KEY POINTS
Both sex (a biological attribute) and gender (a complex social construct incorporating identity, roles, relations and institutionalized gender) may influence infectious disease risk and outcomes, and severe acute respiratory syndrome coronavirus 2 appears to be no exception.
We found institutionalized gender inequality (as measured by the United Nations Development Project’s Gender Inequality Index) to be positively associated with the male:female ratio reported cases of coronavirus disease 2019 (COVID-19) among countries that report sex-disaggregated data; males accounted for more cases in countries with higher gender inequality.
Institutionalized gender and culturally entrenched roles and norms may influence who is most at risk of acquiring infection or who is able to receive a test.
To understand how sex and gender affect disease risk and outcomes for COVID-19 will require expanded testing and collection of relevant data; this understanding will be crucial to managing the current pandemic.
Among the many unknowns regarding severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and coronavirus disease 2019 (COVID-19) is the way in which sex and gender affect the risk of acquiring the virus, illness presentation, disease management and outcomes. Sex, a biological attribute, and gender, a social construct, may both influence an individual’s susceptibility, vulnerability and exposure to infectious disease.1 Immune function differs between sexes and has been shown to affect an individual’s likelihood of acquiring infection upon exposure, or developing complications.2–4 Indeed, early research has shown that these sex differences in immune response may lead to worse COVID-19 outcomes for males in terms of ability to recover from severe infection.5 Gender, which comprises roles, norms and behaviours that may vary by sex, is associated with an individual’s likelihood of exposure6,7 (Box 1). Several institutions, including the Canadian Institutes of Health Research, have appealed to researchers to include sex and gender variables in data analysis, to improve the effectiveness of health interventions and promote gender and health equity goals.8
Box 1:
Sex and gender
Sex refers to biological attributes such as anatomy, chromosomes and hormones that distinguish individuals as male, female or intersex. Sex may therefore influence an individual’s immune response or ability to resist or withstand infection. These characteristics exist on a spectrum, but in publicly available medical data, sex is usually classified as binary male or female.
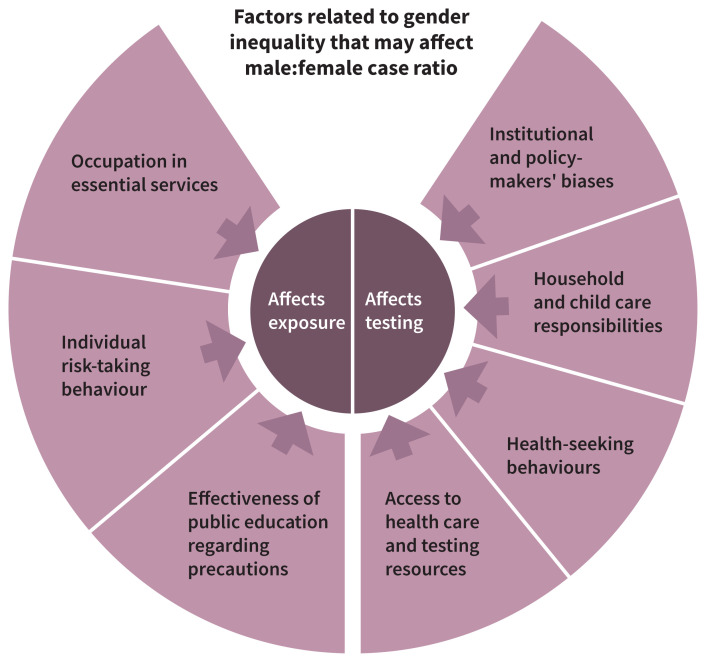
Gender refers to socially constructed norms, roles, identities and behaviours typically ascribed to women, men and gender-diverse individuals. It can also refer to relations among individuals based on gender, or the institutionalization of these norms through distribution of power among genders. Gender may therefore influence an individual’s exposure to infectious disease through occupation in essential services, risk-taking behaviours and employment of precautions, or have an impact on an individual’s ability to seek and receive testing and care, through norms for health-seeking behaviour, responsibilities at home or work, reduced availability of health services or institutional biases and policies. A much broader spectrum of gender exists, as it is a multidimensional social construct, both in terms of gender identity and the roles and norms that individuals fill, and it is distinct from sex. Further effort should be made in considering gender-diverse people and in proper use of the terminology, as misuse from international institutions, which often conflate sex and gender, might generate even more confusion.
