Supplemental Digital Content is available in the text.
Keywords: acute kidney injury, critical illness, epidemiology, mortality, thrombosis
Abstract
Objective:
To determine the prevalence of D-dimer elevation in coronavirus disease 2019 (COVID-19) hospitalization, trajectory of D-dimer levels during hospitalization, and its association with clinical outcomes.
Approach and Results:
Consecutive adults admitted to a large New York City hospital system with a positive polymerase chain reaction test for SARS-CoV-2 (severe acute respiratory syndrome coronavirus 2) between March 1, 2020 and April 8, 2020 were identified. Elevated D-dimer was defined by the laboratory-specific upper limit of normal (>230 ng/mL). Outcomes included critical illness (intensive care, mechanical ventilation, discharge to hospice, or death), thrombotic events, acute kidney injury, and death during admission. Among 2377 adults hospitalized with COVID-19 and ≥1 D-dimer measurement, 1823 (76%) had elevated D-dimer at presentation. Patients with elevated presenting baseline D-dimer were more likely than those with normal D-dimer to have critical illness (43.9% versus 18.5%; adjusted odds ratio, 2.4 [95% CI, 1.9–3.1]; P<0.001), any thrombotic event (19.4% versus 10.2%; adjusted odds ratio, 1.9 [95% CI, 1.4–2.6]; P<0.001), acute kidney injury (42.4% versus 19.0%; adjusted odds ratio, 2.4 [95% CI, 1.9–3.1]; P<0.001), and death (29.9% versus 10.8%; adjusted odds ratio, 2.1 [95% CI, 1.6–2.9]; P<0.001). Rates of adverse events increased with the magnitude of D-dimer elevation; individuals with presenting D-dimer >2000 ng/mL had the highest risk of critical illness (66%), thrombotic event (37.8%), acute kidney injury (58.3%), and death (47%).
Conclusions:
Abnormal D-dimer was frequently observed at admission with COVID-19 and was associated with higher incidence of critical illness, thrombotic events, acute kidney injury, and death. The optimal management of patients with elevated D-dimer in COVID-19 requires further study.
Highlights.
In this cohort study of 2377 consecutive patients with confirmed coronavirus disease 2019 (COVID-19), D-dimer was elevated in 76% of patients at hospital presentation.
D-dimer was independently associated with incidence of critical illness, thrombosis, acute kidney injury, and all-cause mortality.
In patients hospitalized with COVID-19, level of D-dimer may be used to identify gradient of risk.
The SARS-CoV-2 (severe acute respiratory syndrome coronavirus 2) coronavirus (coronavirus disease 2019 [COVID-19]) infection is a global pandemic, with >6 200 000 cases and 375 000 deaths confirmed as of June 1, 2020, and at least 376 000 confirmed cases in New York State alone. The clinical spectrum of COVID-19 infection is broad, encompassing asymptomatic infection, mild upper respiratory tract illness, respiratory failure, and death.1 Recent reports highlight an alarming incidence of acute kidney injury and both arterial and venous thrombotic events.2–8 A recent report by our group found the overall incidence of thrombosis in hospitalized patients with COVID-19 to be 16%, which after multivariable adjustment was associated with a 82% increased hazard of all-cause mortality (P<0.001).8 The most common pattern of abnormal coagulation observed in patients hospitalized with COVID-19 is characterized by elevations in fibrinogen and D-dimer levels.9
D-dimer is the principal breakdown fragment of fibrin and is used as a biomarker of fibrin formation and degradation.10 Numerous studies have shown that D-dimer is a valuable marker of activation of coagulation and fibrinolysis.11 Healthy individuals have low levels of circulating D-dimer, whereas elevated levels are found in conditions associated with thrombosis.11 D-dimer has been extensively investigated for the diagnosis, monitoring, and treatment of venous thromboembolism (VTE) for which it is used routinely.12 D-dimer levels are also elevated in conditions of chronic inflammation, such as active malignancy, rheumatoid arthritis, sickle cell disease, and asthma.13,14 In the setting of COVID-19, D-dimer has been reported to be higher in subjects who are critically ill or those who expire.15–19 However, the incidence of outcomes across different D-dimer levels both at clinical presentation and during the course of hospitalization are not well characterized. In addition, the trajectory of D-dimer in subjects with COVID-19 remains unexplored. Given that widespread microthrombi have been observed in COVID-19 in multiple organ systems,20,21 we hypothesized that elevated D-dimer levels would be associated with increased risk of clinically diagnosed thrombotic events, acute kidney injury, critical illness, and death among patients hospitalized with COVID-19.
We analyzed data from a large health system in New York City to examine the prevalence of D-dimer elevation at presentation and over time, and the association of the biomarker with incident thrombosis as well as acute kidney injury, critical illness, all-cause mortality, and likelihood of being discharged.
