This review summarizes current knowledge about the transmission of SARS-CoV-2. Evidence-based policies and practices should incorporate the accumulating knowledge regarding SARS-CoV-2 transmission to help educate the public and slow spread of this virus.
Abstract
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), the etiologic agent of coronavirus disease 2019 (COVID-19), has spread globally in a few short months. Substantial evidence now supports preliminary conclusions about transmission that can inform rational, evidence-based policies and reduce misinformation on this critical topic. This article presents a comprehensive review of the evidence on transmission of this virus. Although several experimental studies have cultured live virus from aerosols and surfaces hours after inoculation, the real-world studies that detect viral RNA in the environment report very low levels, and few have isolated viable virus. Strong evidence from case and cluster reports indicates that respiratory transmission is dominant, with proximity and ventilation being key determinants of transmission risk. In the few cases where direct contact or fomite transmission is presumed, respiratory transmission has not been completely excluded. Infectiousness peaks around a day before symptom onset and declines within a week of symptom onset, and no late linked transmissions (after a patient has had symptoms for about a week) have been documented. The virus has heterogeneous transmission dynamics: Most persons do not transmit virus, whereas some cause many secondary cases in transmission clusters called “superspreading events.” Evidence-based policies and practices should incorporate the accumulating knowledge about transmission of SARS-CoV-2 to help educate the public and slow the spread of this virus.
Key Summary Points
Respiratory transmission is the dominant mode of transmission.
Vertical transmission occurs rarely; transplacental transmission has been documented.
Cats and ferrets can be infected and transmit to each other, but there are no reported cases to date of transmission to humans; minks transmit to each other and to humans.
Direct contact and fomite transmission are presumed but are likely only an unusual mode of transmission.
Although live virus has been isolated from saliva and stool and viral RNA has been isolated from semen and blood donations, there are no reported cases of SARS-CoV-2 transmission via fecal–oral, sexual, or bloodborne routes. To date, there is 1 cluster of possible fecal–respiratory transmission.
Transmission of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), which causes coronavirus disease 2019 (COVID-19), requires that a minimum but as yet unknown dose of replication-competent virus be delivered to a vulnerable anatomical site in a susceptible host. A combination of viral, host, and environmental characteristics affect transmission. In this review, we discuss the evidence about the relative importance of these factors.
Methods
To review the extensive accumulating evidence about the transmission of SARS-CoV-2, we attempt to answer the following key questions. First, what is the evidence for the environmental viability of the virus in experimental and real-world settings? Second, what viral and host factors affect transmission? Third, what is the evidence for various modes of transmission? Fourth, what is the period of infectiousness for a person with SARS-CoV-2 infection? Fifth, what are the population transmission dynamics, and what is the role of superspreading events?
Data Sources
We manually searched electronic databases, including LitCovid (a literature hub for articles related to COVID-19 indexed on PubMed) and the medRxiv preprint server, for English-language titles and abstracts published from 1 January through 7 September 2020; we also searched reference lists of relevant articles and institutional or governmental reports of SARS-CoV-2 transmission.
Study Selection
Articles were included if they provided relevant information on the key questions. Selected articles included laboratory-based studies of the virus, instructive case and cluster reports, and other observational or modeling studies. Reviewers critically assessed each of the included studies, which had to be self-consistent and detailed enough to support their major conclusions. Limitations of important studies are noted when the studies are cited.
Data Extraction
One reviewer extracted data, and another verified accuracy.
Limitations
It is not possible to assess the exact route of transmission for many transmission events because risk factors often overlap; for example, persons may be exposed through both respiratory droplets and surface contamination.
Environmental Viability of the Virus
In experimental conditions, viable SARS-CoV-2 was cultured from aerosols (fine particles suspended in the air) and various surfaces after inoculation with 105.25 50% tissue culture infectious dose per milliliter (TCID50/mL) for aerosols and 105 TCID50/mL for surfaces, correlating to a reverse transcriptase polymerase chain reaction cycle threshold of 22 to 24, a typical value obtained from a nasopharyngeal sample of a person with COVID-19. Cycle thresholds correlate inversely to viral load, so higher cycle thresholds indicate lower viral loads (1). Viral RNA decayed steadily over time in all conditions, although viable virus was isolated for up to 3 hours from aerosols and up to 72 hours from various surfaces; the longest reported viability was on plastics and stainless steel, with half-lives around 6 hours (1).
A similar experiment found that infectious virus could be isolated from various surfaces after inoculation with a much larger amount of virus (7 to 8 log units TCID50/mL) (2). The same study found that the virus was highly stable at low temperatures but sensitive to heat, with inactivation of the virus in 5 minutes at 70 °C. In addition, SARS-CoV-2 could not be cultured after incubation with various disinfectants, confirming experimentally the effectiveness of cleaning procedures.
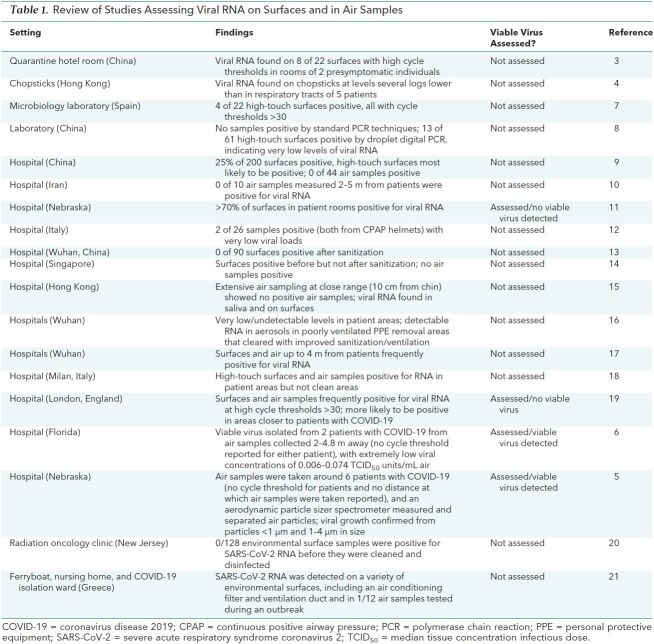
In real-world settings, studies have identified SARS-CoV-2 RNA from samples taken from contaminated environmental surfaces, most commonly high-touch surfaces (Table 1). Viral RNA levels are markedly lower on environmental surfaces than in the nasopharynx of source individuals, as shown in studies of a quarantine hotel and used dining utensils (3, 4). The few studies that have assessed the presence of replication-competent virus with culture have isolated it rarely in air particles of varying size (5, 6).
Table 1. Review of Studies Assessing Viral RNA on Surfaces and in Air Samples.
Viral and Host Factors Affecting Transmission
Binding of the viral spike (S) protein to the host angiotensin-converting enzyme 2 (ACE2) receptor is a critical step for cell entry, and as a result, host ACE2 distribution determines viral tropism (22, 23). Viral load is highest in the upper respiratory tract (nasopharynx and oropharynx) early in disease and then increases in the lower respiratory tract (sputum), suggesting that the upper respiratory tract is the usual initial site of viral replication, with subsequent descending infection (24).
Susceptibility to SARS-CoV-2 infection increases with age; children younger than 10 years are around half as susceptible as adults (25–28). Viral RNA testing of household contacts in Iceland showed 6.7% and 13.7% positivity in children and adults, respectively, and testing in Wuhan, China, showed 4% and 17.1% positivity (29, 30). Decreased ACE2 expression in children compared with adults may partly explain the lower susceptibility seen in children (31, 32).
The relative probability of transmission from an infected child compared with that from an adult is not well understood. Replication-competent virus is readily isolated from children who are infected, and there are conflicting reports about the relative viral loads in children compared with adults, with some studies not controlling for time since symptom onset, a key determinant of viral load (32–35). Multiple large contact tracing studies have suggested a lower secondary attack rate for young children, but these must be interpreted with caution because children are less likely to have symptomatic disease and therefore less likely to be identified as index cases (35–38). Moreover, these studies predominantly took place during periods of school closures, which may have had a confounding effect on the likelihood of a child being an index case.
One study of households in the United States found that household contacts of patients with immunocompromising conditions and COVID-19 had increased risk for infection, a finding that has not yet been replicated but which suggests that this population may be more likely to transmit the virus (39).
Viral factors may also contribute to transmissibility. For instance, a marked increase in the prevalence of SARS-CoV-2 bearing a D614G mutation has been noted over time (40). Whether this mutation provides a selective advantage to the virus has been debated (41). It has now been shown that this variant infects human ACE2 cell lines more efficiently than wild-type virus, that progeny virus has increased expression of S protein, that the S protein has a higher rate of binding to ACE2, and that in vivo viral loads may be higher for this variant (40, 42–44).
Evidence for Various Modes of Transmission
To date, conclusive evidence exists for respiratory transmission of SARS-CoV-2 and transmission to and between certain domestic and farm animals, as well as rare vertical transmission. Direct contact or fomite transmission is suspected and may occur in some cases. Sexual, fecal–oral, and bloodborne transmission are theorized but have not been documented.
Respiratory Transmission
When a virus spreads through respiratory transmission, it does so either with virions suspended on large droplets or fine aerosols expelled from the respiratory tract of the primary case patient. Droplets are classically considered to be particles larger than 5 μm that fall to the ground within about 6 feet and aerosols to be particles smaller than 5 μm that can remain suspended in the air for prolonged periods; however, this dichotomization may be an oversimplification, and distinguishing droplet and aerosol transmission is difficult in clinical settings (45–47).