In previous coronavirus epidemics (severe acute respiratory syndrome and Middle East respiratory syndrome), male sex was associated with worse outcomes;9,10 similarly, early evidence related to COVID-19 appears to largely show increased mortality among males.11 However, the prevalence of reported cases varies between men and women by country, suggesting that social, economic and cultural factors may influence either acquisition of SARS-CoV-2 or patterns of testing for suspected infection. We, a consortium of European and Canadian researchers (www.mcgill.ca/going-fwd4gender/), sought to assess the influence of gender-related factors on the relative male–female burden of COVID-19, to further understanding of the risks and impact of the COVID-19 pandemic.
How might gender influence observed sex differences in epidemiologic research on COVID-19?
Gender-related factors may influence an individual’s likelihood of exposure to SARS-CoV-2, but they may also influence whether an individual tries to obtain a test and whether they are given one. These factors are presented in a conceptual framework in Figure 1.
Figure 1:
Conceptual framework for how gender-related factors may be related to differences in prevalence of coronavirus disease 2019 for males and females.
Gender identity refers to the way in which individuals identify and express their gender as men, women or gender-diverse. How power, opportunities and resources are distributed among men and women within the political, educational and social institutions of a society reflect the institutionalization of gender.7 Institutionalized gender norms may directly affect health through differential access to health care, food education and income, according to gender.7,12–14 Furthermore, they shape social norms that define, reproduce and often justify different opportunities and expectations for women and men, such as social and family roles, job segregation and limitations, dress codes and health practices. Gender roles and norms may be related to sex but are also influenced by cultural differences.
Different disease prevalence between men and women may, therefore, be related to cultural roles and gender norms that influence risk for contracting the disease, such as a higher likelihood of employment in essential services like health care and service industries for women compared with men,15 or greater likelihood of caregiving. Indeed, women make up the majority of personal care and health service workers, child care workers and teachers, domestic cleaners, home aides and supermarket cashiers,16,17 thus increasing their likelihood of exposure to SARS-CoV-2. However, men predominate several other essential sectors, such as construction work and cleaning, security work, taxi and chauffeur services, and low-skilled social care.18
Gender inequality and biases within a society or health care system may also affect who receives a medical test. Research has long shown that although women are more proactive about their health and visit doctors more often than men, they frequently receive less intensive diagnostic and treatment interventions, with women’s symptoms often dismissed by doctors or assumed to be psychosomatic.2,19
Is gender inequality associated with sex ratios of SARS-CoV-2 positivity and deaths from COVID-19?
In an attempt to answer this question, we used publicly available data to explore a hypothesis that a difference between countries in the sex ratios of SARS-CoV-2 positivity and death from COVID-19 is related to institutionalized gender inequality and its potential effects on the relative risks of acquiring SARS-CoV-2, or the distribution of tests among individuals or the rates of mortality.
