Abstract
The American Neurogastroenterology and Motility Society Task Force recommends that gastrointestinal motility procedures should be performed in motility laboratories adhering to the strict recommendations and personal protective equipment (PPE) measures to protect patients, ancillary staff, and motility allied health professionals. When available and within constraints of institutional guidelines, it is preferable for patients scheduled for motility procedures to complete a coronavirus disease 2019 (COVID-19) test within 48 hours before their procedure, similar to the recommendations before endoscopy made by gastroenterology societies. COVID-19 test results must be documented before performing procedures. If procedures are to be performed without a COVID-19 test, full PPE use is recommended, along with all social distancing and infection control measures. Because patients with suspected motility disorders may require multiple procedures, sequential scheduling of procedures should be considered to minimize need for repeat COVID-19 testing. The strategies for and timing of procedure(s) should be adapted, taking into consideration local institutional standards, with the provision for screening without testing in low prevalence areas. If tested positive for COVID-19, subsequent negative testing may be required before scheduling a motility procedure (timing is variable). Specific recommendations for each motility procedure including triaging, indications, PPE use, and alternatives to motility procedures are detailed in the document. These recommendations may evolve as understanding of virus transmission and prevalence of COVID-19 infection in the community changes over the upcoming months.
INTRODUCTION
In December 2019, several cases of pneumonia were identified in Wuhan, China. The causative microbe, a severe acute respiratory syndrome (SARS)-related coronavirus (SARS-CoV-2), was named coronavirus disease 2019 (COVID-19) by the World Health Organization in February 2020 (1). COVID-19 has subsequently been declared a pandemic. According to the Centers for Disease Control and Prevention, as of August 5, the United States has greater than 4.7 million confirmed cases and 156,000 deaths (2). Globally, an August 5 report from the World Health Organization stated that approximately 18 million COVID-19 cases have been identified approximately 700,000 deaths have occurred related to this infection (3). COVID-19 symptoms include fever, cough, fatigue, and loss of taste. However, the prevalence of gastrointestinal symptoms such as nausea, vomiting, and diarrhea in COVID-19-confirmed cases has been significant, and fecal viral excretion may persist for several weeks after the resolution of lung illness (4).
As of 2019, the United States has more than 120 motility laboratories (5). During the COVID-19 pandemic, motility laboratories temporarily shut down, which provided opportunities for protecting staff and patients from spreading COVID-19. Diagnostic procedures performed in motility laboratories provide evidence for appropriate intervention for gastrointestinal symptoms not explained by structural or mucosal disease. The American Neurogastroenterology and Motility Society (ANMS) organized a Task Force for developing guidance strategies regarding reopening of motility laboratories. This document describes how to stratify urgency of motility physiologic procedures, screen before the procedures, optimize personal protective equipment (PPE) utilization, clean, and prepare the motility laboratory space during the COVID-19 pandemic. Prioritizing procedures should take into consideration the impact of symptoms on nutrition, need for hospitalization, impact on quality of life, and the role of testing for preoperative evaluation before invasive procedures, including myotomy, lung transplant, and colectomy.
The ANMS Task Force recommendations for reactivation of motility laboratory operations are not guidelines based on evidence; instead, they are based on societal guidelines for endoscopic procedures (6–9), taking into consideration the available evidence and expert consensus (10). However, we encourage all centers and healthcare providers to consult with local and state public health departments and their institution when implementing these recommendations. Furthermore, the resumption of motility laboratory operations should follow the White House/Centers for Disease Control and Prevention State or Regional Gating Criteria, assuming no additional restrictive state or local policies. Local infection rates should be monitored, and elective procedures should be discontinued in the event of an infection surge (9). The ANMS Task Force recommendations are jointly endorsed by the ANMS and the American College of Gastroenterology.
PREPROCEDURE SCREENING
Gastrointestinal motility procedures should only be performed in motility laboratories that have the capability of adhering to the Task Force recommendations and PPE measures described to protect patients, ancillary staff, and motility allied health professionals. Testing for COVID-19 is not recommended for motility laboratory personnel and physicians; daily symptom and exposure monitoring and temperature checks are recommended. Whenever possible, it is preferable for patients scheduled for motility procedures to undergo COVID-19 testing within 48 hours of the procedure, similar to recommendations for endoscopy made by gastroenterology societies (6–9). Routine COVID-19 testing for patients should be individualized based on the prevalence of COVID-19 in the area, institutional testing recommendations, local availability of testing, turnaround time of test results, and test sensitivity (9). Currently, preprocedure COVID-19 testing seems to be largely covered under major health plans; practitioners need to monitor coverage, which may evolve as the pandemic continues. It is important to note that the polymerase chain reaction test for COVID-19 has an approximate false negative rate of 20% in small studies (11), with even higher rates early in the infection. Therefore, symptom, exposure, and temperature monitoring are essential even when the test is negative.
