derived by the memantine nucleus.
Hybrids of aminoadamantanes with carbazole and tetrahydrocarbazole (Figure 6) were synthesized and tested as inhibitors of hAChE and equine serum BChE, as antagonists of NMDARs and as stimulators of microtubule assembly [47]. In AD, microtubule structure disturbance and tubulin polymerization suppression are signs of the incoming neurodegeneration that lead to failures in the axonal transport; therefore, it is necessary to develop compounds that are able to stabilize microtubule structure and to enhance tubulin assembly [47,48].
Figure 6.
Drug design and biological activities of carbazole/tetrahydrocarbazole-aminoadamantane hybrids 9–11.
All the hybrids act as weak inhibitors of hAChE but are more potent and more selective for BChE and their inhibition activity is generally higher than reference carbazole (IC50 = 5–20 µM vs. >20 µM). The substitution of a carbazole moiety with a tetrahydrocarbazole fragment leads to an enhanced inhibition for BChE, while minimal differences between memantine and amantadine moiety have been observed. Overall, the highest inhibition activity for BChE is showed by compound 11 with a fluorinated tetrahydrocarbazole core. At the same time these compounds were tested as antagonists of NMDA receptors, and their ability to bind to the intrachannel (or MK-801 binding) site, present in all NMDARs, and/or to the allosteric (or ifenprodil-binding) site of NR2B-containing NMDARs, was assessed. The NR2B subunit is of particular interest because its blockade is beneficial for neuroprotection and Aβ-induced neuronal disruption [49].
In the carbazole series, compounds show different activities towards the allosteric site, and this feature depends primarily on the substitution patterns of the carbazole moiety: Indeed, compound 9 with no substituents is the most active. However, in the tetrahydrocarbazole series, this trend is not observed, in fact all the compounds are differently active towards both binding sites, except for compound 10, which is selective towards the allosteric site of the NR2B subunit and also exhibits the most balanced multimodal profile. These heterodimers have substantially lower IC50 values than memantine and amantadine.
In both series, neither memantine moiety nor amantadine one seems important to stimulate tubulin polymerization, while the insertion of a chlorine or a bromine in the carbazole causes a reduction of this stimulating effect. Furthermore, the introduction of a fluorine in the tetrahydrocarbazole core and the unsubstitution of the carbazole one considerably enhances this effect, hence the most active compounds are the fluorinated tetrahydrocarbazole-memantine conjugate and the carbazole-memantine derivative. The fluorine-containing tetrahydrocarbazole hybrids reveal a high neuroprotection profile: Indeed, they are able to reduce the Ca2+-induced swelling of mitochondria and thus inhibit the mitochondria permeability transition (MPT), which is a key process in cell death, either in physiological conditions or in neurotoxicity models.
The same compounds were also evaluated and tested as hydrochlorides with compound 10 that showed the lowest IC50 value for the ifenprodil site [50]. Along with this, their effects were studied on the membrane potential of mitochondria, on the Ca2+ ion-caused depolarization and swelling of mitochondria, both indicating MPT. These novel compounds depolarize the membrane, indicating that they are toxic; however, exceptions can be made for compounds containing a fluorine as R substituent, which causes just a slight depolarization potential and shows a dose-dependent-inhibiting effect on Ca2+ ion-induced mitochondrial swelling, thus increasing mitochondrial stability and being assessed as potential neuroprotectors [50]. Following evaluation of the activity and selectivity of these compounds, molecular docking studies were performed, in order to shed light on the binding poses. It was reported that memantine and amantadine lay in the cavity located at the active site gorge of BChE, and their positions were very stable, while the ones of the linker and of the carbazole moiety changed. These compounds have a chiral centre, but the binding poses of the two enantiomers are very similar, with the hydroxyl groups that establish hydrogen bonds with different amino acid residues depending on the R or S isomer. Taking into account the position of the entire ligand, it was highlighted that it does not vary when amantadine is replaced by memantine, and a similar behavior is observed with the switch from carbazole to tetrahydrocarbazole; however, when a halogen substituent is inserted, the carbazole core undergoes a flip to reduce the steric strain [47].
These studies demonstrate that also carbazoles linked to memantine are able to maintain important NMDAR-blocking activities while adding interesting neuroprotection effects through tackling several pathological pathways involved in AD.
3. Memantine-Antioxidant Hybrids to Explore Neuroinflammation
In light of the above described multifaced nature of AD, the multitarget approach could help to elucidate insights in the complex pathogenetic network triggering pathologic conditions. Beside glutamate-driven excitotoxicity, oxidative stress, misfolded proteins and neuroinflammation are only some of the actors which, playing in liaison, define AD-impaired neuroenvironment. Particularly, prolonged eNMDAR activation leads to increasing cytoplasmic Ca2+ concentration and the onset of oxidative damage, which can in turn pull the trigger of aberrant misfolded protein cascade (e.g., amyloid plaques formation) [11]. Amyloid plaques are one of the classical trademarks of AD, characterized by Aβ42 deposition, which originates from the sequential cleavage of APP by β- and γ-secretases rather than the non-amyloidogenic and physiologic α-secretase cleavage. In concert, Aβ deposition triggered by excitotoxicity-leading oxidative stress can exacerbate oxidative damage in an etiopathogenetic loop, which involves microglia activation and the following neuroinflammatory conditions [14,51].
Based on these premises, linking memantine with bioactive payload able to tackle Aβ/ROS/neuroinflammation could be a promising pathway to deepen knowledge in NMDAR-mediated neurotoxic events in AD.
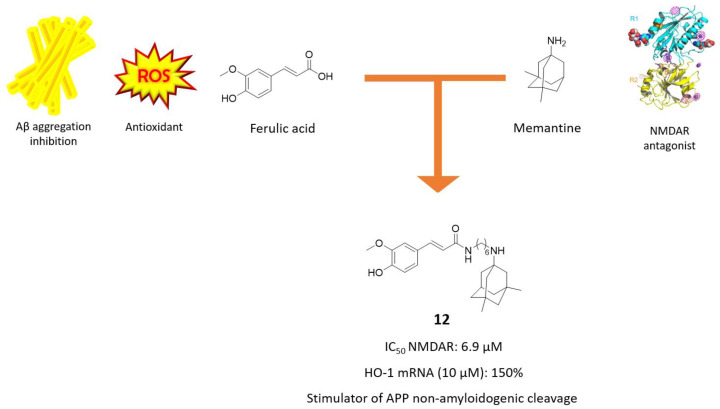
3.1. Memantine-Ferulic Acid Hybrids
Recently, Rosini and coworkers developed a series of hybrids between memantine and ferulic acid (FA), envisioned by the concurrent ability to reduce Aβ-induced neurotoxicity and oxidative stress of this latter [52,53]. The best derivatives of the series are those directly linked at the carboxylic function of FA and nitrogen atom of memantine through alkyl chain of different lengths, which were initially screened for their NMDAR antagonism efficacy. Derivative 12 came out as the most promising NMDAR-blocking agent, with potency only 3-fold less than memantine (IC50 = 6.9 µM vs. 2.3 µM, Figure 7), sharing with the parent compound the same open channel blocking mechanism and the binding site midway through the channel pore. Compound 12 exerted interesting antioxidant efficacy, both directly as radical scavenger and indirectly through activation of Nrf2-ARE pathway. Interestingly, differently from memantine and FA alone, it was also able to stimulate the non-amyloidogenic pathway and consequently limiting Aβ production at 10 µM concentration [53]. This new balanced memantine-hybrid, acting at a different level of AD pathological cascade, could be a starting point for further evaluation in more complex AD models, to deepen our findings in NMDAR-guided oxidative damage.