Our methods are summarized in Appendix 1 (available at www.cmaj.ca/lookup/doi/10.1503/cmaj.200971/tab-related-content). The Global Health 50/50 initiative created a live tracker that aggregates data on COVID-19 cases and mortality from published government reports.20 Sex-disaggregated data were available for 33 of 62 countries represented in the live tracker at the time of our analysis on Apr. 11, 2020. We considered whether the distribution of cases by sex reflected a gender-related inequality by testing for an association between a measure of institutionalized gender inequality at the country level and the sex ratios of COVID-19 cases reported for these countries. To measure institutionalized gender inequality, we used the United Nations Development Project’s Gender Inequality Index (GII), which reflects the distribution of sociopolitical power and resources between men and women by country. The GII is calculated using the relative proportion of men and women employed, the proportions of men and women who attain higher education, the proportion of women in parliament, and reproductive health in terms of teen birth rate and maternal mortality rate.21 The GII is standardized such that 0 indicates perfect gender equality and 1 indicates perfect inequality (in favour of men). Given the availability of data (official government reports include only data on male and female sex and the GII looks only at social equality between men and women), we were able to consider gender as binary and to discuss the social norms traditionally ascribed to men and women only.
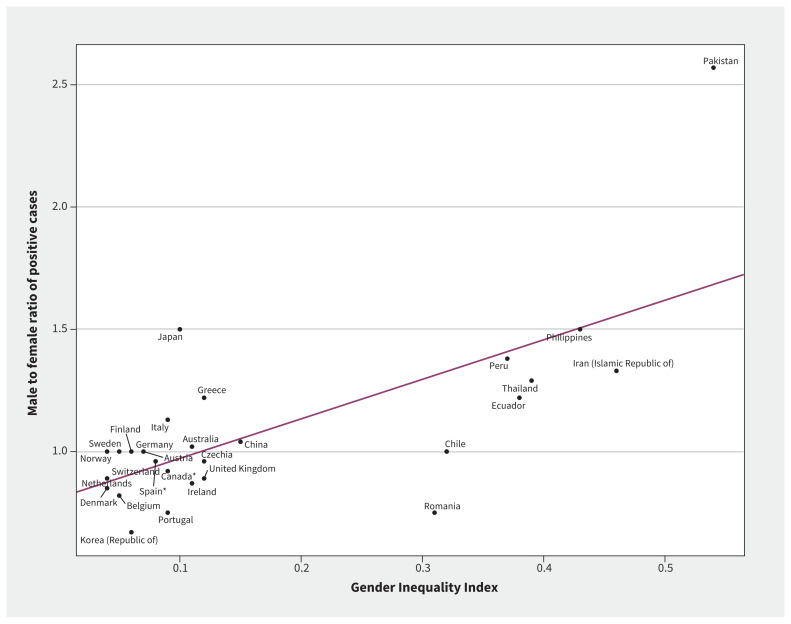
Figure 2 shows the calculated male:female ratio of COVID-19 cases to countries’ GII. Overall, the higher a country’s gender inequality favouring men, the greater the proportion of males among reported cases compared with females. We did not find a significant relationship between the reported male:female death ratio and countries’ GIIs.
Figure 2:
Male:female ratio of coronavirus disease 2019 (COVID-19) cases for all countries that reported sex-disaggregated data on Apr. 11, 2020, as a function of the country’s gender inequality per the 2017 United Nations Development report (estimate: 1.67 ± 0.32, R2 = 0.48, p < 0.001). COVID-19 data for the United Kingdom are represented only by Northern Ireland, as England, Scotland and Wales did not report sex-disaggregated data at the time of analysis. A higher Gender Inequality Index indicates higher inequality between men and women in a country, with women less empowered.
Our observations suggest that gender inequality may play a role in epidemiologic differences by sex. However, it is not clear whether this represents actual differences in men and women’s risks of acquiring COVID-19 or simply differences in who is seeking or receiving tests. It is possible that in countries with high inequality, men are more likely to be employed overall and therefore more likely to be exposed, or that in such countries, men feel more entitled to seek rationed tests or are more likely to receive them, owing to entrenched cultural norms and institutionalized bias against women in health care settings. Without information on the sex ratios of those seeking or receiving tests, it is impossible to disentangle these potential mechanisms. Furthermore, globally, countries’ respective GII and overall economic development are strongly correlated, and therefore the observed association could be related to countries’ availability of resources in terms of testing, record-keeping and reporting.