When multiple motility procedures are indicated, these should be scheduled sequentially on the same day to obviate the need for repeated COVID-19 testing. Test results should be documented in the patient's record. If the COVID-19 test is positive, a 14-day period without symptoms off antipyretics or a subsequent negative test is required before scheduling a motility procedure (timing is variable) (9). If institutional and local health authorities recommend against routine COVID-19 testing before routine procedures, preprocedure symptom screening is imperative, and full PPE use are recommended in addition to social distancing and infection control measures.
On arriving at the healthcare facility for the motility laboratory procedure, we endorse screening for pertinent COVID-19 symptoms, exposure to potential patients with COVID-19, and checking body temperature, even in patients with previous negative COVID-19 testing. Patients who are symptomatic or report potential exposure to COVID-19 should be rescheduled, following similar guidelines used for endoscopy and outpatient clinics (6–10). A standard institutional protocol for patients who fail screening is recommended (9). Proper PPE should be worn by individuals performing motility laboratory procedures. Personal protection concordant with that recommended for endoscopic procedures can be followed, with additional precautions unique to each motility procedure (9). For instance, because catheters and other similar equipment are routinely handled, double gloving is recommended for several motility procedures so that the outer set of gloves can be used for handling the contaminated catheter and the inner glove can be used for the next phase of PPE doffing. Table 1 provides recommendations for proper motility laboratory PPE requirements. These recommendations are derived from expert opinion and gastroenterology society guidelines for endoscopy procedures (6–10). Proper donning and doffing of PPE should be practiced to limit the spread of potential air droplets (12) (Figure 1).
Table 1.
Recommended motility laboratory PPE to safely perform a motility laboratory procedure
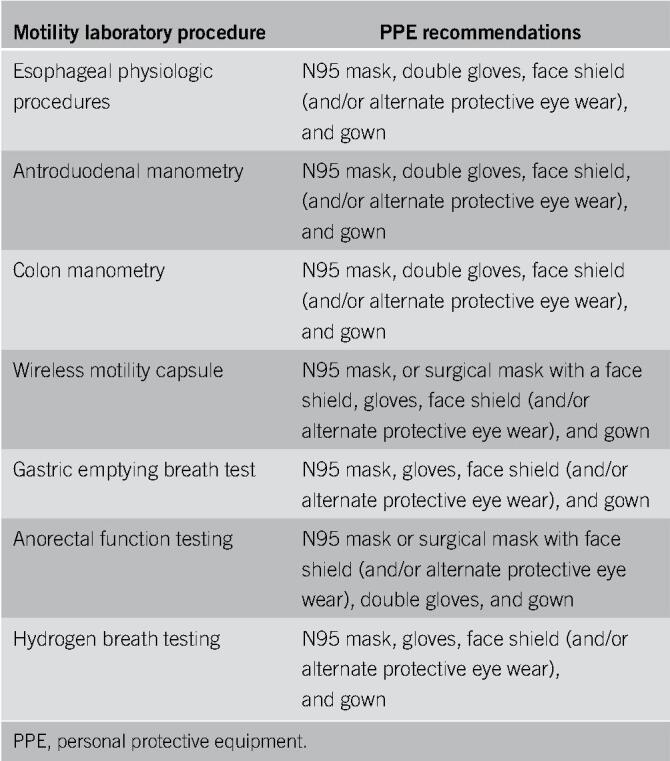
Figure 1.
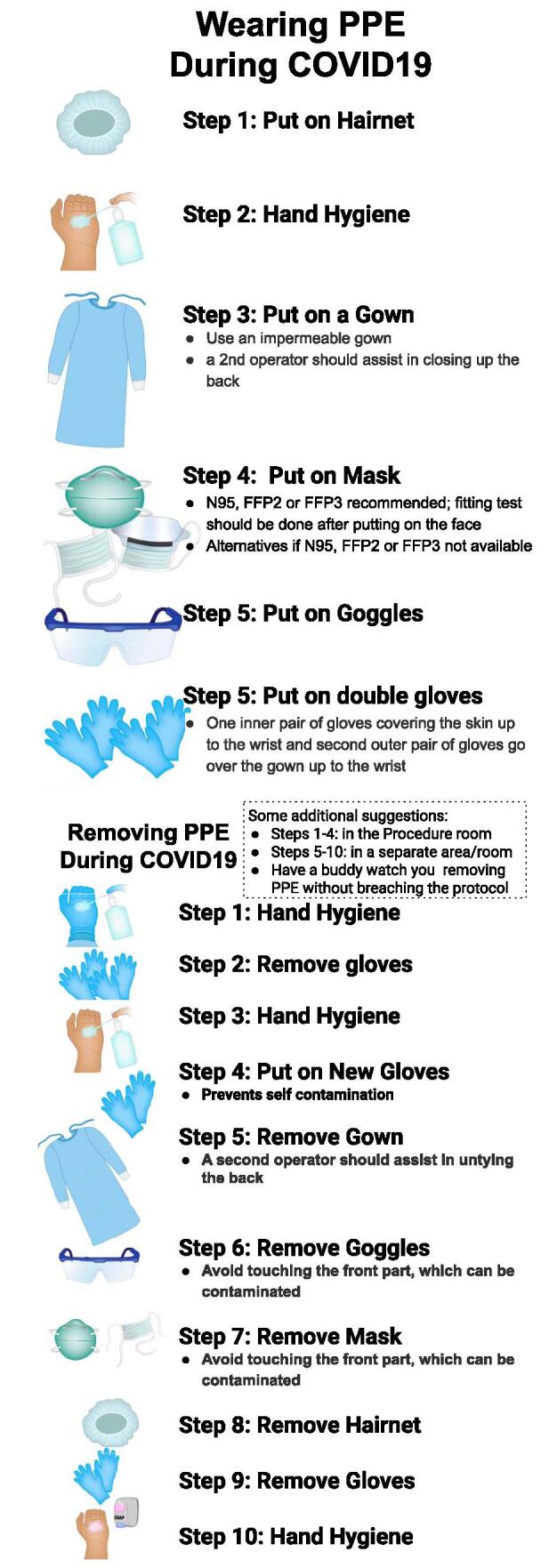
Donning and doffing of PPE. Published with permission from Dr. S. J. Raju, MD Anderson, Houston, TX. PPE, personal protective equipment.