The dominant route of transmission of SARS-CoV-2 is respiratory (48). Growing evidence indicates that infectious virus can be found in aerosols and in exhaled breath samples (5, 6, 49), and it is likely that under certain circumstances, including during aerosol-generating procedures, while singing, or in indoor environments with poor ventilation, the virus may be transmitted at a distance through aerosols.
Nevertheless, there is abundant evidence that proximity is a key determinant of transmission risk (50, 51). A detailed contact tracing study of train passengers that included 2334 index cases and 72 093 close contacts found that the secondary attack rate was closely linked to both the distance between seats and the duration of shared travel (52). In a cluster investigation of 112 cases linked to fitness classes in South Korea, high-intensity exercise in densely packed rooms yielded the most cases; a less crowded Pilates class with a presymptomatic instructor, on the other hand, had no associated secondary cases (53). That proximity so clearly increases risk for infection suggests that classic droplet transmission is more important than aerosol transmission (51).
The role of ventilation in preventing or promoting spread also highlights the importance of respiratory transmission. In a study of household transmission in China, opening windows to allow better air movement led to lower secondary household transmission (54). Poor ventilation has been implicated in numerous transmission clusters, including those in bars, churches, and other locations (55–57). By contrast, such events have rarely occurred outside, and then only in the context of crowding (58–60). In 1 illustrative study of individuals at a religious event who traveled on 2 buses with poor ventilation, 35% of those on 1 bus acquired infection compared with none on the other bus, again highlighting the importance of ventilation (61). In this case, proximity to the single known index patient did not correlate with risk for infection.
In addition, studies have found that masking, both in health care settings and in the community, decreases transmission of SARS-CoV-2 (51, 62–65). A study in China found that mask use in the household before symptom development markedly reduced risk for household transmission (54). All of this evidence supports the dominant role of respiratory spread of this virus.
Direct Contact and Fomites
There is currently no conclusive evidence for fomite or direct contact transmission of SARS-CoV-2 in humans. Rhesus macaques can be infected with SARS-CoV-2 through direct conjunctival inoculation but develop less severe pulmonary disease than macaques inoculated through an intratracheal route (66).
Reports suggesting fomite transmission are circumstantial. For example, in a cluster of infections associated with a mall in China, several affected persons reported no direct contact with other case patients (67). The investigators noted that these individuals used shared common facilities (such as elevators and restrooms) and proposed fomite or respiratory transmission in those settings. In a detailed investigation of a large nosocomial outbreak linked to 119 confirmed cases at a hospital in South Africa, fomite transmission was proposed given the separated distribution of cases in multiple wards (68). However, the hospital did not have a universal mask policy at the time of the outbreak, there was no special ventilation, and the burden of infection among health care workers was substantial. As a result, respiratory transmission from infected staff cannot be excluded. As noted in the description of all known transmission clusters in Japan, it can be difficult to identify primary cases in large health care–associated outbreaks (57). In the case of a suspected transmission during an evacuation flight, the person who acquired infection reportedly wore an N95 mask at all times except when using a toilet that was shared with another passenger with asymptomatic infection (69).
Poor hand hygiene was associated with increased risk for infection among health care workers, and daily use of chlorine or ethanol cleaning products in the household was associated with decreased risk (54, 70). Although this might indirectly suggest direct contact or fomite spread, it can be difficult to tease out the relative importance of simultaneous interventions because, for example, excellent hand hygiene may be associated with better infection control practices overall. As will be discussed in the next section, live virus can be isolated after the period of infectiousness, which suggests a minimum necessary inoculum to initiate infection (71, 72). On the basis of currently available data, we suspect that the levels of viral RNA or live virus transiently remaining on surfaces are unlikely to cause infection, especially outside of settings with known active cases.
Domestic Pets and Farm Animals
Several studies have documented that SARS-CoV-2 can infect domestic animals, including cats, dogs, and ferrets (73–76). The virus replicates well in cats (but not in dogs) and is transmissible between cats and ferrets (75, 77). There are no confirmed cases of transmission from domestic pets to humans. Minks are susceptible to SARS-CoV-2 infection and are farmed in some areas where cases of transmission from minks to human farm workers is suspected (78, 79).
Vertical Transmission
Many studies have evaluated the possibility of vertical transmission of SARS-CoV-2 (80). There are several reports of positive SARS-CoV-2 IgM in neonates (81, 82). Although IgM does not cross the placenta, and thus its presence may indicate in utero infection, IgM testing is prone to false positivity, particularly in the setting of significant inflammation (83). There are also several reports of early nasopharyngeal positivity on polymerase chain reaction testing after delivery in neonates, including a description of 3 infants with positive results on day 2 of life and another of an infant with positive results 16 hours after delivery (84, 85). Several case reports have found placental infection by SARS-CoV-2, and 1 has shown transplacental transmission (86–89). In addition, breast milk can harbor viral RNA, although no confirmed transmissions to infants from breast milk have been reported (90–92). Taken together, these studies suggest that vertical transmission of SARS-CoV-2 rarely occurs.
Fecal–Oral (or Fecal Aerosol) Transmission
Fecal–oral transmission was theorized early in the outbreak because of the known high concentration of ACE2 receptors in the small bowel (93). No evidence currently supports fecal–oral transmission in humans, and intragastric inoculation of SARS-CoV-2 in macaques did not result in infection (94). Although viral RNA is commonly detected in stool, live virus has only rarely been isolated (95–99). This has led some to wonder whether viral aerosolization with toilet flushing could lead to transmission (100). In February 2020, there were news reports of an outbreak from possible fecal aerosol transmission at a multistory apartment complex in Hong Kong; however, an investigation showed that the secondary case patients were likely infected during a dinner party (101). One study did find low detectable levels of RNA in air samples near patient toilets at a hospital in Wuhan, although isolation of live virus was not assessed (16). The spatial distribution of a cluster of 3 infected families living in vertically aligned apartments connected by drainage pipes in a high-rise apartment building in Guangzhou, China, as well as the presence of viral RNA in another vertically aligned, unoccupied apartment, suggests the possibility of fecal aerosol transmission in rare cases (102). Taken together, given how rarely live virus has been isolated from stool, the low levels of replication-competent virus in stool that might be aerosolized from toilet flushing seem highly unlikely to cause infection except under unusual or extraordinary circumstances.
Sexual Transmission
No current evidence supports sexual transmission of SARS-CoV-2. Viral RNA has been found in semen, although infectious virus has not been isolated (103). Vaginal fluid has been negative except in a single case that reported RNA with a low viral level (104, 105). One study reported lack of transmission to a discordant partner among 5 couples who remained sexually active while 1 partner was in the period of infectiousness (106). For linked transmissions between sexual partners, exclusion of respiratory transmission would not be possible.
Bloodborne Transmission
The proportion of persons with viral RNA detectable in blood is currently unknown. An early study found viral RNA in only 3 of 307 blood specimens (95). Another study detected viral RNA in 32.9% of 85 blood samples from symptomatic persons, including 22 of 28 from those requiring hospitalization (107). In another study, viral RNA was detected in 27% (19 of 71) of hospitalized patients (44% of those on a ventilator, 19% of those receiving supplemental oxygen by nasal cannula, and 0% of those on ambient air) and 13% (2 of 16) of outpatients with COVID-19 (108). Viral RNA was found in blood from 4 blood donors without symptoms. The samples were discarded and not administered to other patients (109). To date, no replication-competent virus has been isolated from blood samples, and there are no documented cases of bloodborne transmission.
Transmission Determinants by Symptoms and Timing: the “Period of Infectiousness”
Persons who have SARS-CoV-2 with or without symptoms can transmit. Those without symptoms may be presymptomatic, or they may remain asymptomatic. Transmission can occur from persistently asymptomatic persons, although they seem to be less likely to transmit, and when they are most infectious is currently unknown (110–114). Data are mixed about the dynamics of viral shedding in those with persistently asymptomatic infection (112, 115, 116).
Among those who develop symptoms, 1 report of 3410 close contacts of 391 case patients in China found that the secondary attack rate increased with the severity of the index case and that the specific symptoms of fever and expectoration were associated with secondary infections (113). In another study, researchers determined that transmissibility peaks around 1 day before symptom onset by analyzing a group of 77 transmission pairs (117). Assuming an incubation period of 5.2 days, they estimated that infectiousness started 2.3 days before symptom onset, peaked around a day before symptom onset, and declined rapidly within 7 days (117, 118). In their cohort, they estimated that 44% of secondary cases were acquired from persons who were presymptomatic at the time of transmission. Other studies have replicated these important findings (119–121). Modeling using observed viral load kinetics further supports these findings, suggesting that the threshold viral load for a 50% probability of transmission is approximately 107.5 viral RNA copies/mL and that infected persons are likely to be above this threshold for only about 1 day (122). The amount of presymptomatic transmission varies between populations on the basis of the extent of active case findings and isolation and quarantine of close contacts. The proportion of presymptomatic transmission will be higher in areas without case tracking and isolation of contacts.