Figure 7.
Drug design and biological activities of ferulic acid-memantine hybrid 12.
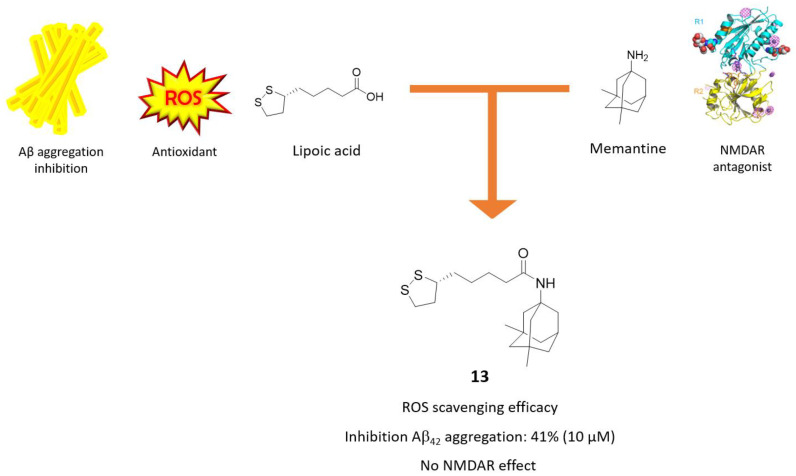
3.2. Memantine-Glutathione/Lipoic Acid Hybrids
The possibility of connecting antioxidant agents with the memantine core has also been explored [53,54] using radical scavengers such as glutathione (GSH) and (R)-α-Lipoic Acid (LA). They are endogenous molecules capable of removing free radicals that accumulate in cells, thus maintaining ROS balance at physiological levels and preventing oxidative stress and cell damage [55,56]. Furthermore, LA has been shown to mitigate Aβ aggregation and to protect from Aβ-mediated citotoxicity in vitro [57]. In light of these findings, Sozio, P. and coworkers developed conjugates of memantine linked to GSH and LA through an amide bond and tested them as NMDAR antagonists, Aβ aggregation inhibitors and as radical scavengers, pointing out compound 13 as the best derivative (Figure 8) [58].
Figure 8.
Drug design and biological activities of lipoic acid-memantine hybrid 13.
The antioxidant properties of compound 13 were assessed in GL15 cell line upon the addition of hydrogen peroxide (H2O2) and superoxide radical anion (O2−); compared to LA, it showed a similar antioxidant activity towards H2O2, while a slightly lower one was shown towards O2−. In addition, compound 13 displayed Aβ antiaggregating properties (41% at 10 µM).
In order to investigate the effects of these conjugates on NMDAR, the authors used an in vitro protocol evaluating the release of [3H]Noradrenaline ([3H]NA) modulated by presynaptic NMDAR from rat hippocampal synaptosomes. Compound 13 turned out to be inactive as NMDAR ligand. This is consistent with previous SAR studies on memantine, which reported a loss of NMDAR activity upon conversion of the free adamantane’s amine group into amide group [40].
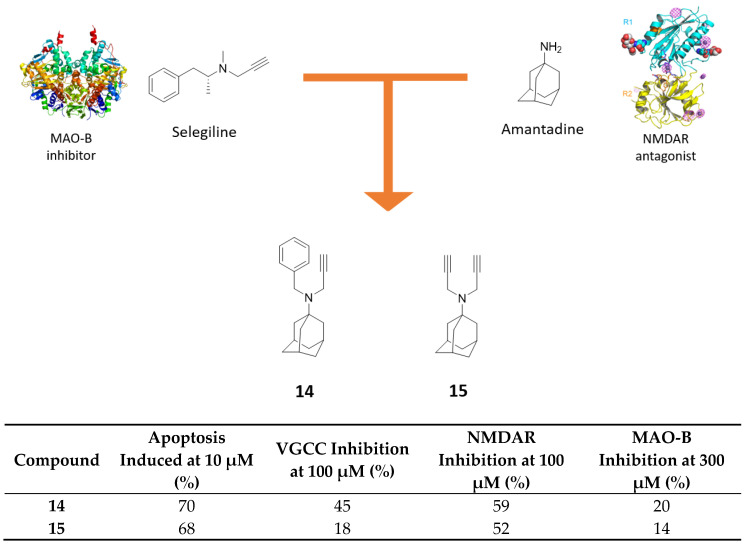
3.3. Amantadine-Propargylamine Hybrids
Monoamine oxidase B (MAO-B) with monoamine oxidase A (MAO-A) belong to flavoenzyme family bound to outer mitochondrial membrane. They exert a pivotal role in neurotransmission, regulating neurotransmitter metabolism and cellular redox balance. Particularly, MAO-B has been gaining particular interest in recent years due to its overexpression in neuroinflammatory condition and the consequential ROS overproduction and neurotransmitters impairment [59,60]. Accordingly, development of MAO-B inhibitors seems to be an interesting strategy to deepen our knowledge on diseases characterized by neuroinflammatory conditions, like AD and Parkinson disease (PD) [59].
In 2014, Malan and coworkers developed a series of polycyclic propargylamine or acetylene derivatives with the aim to synergistically limit apoptotic processes and excitotoxicity, due to aberrant intracellular Ca2+ concentration and oxidative damage deriving from increasing MAO-B activity in AD. Polycyclic cores, such as memantine and amantadine, are established Ca2+ channel blockers, acting on NMDAR, while bigger polycyclic nucleus exert their effect, modulating L-type calcium channels [61]. In parallel, propargylamine moiety is the responsible fragment of MAO-B irreversible inhibition in compounds like selegiline, a drug used for the treatment of PD. Amantadine-propargylamine hybrids 14 and 15, bearing respectively one or two propargyl functions directly connected to the nitrogen atom, demonstrated anti-apoptotic activity similar to selegiline (Figure 9) [62]. Compound 14 exhibited the best L-type voltage-gated calcium channels (VGCC) inhibitory activity (45% at 100 μM), whereas with compound 15 there was a drop of activity (18% at 100 μM), demonstrating the importance of N-benzyl substitution for target recognition. Both compounds maintained mild NMDAR inhibitory activity (52% for 15 and 59% for 14 at 100 μM) thanks to the presence of an amantadine core. Unfortunately, none of them exerted acceptable MAO-B inhibitory potency at 300 μM. These derivatives confirm the ability of memantine/amantadine scaffold to partially maintain NMDAR inhibitory activity, also in N-substituted derivatives (e.g., as previously seen in ferulic and galantamine hybrids), whereas it does not seem a good starting scaffold to reach satisfactory MAO-B inhibition.