PROCEDURE ROOM SETUP
Adequate spacing is recommended in waiting areas and within motility procedure rooms. Strict adherence to scheduled times is recommended to avoid congregation of patients and relatives in the waiting areas. This may require patients to wait in their cars rather than at the facility if delays are expected, with 2-way communication through mobile phones. Only the patient should be brought into the procedure room to limit contact between individuals. The patient should wear a mask as long as technically possible before, during, and after the motility laboratory encounter in the health care facility. Adequate time should be allowed between procedures to allow for delays and extra time for terminal cleaning of the procedure areas between procedures.
Consideration can be given for filtering the air within the motility procedure room in between each patient whenever possible, as per local institutional standards. If available, this could include high-efficiency particulate air (HEPA) filters for the prevention of airborne infections (13). The required time for HEPA filtration is adjusted by the number of exchanges within the specific procedure room. Where HEPA filtration is not available, institutional infection control measures should be followed.
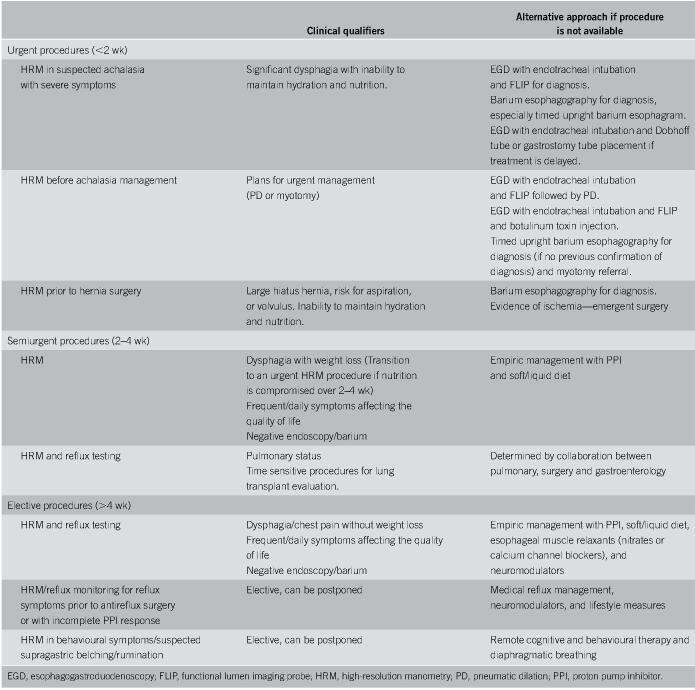
ESOPHAGEAL PHYSIOLOGIC TESTING
Esophageal physiologic procedures, including high-resolution manometry (HRM), pH, and pH-impedance monitoring are typically elective procedures performed in an outpatient motility laboratory by trained allied health professional for nonlife-threatening indications. Accepted indications for testing have not been implemented during the pandemic out of an abundance of caution (14,15). Although infrequent, there are limited urgent indications for esophageal HRM that deserve attention (Table 2), particularly before definitive management of achalasia and obstructive motor disorders (16). However, alternatives exist, particularly barium radiography (especially timed upright barium esophagram) and functional lumen imaging probe (FLIP) to confirm the diagnosis of achalasia and the placement of enteral feeding tubes to maintain nutrition while awaiting definitive management. Although not technically equivalent, barium esophagography and FLIP are alternatives to HRM in the diagnosis of achalasia. Hiatus hernia repair and antireflux surgery are rarely emergent, with the notable exception of gastric volvulus, where surgical repair and partial fundoplication can potentially be performed without HRM assessment of esophageal peristaltic performance. Wireless prolonged pH monitoring can be performed if endoscopy is planned, and the assessment of reflux burden is needed, but this is not anticipated to be an urgent or semiurgent requirement, except in rare instances. Consolidating procedures that can be performed at a single encounter (e.g., esophagogastroduodenoscopy [EGD] and FLIP, EGD and motility catheter placement, and EGD and wireless pH monitoring) will reduce the need for multiple patient interactions.
