During the coronavirus disease 2019 (COVID-19) pandemic, Singapore implemented large-scale institutional isolation facilities to contain outbreaks among migrant workers who contracted COVID-19 but did not have the ability to self-isolate. In this article, the authors share their experience operating one of the largest of these facilities.
Abstract
Singapore is one of the most densely populated small island–states in the world. During the coronavirus disease 2019 (COVID-19) pandemic, Singapore implemented large-scale institutional isolation units called Community Care Facilities (CCFs) to combat the outbreak in the community by housing low-risk COVID-19 patients from April to August 2020. The CCFs were created rapidly by converting existing public spaces and used a protocolized system, augmented by telemedicine to enable a low health care worker–patient ratio (98 health care workers for 3200 beds), to operate these unique facilities. In the first month, a total of 3758 patients were admitted to 4 halls, 4929 in-house medical consults occurred, 136 patients were transferred to a hospital, 1 patient died 2 weeks after discharge, and no health care workers became infected. This article shares the authors' experience in operating these massive-scale isolation facilities while prioritizing safety for all and ensuring holistic patient care in the face of a public health crisis and lean health care resources.
In Singapore, the construction industry employs approximately 293 300 foreign workers. In April, an outbreak of coronavirus disease 2019 (COVID-19) occurred among these workers, who lived in crowded dormitories (1). As of 3 August 2020, 53 051 COVID-19 cases were reported in Singapore, 94.3% of which involved foreign workers living in dormitories (2).
As such, isolation centers called Community Care Facilities (CCFs) were set up throughout the country to house patients with COVID-19 who were at low risk for dying of the disease. The admission of patients to CCFs was mandated by the Infectious Diseases Act, which authorizes the Director of Medical Services to order any person who is—or suspected to be—infected with or carrying an infectious disease or who is a contact of such a person to be detained and isolated in a hospital or other place. The CCFs act as a step-down care facility after diagnosis and admit low-risk foreign workers from dormitories or patients who have recovered well in the hospital and have been discharged. Patients may stay in the CCF for up to 2 weeks and are then transferred to another step-down isolation facility to serve the rest of the minimum 21-day isolation period after diagnosis.
Physical Setup of CCFExpo
Singapore's public health care system is divided into 3 clusters (3), each of which was tasked with operating the several CCFs rapidly created to manage the COVID-19 outbreak. This article focuses on the initial experience (in May 2020) of the SingHealth cluster, which ran halls 7 to 10 (3200 beds) of the CCFExpo facility.
Singapore Expo has 100 000 square meters of column-free, indoor space spread over 10 halls. With a maximum capacity of 8000 beds, CCFExpo is one of the largest isolation facilities of its kind. The first 2 halls were retrofitted to purpose over 3 days and the remaining 8 halls within 20 days.
Each hall was repurposed to accommodate 800 patients, with due consideration given to fire emergencies and contingency plans. The 2.4- × 3.6-m twin-sharing patient cubicles were constructed with partition boards (Figure). Patients were allowed to move freely within their designated hall. Each hall was equipped with medical consultation rooms, pharmacies, self-monitoring stations, Wi-Fi access, recreational amenities, water dispensers, showers and toilets, and self-service laundry facilities. Radiologic service was provided by vehicles retrofitted with imaging machines.
Figure. Setup of halls 7 to 10 at CCFExpo.
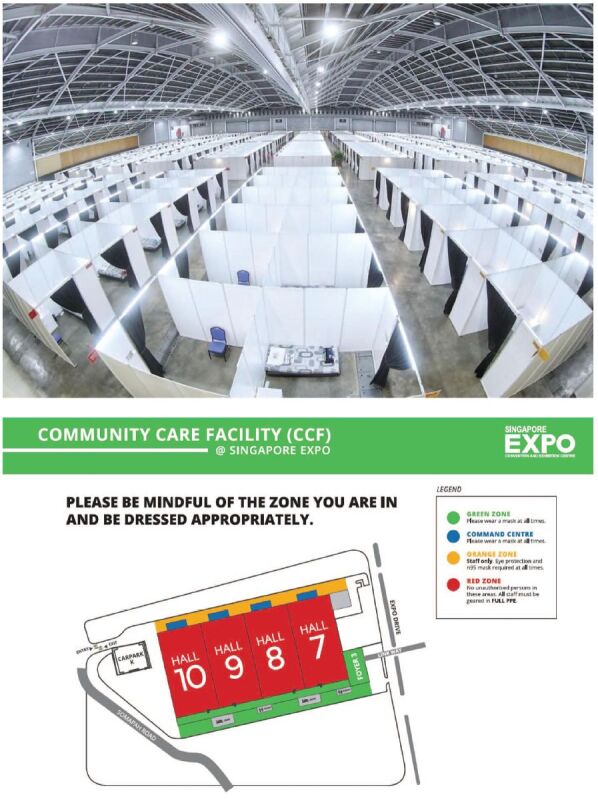
CCF = Community Care Facility; PPE = personal protective equipment. Top. CCFExpo halls 7 to 10 before patients were admitted. (Photograph courtesy of the Ministry of Health, Singapore.) Bottom. Layout plan of CCFExpo halls 7 to 10. The facility had 3 distinct areas: green, red, and orange. The green area was for rest and meals for the staff. The red area is where patients were housed. Staff entered the red area through a designated double-door entrance located at even-numbered halls and exited via odd-numbered halls. Patients were allowed to roam freely. The orange area is where patients departed busses or were picked up by ambulances. (Image courtesy of SingEx.).