Viral loads of SARS-CoV-2 in the respiratory tract decrease rapidly after symptom onset, with higher loads shifting from the upper to the lower respiratory tract (24, 123, 124). Patients with severe disease have higher respiratory viral loads than those with mild disease, although all loads decline with time (125). Researchers from China estimated the duration of RNA shedding from various sites based on detailed sample analysis of 49 patients with COVID-19 and reported a median duration of shedding from the nasopharynx of 22 days for mild and 33 days for severe cases, with some persons shedding for longer than 2 months (97). Figure 1 shows the period of infectiousness and respiratory tract viral load in cycle threshold with time.
Figure 1. The period of infectiousness for immunocompetent, symptomatic adults (dotted line) and respiratory tract viral load with time (solid line).
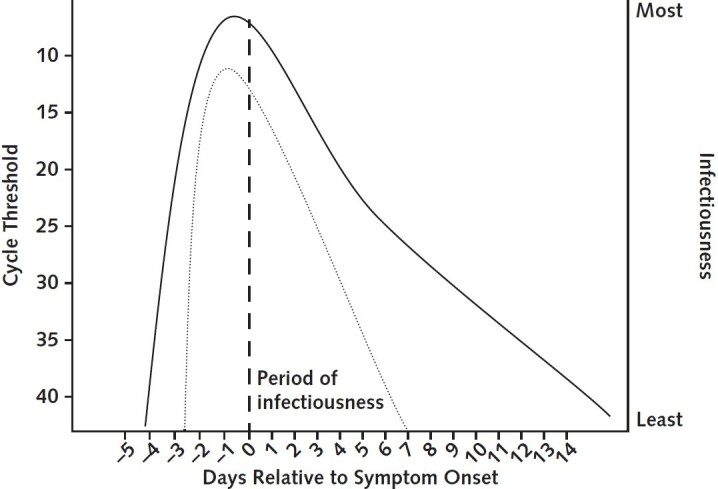
The vertical dashed line represents symptom onset.
Of note, the period of infectiousness is far shorter than the duration of detectable RNA shedding. For mild to moderate cases, infectious virus can be isolated from samples only up until about day 8 of symptoms. Multiple studies have found virtually no viable virus in patients with mild or moderate disease after 10 days of symptoms despite frequent ongoing RNA shedding (24, 126, 127). Higher viral loads are associated with increased likelihood of isolation of infectious virus (24, 127). In a study that included patients from 0 to 21 days after symptom onset, viable virus was isolated in 26 of 90 samples but no viral growth was found when the cycle threshold was greater than 24 or the patient had had more than 8 days of symptoms (128). A study of a major outbreak at a nursing facility in Washington found viable virus 6 days before symptom onset through 9 days after symptom onset (129).
It may be possible to isolate infectious virus longer in hospitalized patients who have severe disease or are critically ill. A group from the Netherlands evaluated 129 hospitalized patients, including 89 who required intensive care, and collected samples from the upper and lower respiratory tracts (71). Isolation of infectious virus occurred a median of 8 days after symptom onset. The probability of isolation of infectious virus was less than 5% after 15.2 days and decreased with time after symptom onset, lower viral loads, and higher neutralizing antibody titers; the latest isolation of infectious virus was 20 days after symptom onset.
Despite late isolation of infectious virus, no late transmissions have been documented, including in health care settings. Perhaps the most detailed real-world confirmation of this period of infectiousness comes from a detailed contact tracing study from Taiwan that found no linked transmissions after index patients had had symptoms for at least 6 days (72). In this study, nearly 3000 close contacts (including nearly 700 health care workers not wearing appropriate personal protective equipment at the time of exposure) of 100 confirmed case patients were followed closely. Hundreds of health care worker exposures occurred after an index patient had had symptoms for at least 6 days, and no late transmissions were found, even in health care settings.
A helpful case report from Hong Kong described a patient with unrecognized COVID-19 who was admitted to a general ward for 35 hours before intubation for respiratory failure (130). Seven staff and 10 patients had close contact, and none developed COVID-19 or had a positive test result for SARS-CoV-2 during follow-up. Of note, the patient had had symptoms for 7 days by the time of admission, and although he had a relatively high viral load—in the range where infectious virus has been isolated in other studies—he did not transmit. Despite these high-risk interactions and relatively high viral load, he may have been outside the period of infectiousness.
Population-Level Transmission Dynamics, Transmission Heterogeneity, and the Role of Superspreading Events
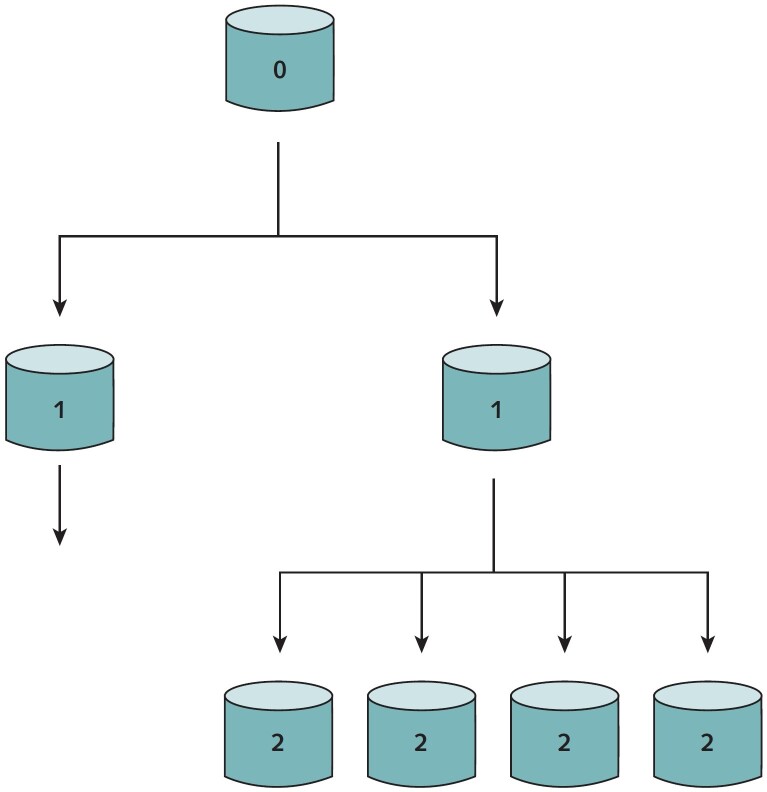
In infectious disease transmission dynamics, the basic reproductive number, or R0, describes the average number of secondary cases generated from an index case in an entirely susceptible population. Estimates for the R0 of SARS-CoV-2 have ranged from 2 to 3 (131, 132). The number of secondary transmissions per index case can show levels of heterogeneity (Figure 2). Overdispersion refers to transmission with high heterogeneity. In such cases, most index cases do not lead to any secondary transmissions and a smaller minority lead to many secondary transmissions in clusters, in what are sometimes called “superspreading events” (133).
Figure 2. A branching schematic of heterogeneous (i.e., overdispersed) transmission with R0 = 2.
The index case transmits to 2 secondary cases. One secondary case has no further transmissions, and the other secondary case transmits to 4 tertiary cases.
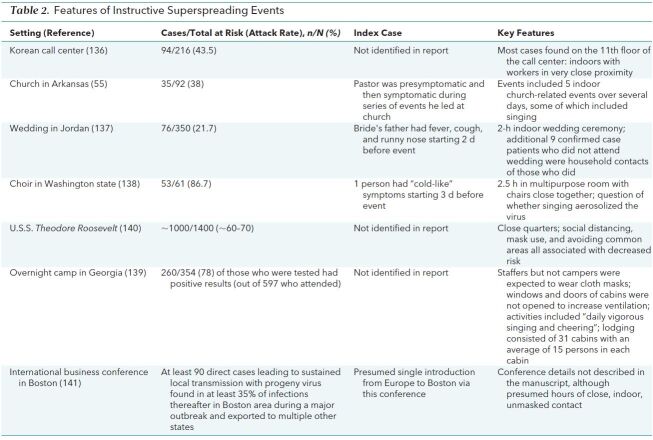
There is mounting evidence that SARS-CoV-2 transmission is highly overdispersed. Contact tracing investigations during the early epidemic in China estimated that 80% of secondary infections arose from 8.9% of index cases (134). This has been further supported by a modeling analysis that used the expected number of local and imported cases in all countries to estimate that approximately 10% of cases lead to 80% of secondary transmissions, a phylodynamic study that used SARS-CoV-2 genetic sequences in Israel to estimate that fewer than 10% of infections lead to 80% of secondary cases, and another detailed contact tracing report of all identified clusters of infection in Hong Kong that found that approximately 20% of infections caused 80% of secondary transmissions (56, 131, 135). In this last report, 1 transmission cluster accounted for more than 10% of all known cases in Hong Kong at the time and 30% of locally acquired cases. Highly publicized superspreading events have occurred, including outbreaks at a Korean call center, a church in Arkansas, a wedding in Jordan, a choir practice in Washington, and an overnight camp in Georgia (Table 2) (55, 136–141). As noted in an analysis of COVID-19 cases in Japan, transmission clusters are frequently characterized by presymptomatic and young adult index cases in settings associated with heavy breathing in close proximity (57). A systematic review of transmission clusters found that most occurred indoors (60). High viral load in the index case at the time of transmission is presumed to be important, but whether other specific host factors contribute to superspreading events remains unknown.
