Abstract
Background
There is increasing concern about the time people spend in sedentary behaviour, including screen time, leisure and occupational sitting. The number of both primary research studies (published trials) and reviews has been growing rapidly in this research area. A summary of the highest level of evidence that provides a broader quantitative synthesis of diverse types of interventions is needed. This research is to articulate the evidence of efficacy of sedentary behaviour interventions to inform interventions to reduce sitting time. The umbrella review, therefore, synthesised systematic reviews that conducted meta-analyses of interventions aiming at reducing sedentary behaviour outcomes across all age group and settings.
Method
A systematic search was conducted on six databases (MEDLINE Complete, PsycINFO, CINAHL, Global Health via EBSCOhost platform, EMBASE, and Cochrane Central Register of Systematic Reviews). Included articles were systematic reviews with meta-analysis of interventions aiming at reducing sedentary behaviour (screen time, sitting time or sedentary time) in the general population across all age group.
Results
Seventeen reviews met the inclusion criteria (7 in children and adolescent, 10 in adults). All reviews of sedentary behaviour interventions in children and adolescents investigated intervention effectiveness in reducing screen time. Six out of 11 meta-analyses (reported in 7 reviews) showed small but significant changes in viewing time. All reviews of sedentary behaviour interventions in office workplaces indicated substantial reduction in occupational sitting time (range: 39.6 to 100 min per 8-h workday). Sub-group analyses reported a trend favouring environmental change components such as sit-stand desks, active permissive workstations etc. Meta-analyses indicated that sedentary behaviour interventions were superior to physical activity alone interventions or combined physical activity and sedentary behaviour interventions in reducing sitting time.
Conclusion
The current systematic reviews and meta-analyses supported sedentary behaviour interventions for reducing occupational sitting time in particular, with small changes seen in screen time in children and adolescents. Future research should explore approaches to maintaining behaviour change beyond the intervention period and investigate the potential of sedentary behaviour reduction interventions in older age groups in non-occupational settings.
Keywords: Systematic review, Sedentary behaviour, Effectiveness, Sitting time, Screen time, Sedentary time
Background
Sedentary behaviour (SB), defined as any posture (sitting, reclining or lying) characterised by an energy expenditure ≤1.5 metabolic equivalents of task (MET) while waking [1], is observed in all domains including behaviours at work or school, at home, during transport, and in leisure-time. Examples are watching television, playing board games, driving or sitting whilst travelling, sitting or lying down, whilst reading, or sitting at work (desk-based computer) [2]. Of particular importance is the evidence of a steady increase in sedentary occupations research, which has emerged over the last few decades [3]. Specifically, evidence from developed countries (using accelerometers) indicates that sedentary time ranges between 55% and 70% of adult waking hours [4], with an average sedentary time of ≥9 h per day [5]. Children aged 2–4-years spend on average almost 1.5 h per day on sedentary activities such as watching TV/DVDs or playing electronic games, while 5–17 years spend over 2.25 h per day [6]. Both age groups had higher levels of SB than recommended by Australian guidelines [7]. The recommendation to limit sedentary recreational screen time to no more than 2 h per day in children and adolescents is consistent across guidelines [8, 9]. However, in adults, there are no recommendations for maximum daily SB time or the frequency of sitting breaks [9, 10].
There is strong evidence that high amounts of SB increase the risk for all-cause [10–12] and cardiovascular disease (CVD) mortality [10, 12] and incident CVD [10] and type 2 diabetes (T2D) in adults [10, 12]. Furthermore, moderate evidence indicates that SB is associated with incident endometrial, colon and lung cancer [10, 13]. The hazardous effects of SB are more pronounced in physically inactive people [10, 14]. In children, longer duration and higher frequencies of screen time negatively impact on body composition, cardiometabolic risk, behaviour, fitness and self-esteem [15].
The problem of too much sitting has been increasingly recognised through public health guidelines that now incorporate explicitly, yet rather broad, messages around SB [8–10]. Given the high exposure to SB and the negative impacts on population health, research in this area has gained prominence over the last 10 years [16], leading to the conduct of intervention studies targeting reductions in SB in different contexts and diverse population groups. As a consequence, a number of systematic reviews have been published in recent years to quantify the impact of SB interventions on measures of sitting time, with most predominantly focusing on workplace interventions and some community-based interventions.
Decision-makers and policymakers are increasingly favouring approaches of summarising the ‘totality’ of the evidence on effectiveness to inform practice and guidelines. In relation to SB, a review of systematic reviews, as a result, would be valuable in providing a high level of synthesised evidence to inform decision-makers about intervention effectiveness. To our knowledge, only one review of systematic reviews has been conducted to date to evaluate the effectiveness behaviour change interventions designed to reduce SB due to TV watching and/or media use in children and adolescents [17]. That umbrella review suggested future research should evaluate interventions targeting other types of SB and other population age groups (e.g. adults), as well as the effectiveness of different behaviour change techniques across different settings [17]. This umbrella review sets out to investigate the efficacy of interventions in reducing SB in healthy populations across all age groups. To contrast and compare the effectiveness of intervention components or strategies (quantified by effect size), a review of systematic reviews that included meta-analysis was conducted.
The aim of this umbrella review (a review of reviews that conducted meta-analyses) was to (a) assess the effectiveness of SB interventions on measures of overall sitting time, occupational sitting time and screen time; (b) examine the effectiveness of specific intervention components; and (c) identify whether there is a research gap in terms of the potential types of interventions targeting SB.
Method
This review adheres to the guidelines in the PRISMA statement 2009 [18] in combination with Joanna Briggs Institute (JBI) guidelines for umbrella reviews [19]. The protocol was registered with PROSPERO: International Prospective Register of Systematic Review Protocols (registration number CRD42020150458).
Search strategies and databases
A literature search for potentially eligible publications was conducted by the first author (PN) in collaboration with an experienced librarian and the review team. The data search was conducted on 29th August 2019 using six bibliographic databases: MEDLINE Complete, PsycINFO, CINAHL, Global Health via EBSCOhost platform, EMBASE and Cochrane Central Register of Systematic Reviews. Search strategies were developed based on three concepts: SB, intervention and study type. The following search terms were modified to reflect subject headings control (or medical subject heading - MeSH terms) that fit individual database searches (details in Additional file 1).