Figure 9.
Drug design and biological activities of propargyl-amantadine hybrids 14 and 15.
4. Miscellaneous Memantine Derivatives
In this section, we review studies reported in the recent chemical and biological literature on the miscellaneous memantine derivatives for which AD neuroprotective activity derived by merging two pharmacophores is claimed, but which lie outside the hybrid series described in the other paragraphs of this review. In this regard, a lot of efforts have been made over the years to enhance memantine potency, synthesizing double-acting prodrug or targeting the second region of the same receptor to increase its efficacy [6,63]. Otherwise, merging two well-known NMDAR antagonists has been exploited as a strategy to obtain more efficient channel blockers with potential further clinical applications [64]. Furthermore, linking memantine to a purinergic receptor blocker has been pursued as a new approach to investigate other pathways involved in AD [65].
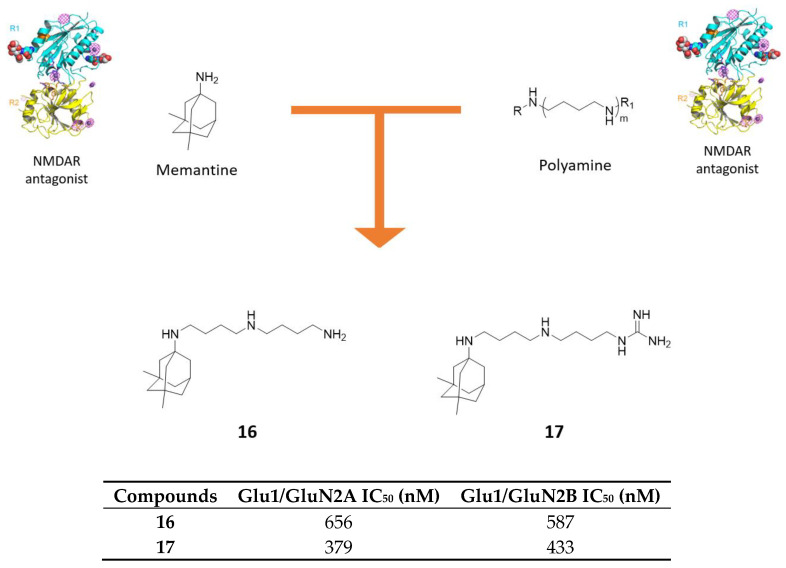
4.1. Memantine-Polyamine Conjugates
Kumamoto, T. and coworkers developed a series of memantine-polyamine conjugates showing very potent NMDAR antagonism, higher than memantine [64]. The rationale is based on the well-known potent blocking NMDAR activity of the polyamine backbone, that the same authors have already conjugated with polycyclic scaffolds, developing compounds endowed with proved strong reversible and voltage-dependent NMDA blocking activity [66,67,68]. These derivatives were further explored and optimized, merging polyamine moiety with memantine scaffold (Figure 10). The triamine 16 and guanidino-diamine 17 demonstrated the highest inhibitory activities against GluN1/N2A and GluN1/N2B NMDAR (Figure 10). Particularly, compound 17 exhibited IC50 3-fold lower against both receptors when compared with parent compound memantine (IC50 = 379 nM and 433 nM vs. 1376 nM and 2099 nM, respectively) [64].
Figure 10.
Drug design and biological activities of polyamine-memantine hybrids 16 and 17.
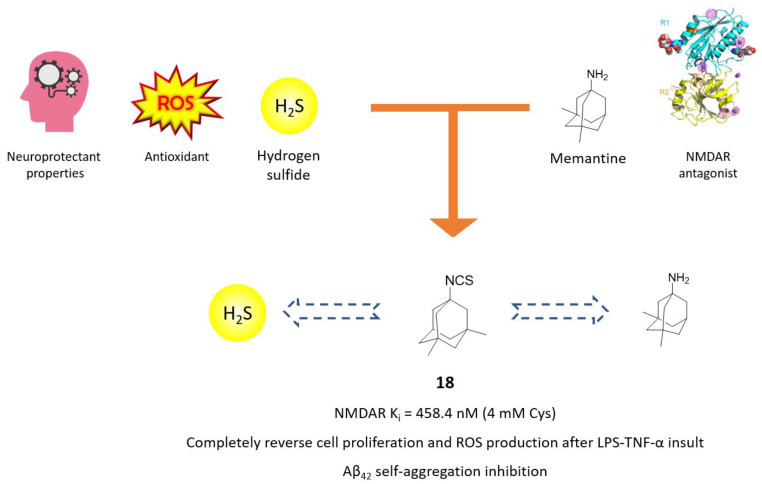
4.2. H2S-Releasing Memantine Prodrug
In recent years, the possibility of linking moieties releasing endogenous gaseous signalling molecules, i.e., gasotransmitters, with a well-known pharmacophore, has assumed particular interest in multitarget drug design [69,70]. Gasotransmitters, such as carbon monoxide (CO), nitric oxide (NO) and hydrogen sulfyde (H2S), are endogenously produced by enzymes and play important roles as antioxidants, neuromodulators and antinflammatory agents [71]. Particularly, H2S combines neuroprotection, antinflammatory and antiapoptotic activities to NMDAR-modulation ability both directly, with sulfhydration of critical cysteine residues, and indirectly, through regulation of intracellular calcium concentration [72,73]. On this basis, the interesting biological outputs of compound 18, an H2S-releasing memantine derivative by Sestito and coworkers, can open a range of possibilities for new MTDL campaign [63]. Compound 18 bears an isothiocyanate moiety as H2S-donating moiety, replacing the characteristic free amino group of memantine (Figure 11). First of all, compound 18 showed to maintain memantine’s NMDAR inhibition (Ki = 458 vs. 329 nM) only in the presence of 4 mM L-cysteine, which can mediate H2S release and memantine’s unveiling. Amperometric analysis on derivative 18 demonstrated a prolonged and persisting cysteine-mediated H2S releasing. Furthermore, compound 18 was able to protect cells from oxidative stress and LPS-TNFα insult, reducing ROS production and stimulating cell proliferation in neuroinflammation in an in vitro model at 10 μM (Figure 11). Antiamyloidogenic properties of memantine were confirmed with compound 18, which demonstrated to reduce Aβ42 self-induced aggregation and to reduce Aβ-induced damage in rat microglia cells to roughly the same extent as its parent compound [63].