Our finding that gender inequality was not associated with sex differences in death rates is similarly difficult to explain. Do biological differences (e.g., in immunity or comorbidities) between men and women contribute to mortality risk of COVID-19, or do sociocultural variables (such as delayed care-seeking among men or reduced testing among women) intersect to influence mortality? It is also possible that differences among countries in criteria for reporting COVID-19 deaths could obscure a relationship between gender equality and mortality (an issue further complicated by reporting protocols changing as the pandemic has progressed).
What can be done to improve our understanding of the role that gender plays in determining risk of disease and mortality related to COVID-19?
Our understanding of gender influences on disease outcomes for COVID-19 is limited by the quality and availability of data. It is important that every country report sex-disaggregated data on COVID-19 cases and deaths, and record gender identity in addition to sex. Additionally, it will be more informative to report not only cases, but also the sex or gender identity or both of those seeking and receiving SARS-CoV-2 tests, in order to uncover whether differences observed are associated with inequalities in access to care or represent actual sex- or gender-based differences in infection rates.
Further research should investigate the contribution of social norms and roles to identify how sex and gender may intersect to influence risk for disease and access to care. Therefore, we suggest the collection and reporting of information on employment status (full-time, part-time employed, unemployed), occupation category, income, household responsibilities (such as caregiving), number of children or household size, risk-taking behaviours such as use of precautions (or attitudes about them), and health-seeking behaviours (such as time from first experiencing symptoms to seeking a test), to determine what types of exposures account for most cases and whether those exposures are gendered.
Clinical biological variables such as immune response and number of comorbidities must also be collected in order to consider the combined effects of these with social variables on outcomes. To manage this pandemic, it will be important to untangle sex- and gender-related factors associated with testing for or contracting SARS-CoV-2, by exploring the interactions between biological and social variables and their effects on acquiring infection, receiving care, and experiencing certain disease outcomes.
Gender is one of many intersecting social constructs that may influence an individual’s lived experience and, therefore, exposure to and acquisition of SARS-CoV-2 and access to care. Information pertaining to other social constructs such as race, ethnicity or immigration status, and how these variables may interact with gender to influence risk related to COVID-19, is crucial to prevent or minimize the impact of a potential second wave. Continued investigation of both biological and social variables and their influence on COVID-19 exposure and vulnerability will be necessary to understand and therefore manage this unprecedented pandemic.
Footnotes
Competing interests: None declared.
This article has been peer reviewed.
Contributors: All of the authors contributed to the conception and design of the work, drafted the manuscript, revised it critically for important intellectual content, gave final approval of the version to be published and agreed to be accountable for all aspects of the work. Christina Tadiri and Teresa Gisinger contributed equally as co-first authors.
Funding: The GOING-FWD Consortium is funded by the GENDER-NET Plus ERA-NET Initiative (Project Ref. No. GNP-78): the Canadian Institutes of Health Research (GNP-161904), La Caixa Foundation (ID 100010434; with code LCF/PR/DE18/52010001), the Swedish Research Council (2018-00932) and the Austrian Science Fund (FWF, I 4209). Valeria Raparelli is funded by the Scientific Independence of Young Researcher Program of the Italian Ministry of University, Education and Research (RBSI14HNVT).