(“sedentary behavio*” OR “sedentary lifestyle*” OR “sedentary time” OR “sedentary activit*” OR “sedentary leisure” OR sitting OR “seated posture” OR “screen time” OR “computer time” OR ((watch* OR view*) N2 (tv OR television)) OR inactive*) AND (effect* OR efficac* OR evaluat* OR intervention* OR program* OR compar*) AND (“systematic review” OR meta-analys* OR meta-analytic* OR “quantitative analys*”)
Inclusion and exclusion criteria
The umbrella review sought to identify all reviews of studies that examined the effects of interventions that aimed to reduce SB and reported behaviour outcomes, e.g. sedentary time, sitting time and sedentary screen time across the age spectrum. Reviews of weight loss or physical activity (PA) interventions that also aimed to reduce sedentary time by incorporating a SB reduction component and reported SB outcomes were included. For inclusion, studies were required to be (a) a systematic review that included a meta-analysis; (b) a review that included randomised controlled trials (RCTs), with or without other types of studies. Whilst there was no restriction placed on the participants’ gender and age groups, studies were limited to the general population, i.e. reviews that included trials targeting specific health conditions such as CVD, T2D etc. were thus excluded. However, reviews of SB interventions for the general population that did not exclude people with specific conditions were included. The search was limited to human studies reported in English with no date restriction.
Identification of relevant studies and data extraction
All citations were imported into Endnote and duplicates were removed using both the Endnote function and manually. Reviews were selected by (a) screening of title and abstract; (b) full-text screening independently by three review authors (PN, LL and DN) using Rayyan web-app for systematic reviews [20]. Discrepancies resulting from the screening were resolved based on consensus amongst the review team.
Overlap of primary research studies in each of the included reviews was identified by comparing the list of included primary studies in each review.
For reviews that met the inclusion criteria, data extraction and quality assessment were conducted independently by two team members (PN and LL, PN and DN). Extracted information included the characteristics of the reviews (databases, number of included trials, search date and range of publication year); sample (total size, age); characteristics of primary studies (type of study, setting, country); intervention description (components, control, SB measurement) and intervention effectiveness results (as reduction in time spent in SB, e.g. sitting time, screen time, total SB time). The primary outcome of interest of this umbrella review was the intervention effect size (post-intervention change-from-baseline difference between intervention and control group) reported in the quantitative analyses.
Quality assessment
Bias and quality of the included systematic reviews and meta-analyses were assessed using A Measurement Tool to Assess Systematic Reviews (AMSTAR) [21]. This tool consists of 16 items that assess both methodological quality and reporting quality. The overall rating of high, moderate, low and critically low, is based on weaknesses or flaws in ten critical domains [21, 22].
Results
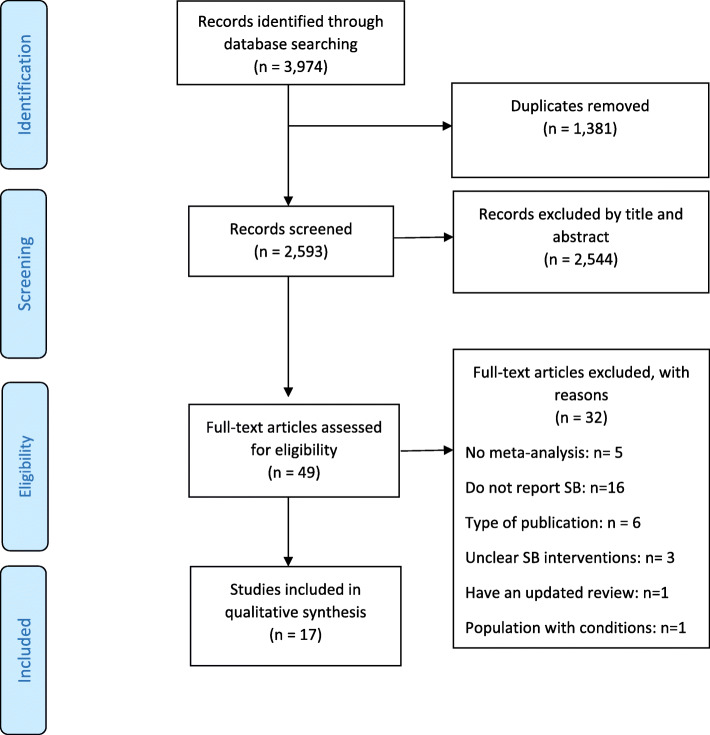
The literature search yielded 3974 titles; of these, 17 systematic reviews with meta-analysis [23–39] were eligible for review (Fig. 1).
Fig. 1.
PRISMA flowchart
Of the 17 included reviews, six reviews examined intervention effectiveness in children and adolescents across various settings [23, 26, 27, 31, 32, 35], mainly schools and home. Three reviews investigated SB interventions targeting adults in office workplaces [24, 28, 29], whilst the other six reviews explored interventions targeting adults across all settings [30, 34, 36–39]. Two reviews evaluated SB interventions across all age groups [25, 33]; however, only one review conducted sub-groups analysis for each age group [33]. Characteristics of the included reviews are presented in Additional file 2.
Behaviour outcomes reported in the included reviews were screen time (measured using self-report), sitting time (measured through self-report or device-measured detecting sit-stand posture) and sedentary time (measured by a device such as an accelerometer that detects intensity level). Screen time was the dominant outcome reported in children and adolescent, and it was reported in all seven studies in this age group, with only one study also investigate total sitting time [26] (Table 1).
Table 1.