Figure 11.
Drug design and biological activities of memantine prodrug 18.
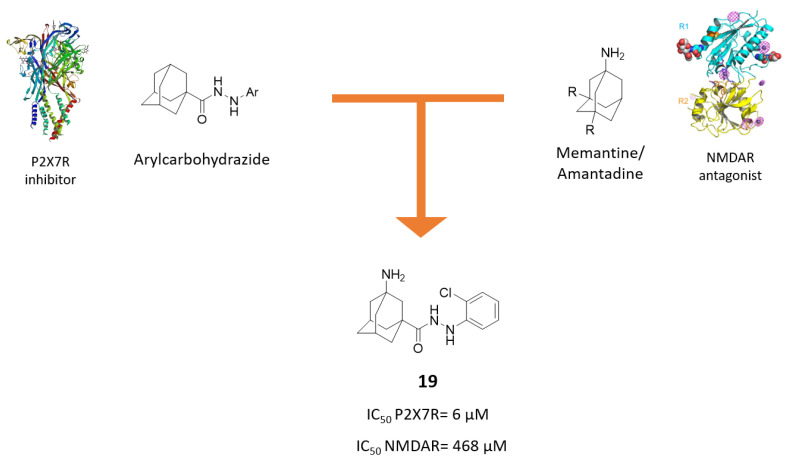
4.3. Dual P2X7-NMDA Receptor Antagonists
P2X7 receptor (P2X7R) is an ATP-sensitive ion channel, present in the CNS (astrocytes, oligodendrocytes and microglia), where it mediates K+ efflux and Ca2+/Na+ influx [74,75]. In physiological conditions, it exerts a neuroprotective effect, i.e., the activation of the cAMP response element-binding (CREB), which inhibits the transcription of genes involved in the microglial inflammatory response [76] and the stimulation of α-secretase, which is responsible for the non-amyloidogenic cleavage of the amyloid precursor protein (APP), with the formation of soluble and non-toxic sAPPα [77].
In the presence of high ATP levels, like in AD, microglial P2X7Rs are upregulated, giving rise to an inflammatory cascade, where IL-1β, INF-γ, TNF-α, and other cytokines are released, and this contributes to the progression of the disease [74,78,79]. Furthermore, P2X7Rs release glutamate [80], which activates NMDARs [81]. A research conducted on AD mouse model reported that the in vivo P2X7R inhibition reduced the levels of Aβ, thus showing a neuroprotective effect. However, the effects of P2X7R inhibition in pathological conditions are still poorly understood and need further investigation [78].
Based on these premises, new P2X7R-NMDAR antagonists were developed based on an amantadine or memantine moiety bound to a N’-arylcarbohydrazide core, which is correlated to strong P2X7R antagonism (Figure 12) [65].
Figure 12.
Drug design and biological activities of N’-arylcarbohydrazide-aminoadamantane hybrid 19.
Compound 19 bearing a o-chloro phenyl ring showed the highest inhibitory activity towards P2X7R, but lower blocker activity towards NMDAR compared to amantadine. Hence, following the encouraging P2X7 inhibition, structural modifications were made to improve NMDAR antagonism by replacing the amantadine core of compound 19 with a memantine moiety. However, the resulting hybrids were not able to significantly inhibit NMDARs and also showed higher IC50 values for P2X7R than compound 19.
The study demonstrates that these molecules could potentially slow down neuroinflammation by preventing the P2X7R-induced inflammatory cascade. Even if they effectively bind to the P2X7R, they did not show an improved activity for NMDAR compared to memantine.
5. Conclusions and Future Perspectives
Although AD current pharmacotherapy is founded on cholinergic and glutamatergic hypotheses, the drugs licensed for AD treatment acting as AChEIs or as NMDAR antagonist (memantine) provide only symptomatic and temporary support. In recent years, the research of new therapeutic agents has been mainly centred on the amyloidogenic hypothesis and based on the multifactorial nature of AD. The assumption that intractable neurodegenerative diseases like AD are caused by more than one interacting mechanism has driven many research groups in designing and synthesising small molecules by merging two or more distinct pharmacophores with different biological properties. In this context, memantine represents a privileged structure in the design of a variety of multifunctional compounds to be developed as new AD therapeutic agents. In this review, we have reported the more recent studies relative to the molecular hybridization of memantine or its amantadine nucleus with the chemical features of AChEI (tacrine and galantamine), on the basis of the close interplay between the glutamatergic and the cholinergic systems in disease process, and with MAO inhibitor (propargylamine) and neuroprotectant (ferulic and lipoic acid, and carbazole) scaffolds with the aim to halt the etiopathogenetic loop of neuroinflammation involving glutamatergic excitotoxicity, oxidative stress and protein aggregation. The biological profile of the new molecules, in some cases very promising, highlights the great challenge for medicinal chemists in finding disease-modifying agents with balanced activities towards the different targets involved in AD. Several issues remain to be addressed to translate AD multitarget approaches into effective drug candidates against AD, mainly a better comprehension of disease processes and a higher predictive validity of animal models.
Author Contributions
G.M. collected articles, organized and wrote the review; F.B. collected articles and contributed in writing the review; M.R. contributed in writing and editing the draft; A.M. conceived, wrote and supervised the preparation of the review. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by Italian Ministry of University and Research (MIUR), PRIN 2017 (2017MT3993_007).
Conflicts of Interest
The authors declare no conflict of interest.