Because monitoring of vital signs is resource intensive, a patient self-monitoring strategy was used. Fifteen self-monitoring stations were set up in each hall, with digital sphygmomanometers, pulse oximeters, thermometers, and computer tablets. Instructions written in several languages guided patients in using the monitors, recording their vital signs on a computer tablet, and disinfecting the station after each use without supervision. The data were evaluated twice daily by a member of the health care team situated outside the halls.
Each hall had 2 primary care medical consultation rooms with pharmacy cabinets. It also had 2 sickbays for short-term patient monitoring—for example, if a patient was awaiting transfer to a hospital or a response to treatment.
Pharmacists from Singapore General Hospital were responsible for stocking key essential medications, such as antihistamines, antitussives, antibiotics, analgesics, antihypertensives, and diabetic medications, and packaging them to facilitate dispensing at CCFExpo. Physicians prescribed and directly dispensed these drugs from the pharmacy cabinets. The electronic health record system in place monitored the pharmacy repository and ensured an adequate stockpile.
Unidirectional laminar airflow was created in the hall to prevent contamination of the surroundings. Side entrances and wall spaces were sealed, and a negative pressure of 2.5 Pa (2.4 atm) was generated, with the outflow air filtered through a HEPA (high-efficiency particulate air) system before being released into the outside environment. Two-doored anterooms were created at the hall's entry and exit points to ensure unidirectional airflow. Security cameras were placed to monitor for any unauthorized exits.
Staffing at CCFExpo
CCFExpo was operated by a team of administrators, pharmacists, 26 doctors, and 72 allied health staff (affectionately called “angels” and from various disciplines, including nursing and physiotherapy) mobilized from the SingHealth cluster. The 72 angels performed the same tasks of screening and monitoring the patients.
Round-the-clock medical care was provided, with both doctors and angels assigned to 12-hour shifts. During the day shift (8 a.m. to 8 p.m.), each hall was staffed by 3 or 4 doctors and 8 to 14 angels. During the night shift (8 p.m. to 8 a.m.), staffing was reduced to 1 doctor and 2 angels per hall.
Staff safety was paramount. All personnel had to be trained in the fitting and use of N95 masks and other personal protective equipment (PPE) before deployment. Illustrated instructions were placed at gowning and degowning stations to remind staff of the proper steps for putting on and taking off their PPE. Trainers also were placed at these stations to ensure that staff adhered to the gowning and degowning procedures. Each health care worker was allowed in the hall for a period not exceeding 2 hours over a continuous stretch. Clean areas were made available to all staff for rest periods.
To ensure the facility's safety and prevent unauthorized exit, 6 security officers were stationed in each hall during each shift. A separate security team was available if needed.
Admission of Patients to CCFExpo
The Ministry of Health (MOH) controlled the disposition of each patient with a positive COVID-19 test result (defined as a positive result on polymerase chain reaction swab testing). The MOH devised a risk-based classification system including symptoms, vital signs, age, existing comorbid conditions, National Early Warning System (NEWS) score (Appendix Figure) (4), body mass index, level of activities of daily living, radiologic findings, and date of disease onset. Although several groups of patients were considered low risk, those chosen for admission to CCFExpo generally were young and had no severe symptoms (such as dyspnea), no serious medical comorbid conditions, normal vital signs, and a NEWS score of 4 or less. The NEWS score is a composite value based on commonly used parameters (respiratory rate, oxygen saturation, supplemental oxygen requirement, temperature, blood pressure, heart rate, and level of consciousness). A score lower than 4 in a patient with acute illness indicates that he or she is at low risk for deterioration (4). Chest radiography was performed in all patients older than 35 years. If pulmonary consolidation was detected on a radiograph, the patient was transferred to a general hospital.