Summary of evidence from quantitative research syntheses
| SB Interventions | Author/year | Effectiveness# Mean (95% CI) | ||
|---|---|---|---|---|
| Screen time | Occupational sitting and/or other sitting time | Overall sitting time with/ without screen time | ||
| Children | Biddle 2011 [23] | − 0.19 (− 0.30; − 0.08)% | ||
| Downing 2018 [26] | −17.12 min/d (− 28.82; − 5.42) | −18.91 min/d (− 33.31; − 4.51) | ||
| Grieken 2012 [31] | −17.95 min/d (− 26.61; − 9.28) | |||
| Kamath 2008 [27] | −0.31 (− 0.38, − 0.24) % | |||
| Maniccia 2011 [35] |
−0.10 (− 0.48; 0.27) %;a − 0.13 (− 0.24; − 0.01) %;b |
|||
| Wahi 2018 [32] | −0.90 h/wk (− 3.47; 1.66) | |||
| Wu 2016 [33] | −2.99 h/wk (− 7.51, 1.52) | |||
| Adolescents | Grieken 2012 [31] | No sub-group analysis | ||
| Kamath 2008 [27] | 0.00 (− 0.25, 0.25) % | |||
| Maniccia 2011 [35] | −0.18 (− 0.30; − 0.05) % | |||
| Wu 2016 [33] | −3.04 h/wk (− 7.62, 1.54) | |||
| Adults | Compernolle 2019 [34] | −0.56 (− 0.90; − 0,07) % | −0.32 (− 0.50; − 0,14) % | |
| Chu 2016 [24] | − 39.6 min/8-h (− 51.7; − 27.5) | |||
| Direito 2016* [25] | −0.26 (− 0.53; − 0.00) % | |||
| Neuhaus 2014 [28] | −77 min/ 8-h (− 120; − 35) | |||
| Martin 2015 [36] | −22.34 min/d (− 35.81; − 8.88) | |||
| Peachey 2018 [37] | −29.96 min/d (− 44.05; − 15.87) | −30.37 min/d (− 40.86; − 19.89) | ||
| Prince 2014 [38] | −1.28 (− 1.68; − 0.87) % | |||
| Shrestha 2018 [29] | −100 min/ 8-h (− 116; − 84) | |||
| Shrestha 2019 [39] | −61.08 min/d (− 79.40 to − 42.76) | −30.18 min/d (− 58.47; − 1.88) | ||
| Stephenson 2017 [30] | −41.28 min/d (− 60.99; − 21.58) | |||
| Wu 2016 [33] | −14.98 h/wk. (− 16.22, − 13.75) | |||
Note: a: effect size in children under 5 years; b: effect size in children 5 to 11 years, h /wk hour per week, min/d minutes per day, SB sedentary behaviour, SMD standardized mean difference, 95% CI 95% confident interval
Bold numbers indicate non-significant effect sizes. Negative numbers indicate reduction
#Meta-analyses reported post-intervention change-from-baseline difference between intervention and control group)
*Meta-analysis did not report effect size for adults and children separately
%Standardized mean difference, where effects were measured in different scale
The majority of reviews of SB intervention in adults had a primary focus on reductions in total sitting time (across all domains), with many focusing on reductions to occupational sitting time. Five reviews pooled screen time and sitting time in the primary analysis to report total time spent in sedentary activities [25, 30, 34, 36, 38]. When sitting time was used as the primary outcome, but not limited to occupational sitting, then the term “sedentary time” was interchanged. There was a significant overlap of primary studies included by Stephenson et al. 2017 [30], examining the effectiveness of technologies to reduce sedentary time, i.e. multi-context sitting time with/ without screen time, and by Chu et al. 2016 [24], investigating the effectiveness of SB interventions in reducing occupational sitting time. Summary of research evidence on SB intervention effectiveness is presented in Table 1.
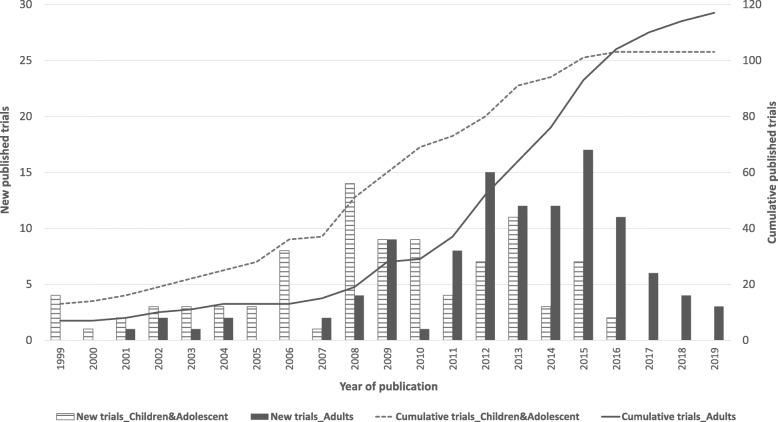
Overlapping was also observed in included reviews. Six out of 17 primary studies included by Stephenson et al. 2017 [30] were office workplace interventions. Seven out of 17 studies in Biddle et al. 2011 [23] were also included in Grieken et al. 2012 [31]. However, none of the reviews had an overlapping of more than 40% of its included trials. The 17 reviews included in this umbrella review comprised a total of 219 trials, of which 102 trials targeted children and adolescents, and 117 targeted adults. Figure 2 presents the cumulative total number of SB trials published in the period 1999–2019. Given the insufficient level of detail reported in the included reviews, the number of primary interventions could not be analysed by settings.
Fig. 2.
Number of new and cumulative sedentary behaviour intervention trials over the two decades, 1999–2019
Sedentary behaviour interventions
Intervention delivery and components
The majority of the primary interventions were conducted in high-income countries including the United States, the United Kingdom, Australia and Europe. The length of interventions varied from a few days to 4 years, with the longer-term trials tending to be interventions targeting children and adolescents in the school setting. The included reviews did not provide sufficient data to quantitatively summarise intervention setting, except for workplace interventions (3 independent reviews [24, 28, 29] with a total of 42 trials adopting offices as the primary setting).
Intervention components were categorised into three main groups, i.e. motivational/volitional component, physical environmental changes and policy changes [24, 29]. Multi-component interventions were defined differently across reviews. Shrestha et al. [29] defined multi-component intervention as those including all three component categories, whilst Chu et al. [24] defined multi-component as a combination of motivational/volitional strategies and environmental changes. Details of common strategies under each component are presented in Table 2. Motivational/volitional strategies were available across all type of settings, while the other components were limited to specific settings, i.e. policy changes were employed mostly in the office setting, whilst environmental changes were observed in both office and classroom/ school as well as home settings.