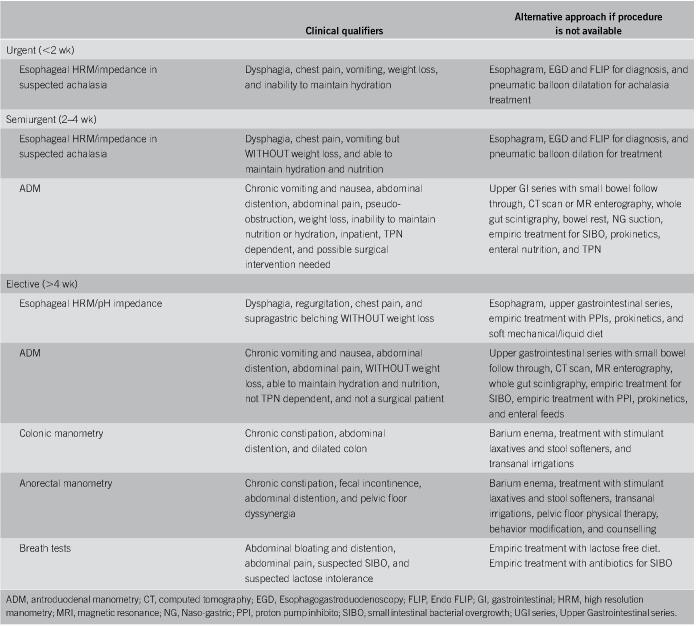
Table 2.
Triaging esophageal physiologic procedures
During the pandemic, some semiurgent procedures have evolved into urgent procedures because of prolonged periods of compromised nutrition and the need for time-sensitive management. Furthermore, motility laboratories will need to balance the backlog of patients that have been cancelled or rescheduled with the urgency of the indication as hospitals resume semielective and elective procedures. Table 2, adapted from a recent publication on the topic (16), provides guidance on indications and clinical qualifiers that elevate the typically elective esophageal physiologic procedures to semiurgent or emergent status during the COVID-19 crisis. In addition, this table provides a framework that can be used during each phase of the pandemic, including active shut down and recovery as various states and regions of the United States are in different stages of recovery.
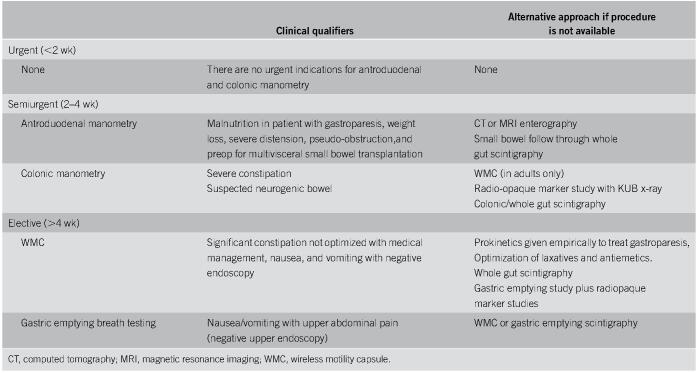
STOMACH, SMALL INTESTINE, AND COLON
Various diagnostic procedures are used to evaluate motor function in sections of the gut from stomach to colon, but none is considered urgent (Table 3). Two Food and Drug Administration-approved diagnostic modalities, wireless motility capsule and gastric emptying breath testing (GEBT), can be performed in lieu of gastric emptying scintigraphy in patients with symptoms suspicious for gastroparesis (17). When performed in patients with suspected gastroparesis and/or slow transit constipation, wireless motility capsule generates information on both whole gut and regional gut transit (18). This procedure does not generate aerosols unless the patient coughs or chokes while swallowing the capsule. Therefore, as long as the operator preforming the procedure can socially distance from the patient during capsule and meal ingestion while wearing adequate PPE, this procedure should be of low risk to the operator.
Table 3.
Triaging motility procedures pertaining to the stomach, small intestine, and colon
Although not as widely available as scintigraphy, GEBT provides a measure of gastric emptying by evaluating CO2 excretion in the breath after a 13C-labeled Streptomyces platensis-enriched meal is ingested (19). Because breath samples are collected, the test generates aerosols and could be of risk to the operator without adequate protective measures and PPE. In the United States, GEBT has been predominantly used for research and therapeutic drug trials. Because elective non-COVID-19 research is currently halted and because GEBT carries aerosol-related risks, this will likely only be reinstated in late phases of resumption of motility laboratory operations in most institutions.