Appendix Figure. The NEWS scoring system.
![Appendix Figure. The NEWS scoring system. A = alert; BP = blood pressure; NEWS = National Early Warning System; P = pain; U = unresponsive; V = voice. (Image courtesy of Royal College of Physicians [4].).](https://cdn.ncbi.nlm.nih.gov/pmc/blobs/8b9d/7505018/086eb76c5bcf/aim-olf-M204746-M204746ffa1.jpg)
A = alert; BP = blood pressure; NEWS = National Early Warning System; P = pain; U = unresponsive; V = voice. (Image courtesy of Royal College of Physicians [4].).
A team of angels was tasked with screening all patients referred to the facility by the MOH for admission. Patients were evaluated for serious medical comorbid conditions (such as ischemic heart disease or renal failure) and abnormal vital signs. If any abnormality was detected, the patient was referred to a physician who decided whether they were suitable for admission to CCFExpo. Patients determined to be unsuitable were transferred to a general hospital for further care.
On admission to the facility, patients received an orientation booklet that was written in their native language and included infographics. The booklet contained information on the patient's responsibility for monitoring their own medical condition as well as the medical facilities available to them—namely, the process for obtaining a medical consultation both during and after office hours, code blue buttons, and self-monitoring stations.
Medical Consults at CCFExpo
Two medical consultation rooms were staffed by physicians from 9 a.m. to noon and 2 p.m. to 5 p.m. daily. During these times, patients could present to the consultation rooms as they would to a primary care provider in the community. For urgent after-hours consultations, patients were instructed to see a physician via teleconsultation; for emergencies, patients were instructed to press one of the code blue buttons located in highly visible areas. In addition, a hotline was created to answer any urgent queries from patients. We also actively surveyed for a secondary disease outbreak, such as chickenpox, measles, or gastroenteritis.
Although some of the physicians staffing the facility were specialists, the degree of care was kept at the primary care level. Patients who needed further investigations or were acutely ill were transferred to a general hospital via an ambulance dedicated to patients with COVID-19.
During the night (8 p.m. to 8 a.m.), only security officers manned the halls; medical staff were stationed in the green area outside the hall. For medical consults after hours, a videoconference-enabled computer terminal was placed in one of the medical consultation rooms and was kept on live stream throughout this period. A physician monitored the videoconference via a computer terminal located in the clean area. Keeping the videoconference on live stream throughout the whole period was necessary, because instructing the patients on how to set up the computer for a teleconference would be difficult.
Patients used a vital sign self-monitoring system that allowed detection of those whose condition may have been deteriorating. Each patient was instructed to measure their vital signs at a self-monitoring station at several points during the day. If a substantially abnormal sign (defined as systolic blood pressure >180 or <90 mm Hg, diastolic blood pressure >110 mm Hg, heart rate >110 beats/min, or SpO2 [oxygen saturation as measured by pulse oximetry] <94%) was noted, the patient was asked to present to the medical consult room for review. Telephone reminders were used to ensure adherence to vital sign monitoring. In the rare event a patient did not have a working mobile phone, a patient experience team was tasked with helping to secure one.
Patient Experience and Well-Being
Apart from looking after patients' health, a patient experience team was created to ensure general well-being and to maintain morale among those housed at CCFExpo. The team made sure that information was easily understood by the patients. It also provided psychological support while a medical humanities team provided language translation and translators. The group organized hairdressing and financial services, counseling, and culturally appropriate movie screenings, and ensured that dietary requirements were met. The team was also critical in preventing mass unrest within the halls. The facility had a free wireless connection so families could be kept up to date on their loved one's progress. These services were provided at no cost to patients.
Discharge
Under MOH authority, patients were discharged from all isolation facilities after day 21 of illness. The start of illness was determined by the date of onset of the first symptoms or, for asymptomatic patients, the date of the first positive swab test result. It has been demonstrated that severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) is probably not viable after the second week of illness, despite the persistence of RNA detected on polymerase chain reaction assay (5). Therefore, it was deemed unlikely that persons would be contagious after day 14 of illness, and day 21 was chosen to err on the side of caution (5, 6). Most of our patients stayed at CCFExpo for around 2 weeks, after which they were discharged to other step-down facilities to complete the remaining isolation period.