Table 2. Features of Instructive Superspreading Events.
The household is another extremely important site of transmission for SARS-CoV-2, with a meta-analysis of 40 studies finding an overall household secondary attack rate of 18.8% (95% CI, 15.4% to 22.2%) (142). In a demonstrative contact tracing study from South Korea including nearly 60 000 contacts of more than 5700 case patients, the attack rate among household contacts was 11.8%, compared with 1.0% for nonhousehold contacts (37). Household attack rates vary with community prevalence and household factors like age distribution, density, and ventilation in the living space (54, 143). In addition, results from serologic and RNA testing may differ depending on timing and characteristics of tests (144). After superspreading events, additional transmission frequently occurs among contacts living in the same household.
Conclusions
In the midst of the COVID-19 pandemic, initial uncertainty about transmission, at times fueled by waves of misinformation or overinterpretation of in vitro studies, understandably led to fear among both health care workers and the general public. Through the extraordinary dedication of health care workers, public health leaders, and scientists around the globe, and with rapid knowledge sharing, we have made remarkable progress in our understanding of transmission of this virus and how to reduce its spread. The accumulated evidence suggests that most transmission is respiratory, with virus suspended either on droplets or, less commonly, on aerosols. Transmission dynamics are heterogeneous, with a major role for superspreading events in sustaining the epidemic. These events often include persons in close proximity in indoor settings with poor ventilation for extended periods. We must continue to stay up to date with the new and emerging evidence and work quickly to revise our policies to reflect this new information.
Footnotes
This article was published at Annals.org on 17 September 2020
* Drs. Meyerowitz and Richterman contributed equally to this work.
References
- 1. van Doremalen N, Bushmaker T, Morris DH, et al. Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1 [Letter]. N Engl J Med. 2020;382:1564-1567. [PMID: 32182409] doi:10.1056/NEJMc2004973 [DOI] [PMC free article] [PubMed]
- 2. Chin AWH, Chu JTS, Perera MRA, et al. Stability of SARS-CoV-2 in different environmental conditions. Lancet Microbe. 2020;1:e10. [PMID: 32835322] doi:10.1016/S2666-5247(20)30003-3 [DOI] [PMC free article] [PubMed]
- 3. Jiang FC, Jiang XL, Wang ZG, et al. Detection of severe acute respiratory syndrome coronavirus 2 RNA on surfaces in quarantine rooms. Emerg Infect Dis. 2020;26. [PMID: 32421495] doi:10.3201/eid2609.201435 [DOI] [PMC free article] [PubMed]
- 4. Lui G, Lai CKC, Chen Z, et al. SARS-CoV-2 RNA detection on disposable wooden chopsticks, Hong Kong [Letter]. Emerg Infect Dis. 2020;26. [PMID: 32491982] doi:10.3201/eid2609.202135 [DOI] [PMC free article] [PubMed]
- 5. Santarpia JL, Herrera VL, Rivera DN, et al. The infectious nature of patient-generated SARS-CoV-2 aerosol. medRxiv. Preprint posted online 21 July 2020. doi:10.1101/2020.07.13.20041632
- 6. Lednicky JA, Lauzardo M, Fan ZH, et al. Viable SARS-CoV-2 in the air of a hospital room with COVID-19 patients. medRxiv. Preprint posted online 4 August 2020. doi:10.1101/2020.08.03.20167395 [DOI] [PMC free article] [PubMed]
- 7. Bloise I, Gómez-Arroyo B, García-Rodríguez J; SARS-CoV-2 Working Group. Detection of SARS-CoV-2 on high-touch surfaces in a clinical microbiology laboratory [Letter]. J Hosp Infect. 2020;105:784-786. [PMID: 32422312] doi:10.1016/j.jhin.2020.05.017 [DOI] [PMC free article] [PubMed]
- 8. Lv J, Yang J, Xue J, et al. Detection of SARS-CoV-2 RNA residue on object surfaces in nucleic acid testing laboratory using droplet digital PCR. Sci Total Environ. 2020;742:140370. [PMID: 32619841] doi:10.1016/j.scitotenv.2020.140370 [DOI] [PMC free article] [PubMed]
- 9. Wu S, Wang Y, Jin X, et al. Environmental contamination by SARS-CoV-2 in a designated hospital for coronavirus disease 2019. Am J Infect Control. 2020;48:910-914. [PMID: 32407826] doi:10.1016/j.ajic.2020.05.003 [DOI] [PMC free article] [PubMed]
- 10. Faridi S, Niazi S, Sadeghi K, et al. A field indoor air measurement of SARS-CoV-2 in the patient rooms of the largest hospital in Iran. Sci Total Environ. 2020;725:138401. [PMID: 32283308] doi:10.1016/j.scitotenv.2020.138401 [DOI] [PMC free article] [PubMed]
- 11. Santarpia JL, Rivera DN, Herrera VL, et al. Aerosol and surface contamination of SARS-CoV-2 observed in quarantine and isolation care. Sci Rep. 2020;10:12732. [PMID: 32728118] doi:10.1038/s41598-020-69286-3 [DOI] [PMC free article] [PubMed]
- 12. Colaneri M, Seminari E, Novati S, et al; COVID19 IRCCS San Matteo Pavia Task Force. Severe acute respiratory syndrome coronavirus 2 RNA contamination of inanimate surfaces and virus viability in a health care emergency unit. Clin Microbiol Infect. 2020;26:1094.e1-1094.e5. [PMID: 32450255] doi:10.1016/j.cmi.2020.05.009 [DOI] [PMC free article] [PubMed]
- 13. Lai X, Wang M, Qin C, et al. Coronavirus disease 2019 (COVID-2019) infection among health care workers and implications for prevention measures in a tertiary hospital in Wuhan, China. JAMA Netw Open. 2020;3:e209666. [PMID: 32437575] doi:10.1001/jamanetworkopen.2020.9666 [DOI] [PMC free article] [PubMed]
- 14. Ong SWX, Tan YK, Chia PY, et al. Air, surface environmental, and personal protective equipment contamination by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) from a symptomatic patient. JAMA. 2020. [PMID: 32129805] doi:10.1001/jama.2020.3227 [DOI] [PMC free article] [PubMed]
- 15. Cheng VC, Wong SC, Chan VW, et al. Air and environmental sampling for SARS-CoV-2 around hospitalized patients with coronavirus disease 2019 (COVID-19). Infect Control Hosp Epidemiol. 2020:1-8. [PMID: 32507114] doi:10.1017/ice.2020.282 [DOI] [PMC free article] [PubMed]
- 16. Liu Y, Ning Z, Chen Y, et al. Aerodynamic analysis of SARS-CoV-2 in two Wuhan hospitals. Nature. 2020;582:557-560. [PMID: 32340022] doi:10.1038/s41586-020-2271-3 [DOI] [PubMed]
- 17. Guo ZD, Wang ZY, Zhang SF, et al. Aerosol and surface distribution of severe acute respiratory syndrome coronavirus 2 in hospital wards, Wuhan, China, 2020. Emerg Infect Dis. 2020;26:1583-1591. [PMID: 32275497] doi:10.3201/eid2607.200885 [DOI] [PMC free article] [PubMed]
- 18. Razzini K, Castrica M, Menchetti L, et al. SARS-CoV-2 RNA detection in the air and on surfaces in the COVID-19 ward of a hospital in Milan, Italy. Sci Total Environ. 2020;742:140540. [PMID: 32619843] doi:10.1016/j.scitotenv.2020.140540 [DOI] [PMC free article] [PubMed]
- 19. Zhou J, Otter JA, Price JR, et al. Investigating SARS-CoV-2 surface and air contamination in an acute healthcare setting during the peak of the COVID-19 pandemic in London. Clin Infect Dis. 2020. [PMID: 32634826] doi:10.1093/cid/ciaa905 [DOI] [PMC free article] [PubMed]
- 20. Jan I, Chen K, Sayan M, et al. Prevalence of surface contamination with SARS-CoV-2 in a radiation oncology clinic. JAMA Oncol. 2020. [PMID: 32852509] doi:10.1001/jamaoncol.2020.3552 [DOI] [PMC free article] [PubMed]
- 21. Mouchtouri VA, Koureas M, Kyritsi M, et al. Environmental contamination of SARS-CoV-2 on surfaces, air-conditioner and ventilation systems. Int J Hyg Environ Health. 2020;230:113599. [PMID: 32823069] doi:10.1016/j.ijheh.2020.113599 [DOI] [PMC free article] [PubMed]