Table 2.
Intervention settings and components of SB interventions
| Component | Settings | ||||
|---|---|---|---|---|---|
| School | Office | Home | Community | Primary care | |
| Motivation/volition |
Educational sessions on healthy lifestyle; Mass media or other health promotion materials, e.g. posters, newsletters etc. |
Goal setting in sitting time; Provide educational materials and tips via email or message; Strategies for self-monitoring and reinforcement for behaviour change; Motivational interview/ counselling sessions; (8 reviews) [24, 29, 33, 34, 36–39] | Goal setting in screen time; Dairy and materials to promote healthy lifestyle. (10 reviews) [26, 27, 31–36, 38, 39] | Group counselling; Mass media or other health promotion, e.g. posters, newsletters etc. (3 reviews) [23, 26, 36] | Counselling sessions, individualized lifestyle plan; Monitoring handbook (3 reviews) [23, 26, 36] |
| Environmental change | Sit-stand or standing desk (1 review) [26] | Sit-stand workstation, portable elliptical/pedal machine; stationary cycle ergometer and treadmill desk; reminder application installed in computer and tracking devices etc. (8 reviews) [24, 28–30, 34, 36–38] | Remove TV out of bed-rooms; screen time monitoring devices; sitting time monitoring/ tracking devices (7 reviews) [27, 30, 33–35, 38, 39] | Not available | Not available |
| Policy change | Curriculum change (3 reviews) [26, 32, 35] | Walking or standing meetings; organizational schedule for sitting breaks and stand up. (1 review) [29] | Not available | Not available | Not available |
Intervention delivery and components in children and adolescent
Interventions promoting healthy lifestyles in children overwhelmingly employed motivational/volitional strategies; they also targeted other risk behaviours such as physical activity and diet [17, 27] and were delivered in multiple-settings, i.e. schools in combination with home and/or community. The included reviews of SB interventions in children and adolescents highlighted the involvement of parents, educators and the importance of trainings for parents [26, 27, 31]. Environmental changes component such as sit-stand desks in class were discussed only in one review (see Table 2).
Intervention delivery and components in adults
Reviews of occupational sitting (3 out of 11 reviews) were workplace interventions that had targeting workers in office-based occupations [24, 28, 29]. A 2016 review reported that motivational/volitional strategies were the most common components with 15 primary trials employing these strategies, compared to only five trials encompassing physical environment changes [24]. In contrast, a 2014 review [28] reported 20 trials in office settings as employing workplace environmental changes, i.e. sit-stand-desk or adjustable standing desk, active work stations, etc. The most recent Cochrane review of workplace interventions in 2018 [29] identified the most popular strategies as physical changes in the workplace (n = 10) followed by motivational/volitional strategies (n = 2).
Eight reviews (out of 11 reviews in adults) investigated SB intervention effectiveness in adults across all settings, including both workplace and non-occupational settings (i.e. home, community, primary care, clinics) [25, 30, 33, 34, 36–39]. Of these, two reviews [25, 30] investigated the effectiveness of technologies to reduce SB such as computer prompts, reminder emails or messages, wearable tracking devices, mobile phone etc. were considered as motivational/volitional components.
Intervention outcomes
All included reviews highlighted that outcome measurement in the trials was often based on self-reported sitting time and sedentary screen time. Trials that used objective measurement predominately investigated interventions within office settings. The difference in intervention effectiveness between objective measurement and self-report remains inconclusive. Greater effect sizes following objective measurement were reported in one review of occupational sitting [24] and general sedentary time [34]. However, another had a more substantial effect based on self-report [30, 37], whilst another [25] reported a non-significant difference between the two types of measurements.
Only one review attempted to analyse the intervention effects on breaks and the number of prolonged sitting bouts but reported non-significant effects in those two outcomes [34, 36].
Intervention effectiveness
Intervention effectiveness in children and adolescent
Of the seven reviews investigating SB in children, all except one reported significant, small to moderate effect sizes on reduction in screen time [23, 26, 27, 31–33]. The other study reported a non-significant reduction in screen time mean difference (MD) -0.90 h per week (95% CI − 3.47 to 1.66) [32]. A meta-analysis of sedentary time and screen time together reported the overall MD of − 17.12 min/day (95% CI − 28.82 to − 5.42) and MD of sedentary time between groups as − 18.91 (95% CI − 33.31 to − 4.51) [26]. The quantitative analysis reported in Biddle et al. [23] indicated larger effect sizes following multi-risk behaviour interventions in children. Motivation/volition components tended to be more effective in children [27], while there was no significant difference between single- and multi-component interventions [31]. Sub-group analyses sought to identify the association between length of intervention and effectiveness, but the results remained inconclusive with one review supporting interventions longer than 12 months (long term interventions) [23], while another review reported larger effect sizes following medium-term interventions (4–6 months) [36]. Another two sub-group analyses revealed larger effect sizes following short-term (3 months or less) interventions [23, 27].
Comparing intervention effectiveness by age group, Kamath et al. [27] reported a more substantial and significant effect size in children (standardized mean difference (SMD) -0.31; 95%CI − 0.39 to − 0.24) and a non-significant effect in adolescents (SMD 0.00; 95%CI − 0.25 to − 0.20). In contrast, a subgroup analysis by Maniccia et al. [35] reported a stronger effect size in the adolescent group (g = − 0.176 (95% CI − 0.386 to − 0.049) versus g = − 0.125 (95%CI − 0.241 to − 0.008) in children. Table 1 provides a summary of intervention effect sizes across all age group.
Intervention effectiveness in adults
One systematic review [38] with meta-analysis reported the effects of reducing SB by three different types of interventions: PA interventions that aimed to reduce SB; SB combined with PA intervention, and solely SB focused-interventions. The study reported moderate-quality evidence (assessed using Cochrane GRADE framework - Grading of Recommendations, Assessment, Development and Evaluations) that large and clinically meaningful reductions in sedentary time resulted from interventions with a focus on reducing SBs (SMD = − 1.28 [95% CI: − 1.68 to − 0.87]). Another meta-analysis [36] supported this evidence with multi-risk behaviour interventions reducing SB by 24 min/day (95% CI − 41 to − 8 min/day, moderate quality). Meanwhile, interventions focusing on SB resulted in a mean reduction of 42 min/day (95% CI − 79 to − 5 min/day, low quality using Grade). There was no evidence of an effect amongst PA and combined PA/SB interventions on reducing sedentary time [36].