References
- 1.Parsons M.P., Raymond L.A. Extrasynaptic NMDA receptor involvement in central nervous system disorders. Neuron. 2014;82:279–293. doi: 10.1016/j.neuron.2014.03.030. [DOI] [PubMed] [Google Scholar]
- 2.Léveillé F., El Gaamouch F., Gouix E., Lecocq M., Lobner D., Nicole O., Buisson A. Neuronal viability is controlled by a functional relation between synaptic and extrasynaptic NMDA receptors. FASEB J. 2008;22:4258–4271. doi: 10.1096/fj.08-107268. [DOI] [PubMed] [Google Scholar]
- 3.Folch J., Busquets O., Ettcheto M., Sánchez-López E., Castro-Torres R.D., Verdaguer E., Garcia M.L., Olloquequi J., Casadesús G., Beas-Zarate C., et al. Memantine for the Treatment of Dementia: A Review on its Current and Future Applications. J. Alzheimer’s Dis. 2018;62:1223–1240. doi: 10.3233/JAD-170672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Xia P., Chen H.S., Zhang D., Lipton S.A. Memantine preferentially blocks extrasynaptic over synaptic NMDA receptor currents in hippocampal autapses. J. Neurosci. 2010;30:11246–11250. doi: 10.1523/JNEUROSCI.2488-10.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lipton S.A. Pathologically activated therapeutics for neuroprotection. Nat. Rev. Neurosci. 2007;8:803–808. doi: 10.1038/nrn2229. [DOI] [PubMed] [Google Scholar]
- 6.Takahashi H., Xia P., Cui J., Talantova M., Bodhinathan K., Li W., Saleem S., Holland E.A., Tong G., Piña-Crespo J., et al. Pharmacologically targeted NMDA receptor antagonism by NitroMemantine for cerebrovascular disease. Sci. Rep. 2015;5:14781. doi: 10.1038/srep14781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lipton S.A. Paradigm shift in neuroprotection by NMDA receptor blockade: Memantine and beyond. Nat. Rev. Drug Discov. 2006;5:160–170. doi: 10.1038/nrd1958. [DOI] [PubMed] [Google Scholar]
- 8.Parsons C.G., Danysz W., Dekundy A., Pulte I. Memantine and cholinesterase inhibitors: Complementary mechanisms in the treatment of Alzheimer’s disease. Neurotox. Res. 2013;24:358–369. doi: 10.1007/s12640-013-9398-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Barnham K.J., Bush A.I. Biological metals and metal-targeting compounds in major neurodegenerative diseases. Chem. Soc. Rev. 2014;43:6727–6749. doi: 10.1039/C4CS00138A. [DOI] [PubMed] [Google Scholar]
- 10.Santos M.A., Chand K., Chaves S. Recent progress in multifunctional metal chelators as potential drugs for Alzheimer’s disease. Coord. Chem. Rev. 2016;327–328:287–303. doi: 10.1016/j.ccr.2016.04.013. [DOI] [Google Scholar]
- 11.Lipton S. NMDA receptor activity regulates transcription of antioxidant pathways. Nat. Neurosci. 2008;11:381–382. doi: 10.1038/nn0408-381. [DOI] [PubMed] [Google Scholar]
- 12.Nakamura T., Lipton S.A. Preventing Ca2+-mediated nitrosative stress in neurodegenerative diseases: Possible pharmacological strategies. Cell Calcium. 2010;47:190–197. doi: 10.1016/j.ceca.2009.12.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kodis E.J., Choi S., Swanson E., Ferreira G., Bloom G.S. N-methyl-D-aspartate receptor-mediated calcium influx connects amyloid-β oligomers to ectopic neuronal cell cycle reentry in Alzheimer’s disease. Alzheimer’s Dement. 2018;14:1302–1312. doi: 10.1016/j.jalz.2018.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Tu S., Okamoto S., Lipton S.A., Xu H. Oligomeric Aβ-induced synaptic dysfunction in Alzheimer’s disease. Mol. Neurodegener. 2014;9:48. doi: 10.1186/1750-1326-9-48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Banks W.A. A Spectrum of Topics for 2019: Advances in Neuroinflammation, Oxidative Stress, Obesity, Diabetes Mellitus, Cardiovascular Disease, Autism, Exosomes, and Central Nervous System Diseases. Curr. Pharm. Des. 2020;26:1–5. doi: 10.2174/138161282601200225102049. [DOI] [PubMed] [Google Scholar]
- 16.Rosini M., Simoni E., Minarini A., Melchiorre C. Multi-target design strategies in the context of Alzheimer’s disease: Acetylcholinesterase inhibition and NMDA receptor antagonism as the driving forces. Neurochem. Res. 2014;39:1914–1923. doi: 10.1007/s11064-014-1250-1. [DOI] [PubMed] [Google Scholar]
- 17.Rosini M., Simoni E., Caporaso R., Minarini A. Multitarget strategies in Alzheimer’s disease: Benefits and challenges on the road to therapeutics. Future Med. Chem. 2016;8:697–711. doi: 10.4155/fmc-2016-0003. [DOI] [PubMed] [Google Scholar]
- 18.Rosini M. Polypharmacology: The rise of multitarget drugs over combination therapies. Future Med. Chem. 2014;6:485–487. doi: 10.4155/fmc.14.25. [DOI] [PubMed] [Google Scholar]
- 19.Colović M.B., Krstić D.Z., Lazarević-Pašti T.D., Bondžić A.M., Vasić V.M. Acetylcholinesterase inhibitors: Pharmacology and toxicology. Curr. Neuropharmacol. 2013;11:315–335. doi: 10.2174/1570159X11311030006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Li Q., Yang H., Chen Y., Sun H. Recent progress in the identification of selective butyrylcholinesterase inhibitors for Alzheimer’s disease. Eur. J. Med. Chem. 2017;132:294–309. doi: 10.1016/j.ejmech.2017.03.062. [DOI] [PubMed] [Google Scholar]
- 21.Korabecny J., Spilovska K., Mezeiova E., Benek O., Juza R., Kaping D., Soukup O. A Systematic Review on Donepezil-based Derivatives as Potential Cholinesterase Inhibitors for Alzheimers Disease. Curr. Med. Chem. 2019;26:5625–5648. doi: 10.2174/0929867325666180517094023. [DOI] [PubMed] [Google Scholar]
- 22.Li Q., He S., Chen Y., Feng F., Qu W., Sun H. Donepezil-based multi-functional cholinesterase inhibitors for treatment of Alzheimer’s disease. Eur. J. Med. Chem. 2018;158:463–477. doi: 10.1016/j.ejmech.2018.09.031. [DOI] [PubMed] [Google Scholar]
- 23.Lushchekina S.V., Kots E.D., Novichkova D.A., Petrov K.A., Masson P. Role of Acetylcholinesterase in beta-amyloid Aggregation Studied by Accelerated Molecular Dynamics. BioNanoScience. 2017;7:396–402. doi: 10.1007/s12668-016-0375-x. [DOI] [Google Scholar]