- 22. Hoffmann M, Kleine-Weber H, Schroeder S, et al. SARS-CoV-2 cell entry depends on ACE2 and TMPRSS2 and is blocked by a clinically proven protease inhibitor. Cell. 2020;181:271-280.e8. [PMID: 32142651] doi:10.1016/j.cell.2020.02.052 [DOI] [PMC free article] [PubMed]
- 23. Walls AC, Park YJ, Tortorici MA, et al. Structure, function, and antigenicity of the SARS-CoV-2 spike glycoprotein. Cell. 2020;181:281-292.e6. [PMID: 32155444] doi:10.1016/j.cell.2020.02.058 [DOI] [PMC free article] [PubMed]
- 24. Wölfel R, Corman VM, Guggemos W, et al. Virological assessment of hospitalized patients with COVID-2019. Nature. 2020;581:465-469. [PMID: 32235945] doi:10.1038/s41586-020-2196-x [DOI] [PubMed]
- 25. Jing QL, Liu MJ, Zhang ZB, et al. Household secondary attack rate of COVID-19 and associated determinants in Guangzhou, China: a retrospective cohort study. Lancet Infect Dis. 2020. [PMID: 32562601] doi:10.1016/S1473-3099(20)30471-0 [DOI] [PMC free article] [PubMed]
- 26. Rosenberg ES, Dufort EM, Blog DS, et al; New York State Coronavirus 2019 Response Team. COVID-19 testing, epidemic features, hospital outcomes, and household prevalence, New York State—March 2020. Clin Infect Dis. 2020. [PMID: 32382743] doi:10.1093/cid/ciaa549 [DOI] [PMC free article] [PubMed]
- 27. Zhang J, Litvinova M, Liang Y, et al. Changes in contact patterns shape the dynamics of the COVID-19 outbreak in China. Science. 2020;368:1481-1486. [PMID: 32350060] doi:10.1126/science.abb8001 [DOI] [PMC free article] [PubMed]
- 28. Davies NG, Klepac P, Liu Y, et al; CMMID COVID-19 working group. Age-dependent effects in the transmission and control of COVID-19 epidemics. Nat Med. 2020;26:1205-1211. [PMID: 32546824] doi:10.1038/s41591-020-0962-9 [DOI] [PubMed]
- 29. Gudbjartsson DF, Helgason A, Jonsson H, et al. Spread of SARS-CoV-2 in the Icelandic population. N Engl J Med. 2020;382:2302-2315. [PMID: 32289214] doi:10.1056/NEJMoa2006100 [DOI] [PMC free article] [PubMed]
- 30. Li W, Zhang B, Lu J, et al. The characteristics of household transmission of COVID-19. Clin Infect Dis. 2020. [PMID: 32301964] doi:10.1093/cid/ciaa450 [DOI] [PMC free article] [PubMed]
- 31. Bunyavanich S, Do A, Vicencio A. Nasal gene expression of angiotensin-converting enzyme 2 in children and adults. JAMA. 2020. [PMID: 32432657] doi:10.1001/jama.2020.8707 [DOI] [PMC free article] [PubMed]
- 32. Yonker LM, Neilan AM, Bartsch Y, et al. Pediatric SARS-CoV-2: clinical presentation, infectivity, and immune responses. J Pediatr. 2020. [PMID: 32827525] doi:10.1016/j.jpeds.2020.08.037 [DOI] [PMC free article] [PubMed]
- 33. L'Huillier AG, Torriani G, Pigny F, et al. Culture-competent SARS-CoV-2 in nasopharynx of symptomatic neonates, children, and adolescents. Emerg Infect Dis. 2020;26. [PMID: 32603290] doi:10.3201/eid2610.202403 [DOI] [PMC free article] [PubMed]
- 34. Heald-Sargent T, Muller WJ, Zheng X, et al. Age-related differences in nasopharyngeal severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) levels in patients with mild to moderate coronavirus disease 2019 (COVID-19). JAMA Pediatr. 2020. [PMID: 32745201] doi:10.1001/jamapediatrics.2020.3651 [DOI] [PMC free article] [PubMed]
- 35. Maltezou HC, Vorou R, Papadima K, et al. Transmission dynamics of SARS-CoV-2 within families with children in Greece: a study of 23 clusters. J Med Virol. 2020. [PMID: 32767703] doi:10.1002/jmv.26394 [DOI] [PMC free article] [PubMed]
- 36. Posfay-Barbe KM, Wagner N, Gauthey M, et al. COVID-19 in children and the dynamics of infection in families. Pediatrics. 2020;146. [PMID: 32457213] doi:10.1542/peds.2020-1576 [DOI] [PubMed]
- 37. Park YJ, Choe YJ, Park O, et al; COVID-19 National Emergency Response Center, Epidemiology and Case Management Team. Contact tracing during coronavirus disease outbreak, South Korea, 2020. Emerg Infect Dis. 2020;26. [PMID: 32673193] doi:10.3201/eid2610.201315 [DOI] [PMC free article] [PubMed]
- 38. Kim J, Choe YJ, Lee J, et al. Role of children in household transmission of COVID-19. Arch Dis Child. 2020. [PMID: 32769089] doi:10.1136/archdischild-2020-319910 [DOI] [PubMed]
- 39. Lewis NM, Chu VT, Ye D, et al. Household transmission of SARS-CoV-2 in the United States. Clin Infect Dis. 2020. doi:10.1093/cid/ciaa1166
- 40. Korber B, Fischer WM, Gnanakaran S, et al; Sheffield COVID-19 Genomics Group. Tracking changes in SARS-CoV-2 spike: evidence that D614G increases infectivity of the COVID-19 virus. Cell. 2020;182:812-827.e19. [PMID: 32697968] doi:10.1016/j.cell.2020.06.043 [DOI] [PMC free article] [PubMed]
- 41. Volz EM, Hill V, McCrone JT, et al. Evaluating the effects of SARS-CoV-2 Spike mutation D614G on transmissibility and pathogenicity. medRxiv. Preprint posted online 4 August 2020. doi:10.1101/2020.07.31.20166082 [DOI] [PMC free article] [PubMed]
- 42. Daniloski Z, Guo X, Sanjana NE. The D614G mutation in SARS-CoV-2 Spike increases transduction of multiple human cell types. bioRxiv. Preprint posted online 15 June 2020. doi:10.1101/2020.06.14.151357
- 43. Zhang L, Jackson CB, Mou H, et al. The D614G mutation in the SARS-CoV-2 spike protein reduces S1 shedding and increases infectivity. bioRxiv. Preprint posted online 12 June 2020. doi:10.1101/2020.06.12.148726
- 44. Mansbach RA, Chakraborty S, Nguyen K, et al. The SARS-CoV-2 Spike variant D614G favors an open conformational state. bioRxiv. Preprint posted online 26 July 2020. doi:10.1101/2020.07.26.219741 [DOI] [PMC free article] [PubMed]
- 45. Wei J, Li Y. Airborne spread of infectious agents in the indoor environment. Am J Infect Control. 2016;44:S102-8. [PMID: 27590694] doi:10.1016/j.ajic.2016.06.003 [DOI] [PMC free article] [PubMed]
- 46. Klompas M, Baker MA, Rhee C. Airborne transmission of SARS-CoV-2: theoretical considerations and available evidence. JAMA. 2020;324:441-442. [PMID: 32749495] doi:10.1001/jama.2020.12458 [DOI] [PubMed]
- 47. Fennelly KP. Particle sizes of infectious aerosols: implications for infection control. Lancet Respir Med. 2020;8:914-924. [PMID: 32717211] doi:10.1016/S2213-2600(20)30323-4 [DOI] [PMC free article] [PubMed]
- 48. Lu J, Gu J, Li K, et al. COVID-19 outbreak associated with air conditioning in restaurant, Guangzhou, China, 2020. Emerg Infect Dis. 2020;26:1628-1631. [PMID: 32240078] doi:10.3201/eid2607.200764 [DOI] [PMC free article] [PubMed]
- 49. Ma J, Qi X, Chen H, et al. COVID-19 patients in earlier stages exhaled millions of SARS-CoV-2 per hour. Clin Infect Dis. 2020. [PMID: 32857833] doi:10.1093/cid/ciaa1283 [DOI] [PMC free article] [PubMed]
- 50. Courtemanche C, Garuccio J, Le A, et al. Strong social distancing measures in the United States reduced the COVID-19 growth rate. Health Aff (Millwood). 2020;39:1237-1246. [PMID: 32407171] doi:10.1377/hlthaff.2020.00608 [DOI] [PubMed]
- 51. Chu DK, Akl EA, Duda S, et al; COVID-19 Systematic Urgent Review Group Effort (SURGE) study authors. Physical distancing, face masks, and eye protection to prevent person-to-person transmission of SARS-CoV-2 and COVID-19: a systematic review and meta-analysis. Lancet. 2020;395:1973-1987. [PMID: 32497510] doi:10.1016/S0140-6736(20)31142-9 [DOI] [PMC free article] [PubMed]
- 52. Hu M, Lin H, Wang J, et al. The risk of COVID-19 transmission in train passengers: an epidemiological and modelling study. Clin Infect Dis. 2020. [PMID: 32726405] doi:10.1093/cid/ciaa1057 [DOI] [PMC free article] [PubMed]
- 53. Jang S, Han SH, Rhee JY. Cluster of coronavirus disease associated with fitness dance classes, South Korea. Emerg Infect Dis. 2020;26:1917-1920. [PMID: 32412896] doi:10.3201/eid2608.200633 [DOI] [PMC free article] [PubMed]