Patients with gastric stimulators implanted for management of severe gastroparesis through the Food and Drug Administration's Humanitarian Device Exemption program will need to be seen for symptom and device monitoring in outpatient clinics. For patients who present for gastric stimulator interrogation, operators and treating physicians will need to follow local guidelines for PPE, similar to other outpatient encounters, which could include mask, face shield, head cover, gloves, and gown, when adjustments are made to their device.
Two advanced motility procedures performed in tertiary care centers consist of antroduodenal manometry (ADM) to evaluate chronic intestinal pseudo-obstruction and colonic manometry to evaluate neurogenic bowel and severe constipation refractory to medication (20). Both procedures are performed predominantly in the pediatric setting and not routinely in adults.
For the most part, ADM is an elective procedure but could be semiurgent in sick patients with suspected small bowel dysmotility. ADM is also recommended for evaluation of small bowel dysmotility in severe gastroparesis to triage decision-making before enteral feeding vs total parenteral nutrition and in patients with primary or secondary chronic intestinal pseudo-obstruction from either neuropathic or myopathic disease before multiorgan transplantation. ADM involves the placement of a manometry catheter using fluoroscopy, or EGD which is an aerosol-generating procedure. Therefore, PPE, including N95 mask or equivalent, are needed for all staff during the placement and removal of the ADM catheter. After placement of the catheter, motility recordings should be performed in a private area that minimizes broad aerosolization. Patients should wear a surgical mask whenever possible. COVID-19 testing before ADM is important because this procedure is typically performed in an ambulatory setting, sometimes involving admission to an observation unit for prolonged monitoring.
Colonic manometry is performed for the evaluation of neurogenic bowel and in severe constipation to determine the presence of colonic dysmotility before surgical management and triaging of decision-making between medical options and partial/subtotal colectomy. In children, it is also performed before considering Malone antegrade continence enema as treatment for chronic constipation (21). Colonic manometry is performed via colonoscopy, and because fecal shedding of the coronavirus has been reported (12), standard preprocedure COVID-19 testing of the patient can be considered, and PPE requirements will be similar to society recommendations for colonoscopy (6–9).
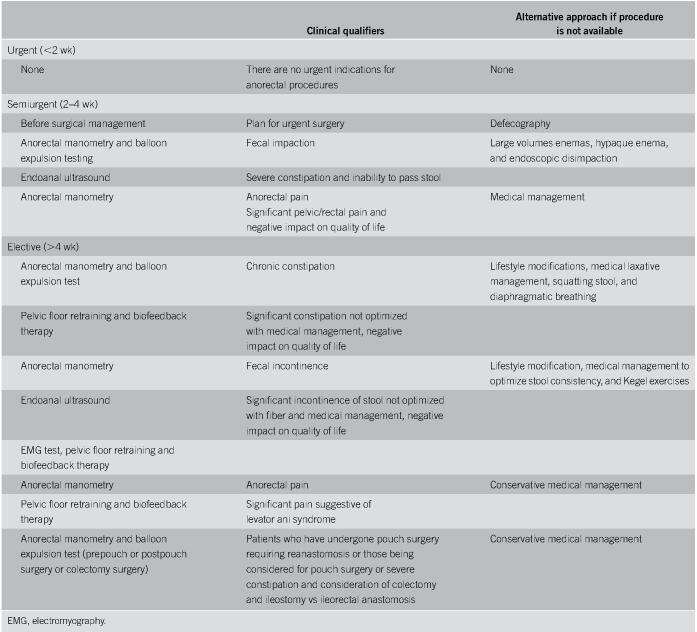
ANORECTAL FUNCTION TESTING AND BIOFEEDBACK THERAPY
The anorectal physiologic procedures are routinely performed for the evaluation of chronic anorectal diseases including constipation, pelvic floor dysfunction, fecal incontinence presurgical or postsurgical evaluations, and levator ani syndrome (22). Therefore, indications for these tests are typically nonurgent (Table 4). In addition, pelvic floor retraining and biofeedback therapy are the only evidence-based treatments for anorectal disorders and are generally considered nonurgent, although these disorders carry significant morbidity and negatively affect the quality of life (22). Furthermore, many of these disorders remain undiagnosed for years, further adding to the burden of ill health and overall health care utilization. We therefore propose measures to adequately care for patients without COVID-19 undergoing anorectal physiologic procedures and pelvic biofeedback therapy programs and steps for resuming these operations.
Table 4.
Triaging patients for anorectal function testing and procedures
Scheduling of patients with anorectal and pelvic floor disorders should be based on the indications for anorectal physiologic procedures and pelvic biofeedback therapy programs. Resources should be prioritized toward patients in whom anorectal manometry and balloon expulsion testing will change management strategy and/or triage decision-making for surgery. This is particularly important because most facilities anticipate reduced access to motility procedures and pelvic biofeedback programs, mostly dictated by the need for extra measures taken to mitigate the risk of spread of COVID-19.