References
- 1.Griesbeck M, Ziegler S, Laffont S, et al. Sex differences in plasmacytoid dendritic cell levels of IRF5 drive higher IFN-α production in women. J Immunol 2015;195:5327–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Oksuzyan A, Juel K, Vaupel JW, et al. Men: good health and high mortality. Sex differences in health and aging. Aging Clin Exp Res 2008;20:91–102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Torcia MG, Nencioni L, Clemente AM, et al. Sex differences in the response to viral infections: TLR8 and TLR9 ligand stimulation induce higher IL10 production in males. PLoS One 2012;7:e39853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Scully EP, Haverfield J, Ursin RL, et al. Considering how biological sex impacts immune responses and COVID-19 outcomes. Nat Rev Immunol 2020;20:442–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Klein SL, Dhakal S, Ursin RL, et al. Biological sex impacts COVID-19 outcomes. PLoS Pathog 2020;16:e1008570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.What is gender? What is sex? Ottawa: Canadian Institutes of Health Research; modified 2020 Apr. 28. Available: https://cihr-irsc.gc.ca/e/48642.html (accessed 2020 Apr. 30). [Google Scholar]
- 7.Johnson JL, Greaves L, Repta R. Better science with sex and gender: facilitating the use of a sex and gender-based analysis in health research. Int J Equity Health 2009;8:14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Why sex and gender need to be considered in COVID-19 research: a guide for applicants and peer reviewers [infographic]. Ottawa: Canadian Institutes of Health Research; modified 2020 Apr. 20. Available: https://cihr-irsc.gc.ca/e/documents/sex_gender_covid19_guide-en.pdf (accessed 2020 Apr. 30). [Google Scholar]
- 9.Karlberg J, Chong DSY, Lai WYY. Do men have a higher case fatality rate of severe acute respiratory syndrome than women do? Am J Epidemiol 2004;159:229–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chen X, Chughtai AA, Dyda A, et al. Comparative epidemiology of Middle East respiratory syndrome coronavirus (MERS-CoV) in Saudi Arabia and South Korea. Emerg Microbes Infect 2017;6:e51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Palaiodimos L, Kokkinidis DG, Li W, et al. Severe obesity, increasing age and male sex are independently associated with worse in-hospital outcomes, and higher in-hospital mortality, in a cohort of patients with COVID-19 in the Bronx, New York. Metabolism 2020;108:154262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Choudhury KK, Hanifi MA, Rasheed S, et al. Gender inequality and severe malnutrition among children in a remote rural area of Bangladesh. J Health Popul Nutr 2000;18:123–30. [PubMed] [Google Scholar]
- 13.Ene-Obong HN, Enugu GI, Uwaegbute AC. Determinants of health and nutritional status of rural Nigerian women. J Health Popul Nutr 2001;19:320–30. [PubMed] [Google Scholar]
- 14.Attanapola CT. Changing gender roles and health impacts among female workers in export-processing industries in Sri Lanka. Soc Sci Med 2004;58: 2301–12. [DOI] [PubMed] [Google Scholar]
- 15.Meleis AI, Caglia J, Langer A. Women and health: women’s dual roles as both recipients and providers of healthcare. J Womens Health (Larchmt) 2016;25:329–31. [DOI] [PubMed] [Google Scholar]
- 16.Labour Force Survey. European Commission; Available: https://ec.europa.eu/eurostat/web/microdata/labour-force-survey (accessed 2020 Apr. 30). [Google Scholar]
- 17.COVID-19 and gender equality: frontline workers. Vilnius (Lithuania): European Institute for Gender Equality; Available: https://eige.europa.eu/covid-19-and-gender-equality/frontline-workers (accessed 2020 Apr. 30). [Google Scholar]
- 18.Wise J. COVID-19: low skilled men have highest death rate of working age adults. BMJ 2020;369:m1906. [DOI] [PubMed] [Google Scholar]
- 19.Wingard DL. The sex differential in morbidity, mortality, and lifestyle. Annu Rev Public Health 1984;5:433–58. [DOI] [PubMed] [Google Scholar]
- 20.Sex, gender and COVID-19: overview and resources — Tracking differences in COVID-19 illness and death among women and men. Global Health 5050. Available: https://globalhealth5050.org/covid19/#1586352650173-d9a8b64b-670a (accessed 2020 Apr. 11).
- 21.Gender Inequality Index (GII). United Nations Development Programme. Available: http://hdr.undp.org/en/content/gender-inequality-index-gii (accessed 2020 Apr. 11).