- 24.Hoffmann M., Stiller C., Endres E., Scheiner M., Gunesch S., Sotriffer C., Maurice T., Decker M. Highly Selective Butyrylcholinesterase Inhibitors with Tunable Duration of Action by Chemical Modification of Transferable Carbamate Units Exhibit Pronounced Neuroprotective Effect in an Alzheimer’s Disease Mouse Model. J. Med. Chem. 2019;62:9116–9140. doi: 10.1021/acs.jmedchem.9b01012. [DOI] [PubMed] [Google Scholar]
- 25.Horak M., Holubova K., Nepovimova E., Krusek J., Kaniakova M., Korabecny J., Vyklicky L., Kuca K., Stuchlik A., Ricny J., et al. The pharmacology of tacrine at N-methyl-d-aspartate receptors. Prog. Neuropsychopharmacol. Biol. Psychiatry. 2017;75:54–62. doi: 10.1016/j.pnpbp.2017.01.003. [DOI] [PubMed] [Google Scholar]
- 26.Romero A., Cacabelos R., Oset-Gasque M.J., Samadi A., Marco-Contelles J. Novel tacrine-related drugs as potential candidates for the treatment of Alzheimer’s Disease. Bioorg. Med. Chem. Lett. 2013;23:1916–1922. doi: 10.1016/j.bmcl.2013.02.017. [DOI] [PubMed] [Google Scholar]
- 27.Gancar M., Ho K., Mohid S.A., Thai N.Q., Bednarikova Z., Nguyen H.L., Bhunia A., Nepovimova E., Li M.S., Gazova Z. 7-Methoxytacrine and 2-Aminobenzothiazole Heterodimers: Structure-Mechanism Relationship of Amyloid Inhibitors Based on Rational Design. ACS Chem. Neurosci. 2020;11:715–729. doi: 10.1021/acschemneuro.9b00419. [DOI] [PubMed] [Google Scholar]
- 28.Misik J., Nepovimova E., Pejchal J., Kassa J., Korabecny J., Soukup O. Cholinesterase Inhibitor 6-Chlorotacrine—In Vivo Toxicological Profile and Behavioural Effects. Curr. Alzheimer Res. 2018;15:552–560. doi: 10.2174/1567205015666171212105412. [DOI] [PubMed] [Google Scholar]
- 29.Spilovska K., Korabecny J., Kral J., Horova A., Musilek K., Soukup O., Drtinova L., Gazova Z., Siposova K., Kuca K. 7-Methoxytacrine-adamantylamine heterodimers as cholinesterase inhibitors in Alzheimer’s disease treatment--synthesis, biological evaluation and molecular modeling studies. Molecules. 2013;18:2397–2418. doi: 10.3390/molecules18022397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Spilovska K., Korabecny J., Horova A., Musilek K., Nepovimova E., Drtinova L., Gazova Z., Siposova K., Dolezal R., Jun D., et al. Design, synthesis and in vitro testing of 7-methoxytacrine-amantadine analogues: A novel cholinesterase inhibitors for the treatment of Alzheimer’s disease. Med. Chem. Res. 2015;24:2645–2655. doi: 10.1007/s00044-015-1316-x. [DOI] [Google Scholar]
- 31.Gazova Z., Soukup O., Sepsova V., Siposova K., Drtinova L., Jost P., Spilovska K., Korabecny J., Nepovimova E., Fedunova D., et al. Multi-target-directed therapeutic potential of 7-methoxytacrine-adamantylamine heterodimers in the Alzheimer’s disease treatment. Biochim. Biophys. Acta Mol. Basis Dis. 2017;1863:607–619. doi: 10.1016/j.bbadis.2016.11.020. [DOI] [PubMed] [Google Scholar]
- 32.Vyklicky V., Smejkalova T., Krausova B., Balik A., Korinek M., Borovska J., Horak M., Chvojkova M., Kleteckova L., Vales K., et al. Preferential Inhibition of Tonically over Phasically Activated NMDA Receptors by Pregnane Derivatives. J. Neurosci. 2016;36:2161–2175. doi: 10.1523/JNEUROSCI.3181-15.2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kaniakova M., Nepovimova E., Kleteckova L., Skrenkova K., Holubova K., Chrienova Z., Hepnarova V., Kucera T., Kobrlova T., Vales K., et al. Combination of Memantine and 6-Chlorotacrine as Novel Multi-Target Compound against Alzheimer’s Disease. Curr. Alzheimer Res. 2019;16:821–833. doi: 10.2174/1567205016666190228122218. [DOI] [PubMed] [Google Scholar]
- 34.Valverde E., Sureda F.X., Vázquez S. Novel benzopolycyclic amines with NMDA receptor antagonist activity. Bioorg. Med. Chem. 2014;22:2678–2683. doi: 10.1016/j.bmc.2014.03.025. [DOI] [PubMed] [Google Scholar]
- 35.Pérez-Areales F.J., Turcu A.L., Barniol-Xicota M., Pont C., Pivetta D., Espargaró A., Bartolini M., De Simone A., Andrisano V., Pérez B., et al. A novel class of multitarget anti-Alzheimer benzohomoadamantane‒chlorotacrine hybrids modulating cholinesterases and glutamate NMDA receptors. Eur. J. Med. Chem. 2019;180:613–626. doi: 10.1016/j.ejmech.2019.07.051. [DOI] [PubMed] [Google Scholar]
- 36.Santos M.D., Alkondon M., Pereira E.F., Aracava Y., Eisenberg H.M., Maelicke A., Albuquerque E.X. The nicotinic allosteric potentiating ligand galantamine facilitates synaptic transmission in the mammalian central nervous system. Mol. Pharmacol. 2002;61:1222–1234. doi: 10.1124/mol.61.5.1222. [DOI] [PubMed] [Google Scholar]
- 37.Moriguchi S., Marszalec W., Zhao X., Yeh J.Z., Narahashi T. Mechanism of action of galantamine on N-methyl-D-aspartate receptors in rat cortical neurons. J. Pharmacol. Exp. Ther. 2004;310:933–942. doi: 10.1124/jpet.104.067603. [DOI] [PubMed] [Google Scholar]
- 38.McGehee D.S., Heath M.J., Gelber S., Devay P., Role L.W. Nicotine enhancement of fast excitatory synaptic transmission in CNS by presynaptic receptors. Science. 1995;269:1692–1696. doi: 10.1126/science.7569895. [DOI] [PubMed] [Google Scholar]
- 39.Lopes J.P., Tarozzo G., Reggiani A., Piomelli D., Cavalli A. Galantamine potentiates the neuroprotective effect of memantine against NMDA-induced excitotoxicity. Brain Behav. 2013;3:67–74. doi: 10.1002/brb3.118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Simoni E., Daniele S., Bottegoni G., Pizzirani D., Trincavelli M.L., Goldoni L., Tarozzo G., Reggiani A., Martini C., Piomelli D., et al. Combining galantamine and memantine in multitargeted, new chemical entities potentially useful in Alzheimer’s disease. J. Med. Chem. 2012;55:9708–9721. doi: 10.1021/jm3009458. [DOI] [PubMed] [Google Scholar]