Reductions in sitting time were similar between interventions in workplaces (− 29.96 min/day; 95% CI − 44.05 to − 15.87) and other settings, which included community, domestic and recreational environments (− 30.47 min/day; 95% CI − 44.68 to − 16.26) [37]. However, looking at the level of evidence and effect size, stronger and consistent evidence is more likely to support SB intervention effectiveness in the office setting (Table 1).
For interventions specifically targeting adults in workplace settings, one review reported a more substantial effect size for multi-component interventions (mean difference MD − 88.8 min/8 h workday 95% CI − 132.7 to − 44.9 [24], compared to environmental changes intervention (MD − 72.8 min/8-h workday; 95% CI − 104.9 to − 40.6) and motivation/volition components (MD − 15.5 min/8-h workday, 95% CI − 22.9 to − 8.2) [24]. However, two other reviews concluded that environmental changes components were more effective than the other components. The meta-analysis in the Cochrane review reported that physical workplace changes resulted in a change of − 100 min/8-h working day (95% CI − 116 to − 84), while the effect size of workplace policy changes and counselling components were non-significant [29]. Another review that quantitatively analysed intervention effects on sitting time across all settings reported similar results; environmental interventions had the largest reduction in daily sitting time (− 40.59 min/day; 95% CI − 61.65 to − 19.53), followed by multi-component (− 35.53 min/day; 95% CI − 57.27 to − 13.79) and motivation/volition component (− 23.87 min/day; 95% CI − 37.24 to − 10.49) [37]. Another review reported a reduction of − 77 min/8 h workday following active-permissive workstation component [28].
No evidence was available on the effectiveness of interventions for reducing non-occupational sedentary time in older adults (age > 70 years) [39]. One review identified five interventions targeting older adults [34]; of those, only three trials involved a healthy population, whilst the other two targeted breast cancer survivors and people with T2D. No subgroup analysis was conducted [34].
A review of interventions using technology to reduce time spent in SB in various settings reported an overall reduction in sitting time of − 41.28 min/day (95% CI − 60.99 to 21.58) [30], which is a slightly smaller effect size compared to interventions in the office setting. Another review investigating the effectiveness of technologies in reducing SB in all age group 8–71 years, reported a small effect of − 0.26 h/day (95% CI − 0.53 to 0.00) [25].
Methodological issues in trials evaluating the effectiveness of SB interventions
The included reviews highlighted a range of methodological issues of trials for SB interventions. Evidence highlighted that non-random allocation and concealment were generally inevitable for trials evaluating SB interventions in workplaces, communities and schools [26, 29, 30, 32]. Non-continuous measures (percentage) of screen time or sitting time reported in the primary studies raised an issue in the quantitative analyses, making it challenging to compare intervention effectiveness [26]. Issues with self-reported SB were highlighted, such as an unclear description of the self-report methods and measures captured and the lack of standardised methods in measuring screen time [31, 33]. Reviews suggested that while objective measurement is preferred for accuracy and validity, self-report measurements are also beneficial in analysis of SB domains, i.e. behaviours undertaken during sitting [28, 39]. The reviews also highlighted the lack of long-term, large scale and low risk of bias trials [26, 28].
Quality of included systematic reviews
The quality of the majority of the included reviews was rated as moderate using AMSTAR. Three reviews [29, 38, 39] were rated as high quality, eight as moderate quality [24, 26, 28, 30, 32–34, 37] and six as low quality [23, 25, 27, 31, 35, 36]. Whilst one review confined its literature search to three databases [33], the majority of reviews included five databases [23, 24, 27, 30, 31, 34, 37] or more [25, 26, 28, 29, 32, 35, 36, 38, 39].
For systematic reviews with meta-analysis, it is imperative to describe the controls, but only 11 of the 17 reviews provided information regarding comparator groups [25, 29–31, 33–39]. Different comparators were employed across trials, i.e. do-nothing control or counselling or other types of interventions, however, only seven of the meta-analyses conducted a sub-group analysis for different controls [29, 33–35, 37, 39]. Six reviews had a mixed population, i.e. included both healthy people and people with co-morbidities [34–39], but only one review conducted subgroup analysis for people with conditions [35]. Additionally, some reviews did not provide sufficient data regarding settings in individual primary studies included [25, 34, 38]. It is noted that some meta-analyses [24, 29] reported reduction in occupation sitting per 8-h working day but the analysis also included trials having office as primary setting but reported overall sitting time, i.e. total sitting time per day or per week outside of office hour.
Discussion
This umbrella review provides a state-of-art level of evidence syntheses of the findings from 17 systematic reviews that conducted meta-analyses of interventions designed to reduce SB across different age groups. This area of research continues to be highly productive, and new trials are emerging at a rapid rate [40]. Moreover, this umbrella review is the first review of reviews making an effort to examine the effectiveness of SB interventions on measures of behaviour change (both screen time and sitting time), and to cover a broader span of interventions. This umbrella review also summarises quantitative evidence regarding the effectiveness of different intervention components and different settings.
With many primary studies published, all the included reviews often addressed different outcomes, or different age groups and/or settings despite some overlap in the primary studies investigated. Since the overlap observed was small, their impact on the results of the quantitative analyses was not explored. Given that data extraction was conducted at the review level, there were some uncertainties around whether the included primary studies were SB intervention per se or PA focused interventions that aimed to reduce SB. This umbrella review, therefore, accepted the reviews’ classification of trials. Lastly, SB interventions targeting the older age group were not captured in this review. A potential reason may be the lack of sufficient data or primary studies to conduct a meta-analysis. One review, included five studies in older people, with only one being an RCT and the rest pilot studies [41]. Another reason is that interventions targeting this age group often focus on participants’ conditions, i.e. stroke survivors, CVDs, cancer, which is outside of the scope of this umbrella review [41].