Early Patient Care Results
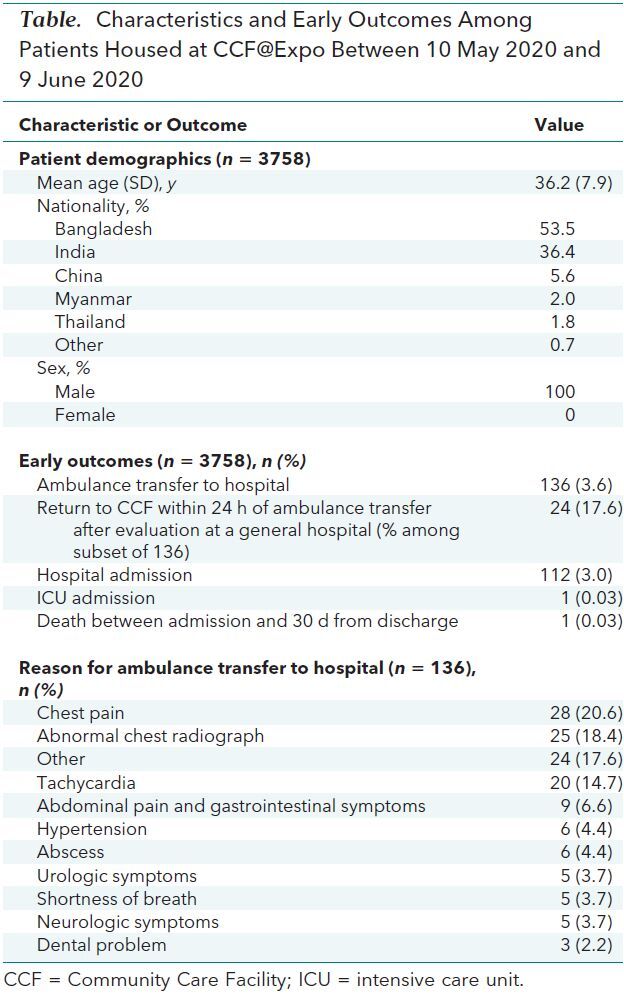
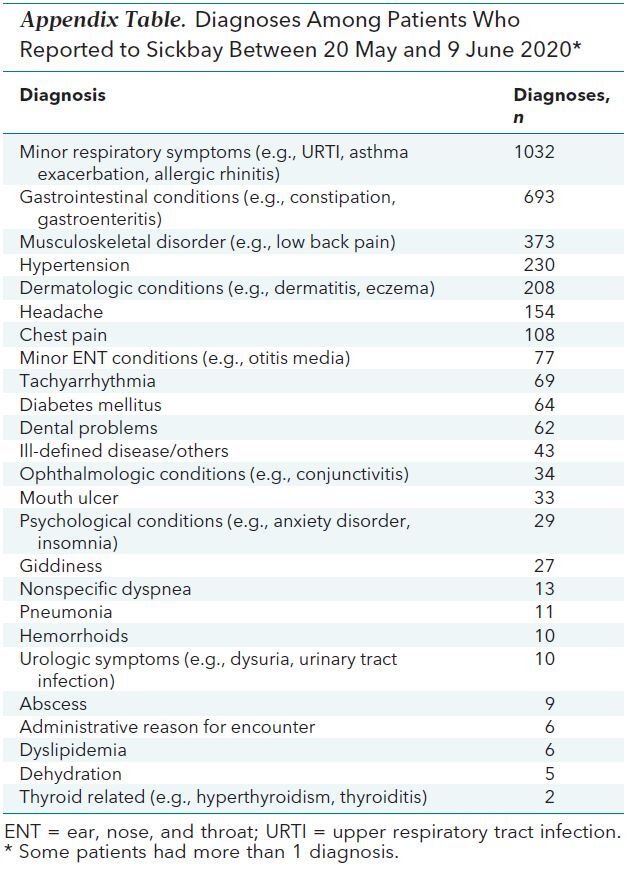
An audit of the first month's cases (10 May to 9 June 2020) showed that a total of 3758 patients were admitted to the facility during this period. Each day, there were 121.2 admissions (SD, 67.9), 124.4 discharges (SD, 106.8), 2593.5 bed occupancies (SD, 227.0), and 159.0 medical consults (SD, 31.6). Patient characteristics and early outcomes are provided in the Table. A total of 4929 medical consultations occurred during the audit period; diagnoses made during the consultations are aggregated in the Appendix Table. Patients presented for various reasons, both related and unrelated to COVID-19; the most common were minor respiratory conditions, gastrointestinal conditions, and musculoskeletal disorder. The reasons for patient transfer to a general hospital are listed in the Table.
