Abstract
During the first 12 weeks of the coronavirus disease 2019 (COVID-19) pandemic, endometrial cancer diagnoses declined 35% and patient calls for abnormal bleeding declined 33% compared with 2019 levels.
INTRODUCTION
On March 4, 2020, the first coronavirus disease 2019 (COVID-19)–related death was reported in California, followed by a statewide shelter-in-place order on March 19, 2020.1 Declines in acute presentations of conditions such as myocardial infarction have since been reported.2,3 However, little is known about how the COVID-19 pandemic has influenced clinical detection of cancer. We therefore evaluated pandemic-associated changes in the diagnosis rate of endometrial cancer, which affects more than 65,000 women in the United States annually and is usually detected by biopsy after reports of abnormal bleeding.4
METHODS
Approval was obtained from the institutional review board for Kaiser Permanente Northern California, a large, integrated health system with more than 4.4 million members. We compared weekly endometrial cancer incidence rates (diagnoses per 100,000 person-weeks) during the pandemic (March 4, 2020–May 26, 2020) with prepandemic rates (February 4, 2020–March 3, 2020) as well as with rates during these same time periods in 2019. Cancers were identified by pathology reports and confirmed by manual review, and patient characteristics were assessed using electronic databases linked to medical records. We also examined weekly rates of telephone calls for abnormal bleeding to the health system's call center, a centralized service that handles calls for advice. All rates were based on the population of female health plan members aged 18 years or older at the time and compared using incidence rate ratios. Chi-square test, Student t test, or Wilcoxon rank sum test were used to compare characteristics. Analyses were performed using SAS 9.4.
RESULTS
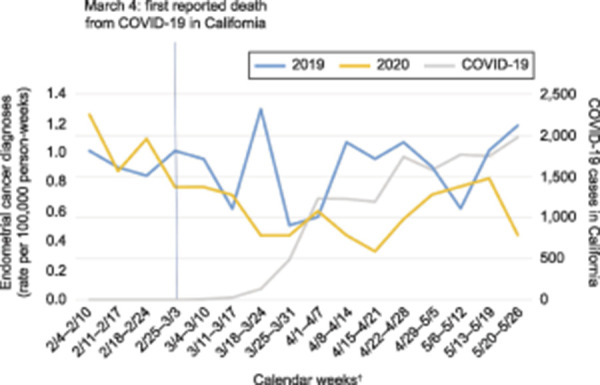
From February 4 to March 3, the average weekly endometrial cancer incidence rate in 2020 (1.0, 95% CI 0.79–1.26) was similar to the rate in 2019 (0.94, 95% CI 0.74–1.19). Whereas the rate from March 4–May 26 remained stable in 2019 at 0.88 (95% CI 0.77–1.02), with 191 cancers detected, the rate in 2020 during the pandemic dropped to 0.58 (95% CI 0.48–0.69), with 127 cancers detected—a decline of 41% relative to prepandemic rates (incidence rate ratio 0.59, 95% CI 0.44–0.78, P<.001) and 35% relative to the same period in 2019 (incidence rate ratio 0.65, 95% CI 0.52–0.82, P<.001) (Fig. 1). Calls for abnormal bleeding preceded diagnoses in 41% of cases in 2020 compared with 35% of cases in 2019. However, the volume of calls about abnormal vaginal bleeding during the pandemic was 33% lower in 2020, at 52.8 (95% CI 51.9–53.8) compared with 78.5 (95% CI 77.3–79.7) in 2019 (incidence rate ratio 0.67, 95% CI 0.66–0.69, P<.001). Patient characteristics during the two time periods were similar (Appendix 1, available online at http://links.lww.com/AOG/C20).
Fig. 1. Weekly incidence rates* of endometrial cancer diagnosis from March 4, 2020 to May 26, 2020, vs 2019, relative to coronavirus disease 2019 (COVID-19) cases in California.5 *Incidence rate calculated as diagnosis per 100,000 person-weeks based on the population of female health plan members aged 18 years or older at the time. †Dates in February are shifted 1 day in 2019 because of leap year.
Suh-Burgmann. Coronavirus Disease 2019 and Endometrial Cancer Detection. Obstet Gynecol 2020.
DISCUSSION
Endometrial cancer diagnoses were 35% lower during the first 12 weeks of the pandemic response compared with 2019 levels. Although a similar proportion of cancer diagnoses was preceded by calls for abnormal bleeding, calls about bleeding decreased 33% during this time. This suggests that reluctance to report symptoms, potentially owing to fear of COVID-19, was the main driver of lower detection rates. There was no indication that women at higher risk of severe COVID-19 illness based on age or comorbidities were less likely to be diagnosed during the pandemic. In response to the shelter-in-place order, routine screening visits were deferred and some reports of bleeding were initially evaluated by phone or video, but all outpatient women's health clinics remained open and physicians continued to perform biopsies. Therefore, the effect of this alone on diagnosis rates should have been transient. However, because abnormal bleeding histories are sometimes elicited in the course of other visits, patient deferral of routine visits or shifts to virtual visits may have reduced opportunities for incidental detection. Given the potential durability of public fears about COVID-19 and effects on care delivery, these findings indicate a need to raise awareness among women not to delay evaluation of abnormal bleeding and to consider strategies such as routinely inquiring about abnormal bleeding in virtual visits. Ongoing analysis is planned to assess the durability of these changes over time and potential long-term effects on outcomes.
Footnotes
Financial Disclosure The authors did not report any potential conflicts of interest.
The study was funded by The Permanente Medical Group Physician Researcher Program.
Each author has confirmed compliance with the journal's requirements for authorship.
Published online ahead-of-print July 21, 2020.
Peer reviews and author correspondence are available at http://links.lww.com/AOG/C21.
REFERENCES
- 1.Graff A. California reports its first coronavirus death. San Francisco Chronicle, March 4 2020. [Google Scholar]
- 2.Solomon MD, McNulty EJ, Rana JS, Leong TK, Lee C, Sung SH, et al. The Covid-19 pandemic and the incidence of acute myocardial infarction. N Engl J Med 2020 May 19. [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 3.Baum A, Schwartz MD. Admissions to Veterans Affairs hospitals for emergency conditions during the COVID-19 pandemic. JAMA 2020;324:96–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.American Cancer Society. Cancer facts & figures 2020. Available at: https://www.cancer.org/research/cancer-facts-statistics/all-cancer-facts-figures/cancer-facts-figures-2020.html. Retrieved May 18, 2020. [Google Scholar]
- 5.California Department of Public Health. Coronavirus disease 2019 (COVID-19). Available at: https://www.cdph.ca.gov. Retrieved May 31, 2020. [Google Scholar]