This evidence synthesis indicated that SB interventions were superior to PA interventions and PA + SB combined in reducing sedentary time. This result is supported by the fact that SB is different from insufficient physical activity, where the latter refers to not meeting the recommended level of PA as per guidelines [1, 42]. Moreover, this SB superiority is probably strongly related to the distinct differences in behavioural barriers/ facilitators of SB and PA. Targeting specific SB behavioural elements is likely to have unique effects. However, this in turn raises the question of how PA components can be incorporated effectively into an SB intervention. The relative benefits of a greater reduction in sitting time being replaced with standing or light-intensity PA compared with a smaller reduction in sitting time being replaced with moderate-vigorous PA warrants further research. Different strategies can achieve comparable benefits, and replacing SB with light-intensity PA might be of value for those individuals who find moderate-vigorous PA challenging [14, 43].
Secondly, our findings support employing environmental changes components to facilitate the reduction in SB. This component was shown to yield the most significant effect size; it was also the most common component for SB interventions, especially in workplace settings [29, 37]. However, analyses indicated that environmental changes such as sit-stand desks in office setting offered greater effects in the short and medium-term.
Interestingly, the effects of motivational/volitional strategies tended to increase in accordance with the length of intervention, i.e. non-significant effect in the short term but a significant reduction at medium-term follow-up [29]. Furthermore, in one review, motivational/volitional strategies were favoured over environmental changes in SB intervention in reducing screen time in children and adolescents [27]. These findings have important implications for developing SB intervention strategies and components that are suitable for different age groups in different settings.
Exposure to SB is frequently operationalised under a socio-ecological system where an individual’s SB is highly influenced by multiple factors such as the nature of their tasks and the tools/ equipment used to perform the tasks [16]. It explained why sit-stand desks in the workplace setting could be very effective in reducing sitting time as sitting itself is not a prerequisite for the work at hand [44, 45].
This contrasts to other types of SB such as driving an automobile, where inherent challenges still remain in terms of addressing all the behavioural influences to promote meaningful reductions in time spent sitting. One review attempted to investigate the intervention effectiveness in reducing sitting while using public transport, but there were insufficient primary studies to conduct a meaningful evidence synthesis [39]. Future research should also focus on initiatives to explore other SB non-occupational settings such as leisure or domestic activities.
Moreover, future research efforts should be directed at unpacking the finer details of SB reduction interventions, including identifying the constituent behaviour change techniques/strategies applied and the relative effectiveness of such approaches [44–46].
Conclusion
In conclusion, there is strong evidence supporting the effectiveness of SB interventions in reducing sedentary time, especially interventions targeting occupational sitting in office settings with a clinically meaningful reduction of at least 30 min per day [47]. SB interventions were also effective in reducing screen time in children and adolescents; however, the effect size appears to be small. Future research needs to explore the potential of SB in older age groups outside of occupational settings as well as during sedentary leisure time. Moreover, sustainability of changes in SB remains a challenge.
Supplementary information
Additional file 1. Search strategy by database.
Additional file 2. Characteristics of included studies.
Acknowledgements
We thank Deakin University liaison librarian for her support in developing search strategies.
Abbreviations
- AMSTAR
A measure tool to assess systematic reviews
- CVD
Cardiovascular disease
- GRADE
Grading of recommendations, assessment, development and evaluations
- JBI
Joanna Briggs Institute
- MD
Mean difference
- MET
Metabolic equivalents of task
- PA
Physical activity
- RCT
Randomised controlled trial
- SB
Sedentary behaviour
- SMD
Standardized mean difference
- T2D
Type 2 diabetes
Authors’ contributions
PN conceived the study, carried out the design, bibliographic search, paper screening, quality assessment, data extraction and synthesis, interpreted the results, and drafted and edited the paper. LL and DN independently conducted paper screening, quality assessment, data extraction and helped editing the paper. MM, DD and LG participated in the design of the study, provided methodological input, and assisted in the editing of the paper. All authors read and approved the final manuscript.
Funding
PN is funded by a PhD stipend provided jointly by Deakin University and the Baker Heart and Diabetes Institute.
DD is supported by NHMRC Senior Research Fellowships (#1078360) and by the Victorian Government’s Operational Infrastructure Support program.
The funders had no role in the research.
Availability of data and materials
All data generated or analysed during this study are included in this published article and its supplementary information files.
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Supplementary information accompanies this paper at 10.1186/s12966-020-01009-3.
References
- 1.Tremblay MS, Aubert S, Barnes JD, Saunders TJ, Carson V, Latimer-Cheung AE, et al. Sedentary behavior research network (SBRN)–terminology consensus project process and outcome. Int J Behav Nutr Phys Act. 2017;14(1):75. doi: 10.1186/s12966-017-0525-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Owen N, Sugiyama T, Eakin EE, Gardiner PA, Tremblay MS, Sallis JF. Adults’ sedentary behavior: determinants and interventions. Am J Prev Med. 2011;41(2):189–196. doi: 10.1016/j.amepre.2011.05.013. [DOI] [PubMed] [Google Scholar]
- 3.Church TS, Thomas DM, Tudor-Locke C, Katzmarzyk PT, Earnest CP, Rodarte RQ, et al. Trends over 5 decades in US occupation-related physical activity and their associations with obesity. PLoS One. 2011;6(5):e19657. doi: 10.1371/journal.pone.0019657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dempsey PC, Owen N, Biddle SJ, Dunstan DW. Managing sedentary behavior to reduce the risk of diabetes and cardiovascular disease. Curr Diab Rep. 2014;14(9):522. doi: 10.1007/s11892-014-0522-0. [DOI] [PubMed] [Google Scholar]
- 5.Bauman A, Allman-Farinelli M, Huxley R, James W. Leisure-time physical activity alone may not be a sufficient public health approach to prevent obesity–a focus on China. Obes Rev. 2008;9(s1):119–126. doi: 10.1111/j.1467-789X.2007.00452.x. [DOI] [PubMed] [Google Scholar]
- 6.Australian Bureau of Statistics . Australian health survey: physical activity 2011–12. Canberra: ABS; 2013. [Google Scholar]
- 7.Government A. Australia’s physical activity and sedentary behaviour guidelines. In: Department of Health, editor. 2017.