Table. Characteristics and Early Outcomes Among Patients Housed at CCFExpo Between 10 May 2020 and 9 June 2020.
Appendix Table. Diagnoses Among Patients Who Reported to Sickbay Between 20 May and 9 June 2020*.
Of the patients admitted to CCFExpo, 3.6% (n = 136) were transferred to a general hospital (Table). Of this group, 1 patient required intensive care for post–COVID-19 pneumonia complicated by Staphylococcus aureus pyogenic myopericarditis and polymicrobial bacteremia. This patient was subsequently discharged well from the general hospital. One patient died of a massive pulmonary embolism 2 weeks after his discharge from the facility.
Adherence to vital sign monitoring was 99.3% after telephone reminders were issued. Between 31 May and 9 June 2020, a mean of 4.1 patients (SD, 2.71) presented each day with persistently abnormal vital signs requiring a consult.
Discussion
Isolation strategies may be divided broadly into institution-based and home-based isolation. The predominant problem with home-based isolation is the reliance on personal adherence. Consequently, a modeling study showed that institution-based isolation is 3 times more efficient than home-based isolation in reducing the number of COVID-19 cases (7).
Like many countries, Singapore decided to pursue an institution-based isolation strategy. Before the pandemic, acute hospitals in Singapore had a total of 11 321 beds (8), including 1100 intensive care beds (9). If we contained the disease by hospitalizing patients with COVID-19, as was the strategy adopted in Singapore during the 2003 SARS outbreak (5), the nation's health care infrastructure would have been rapidly overwhelmed.
Foreign workers made up most of the COVID-19 cases in Singapore. To control the spread of the virus, the country underwent a lockdown from 7 April to 1 June 2020, and foreign workers were confined to their dormitories.
To encourage foreign workers to report symptoms, the Ministry of Manpower issued an advisory in April 2020 mandating that they be paid their salaries, through government assistance, during the lockdown period. Workers who were diagnosed with COVID-19 and subject to treatment order under the Infectious Diseases Act were reassured that treatment would be provided at no cost them.
CCFExpo was partly modeled after the Fangcang shelter hospitals, the first large-scale COVID-19 isolation facilities, which were built quickly by modifying exhibition centers and stadiums in Wuhan, China (6–9). However, CCFExpo's design included a few unique considerations. First, it served as an isolation facility rather than a hospital. As such, patients who were identified to be at risk for deterioration were sent to a general hospital for further evaluation and monitoring. Second, the staffing level at the facility was low to avoid overwhelming the health care system. Third, the facility served a unique population—foreign workers living in crowded dormitories who were predominantly non–English speaking and had low literacy rates.
We addressed the first and second issues by admitting only patients presumed to have a low risk for death and who could participate in self-monitoring. Patients could have no serious medical comorbid conditions and had to be mostly asymptomatic.
To address the high patient–health care staff ratio, we designed the facility as an isolation unit with primary care support, rather than using the admission and consultation process typically seen in a hospital setting (detailed clerking, daily rounding). Instead, we relied on the patients to be responsible for their self-monitoring. The rapid conversion of an existing facility, together with a low patient–staff ratio, also allowed our facility to be functional within a short period.
Regarding the third issue, the patients were a unique group. Many had difficulties communicating in English, and some were illiterate. To mitigate this challenge, we created admission kits (containing screening questions for suitability for admission to the facility) that were translated into various languages and also included infographics. In the medical consultation rooms, posters containing translated phrases and infographics were plastered on the walls. If these were insufficient, telephone translators were used.
Apart from language issues, we recognized that a high level of anxiety was present among persons housed at CCFExpo. Therefore, the patient experience team canvassed the halls to collect feedback from the patients. This information led us to provide culturally appropriate food, modify lighting in the halls to mimic natural day–night lighting, and offer hairdressing services.
A substantial challenge that we faced was the switch in mindset from tertiary to primary care. Most of our team members were used to providing care in a high-volume center, and mental barriers existed early on among the team in delivering medical care at the primary level.
Overall, 1 patient died, 2 weeks after he was discharged from CCFExpo, of massive pulmonary thromboembolism after COVID-19. Even considering the young age of our patients, this death rate is substantially lower than the rates reported in most countries (10). We postulate that the reason for this low mortality is the high COVID-19 detection rate among asymptomatic persons because of compulsory mass testing of the foreign worker dormitories in Singapore.