- 41.Reggiani A.M., Simoni E., Caporaso R., Meunier J., Keller E., Maurice T., Minarini A., Rosini M., Cavalli A. In Vivo Characterization of ARN14140, a Memantine/Galantamine-Based Multi-Target Compound for Alzheimer’s Disease. Sci. Rep. 2016;6:33172. doi: 10.1038/srep33172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Singhal M., Merino V., Rosini M., Cavalli A., Kalia Y.N. Controlled Iontophoretic Delivery in vitro and in vivo of ARN14140—A Multitarget Compound for Alzheimer’s Disease. Mol. Pharm. 2019;16:3460–3468. doi: 10.1021/acs.molpharmaceut.9b00252. [DOI] [PubMed] [Google Scholar]
- 43.Saturnino C., Iacopetta D., Sinicropi M.S., Rosano C., Caruso A., Caporale A., Marra N., Marengo B., Pronzato M.A., Parisi O.I., et al. N-alkyl carbazole derivatives as new tools for Alzheimer’s disease: Preliminary studies. Molecules. 2014;19:9307–9317. doi: 10.3390/molecules19079307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Pieper A.A., McKnight S.L., Ready J.M. P7C3 and an unbiased approach to drug discovery for neurodegenerative diseases. Chem. Soc. Rev. 2014;43:6716–6726. doi: 10.1039/C3CS60448A. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Choubdar N., Golshani M., Jalili-Baleh L., Nadri H., Küçükkilinç T.T., Ayazgök B., Moradi A., Moghadam F.H., Abdolahi Z., Ameri A., et al. New classes of carbazoles as potential multi-functional anti-Alzheimer’s agents. Bioorg. Chem. 2019;91:103164. doi: 10.1016/j.bioorg.2019.103164. [DOI] [PubMed] [Google Scholar]
- 46.Ghobadian R., Nadri H., Moradi A., Bukhari S.N.A., Mahdavi M., Asadi M., Akbarzadeh T., Khaleghzadeh-Ahangar H., Sharifzadeh M., Amini M. Design, synthesis, and biological evaluation of selective and potent Carbazole-based butyrylcholinesterase inhibitors. Bioorg. Med. Chem. 2018;26:4952–4962. doi: 10.1016/j.bmc.2018.08.035. [DOI] [PubMed] [Google Scholar]
- 47.Bachurin S.O., Shevtsova E.F., Makhaeva G.F., Grigoriev V.V., Boltneva N.P., Kovaleva N.V., Lushchekina S.V., Shevtsov P.N., Neganova M.E., Redkozubova O.M., et al. Novel conjugates of aminoadamantanes with carbazole derivatives as potential multitarget agents for AD treatment. Sci. Rep. 2017;7:45627. doi: 10.1038/srep45627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Ballatore C., Brunden K.R., Huryn D.M., Trojanowski J.Q., Lee V.M., Smith A.B. Microtubule stabilizing agents as potential treatment for Alzheimer’s disease and related neurodegenerative tauopathies. J. Med. Chem. 2012;55:8979–8996. doi: 10.1021/jm301079z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Zhang Y., Li P., Feng J., Wu M. Dysfunction of NMDA receptors in Alzheimer’s disease. Neurol. Sci. 2016;37:1039–1047. doi: 10.1007/s10072-016-2546-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Sokolov V.B., Aksinenko A.Y., Goreva T.V., Epishina T.A., Grigor’ev V.V., Gabrel’yan A.V., Vinogradova D.V., Neganova M.E., Shevtsova E.F., Bachurin S.O. Molecular design of multitarget neuroprotectors 3. Synthesis and bioactivity of tetrahydrocarbazole-aminoadamantane conjugates. Russ. Chem. Bull. 2016;65:1354–1359. doi: 10.1007/s11172-016-1461-5. [DOI] [Google Scholar]
- 51.Von Bernhardi R., Eugenín-von Bernhardi L., Eugenín J. Microglial cell dysregulation in brain aging and neurodegeneration. Front. Aging Neurosci. 2015;7:124. doi: 10.3389/fnagi.2015.00124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Benchekroun M., Romero A., Egea J., León R., Michalska P., Buendía I., Jimeno M.L., Jun D., Janockova J., Sepsova V., et al. The Antioxidant Additive Approach for Alzheimer’s Disease Therapy: New Ferulic (Lipoic) Acid Plus Melatonin Modified Tacrines as Cholinesterases Inhibitors, Direct Antioxidants, and Nuclear Factor (Erythroid-Derived 2)-Like 2 Activators. J. Med. Chem. 2016;59:9967–9973. doi: 10.1021/acs.jmedchem.6b01178. [DOI] [PubMed] [Google Scholar]
- 53.Rosini M., Simoni E., Caporaso R., Basagni F., Catanzaro M., Abu I.F., Fagiani F., Fusco F., Masuzzo S., Albani D., et al. Merging memantine and ferulic acid to probe connections between NMDA receptors, oxidative stress and amyloid-β peptide in Alzheimer’s disease. Eur. J. Med. Chem. 2019;180:111–120. doi: 10.1016/j.ejmech.2019.07.011. [DOI] [PubMed] [Google Scholar]
- 54.Jalili-Baleh L., Forootanfar H., Küçükkılınç T.T., Nadri H., Abdolahi Z., Ameri A., Jafari M., Ayazgok B., Baeeri M., Rahimifard M., et al. Design, synthesis and evaluation of novel multi-target-directed ligands for treatment of Alzheimer’s disease based on coumarin and lipoic acid scaffolds. Eur. J. Med. Chem. 2018;152:600–614. doi: 10.1016/j.ejmech.2018.04.058. [DOI] [PubMed] [Google Scholar]
- 55.Bansal A., Simon M.C. Glutathione metabolism in cancer progression and treatment resistance. J. Cell Biol. 2018;217:2291–2298. doi: 10.1083/jcb.201804161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Tibullo D., Li Volti G., Giallongo C., Grasso S., Tomassoni D., Anfuso C.D., Lupo G., Amenta F., Avola R., Bramanti V. Biochemical and clinical relevance of alpha lipoic acid: Antioxidant and anti-inflammatory activity, molecular pathways and therapeutic potential. Inflamm. Res. 2017;66:947–959. doi: 10.1007/s00011-017-1079-6. [DOI] [PubMed] [Google Scholar]
- 57.Ono K., Hirohata M., Yamada M. Alpha-lipoic acid exhibits anti-amyloidogenicity for beta-amyloid fibrils in vitro. Biochem. Biophys. Res. Commun. 2006;341:1046–1052. doi: 10.1016/j.bbrc.2006.01.063. [DOI] [PubMed] [Google Scholar]
- 58.Sozio P., Cerasa L.S., Laserra S., Cacciatore I., Cornacchia C., Di Filippo E.S., Fulle S., Fontana A., Di Crescenzo A., Grilli M., et al. Memantine-sulfur containing antioxidant conjugates as potential prodrugs to improve the treatment of Alzheimer’s disease. Eur. J. Pharm. Sci. 2013;49:187–198. doi: 10.1016/j.ejps.2013.02.013. [DOI] [PubMed] [Google Scholar]
- 59.Edmonson D.E., Binda C. Monoamine Oxidases. In: Harris J.R., Boekema E.J., editors. Membrane Protein Complexes: Structure and Function. Springer Nature; Singapore: 2018. pp. 117–140. [Google Scholar]