- 8.Tremblay MS, LeBlanc AG, Janssen I, Kho ME, Hicks A, Murumets K, et al. Canadian sedentary behaviour guidelines for children and youth. Appl Physiol Nutr Metab. 2011;36(1):59–64. doi: 10.1139/H11-012. [DOI] [PubMed] [Google Scholar]
- 9.Australian Government. Australia’s Physical Activity and Sedentary Behaviour Guidelines 2017 [Available from: https://www1.health.gov.au/internet/main/publishing.nsf/Content/sbehaviour.
- 10.The US. Physical activity guidelines advisory committee. Washington: Physical Activity Guidelines Advisory Committee Scientific Report; 2018. [Google Scholar]
- 11.Peterson MD, Sarma AV, Gordon PM. Sitting time and all-cause mortality risk. Arch Intern Med. 2012;172(16):1270–1272. doi: 10.1001/archinternmed.2012.2527. [DOI] [PubMed] [Google Scholar]
- 12.Patterson R, McNamara E, Tainio M, de Sá TH, Smith AD, Sharp SJ, et al. Sedentary behaviour and risk of all-cause, cardiovascular and cancer mortality, and incident type 2 diabetes: a systematic review and dose response meta-analysis. Eur J Epidemiol. 2018;33:811–829. doi: 10.1007/s10654-018-0380-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Schmid D, Leitzmann MF. Television Viewing and Time Spent Sedentary in Relation to Cancer Risk: A Meta-Analysis. J Natl Cancer Inst. 2014;106(7). [DOI] [PubMed]
- 14.Biswas A, Oh PI, Faulkner GE, Bonsignore A, Pakosh MT, Alter DA. The energy expenditure benefits of reallocating sedentary time with physical activity: a systematic review and meta-analysis. J Public Health. 2018;40(2):295–303. doi: 10.1093/pubmed/fdx062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Carson V, Hunter S, Kuzik N, Gray CE, Poitras VJ, Chaput J-P, et al. Systematic review of sedentary behaviour and health indicators in school-aged children and youth: an update. Appl Physiol Nutri Metab. 2016;41(6 (Suppl. 3)):S240-SS65. [DOI] [PubMed]
- 16.Straker L, Dunstan D, Gilson N, Healy G. Sedentary work - Evidence on an emergent work health and safety issue - Final report. Canberra; 2016.
- 17.Biddle SJ, Petrolini I, Pearson N. Interventions designed to reduce sedentary behaviours in young people: a review of reviews. Br J Sports Med. 2014;48(3):182–186. doi: 10.1136/bjsports-2013-093078. [DOI] [PubMed] [Google Scholar]
- 18.Moher D, Liberati A, Tetzlaff J, Altman DG. The Prisma Group. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLoS Med. 2009;6(7):e1000097. doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Aromataris E, Fernandez R, Godfrey CM, Holly C, Khalil H, Tungpunkom P. Summarizing systematic reviews: methodological development, conduct and reporting of an umbrella review approach. Int J Evid Based Healthc. 2015;13(3):132–140. doi: 10.1097/XEB.0000000000000055. [DOI] [PubMed] [Google Scholar]
- 20.Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A. Rayyan—a web and mobile app for systematic reviews. J Syst Rev. 2016;5(1):210. doi: 10.1186/s13643-016-0384-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Shea BJ, Hamel C, Wells GA, Bouter LM, Kristjansson E, Grimshaw J, et al. AMSTAR is a reliable and valid measurement tool to assess the methodological quality of systematic reviews. J Clin Epidemiol. 2009;62(10):1013–1020. doi: 10.1016/j.jclinepi.2008.10.009. [DOI] [PubMed] [Google Scholar]
- 22.Shea BJ, Reeves BC, Wells G, Thuku M, Hamel C, Moran J, et al. AMSTAR 2: a critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ. 2017;358:j4008. doi: 10.1136/bmj.j4008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Biddle SJ, O’Connell S, Braithwaite RE. Sedentary behaviour interventions in young people: a meta-analysis. Br J Sports Med. 2011;45(11):937–942. doi: 10.1136/bjsports-2011-090205. [DOI] [PubMed] [Google Scholar]
- 24.Chu AHY, Ng SHX, Tan CS, Win AM, Koh D, Müller-Riemenschneider F. A systematic review and meta-analysis of workplace intervention strategies to reduce sedentary time in white-collar workers. Obes Rev. 2016;17(5):467–481. doi: 10.1111/obr.12388. [DOI] [PubMed] [Google Scholar]
- 25.Direito A, Carraça E, Rawstorn J, Whittaker R, Maddison R. mHealth technologies to influence physical activity and sedentary behaviors: behavior change techniques, systematic review and Meta-analysis of randomized controlled trials. Ann Behav Med. 2017;51(2):226–239. doi: 10.1007/s12160-016-9846-0. [DOI] [PubMed] [Google Scholar]
- 26.Downing KL, Hnatiuk JA, Hinkley T, Salmon J, Hesketh KD. Interventions to reduce sedentary behaviour in 0-5-year-olds: a systematic review and meta-analysis of randomised controlled trials. Br J Sports Med. 2018;52(5):314–321. doi: 10.1136/bjsports-2016-096634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kamath CC, Vickers KS, Ehrlich A, McGovern L, Johnson J, Singhal V, et al. Behavioral interventions to prevent childhood obesity: a systematic review and meta analyses of randomized trials. J Clin Endocrinol Metab. 2008;93(12):4606–4615. doi: 10.1210/jc.2006-2411. [DOI] [PubMed] [Google Scholar]
- 28.Neuhaus M, Eakin EG, Straker L, Owen N, Dunstan DW, Reid N, et al. Reducing occupational sedentary time: a systematic review and meta-analysis of evidence on activity-permissive workstations. Obes Rev. 2014;15(10):822–838. doi: 10.1111/obr.12201. [DOI] [PubMed] [Google Scholar]
- 29.Shrestha N, Kukkonen-Harjula KT, Verbeek JH, Ijaz S, Hermans V, Pedisic Z. Workplace interventions for reducing sitting at work. Cochrane Database Syst Rev. 2018;6. [DOI] [PMC free article] [PubMed]