Anorectal physiologic procedures, pelvic floor retraining, and biofeedback are considered “medium risk” for virus transmission. SARS-CoV-2 shedding in the stool has been reported in 50%–60% of patients and may take as long as 3–6 weeks to clear after respiratory symptoms subside (23). Propensity for fecal-oral transmission remains unclear (26), although SARS-CoV-2 may spread through the aerosolization of feces after flushing. Risk of aerosolization during the maneuvers performed during testing such as cough or forceful breathing is low but can be mitigated by both the patient and the operator wearing masks and the operator wearing a face shield, gown, hair covering and gloves.
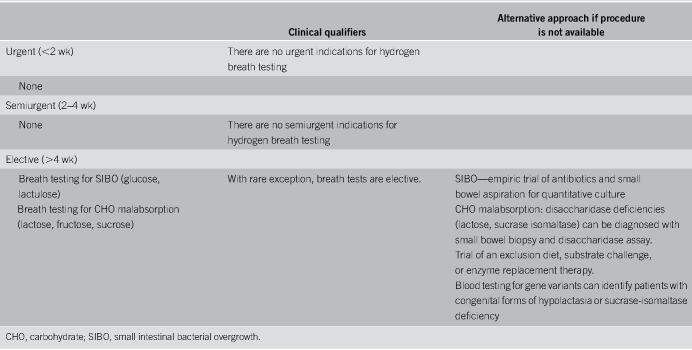
HYDROGEN BREATH TESTING
Breath testing can be a valuable adjunct to identify patients with small intestinal bacterial overgrowth (SIBO) or carbohydrate malabsorption. For SIBO, breath tests using glucose or lactulose are commonly used. Each of these tests has its strengths and weaknesses. Most agree that lactulose is likely to be the more sensitive of the 2 options, but glucose is likely to be the more specific testing substrate (24). Breath testing can also be used to identify patients with lactose, fructose, or sucrose malabsorption. Protocols for conducting breath tests can be found in the Rome consensus document (25) and the North American Consensus document (26). For the most part, breath tests should be considered elective procedures (Table 5). There are several alternative means by which to diagnose SIBO or carbohydrate malabsorption (Table 5). SIBO can be diagnosed with small bowel aspiration for quantitative culture (24). Patients with a high pretest probability of SIBO such as those with scleroderma, diabetes with autonomic neuropathy, gastric or small bowel surgery, radiation enteritis, to name a few, may not need testing before offering a course of antibiotics. Disaccharidase deficiency (lactase and sucrase isomaltase) can be identified with small bowel biopsy and quantitative disaccharidase enzyme assay (27). Oral enzyme replacement therapy is available for lactase and sucrase. Clinicians can attempt a trial with substrate (sucrose, lactose, and fructose) restriction or challenge. There are also blood tests for gene variants that identify patients with congenital forms of hypolactasia or sucrase-isomaltase deficiency. Because breath testing is considered an aerosol-generating procedure, patients should optimally have a negative COVID-19 test before their procedure. Patients with a positive test should be rescheduled to a later date, at least 2 weeks later. In circumstances where patients do not undergo preprocedure COVID-19 testing, the patient should be delayed allowing for COVID-19 testing or managed by staff with full PPE including an N95 mask. At-home breath testing, offered by several commercial vendors, is an alternative to traditional laboratory-based breath testing. This option may be attractive to practices which do not otherwise perform breath testing or in circumstances where COVID-19 testing is not readily available or in which a patient resides far from their physician's facilities.
Table 5.
Triaging patients needing hydrogen breath testing
PEDIATRIC MOTILITY TESTING
Pediatric motility procedures include mainly 5 types of physiologic tests: (i) esophageal physiologic procedures, including esophageal manometry (water perfused and HRM with and without impedance, pH, and pH-impedance monitoring systems; (ii) ADM, (iii) colonic manometry, (iv) anorectal manometry, and (v) hydrogen and lactose breath tests. These procedures are typically considered elective and performed in an outpatient motility laboratory by allied health professionals and physician motility experts (Table 6). Alternatives include radiological studies such as esophagram, upper gastrointestinal series, small bowel follow through, and barium enema. Urgent/emergent indications are rare for these procedures in pediatrics, other than for achalasia and for the rare patient who needs assessment of gut motility prior to surgical treatment. For institutions that have FLIP available, this can be an alternative for confirmation of achalasia, and precautions are the same as for upper endoscopy (6,8,9). The risks that each of these procedures carry and the precautions needed are the same as in the adult setting.
Table 6.