- 60.Schedin-Weiss S., Inoue M., Hromadkova L., Teranishi Y., Yamamoto N.G., Wiehager B., Bogdanovic N., Winblad B., Sandebring-Matton A., Frykman S., et al. Monoamine oxidase B is elevated in Alzheimer disease neurons, is associated with γ-secretase and regulates neuronal amyloid β-peptide levels. Alzheimers Res. Ther. 2017;9:57. doi: 10.1186/s13195-017-0279-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Joubert J., Geldenhuys W.J., Van der Schyf C.J., Oliver D.W., Kruger H.G., Govender T., Malan S.F. Polycyclic cage structures as lipophilic scaffolds for neuroactive drugs. ChemMedChem. 2012;7:375–384. doi: 10.1002/cmdc.201100559. [DOI] [PubMed] [Google Scholar]
- 62.Zindo F.T., Barber Q.R., Joubert J., Bergh J.J., Petzer J.P., Malan S.F. Polycyclic propargylamine and acetylene derivatives as multifunctional neuroprotective agents. Eur. J. Med. Chem. 2014;80:122–134. doi: 10.1016/j.ejmech.2014.04.039. [DOI] [PubMed] [Google Scholar]
- 63.Sestito S., Daniele S., Pietrobono D., Citi V., Bellusci L., Chiellini G., Calderone V., Martini C., Rapposelli S. Memantine prodrug as a new agent for Alzheimer’s Disease. Sci. Rep. 2019;9:4612. doi: 10.1038/s41598-019-40925-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Kumamoto T., Nakajima M., Uga R., Ihayazaka N., Kashihara H., Katakawa K., Ishikawa T., Saiki R., Nishimura K., Igarashi K. Design, synthesis, and evaluation of polyamine-memantine hybrids as NMDA channel blockers. Bioorg. Med. Chem. 2018;26:603–608. doi: 10.1016/j.bmc.2017.12.021. [DOI] [PubMed] [Google Scholar]
- 65.Karoutzou O., Kwak S.H., Lee S.D., Martínez-Falguera D., Sureda F.X., Vázquez S., Kim Y.C., Barniol-Xicota M. Towards a Novel Class of Multitarget-Directed Ligands: Dual P2X7-NMDA Receptor Antagonists. Molecules. 2018;23:230. doi: 10.3390/molecules23010230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Jin L., Sugiyama H., Takigawa M., Katagiri D., Tomitori H., Nishimura K., Kaur N., Phanstiel O., Kitajima M., Takayama H., et al. Comparative studies of anthraquinone- and anthracene-tetraamines as blockers of N-methyl-D-aspartate receptors. J. Pharmacol. Exp. Ther. 2007;320:47–55. doi: 10.1124/jpet.106.110528. [DOI] [PubMed] [Google Scholar]
- 67.Takayama H., Yaegashi Y., Kitajima M., Han X., Nishimura K., Okuyama S., Igarashi K. Design, synthesis, and biological evaluation of tricyclic heterocycle-tetraamine conjugates as potent NMDA channel blockers. Bioorg. Med. Chem. Lett. 2007;17:4729–4732. doi: 10.1016/j.bmcl.2007.06.069. [DOI] [PubMed] [Google Scholar]
- 68.Saiki R., Yoshizawa Y., Minarini A., Milelli A., Marchetti C., Tumiatti V., Toida T., Kashiwagi K., Igarashi K. In vitro and in vivo evaluation of polymethylene tetraamine derivatives as NMDA receptor channel blockers. Bioorg. Med. Chem. Lett. 2013;23:3901–3904. doi: 10.1016/j.bmcl.2013.04.063. [DOI] [PubMed] [Google Scholar]
- 69.Sestito S., Nesi G., Pi R., Macchia M., Rapposelli S. Hydrogen Sulfide: A Worthwhile Tool in the Design of New Multitarget Drugs. Front. Chem. 2017;5:72. doi: 10.3389/fchem.2017.00072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Basagni F., Lanni C., Minarini A., Rosini M. Lights and shadows of electrophile signaling: Focus on the Nrf2-Keap1 pathway. Future Med. Chem. 2019;11:707–721. doi: 10.4155/fmc-2018-0423. [DOI] [PubMed] [Google Scholar]
- 71.Shefa U., Yeo S.G., Kim M.S., Song I.O., Jung J., Jeong N.Y., Huh Y. Role of Gasotransmitters in Oxidative Stresses, Neuroinflammation, and Neuronal Repair. Biomed. Res. Int. 2017;2017:1689341. doi: 10.1155/2017/1689341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Kimura H. Physiological role of hydrogen sulfide and polysulfide in the central nervous system. Neurochem. Int. 2013;63:492–497. doi: 10.1016/j.neuint.2013.09.003. [DOI] [PubMed] [Google Scholar]
- 73.Nagai Y., Tsugane M., Oka J., Kimura H. Hydrogen sulfide induces calcium waves in astrocytes. FASEB J. 2004;18:557–559. doi: 10.1096/fj.03-1052fje. [DOI] [PubMed] [Google Scholar]
- 74.Cieślak M., Wojtczak A. Role of purinergic receptors in the Alzheimer’s disease. Purinergic Signal. 2018;14:331–344. doi: 10.1007/s11302-018-9629-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Deussing J.M., Arzt E. P2X7 Receptor: A Potential Therapeutic Target for Depression? Trends Mol. Med. 2018;24:736–747. doi: 10.1016/j.molmed.2018.07.005. [DOI] [PubMed] [Google Scholar]
- 76.Kopp R., Krautloher A., Ramírez-Fernández A., Nicke A. P2X7 Interactions and Signaling—Making Head or Tail of It. Front. Mol. Neurosci. 2019;12:183. doi: 10.3389/fnmol.2019.00183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Erb L., Woods L.T., Khalafalla M.G., Weisman G.A. Purinergic signaling in Alzheimer’s disease. Brain Res. Bull. 2019;151:25–37. doi: 10.1016/j.brainresbull.2018.10.014. [DOI] [PubMed] [Google Scholar]
- 78.Martin E., Amar M., Dalle C., Youssef I., Boucher C., Le Duigou C., Brückner M., Prigent A., Sazdovitch V., Halle A., et al. New role of P2X7 receptor in an Alzheimer’s disease mouse model. Mol. Psychiatry. 2019;24:108–125. doi: 10.1038/s41380-018-0108-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Illes P., Rubini P., Ulrich H., Zhao Y., Tang Y. Regulation of Microglial Functions by Purinergic Mechanisms in the Healthy and Diseased CNS. Cells. 2020;9:1108. doi: 10.3390/cells9051108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Burnstock G. Purinergic signalling and disorders of the central nervous system. Nat. Rev. Drug Discov. 2008;7:575–590. doi: 10.1038/nrd2605. [DOI] [PubMed] [Google Scholar]
- 81.Gao P., Ding X., Khan T.M., Rong W., Franke H., Illes P. P2X7 receptor-sensitivity of astrocytes and neurons in the substantia gelatinosa of organotypic spinal cord slices of the mouse depends on the length of the culture period. Neuroscience. 2017;349:195–207. doi: 10.1016/j.neuroscience.2017.02.030. [DOI] [PubMed] [Google Scholar]