- 54. Wang Y, Tian H, Zhang L, et al. Reduction of secondary transmission of SARS-CoV-2 in households by face mask use, disinfection and social distancing: a cohort study in Beijing, China. BMJ Glob Health. 2020;5. [PMID: 32467353] doi:10.1136/bmjgh-2020-002794 [DOI] [PMC free article] [PubMed]
- 55. James A, Eagle L, Phillips C, et al. High COVID-19 attack rate among attendees at events at a church — Arkansas, March 2020. MMWR Morb Mortal Wkly Rep. 2020;69:632-635. [PMID: 32437338] doi:10.15585/mmwr.mm6920e2 [DOI] [PubMed]
- 56. Adam D, Wu P, Wong J, et al. Clustering and superspreading potential of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infections in Hong Kong. Research Square. Preprint posted online 21 May 2020. doi:10.21203/rs.3.rs-29548/v1
- 57. Furuse Y, Sando E, Tsuchiya N, et al. Clusters of coronavirus disease in communities, Japan, January-April 2020. Emerg Infect Dis. 2020;26. [PMID: 32521222] doi:10.3201/eid2609.202272 [DOI] [PMC free article] [PubMed]
- 58. Qian H, Miao T, Liu L, et al. Indoor transmission of SARS-CoV-2. medRxiv. Preprint posted online 7 April 2020. doi:10.1101/2020.04.04.20053058
- 59. Nishiura H, Oshitani H, Kobayashi T, et al. Closed environments facilitate secondary transmission of coronavirus disease 2019 (COVID-19). medRxiv. Preprint posted online 16 April 2020. doi:10.1101/2020.02.28.20029272
- 60. Leclerc QJ, Fuller NM, Knight LE, et al; CMMID COVID-19 Working Group. What settings have been linked to SARS-CoV-2 transmission clusters? Wellcome Open Res. 2020;5:83. [PMID: 32656368] doi:10.12688/wellcomeopenres.15889.2 [DOI] [PMC free article] [PubMed]
- 61. Shen Y, Li C, Dong H, et al. Community outbreak investigation of SARS-CoV-2 transmission among bus riders in eastern China. JAMA Intern Med. 2020. [PMID: 32870239] doi:10.1001/jamainternmed.2020.5225 [DOI] [PMC free article] [PubMed]
- 62. Lee JK, Jeong HW. Wearing face masks regardless of symptoms is crucial for preventing the spread of COVID-19 in hospitals. Infect Control Hosp Epidemiol. 2020:1-2. [PMID: 32372736] doi:10.1017/ice.2020.202 [DOI] [PMC free article] [PubMed]
- 63. Mitze T, Kosfeld R, Rode J, et al. Face masks considerably reduce Covid-19 cases in Germany: a synthetic control method approach. IZA Discussion Paper no. 13319. 9 June 2020. Accessed at https://ssrn.com/abstract=3620634 on 8 August 2020. [DOI] [PMC free article] [PubMed]
- 64. Lyu W, Wehby GL. Community use of face masks and COVID-19: evidence from a natural experiment of state mandates in the US. Health Aff (Millwood). 2020;39:1419-1425. [PMID: 32543923] doi:10.1377/hlthaff.2020.00818 [DOI] [PubMed]
- 65. Chou R, Dana T, Jungbauer R, et al. Masks for prevention of respiratory virus infections, including SARS-CoV-2, in health care and community settings. A living rapid review. Ann Intern Med. 2020. [PMID: 32579379] doi:10.7326/M20-3213 [DOI] [PMC free article] [PubMed]
- 66. Deng W, Bao L, Gao H, et al. Ocular conjunctival inoculation of SARS-CoV-2 can cause mild COVID-19 in rhesus macaques. Nat Commun. 2020;11:4400. [PMID: 32879306] doi:10.1038/s41467-020-18149-6 [DOI] [PMC free article] [PubMed]
- 67. Cai J, Sun W, Huang J, et al. Indirect virus transmission in cluster of COVID-19 cases, Wenzhou, China, 2020. Emerg Infect Dis. 2020;26:1343-1345. [PMID: 32163030] doi:10.3201/eid2606.200412 [DOI] [PMC free article] [PubMed]
- 68. Lessells R, Moosa Y, de Oliveira T. Report into a nosocomial outbreak of coronavirus disease 2019 (COVID-19) at Netcare St. Augustine's Hospital. 15 May 2020. Accessed at www.krisp.org.za/manuscripts/StAugustinesHospitalOutbreakInvestigation_FinalReport_15may2020_comp.pdf on 8 August 2020.
- 69. Bae SH, Shin H, Koo HY, et al. Asymptomatic transmission of SARS-CoV-2 on evacuation flight. Emerg Infect Dis. 2020;26. [PMID: 32822289] doi:10.3201/eid2611.203353 [DOI] [PMC free article] [PubMed]
- 70. Ran L, Chen X, Wang Y, et al. Risk factors of healthcare workers with corona virus disease 2019: a retrospective cohort study in a designated hospital of Wuhan in China. Clin Infect Dis. 2020. [PMID: 32179890] doi:10.1093/cid/ciaa287 [DOI] [PMC free article] [PubMed]
- 71. van Kampen JJA, van de Vijver DAMC, Fraaij PLA, et al. Shedding of infectious virus in hospitalized patients with coronavirus disease-2019 (COVID-19): duration and key determinants. medRxiv. Preprint posted online 9 June 2020. doi:10.1101/2020.06.08.20125310 [DOI] [PMC free article] [PubMed]
- 72. Cheng HY, Jian SW, Liu DP, et al; Taiwan COVID-19 Outbreak Investigation Team. Contact tracing assessment of COVID-19 transmission dynamics in Taiwan and risk at different exposure periods before and after symptom onset. JAMA Intern Med. 2020. [PMID: 32356867] doi:10.1001/jamainternmed.2020.2020 [DOI] [PMC free article] [PubMed]
- 73. Shi J, Wen Z, Zhong G, et al. Susceptibility of ferrets, cats, dogs, and other domesticated animals to SARS-coronavirus 2. Science. 2020;368:1016-1020. [PMID: 32269068] doi:10.1126/science.abb7015 [DOI] [PMC free article] [PubMed]
- 74. Sit THC, Brackman CJ, Ip SM, et al. Infection of dogs with SARS-CoV-2. Nature. 2020. [PMID: 32408337] doi:10.1038/s41586-020-2334-5 [DOI] [PMC free article] [PubMed]
- 75. Richard M, Kok A, de Meulder D, et al. SARS-CoV-2 is transmitted via contact and via the air between ferrets. Nat Commun. 2020;11:3496. [PMID: 32641684] doi:10.1038/s41467-020-17367-2 [DOI] [PMC free article] [PubMed]
- 76. Garigliany M, Van Laere AS, Clercx C, et al. SARS-CoV-2 natural transmission from human to cat, Belgium, March 2020. Emerg Infect Dis. 2020;26. [PMID: 32788033] doi:10.3201/eid2612.202223 [DOI] [PMC free article] [PubMed]
- 77. Halfmann PJ, Hatta M, Chiba S, et al. Transmission of SARS-CoV-2 in domestic cats [Letter]. N Engl J Med. 2020;383:592-594. [PMID: 32402157] doi:10.1056/NEJMc2013400 [DOI] [PMC free article] [PubMed]
- 78. Oreshkova N, Molenaar RJ, Vreman S, et al. SARS-CoV-2 infection in farmed minks, the Netherlands, April and May 2020. Euro Surveill. 2020;25. [PMID: 32553059] doi:10.2807/1560-7917.ES.2020.25.23.2001005 [DOI] [PMC free article] [PubMed]
- 79. Oude Munnink BB, Sikkema RS, Nieuwenhuijse DF, et al. Jumping back and forth: anthropozoonotic and zoonotic transmission of SARS-CoV-2 on mink farms. bioRxiv. Preprint posted online 1 September 2020. doi:10.1101/2020.09.01.277152
- 80. Yang Z, Liu Y. Vertical transmission of severe acute respiratory syndrome coronavirus 2: a systematic review. Am J Perinatol. 2020;37:1055-1060. [PMID: 32403141] doi:10.1055/s-0040-1712161 [DOI] [PMC free article] [PubMed]
- 81. Zeng H, Xu C, Fan J, et al. Antibodies in infants born to mothers with COVID-19 pneumonia. JAMA. 2020. [PMID: 32215589] doi:10.1001/jama.2020.4861 [DOI] [PMC free article] [PubMed]
- 82. Dong L, Tian J, He S, et al. Possible vertical transmission of SARS-CoV-2 from an infected mother to her newborn. JAMA. 2020. [PMID: 32215581] doi:10.1001/jama.2020.4621 [DOI] [PMC free article] [PubMed]
- 83. Kimberlin DW, Stagno S. Can SARS-CoV-2 infection be acquired in utero? More definitive evidence is needed. JAMA. 2020. [PMID: 32215579] doi:10.1001/jama.2020.4868 [DOI] [PubMed]
- 84. Zeng L, Xia S, Yuan W, et al. Neonatal early-onset infection with SARS-CoV-2 in 33 neonates born to mothers with COVID-19 in Wuhan, China. JAMA Pediatr. 2020. [PMID: 32215598] doi:10.1001/jamapediatrics.2020.0878 [DOI] [PMC free article] [PubMed]
- 85. Alzamora MC, Paredes T, Caceres D, et al. Severe COVID-19 during pregnancy and possible vertical transmission. Am J Perinatol. 2020;37:861-865. [PMID: 32305046] doi:10.1055/s-0040-1710050 [DOI] [PMC free article] [PubMed]