Triaging pediatric patients for motility procedures
BILLING FOR MOTILITY TESTING RELATIVE TO COVID-19
During the COVID-19 pandemic, we anticipate that many gastrointestinal physiology and motility laboratories will face significant financial challenges. We recommend that physicians involved in the leadership of motility laboratories become familiar with methods to optimize reimbursement for the procedures performed. A recent review provided a comprehensive outline of Current Procedural Terminology codes for gastrointestinal physiology and motility procedures in the year 2020, along with important reimbursement suggestions (5). In addition, the ANMS commissioned a billing and coding update specific to esophageal function testing in 2018 (28). These are useful resources for motility laboratories.
The Centers for Medicare & Medicaid Services has greatly expanded the coverage for telehealth, including audio-only evaluations amid this pandemic (29). We recommend that clinicians managing gastrointestinal motility disorders and leaders of motility laboratories remain current with evolving telehealth opportunities across insurers. During the upcoming months, gastrointestinal physiology and motility procedures may be postponed or alternative tests may be recommended, which will often require detailed discussion with each patient regarding options and ongoing management. Specifically, for hydrogen and methane breath testing, practitioners may opt to pursue home testing for their patients, which could shift motility laboratory revenue to the entity reporting home testing results. A telehealth visit explaining the appropriate methods for home breath testing, interpretation of testing, and explaining management recommendations may provide an opportunity for the motility laboratory to engage with the patient. Overall, all providers should continue to interact with their patients and follow safety guidelines when performing motility-related procedures.
CONCLUSION
As healthcare professionals return to their medical offices and resume operations, rescheduling of patients for elective gastrointestinal motility procedures is being considered, and the safety of staff, patients, and family members is of paramount importance. We present a framework based on stratification of motility procedure indications to urgent, semiurgent, and elective using clinical qualifiers and alternatives to the primary procedure to make appropriate testing decisions. The reactivation timeline will need to be based on individual institutional policies. The ANMS task force acknowledges that these expert recommendations may need to be modified as the COVID-19 pandemic evolves, and new data become available once motility laboratories reopen. Careful monitoring of resurgence will likely also affect future policies and recommendations. Evolving information may result in either loosening or tightening of reactivation measures, depending on whether peaks or surges of COVID-19 cases reoccur. Recommendations may also change, depending on exposure risks in individual institutions and regions, and further monitoring of the outcome of patients presenting for motility laboratory procedures.
CONFLICTS OF INTEREST
Guarantor of the article: C. Prakash Gyawali, MD.
Specific author contributions: All authors contributed equally to the manuscript.
Financial support: None to report.
Potential competing interests: J.R.B.: Consultant: Medtronic, Diversatek; B.M.: Research support: Medtronic; S.R.: none; L.Ne: none ; L.Ng: none; W.D.C.: consulting: commonwealth diagnostic international, Gemelli, Progenity; grant funding: commonwealth diagnostics international; R.S.: none; J.M.G.: consulting: Medtronic; speaking: Abbott, Biogaia, Medtronic; S.W.: none ; A.R.K.: consulting: Medtronic, Progenity ;J.E.P.: consulting: Medtronic, Diversatek; speaking: Medtronic, Diversatek, Ethicon; stock options: Crospon; licensing arrangement: Medtronic; C.P.G.: consulting: Medtronic, Diversatek, Ironwood, Quintiles, Isothrive.
REFERENCES
- 1.Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020;395:497–506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention. Coronavirus 2019 (COVID 2019): Cases, Data and Surveillance. (https://www.cdc.gov/coronavirus/2019-ncov/cases-updates/cases-in-us.html). Accessed August 5, 2020. [Google Scholar]
- 3.WHO. Coronavirus Disease (COVID 19): Situation Report 116. (https://www.who.int/). Accessed August 5, 2020. [Google Scholar]
- 4.Ng SC, Tilg H. COVID-19 and the gastrointestinal tract: More than meets the eye. Gut 2020;69:973–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Yadlapati R, Chen JW, Khan A. How to set up a successful motility lab. Gastroenterology 2020;158:1202–10. [DOI] [PubMed] [Google Scholar]
- 6.AGA, DHPA. Joint AGA/DHPA Guidance: Recommendations for Resumption of Elective Endoscopy During the COVID-19 Pandemic. (https://www.dhpassociation.org/2020/04/27/aga-dhpa-resume-endoscopy-covid19/2020). Accessed August 5, 2020. [Google Scholar]