- 30.Stephenson A, McDonough SM, Murphy MH, Nugent CD, Mair JL. Using computer, mobile and wearable technology enhanced interventions to reduce sedentary behaviour: a systematic review and meta-analysis. Int J Behav Nutr Phys Act. 2017;14(1):105. doi: 10.1186/s12966-017-0561-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Grieken AV, NPM E, Paulis WD, van der Wouden JC, Raat H. Primary prevention of overweight in children and adolescents: a meta-analysis of the effectiveness of interventions aiming to decrease sedentary behaviour. Int J Behav Nutr Phys Act. 2012;9(61). [DOI] [PMC free article] [PubMed]
- 32.Wahi G, Parkin PC, Beyene J, Uleryk EM, Birken CS. Effectiveness of interventions aimed at reducing screen time in children: a systematic review and meta-analysis of randomized controlled trials. Arch Pediatr Adolesc Med. 2011;165(11):979–986. doi: 10.1001/archpediatrics.2011.122. [DOI] [PubMed] [Google Scholar]
- 33.Wu L, Sun S, He Y, Jiang B. The effect of interventions targeting screen time reduction: A systematic review and meta-analysis. Medicine. 2016;95(27):e4029-e. [DOI] [PMC free article] [PubMed]
- 34.Compernolle S, Desmet A, Poppe L, Crombez G, De Bourdeaudhuij I, Cardon G, et al. Effectiveness of interventions using self-monitoring to reduce sedentary behavior in adults: A systematic review and meta-analysis. Int J Behav Nutr Phys Act. 2019;16(1). [DOI] [PMC free article] [PubMed]
- 35.Maniccia DM, Davison KK, Marshall SJ, Manganello JA, Dennison BA. A meta-analysis of interventions that target children's screen time for reduction. Pediatrics. 2011;128(1):e193–e210. doi: 10.1542/peds.2010-2353. [DOI] [PubMed] [Google Scholar]
- 36.Martin A, Fitzsimons C, Jepson R, Saunders DH, van der Ploeg HP, Teixeira PJ, et al. Interventions with potential to reduce sedentary time in adults: systematic review and meta-analysis. Br J Sports Med. 2015;49(16):1056–1063. doi: 10.1136/bjsports-2014-094524. [DOI] [PubMed] [Google Scholar]
- 37.Peachey MM, Richardson J, Tang AV, Haas VD-B, Gravesande J. Environmental, behavioural and multicomponent interventions to reduce adults’ sitting time: a systematic review and meta-analysis. Br J Sports Med. 2018;54:315–325. doi: 10.1136/bjsports-2017-098968. [DOI] [PubMed] [Google Scholar]
- 38.Prince SA, Saunders TJ, Gresty K, Reid RD. A comparison of the effectiveness of physical activity and sedentary behaviour interventions in reducing sedentary time in adults: a systematic review and meta-analysis of controlled trials. Obes Rev. 2014;15(11):905–919. doi: 10.1111/obr.12215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Shrestha N, Grgic J, Wiesner G, Parker A, Podnar H, Bennie JA, et al. Effectiveness of interventions for reducing non-occupational sedentary behaviour in adults and older adults: a systematic review and meta-analysis. Br J Sports Med. 2019;53(19):1206–1213. doi: 10.1136/bjsports-2017-098270. [DOI] [PubMed] [Google Scholar]
- 40.Chau JY, Reyes-Marcelino G, Burnett AC, Bauman AE, Freeman B. Hyping health effects: a news analysis of the ‘new smoking’and the role of sitting. Br J Sports Med. 2019;53(16):1039–1040. doi: 10.1136/bjsports-2018-099432. [DOI] [PubMed] [Google Scholar]
- 41.Aunger JA, Doody P, Greig CA. Interventions targeting sedentary behavior in non-working older adults: a systematic review. Maturitas. 2018;116:89–99. doi: 10.1016/j.maturitas.2018.08.002. [DOI] [PubMed] [Google Scholar]
- 42.van der Ploeg HP, Hillsdon M. Is sedentary behaviour just physical inactivity by another name? Int J Behav Nutr Phys Act. 2017;14(1):142. doi: 10.1186/s12966-017-0601-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Stamatakis E, Gill JMR. Sitting behaviour and physical activity: two sides of the same cardiovascular health coin? Br J Sports Med. 2019;53(14):852–853. doi: 10.1136/bjsports-2018-099640. [DOI] [PubMed] [Google Scholar]
- 44.Gardner B, Smith L, Lorencatto F, Hamer M, Biddle SJH. How to reduce sitting time? A review of behaviour change strategies used in sedentary behaviour reduction interventions among adults. Health Psychol Rev. 2016;10(1):89–112. doi: 10.1080/17437199.2015.1082146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Gardner B, Flint S, Rebar AL, Dewitt S, Quail SK, Whall H, et al. Is sitting invisible? Exploring how people mentally represent sitting. Int J Behav Nutr Phys Act. 2019;16(1):85. doi: 10.1186/s12966-019-0851-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Ojo SO, Bailey DP, Hewson DJ, Chater AM. Perceived barriers and facilitators to breaking up sitting time among desk-based office workers: a qualitative investigation using the TDF and COM-B. Int J Environ Res Public Health. 2019;16(16):2903. [DOI] [PMC free article] [PubMed]
- 47.Buman MP, Winkler EAH, Kurka JM, Hekler EB, Baldwin CM, Owen N, et al. Reallocating time to sleep, sedentary behaviors, or active behaviors: associations with cardiovascular disease risk biomarkers, NHANES 2005–2006. Am J Epidemiol. 2013;179(3):323–334. doi: 10.1093/aje/kwt292. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1. Search strategy by database.
Additional file 2. Characteristics of included studies.
Data Availability Statement
All data generated or analysed during this study are included in this published article and its supplementary information files.