- 86. Patanè L, Morotti D, Giunta MR, et al. Vertical transmission of coronavirus disease 2019: severe acute respiratory syndrome coronavirus 2 RNA on the fetal side of the placenta in pregnancies with coronavirus disease 2019-positive mothers and neonates at birth. Am J Obstet Gynecol MFM. 2020;2:100145. [PMID: 32427221] doi:10.1016/j.ajogmf.2020.100145 [DOI] [PMC free article] [PubMed]
- 87. Baud D, Greub G, Favre G, et al. Second-trimester miscarriage in a pregnant woman with SARS-CoV-2 infection. JAMA. 2020. [PMID: 32352491] doi:10.1001/jama.2020.7233 [DOI] [PMC free article] [PubMed]
- 88. Vivanti AJ, Vauloup-Fellous C, Prevot S, et al. Transplacental transmission of SARS-CoV-2 infection. Nat Commun. 2020;11:3572. [PMID: 32665677] doi:10.1038/s41467-020-17436-6 [DOI] [PMC free article] [PubMed]
- 89. Alamar I, Abu-Arja MH, Heyman T, et al. A possible case of vertical transmission of SARS-CoV-2 in a newborn with positive placental in situ hybridization of SARS-CoV-2 RNA. J Pediatric Infect Dis Soc. 2020. [PMID: 32888013] doi:10.1093/jpids/piaa109 [DOI] [PMC free article] [PubMed]
- 90. Groß R, Conzelmann C, Müller JA, et al. Detection of SARS-CoV-2 in human breastmilk [Letter]. Lancet. 2020;395:1757-1758. [PMID: 32446324] doi:10.1016/S0140-6736(20)31181-8 [DOI] [PMC free article] [PubMed]
- 91. Marín Gabriel MA, Cuadrado I, Álvarez Fernández B, et al; Neo-COVID-19 Research Group. Multicentre Spanish study found no incidences of viral transmission in infants born to mothers with COVID-19. Acta Paediatr. 2020. [PMID: 32649784] doi:10.1111/apa.15474 [DOI] [PMC free article] [PubMed]
- 92. Chambers C, Krogstad P, Bertrand K, et al. Evaluation for SARS-CoV-2 in breast milk from 18 infected women. JAMA. 2020. [PMID: 32822495] doi:10.1001/jama.2020.15580 [DOI] [PMC free article] [PubMed]
- 93. Gu J, Han B, Wang J. COVID-19: gastrointestinal manifestations and potential fecal-oral transmission [Editorial]. Gastroenterology. 2020;158:1518-1519. [PMID: 32142785] doi:10.1053/j.gastro.2020.02.054 [DOI] [PMC free article] [PubMed]
- 94. Deng W, Bao L, Gao H, et al. Ocular conjunctival inoculation of SARS-CoV-2 can cause mild COVID-19 in Rhesus macaques. bioRxiv. Preprint posted online 30 March 2020. doi:10.1101/2020.03.13.990036 [DOI] [PMC free article] [PubMed]
- 95. Wang W, Xu Y, Gao R, et al. Detection of SARS-CoV-2 in different types of clinical specimens. JAMA. 2020. [PMID: 32159775] doi:10.1001/jama.2020.3786 [DOI] [PMC free article] [PubMed]
- 96. Kim JM, Kim HM, Lee EJ, et al. Detection and isolation of SARS-CoV-2 in serum, urine, and stool specimens of COVID-19 patients from the Republic of Korea. Osong Public Health Res Perspect. 2020;11:112-117. [PMID: 32528816] doi:10.24171/j.phrp.2020.11.3.02 [DOI] [PMC free article] [PubMed]
- 97. Sun J, Xiao J, Sun R, et al. Prolonged persistence of SARS-CoV-2 RNA in body fluids. Emerg Infect Dis. 2020;26:1834-1838. [PMID: 32383638] doi:10.3201/eid2608.201097 [DOI] [PMC free article] [PubMed]
- 98. Parasa S, Desai M, Thoguluva Chandrasekar V, et al. Prevalence of gastrointestinal symptoms and fecal viral shedding in patients with coronavirus disease 2019: a systematic review and meta-analysis. JAMA Netw Open. 2020;3:e2011335. [PMID: 32525549] doi:10.1001/jamanetworkopen.2020.11335 [DOI] [PMC free article] [PubMed]
- 99. van Doorn AS, Meijer B, Frampton CMA, et al. Systematic review with meta-analysis: SARS-CoV-2 stool testing and the potential for faecal-oral transmission. Aliment Pharmacol Ther. 2020. [PMID: 32852082] doi:10.1111/apt.16036 [DOI] [PMC free article] [PubMed]
- 100. Patel J. Viability of SARS-CoV-2 in faecal bio-aerosols [Letter]. Colorectal Dis. 2020. [PMID: 32515130] doi:10.1111/codi.15181 [DOI] [PMC free article] [PubMed]
- 101. Lai CKC, Ng RWY, Wong MCS, et al. Epidemiological characteristics of the first 100 cases of coronavirus disease 2019 (COVID-19) in Hong Kong Special Administrative Region, China, a city with a stringent containment policy. Int J Epidemiol. 2020. [PMID: 32601677] doi:10.1093/ije/dyaa106 [DOI] [PMC free article] [PubMed]
- 102. Kang M, Wei J, Yuan J, et al. Probable evidence of fecal aerosol transmission of SARS-CoV-2 in a high-rise building. Ann Intern Med. 2020. [PMID: 32870707] doi:10.7326/M20-0928 [DOI] [PMC free article] [PubMed]
- 103. Li D, Jin M, Bao P, et al. Clinical characteristics and results of semen tests among men with coronavirus disease 2019. JAMA Netw Open. 2020;3:e208292. [PMID: 32379329] doi:10.1001/jamanetworkopen.2020.8292 [DOI] [PMC free article] [PubMed]
- 104. Qiu L, Liu X, Xiao M, et al. SARS-CoV-2 is not detectable in the vaginal fluid of women with severe COVID-19 infection. Clin Infect Dis. 2020;71:813-817. [PMID: 32241022] doi:10.1093/cid/ciaa375 [DOI] [PMC free article] [PubMed]
- 105. Scorzolini L, Corpolongo A, Castilletti C, et al. Comment of the potential risks of sexual and vertical transmission of Covid-19 infection. Clin Infect Dis. 2020. [PMID: 32297915] doi:10.1093/cid/ciaa445 [DOI] [PMC free article] [PubMed]
- 106. Prazuck T, Giaché S, Gubavu C, et al. Investigation of a family outbreak of COVID-19 using systematic rapid diagnostic tests raises new questions about transmission [Letter]. J Infect. 2020. [PMID: 32610107] doi:10.1016/j.jinf.2020.06.066 [DOI] [PMC free article] [PubMed]
- 107. Hogan CA, Stevens B, Sahoo MK, et al. High frequency of SARS-CoV-2 RNAemia and association with severe disease. medRxiv. Preprint posted online 1 May 2020. doi:10.1101/2020.04.26.20080101 [DOI] [PMC free article] [PubMed]
- 108. Fajnzylber JM, Regan J, Coxen K, et al. SARS-CoV-2 viral load is associated with increased disease severity and mortality. medRxiv. Preprint posted online 17 July 2020. doi:10.1101/2020.07.15.20131789 [DOI] [PMC free article] [PubMed]
- 109. Chang L, Zhao L, Gong H, et al. Severe acute respiratory syndrome coronavirus 2 RNA detected in blood donations. Emerg Infect Dis. 2020;26:1631-1633. [PMID: 32243255] doi:10.3201/eid2607.200839 [DOI] [PMC free article] [PubMed]
- 110. Qian G, Yang N, Ma AHY, et al. COVID-19 transmission within a family cluster by presymptomatic carriers in China. Clin Infect Dis. 2020;71:861-862. [PMID: 32201889] doi:10.1093/cid/ciaa316 [DOI] [PMC free article] [PubMed]
- 111. Bai Y, Yao L, Wei T, et al. Presumed asymptomatic carrier transmission of COVID-19. JAMA. 2020. [PMID: 32083643] doi:10.1001/jama.2020.2565 [DOI] [PMC free article] [PubMed]
- 112. Chau NVV, Thanh Lam V, Thanh Dung N, et al; OUCRU COVID-19 research group. The natural history and transmission potential of asymptomatic SARS-CoV-2 infection. Clin Infect Dis. 2020. [PMID: 32497212] doi:10.1093/cid/ciaa711 [DOI] [PMC free article] [PubMed]
- 113. Luo L, Liu D, Liao X, et al. Contact settings and risk for transmission in 3410 close contacts of patients with COVID-19 in Guangzhou, China. A prospective cohort study. Ann Intern Med. 2020. [PMID: 32790510] doi:10.7326/M20-2671 [DOI] [PMC free article] [PubMed]
- 114. Qiu X, Nergiz AI, Maraolo AE, et al. Defining the role of asymptomatic SARS-CoV-2 transmission: a living systematic review. medRxiv. Preprint posted online 3 September 2020. doi:10.1101/2020.09.01.20135194
- 115. Long QX, Tang XJ, Shi QL, et al. Clinical and immunological assessment of asymptomatic SARS-CoV-2 infections. Nat Med. 2020;26:1200-1204. [PMID: 32555424] doi:10.1038/s41591-020-0965-6 [DOI] [PubMed]