- 7.ASGE, SGNA, ACG, AGA, ASCRS, SAGES. Management of Endoscopes, Endoscope Reprocessing, and Storage Areas during the COVID-19 Pandemic. (https://fascrs.org/getattachment/5ef92409-cade-4928-96cf-91ca53ebad93/GI-Society-management-of-endoscope-fleet.pdf?lang=en-US). Accessed August 5, 2020. [Google Scholar]
- 8.AASLD, ACG, AGA, ASGE. Gastroenterology Professional Society Guidance on Endoscopic Procedures During The Covid-19 Pandemic. (https://webfiles.gi.org/links/media/Joint_GI_Society_Guidance_on_Endoscopic_Procedure_During_COVID19_FINAL_impending_3312020.pdf). Accessed August 5, 2020. [Google Scholar]
- 9.The American College of Gastroenterology (ACG) Roadmap for Safely Resuming or Ramping-Up Endoscopy in the COVID-19 Pandemic. (https://webfiles.gi.org/docs/policy/2020resuming-endoscopy-fin-05122020.pdf). Accessed August 5, 2020. [Google Scholar]
- 10.Gross SA, Robbins DH, Greenwald DA, et al. Preparation in the Big Apple: New York City, a new epicenter of the COVID-19 pandemic. Am J Gastroenterol 2020;115:801–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Li D, Wang D, Dong J, et al. False-negative results of real-time reverse-transcriptase polymerase chain reaction for severe acute respiratory syndrome coronavirus 2: Role of deep-learning-based CT diagnosis and insights from two cases. Korean J Radiol 2020;21:505–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Repici A, Maselli R, Colombo M, et al. Coronavirus (COVID-19) outbreak: What the department of endoscopy should know. Gastrointest Endosc 2020;92:192–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Roberts V. To PAPR or not to PAPR? Can J Respir Ther 2014;50:87–90. [PMC free article] [PubMed] [Google Scholar]
- 14.Trudgill NJ, Sifrim D, Sweis R, et al. British Society of Gastroenterology guidelines for oesophageal manometry and oesophageal reflux monitoring. Gut 2019;68:1731–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gyawali CP, Carlson DA, Chen J, et al. ACG clinical guideline: Clinical use of esophageal physiologic testing. Am J Gastroenterol 2020, in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lee YY, Bredenoord AJ, Gyawali CP. Recommendations for essential esophageal physiologictesting during the covid-19 pandemic. Clin Gastroenterol Hepatol 2020;18:1906–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rao SS, Camilleri M, Hasler WL, et al. Evaluation of gastrointestinal transit in clinical practice: Position paper of the American and European Neurogastroenterology and Motility Societies. Neurogastroenterol Motil 2011;23:8–23. [DOI] [PubMed] [Google Scholar]
- 18.Kuo B, McCallum RW, Koch KL, et al. Comparison of gastric emptying of a nondigestible capsule to a radio-labelled meal in healthy and gastroparetic subjects. Aliment Pharmacol Ther 2008;27:186–96. [DOI] [PubMed] [Google Scholar]
- 19.Szarka LA, Camilleri M, Vella A, et al. A stable isotope breath test with a standard meal for abnormal gastric emptying of solids in the clinic and in research. Clin Gastroenterol Hepatol 2008;6:635–43.e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gronlund D, Poulsen JL, Sandberg TH, et al. Established and emerging methods for assessment of small and large intestinal motility. Neurogastroenterol Motil 2017;29:e13008. [DOI] [PubMed] [Google Scholar]
- 21.Har AF, Rescorla FJ, Croffie JM. Quality of life in pediatric patients with unremitting constipation pre and post Malone Antegrade Continence Enema (MACE) procedure. J Pediatr Surg 2013;48:1733–7. [DOI] [PubMed] [Google Scholar]
- 22.Carrington EV, Heinrich H, Knowles CH, et al. The international anorectal physiology working group (IAPWG) recommendations: Standardized testing protocol and the London classification for disorders of anorectal function. Neurogastroenterol Motil 2020;32:e13679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wu Y, Guo C, Tang L, et al. Prolonged presence of SARS-CoV-2 viral RNA in faecal samples. Lancet Gastroenterol Hepatol 2020;5:434–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Pimentel M, Saad RJ, Long MD, et al. ACG clinical guideline: Small intestinal bacterial overgrowth. Am J Gastroenterol 2020;115:165–78. [DOI] [PubMed] [Google Scholar]
- 25.Gasbarrini A, Corazza GR, Gasbarrini G, et al. Methodology and indications of H2-breath testing in gastrointestinal diseases: The Rome Consensus Conference. Aliment Pharmacol Ther 2009;29(Suppl 1):1–49. [DOI] [PubMed] [Google Scholar]
- 26.Rezaie A, Buresi M, Lembo A, et al. Hydrogen and methane-based breath testing in gastrointestinal disorders: The North American Consensus. Am J Gastroenterol 2017;112:775–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Puertolas MV, Fifi AC. The role of disaccharidase deficiencies in functional abdominal pain disorders-A narrative review. Nutrients 2018;10:1835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Khan A, Massey B, Rao S, et al. Esophageal function testing: Billing and coding update. Neurogastroenterol Motil 2018;30:e13158. [DOI] [PubMed] [Google Scholar]
- 29.Covered Telehealth Services for PHE for the COVID-19 Pandemic. (https://www.cms.gov/Medicare/Medicare-General-Information/Telehealth/). Accessed August 5, 2020. [Google Scholar]