Although mandated institution-based isolation is highly effective from a public health perspective, we acknowledge that it substantially restricts individual freedom. It also may be a disincentive for patients to come forward if they have symptoms or have been in contact with others who have tested positive for COVID-19. On a practical note, implementing these isolation measures met with little resistance, which may be a result of the collectivistic culture of Asian societies (11). However, applying such a strategy in countries with an individualistic culture (where individual freedom is more highly valued) or in less economically developed nations may be more difficult.
Nevertheless, the experience gleaned at CCFExpo shows that institution-based isolation can probably be performed safely outside the hospital setting. This approach prevents health care infrastructure from becoming overwhelmed by curtailing the spread of the virus, thereby reducing bed use in acute hospitals, without the need for a large staff.
A substantial proportion of stable patients with COVID-19 can be isolated safely outside a hospital setting with a small health care team. Isolation facilities can be created rapidly to care for patients without serious adverse outcomes. Lastly, the use of technology, telemedicine, and patient self-monitoring is effective in managing a large cohort of stable patients with COVID-19.
Footnotes
This article was published at Annals.org on 17 September 2020
* All authors contributed equally to the work reported in this article.
References
- 1. Ali SH, Foster T, Hall NL. The relationship between infectious diseases and housing maintenance in indigenous Australian households. Int J Environ Res Public Health. 2018;15. [PMID: 30545014] doi:10.3390/ijerph15122827 [DOI] [PMC free article] [PubMed]
- 2. Singapore Ministry of Health. COVID-19 Situation Report. Accessed at https://covidsitrep.moh.gov.sg on 20 June 2020.
- 3. Singapore Ministry of Health. Reorganisation of Healthcare System Into Three Integrated Clusters to Better Meet Future Healthcare Needs. Accessed at www.moh.gov.sg/news-highlights/details/reorganisation-of-healthcare-system-into-three-integrated-clusters-to-better-meet-future-healthcare-needs on 29 July 2020.
- 4. Royal College of Physicians. National Early Warning Score (NEWS): Standardising the Assessment of Acute Illness Severity in the NHS. Report of a working party. Royal Coll Physicians; 2012.
- 5. Goh KT, Cutter J, Heng BH, et al. Epidemiology and control of SARS in Singapore. Ann Acad Med Singap. 2006;35:301-16. [PMID: 16829997] [PubMed]
- 6. Chen S, Zhang Z, Yang J, et al. Fangcang shelter hospitals: a novel concept for responding to public health emergencies. Lancet. 2020;395:1305-1314. [PMID: 32247320] doi:10.1016/S0140-6736(20)30744-3 [DOI] [PMC free article] [PubMed]
- 7. Fang D, Pan S, Li Z, et al. Large-scale public venues as medical emergency sites in disasters: lessons from COVID-19 and the use of Fangcang shelter hospitals in Wuhan, China. BMJ Glob Health. 2020;5. [PMID: 32546589] doi:10.1136/bmjgh-2020-002815 [DOI] [PMC free article] [PubMed]
- 8. Shang L, Xu J, Cao B. Fangcang shelter hospitals in COVID-19 pandemic: the practice and its significance. Clin Microbiol Infect. 2020;26:976-978. [PMID: 32360781] doi:10.1016/j.cmi.2020.04.038 [DOI] [PMC free article] [PubMed]
- 9. Dickens BL, Koo JR, Wilder-Smith A, et al. Institutional, not home-based, isolation could contain the COVID-19 outbreak [Letter]. Lancet. 2020;395:1541-1542. [PMID: 32423581] doi:10.1016/S0140-6736(20)31016-3 [DOI] [PMC free article] [PubMed]
- 10. Liao S, Shao S, Chen Y, et al. Incidence and mortality of pulmonary embolism in COVID-19: a systematic review and meta-analysis. Critical Care. 2020;24:464. doi.org/10.1186/s13054-020-03175-z [DOI] [PMC free article] [PubMed]
- 11. Hofstede Insights. Country Comparison: Individualism. Accessed at www.hofstede-insights.com/country-comparison/singapore/#:~:text=In%20Individualist%20societies%20people%20are,and%20their%20direct%20family%20only.&text=Singapore%2C%20with%20a%20score%20of,other%20in%20exchange%20for%20loyalty) on 24 August 2020.