- 116. Lee S, Kim T, Lee E, et al. Clinical course and molecular viral shedding among asymptomatic and symptomatic patients with SARS-CoV-2 infection in a community treatment center in the Republic of Korea. JAMA Intern Med. 2020. [PMID: 32780793] doi:10.1001/jamainternmed.2020.3862 [DOI] [PMC free article] [PubMed]
- 117. He X, Lau EHY, Wu P, et al. Temporal dynamics in viral shedding and transmissibility of COVID-19. Nat Med. 2020;26:672-675. [PMID: 32296168] doi:10.1038/s41591-020-0869-5 [DOI] [PubMed]
- 118. Lauer SA, Grantz KH, Bi Q, et al. The incubation period of coronavirus disease 2019 (COVID-19) from publicly reported confirmed cases: estimation and application. Ann Intern Med. 2020;172:577-582. [PMID: 32150748] doi:10.7326/M20-0504 [DOI] [PMC free article] [PubMed]
- 119. Yang L, Dai J, Zhao J, et al. Estimation of incubation period and serial interval of COVID-19: analysis of 178 cases and 131 transmission chains in Hubei province, China. Epidemiol Infect. 2020;148:e117. [PMID: 32594928] doi:10.1017/S0950268820001338 [DOI] [PMC free article] [PubMed]
- 120. Xu XK, Liu XF, Wu Y, et al. Reconstruction of transmission pairs for novel coronavirus disease 2019 (COVID-19) in mainland China: estimation of super-spreading events, serial interval, and hazard of infection. Clin Infect Dis. 2020. [PMID: 32556265] doi:10.1093/cid/ciaa790 [DOI] [PMC free article] [PubMed]
- 121. Shrestha NK, Marco Canosa F, Nowacki AS, et al. Distribution of transmission potential during non-severe COVID-19 illness. Clin Infect Dis. 2020. [PMID: 32594116] doi:10.1093/cid/ciaa886 [DOI] [PMC free article] [PubMed]
- 122. Goyal A, Reeves DB, Cardozo-Ojeda EF, et al. Wrong person, place and time: viral load and contact network structure predict SARS-CoV-2 transmission and super-spreading events. medRxiv. Preprint posted online 7 August 2020. doi:10.1101/2020.08.07.20169920
- 123. To KK, Tsang OT, Leung WS, et al. Temporal profiles of viral load in posterior oropharyngeal saliva samples and serum antibody responses during infection by SARS-CoV-2: an observational cohort study. Lancet Infect Dis. 2020;20:565-574. [PMID: 32213337] doi:10.1016/S1473-3099(20)30196-1 [DOI] [PMC free article] [PubMed]
- 124. Guo L, Ren L, Yang S, et al. Profiling early humoral response to diagnose novel coronavirus disease (COVID-19). Clin Infect Dis. 2020;71:778-785. [PMID: 32198501] doi:10.1093/cid/ciaa310 [DOI] [PMC free article] [PubMed]
- 125. Liu Y, Yan LM, Wan L, et al. Viral dynamics in mild and severe cases of COVID-19 [Letter]. Lancet Infect Dis. 2020;20:656-657. [PMID: 32199493] doi:10.1016/S1473-3099(20)30232-2 [DOI] [PMC free article] [PubMed]
- 126. Perera RAPM, Tso E, Tsang OTY, et al. SARS-CoV-2 virus culture and subgenomic RNA for respiratory specimens from patients with mild coronavirus disease. Emerg Infect Dis. 2020;26. [PMID: 32749957] doi:10.3201/eid2611.203219 [DOI] [PMC free article] [PubMed]
- 127. Singanayagam A, Patel M, Charlett A, et al. Duration of infectiousness and correlation with RT-PCR cycle threshold values in cases of COVID-19, England, January to May 2020. Euro Surveill. 2020;25. [PMID: 32794447] doi:10.2807/1560-7917.ES.2020.25.32.2001483 [DOI] [PMC free article] [PubMed]
- 128. Bullard J, Dust K, Funk D, et al. Predicting infectious SARS-CoV-2 from diagnostic samples. Clin Infect Dis. 2020. [PMID: 32442256] doi:10.1093/cid/ciaa638 [DOI] [PMC free article] [PubMed]
- 129. Arons MM, Hatfield KM, Reddy SC, et al; Public Health–Seattle and King County and CDC COVID-19 Investigation Team. Presymptomatic SARS-CoV-2 infections and transmission in a skilled nursing facility. N Engl J Med. 2020;382:2081-2090. [PMID: 32329971] doi:10.1056/NEJMoa2008457 [DOI] [PMC free article] [PubMed]
- 130. Wong SCY, Kwong RT, Wu TC, et al. Risk of nosocomial transmission of coronavirus disease 2019: an experience in a general ward setting in Hong Kong. J Hosp Infect. 2020;105:119-127. [PMID: 32259546] doi:10.1016/j.jhin.2020.03.036 [DOI] [PMC free article] [PubMed]
- 131. Endo A, Abbott S, Kucharski AJ, et al; Centre for the Mathematical Modelling of Infectious Diseases COVID-19 Working Group. Estimating the overdispersion in COVID-19 transmission using outbreak sizes outside China. Wellcome Open Res. 2020;5:67. [PMID: 32685698] doi:10.12688/wellcomeopenres.15842.3 [DOI] [PMC free article] [PubMed]
- 132. Ferretti L, Wymant C, Kendall M, et al. Quantifying SARS-CoV-2 transmission suggests epidemic control with digital contact tracing. Science. 2020;368. [PMID: 32234805] doi:10.1126/science.abb6936 [DOI] [PMC free article] [PubMed]
- 133. Althouse BM, Wenger EA, Miller JC, et al. Stochasticity and heterogeneity in the transmission dynamics of SARS-CoV-2. arXiv. Preprint posted online 27 May 2020. arXiv:2005.13689
- 134. Bi Q, Wu Y, Mei S, et al. Epidemiology and transmission of COVID-19 in 391 cases and 1286 of their close contacts in Shenzhen, China: a retrospective cohort study. Lancet Infect Dis. 2020;20:911-919. [PMID: 32353347] doi:10.1016/S1473-3099(20)30287-5 [DOI] [PMC free article] [PubMed]
- 135. Miller D, Martin MA, Harel N, et al. Full genome viral sequences inform patterns of SARS-CoV-2 spread into and within Israel. medRxiv. Preprint posted online 22 May 2020. doi:10.1101/2020.05.21.20104521 [DOI] [PMC free article] [PubMed]
- 136. Park SY, Kim YM, Yi S, et al. Coronavirus disease outbreak in call center, South Korea. Emerg Infect Dis. 2020;26:1666-1670. [PMID: 32324530] doi:10.3201/eid2608.201274 [DOI] [PMC free article] [PubMed]
- 137. Yusef D, Hayajneh W, Awad S, et al. Large outbreak of coronavirus disease among wedding attendees, Jordan. Emerg Infect Dis. 2020;26. [PMID: 32433907] doi:10.3201/eid2609.201469 [DOI] [PMC free article] [PubMed]
- 138. Hamner L, Dubbel P, Capron I, et al. High SARS-CoV-2 attack rate following exposure at a choir practice — Skagit County, Washington, March 2020. MMWR Morb Mortal Wkly Rep. 2020;69:606-610. [PMID: 32407303] doi:10.15585/mmwr.mm6919e6 [DOI] [PubMed]
- 139. Szablewski CM, Chang KT, Brown MM, et al. SARS-CoV-2 transmission and infection among attendees of an overnight camp — Georgia, June 2020. MMWR Morb Mortal Wkly Rep. 2020;69:1023-1025. [PMID: 32759921] doi:10.15585/mmwr.mm6931e1 [DOI] [PMC free article] [PubMed]
- 140. Payne DC, Smith-Jeffcoat SE, Nowak G, et al; CDC COVID-19 Surge Laboratory Group. SARS-CoV-2 infections and serologic responses from a sample of U.S. Navy service members — USS Theodore Roosevelt, April 2020. MMWR Morb Mortal Wkly Rep. 2020;69:714-721. [PMID: 32525850] doi:10.15585/mmwr.mm6923e4 [DOI] [PMC free article] [PubMed]
- 141. Lemieux J, Siddle KJ, Shaw BM, et al. Phylogenetic analysis of SARS-CoV-2 in the Boston area highlights the role of recurrent importation and superspreading events. medRxiv. Preprint posted online 25 August 2020. doi:10.1101/2020.08.23.20178236
- 142. Madewell ZJ, Yang Y, Longini IM Jr, et al. Household transmission of SARS-CoV-2: a systematic review and meta-analysis of secondary attack rate. medRxiv. Preprint posted online 1 August 2020. doi:10.1101/2020.07.29.20164590
- 143. Emeruwa UN, Ona S, Shaman JL, et al. Associations between built environment, neighborhood socioeconomic status, and SARS-CoV-2 infection among pregnant women in New York City. JAMA. 2020. [PMID: 32556085] doi:10.1001/jama.2020.11370 [DOI] [PMC free article] [PubMed]
- 144. Cox RJ, Brokstad KA, Krammer F, et al; Bergen COVID-19 Research Group. Seroconversion in household members of COVID-19 outpatients [Letter]. Lancet Infect Dis. 2020. [PMID: 32553187] doi:10.1016/S1473-3099(20)30466-7 [DOI] [PMC free article] [PubMed]