Methods
Identifiable patient level data from this project are not available to the public.
Study Setting
The study was approved by the New York University (NYU) Grossman School of Medicine Institutional Review Board and performed with a waiver of informed consent. We identified consecutive adults aged ≥18 years with a positive real-time polymerase chain reaction COVID-19 test between March 1, 2020 and April 08, 2020 who were admitted to NYU Langone Health, a multihospital health system in New York City. Follow-up was complete through May 13, 2020.
Data Collection
Data were obtained from the electronic health record (Epic Systems, Verona, WI), which is an integrated electronic health record including all inpatient and outpatient visits in the health system.
Patients hospitalized with a positive polymerase chain reaction test for COVID-19 were eligible for this retrospective, observational study if ≥1 D-dimer was measured during hospital admission. At all 4 NYU Langone Health inpatient facilities, routine D-dimer surveillance for individuals with suspected or confirmed diagnoses of COVID-19 was included in COVID-19-specific admission order sets in the electronic heath record at the time of hospital admission starting March 25. At all NYU Langone Health sites, D-dimer assay was measured using the Hemosil D-dimer HS 500 on an automated coagulation analyzer (ACL TOP, Instrumentation Laboratory). The initial D-dimer and all D-dimers measured during hospital admission were recorded for all eligible patients. The upper limit of normal for the D-dimer assay is 230 ng/mL. Subjects were categorized into normal (D-dimer <230 ng/mL) and elevated (D-dimer ≥230 ng/mL) categories. We conducted sensitivity analyses using different D-Dimer categories: <230 ng/mL (normal), 230 to 500 ng/mL, 500 to 2000 ng/mL, and >2000 ng/mL.
Study Variables
Demographic variables included age, sex, race/ethnicity (defined as non-Hispanic White, non-Hispanic Black, Hispanic, Asian, multiracial/other, and unknown), smoking status, and body mass index. Preexisting comorbidities included hypertension, hyperlipidemia, coronary artery disease, heart failure, diabetes mellitus, chronic kidney disease, and atrial fibrillation. Prior medication information included statins, β-blockers, ACE (angiotensin-converting enzyme) inhibitor (ACE-I) or angiotensin receptor blocker, and oral anticoagulants.
Clinical Outcomes
All-cause, in-hospital mortality was recorded for all patients. Critical illness was defined by a composite of treatment in an intensive care unit, need for mechanical ventilation, discharge to hospice, or death. Thrombotic events, as determined by the treating physician, were defined as a composite of deep venous thrombosis, pulmonary embolism, myocardial infarction, ischemic stroke, or systemic embolism.8 Acute kidney injury was defined according to the acute kidney injury network guidelines as an absolute increase of 0.3 mg/dL or more or a relative increase of 50% or more from baseline to peak creatinine.22 The most recent outpatient creatinine in the past 6 months was used as baseline. When no creatinine was available, admission creatinine was used.
Statistical Analyses
Continuous variables are shown using mean (SD) and median (interquartile range [IQR]) and compared using the nonparametric Mann-Whitney U test for all non-normally distributed data. Categorical variables are reported as frequency rates and percentages and compared by χ2 tests. The longitudinal trajectory of the mean D-dimer per day of hospitalization for patients in each outcome category was visualized using the fitted values from the loess regression for each end point separately. Logistic regression models were generated to estimate the odds of the study end points, adjusted for demographics, clinical comorbidities, vital signs at presentation, and baseline medications. Covariates in the multivariable models included age, sex, race, body mass index, tobacco use, hypertension, hyperlipidemia, chronic kidney disease, prior heart failure, atrial fibrillation, coronary artery disease, cancer, prior prescriptions for ACE or angiotensin receptor blockers, anticoagulants, statins, and β-blockers, and initial laboratory results for lymphocyte count, ferritin, and C-reactive protein. The c-index was reported as a measure of the model fitness. Statistical analyses were performed using statistical software R (R Foundation for Statistical Computing, Vienna, Austria), with packages forestplot, ggplot2, and base R. Statistical tests are 2-sided, and P values <0.05 were considered to be statistically significant.
Results
Of 2782 consecutive hospitalized subjects testing positive for SARS-CoV-2 between March 1, 2020 and April 8, 2020, a total of 405 (14.6%) subjects had no D-dimer drawn and were excluded (Figure I in the Data Supplement). Of the remaining 2377, the median age was 64 (IQR, 52–74), and 39% were female. Overall, the initial median D-dimer was 387 (25th–75th percentile, 237–713), and 1823 (76%) presented with an elevated D-dimer (>230 ng/mL). The median peak D-dimer was 767 (25th–75th percentile, 328–3372), and 2049 (86%) had an elevated D-dimer >230 ng/mL at some point during the course of hospitalization.
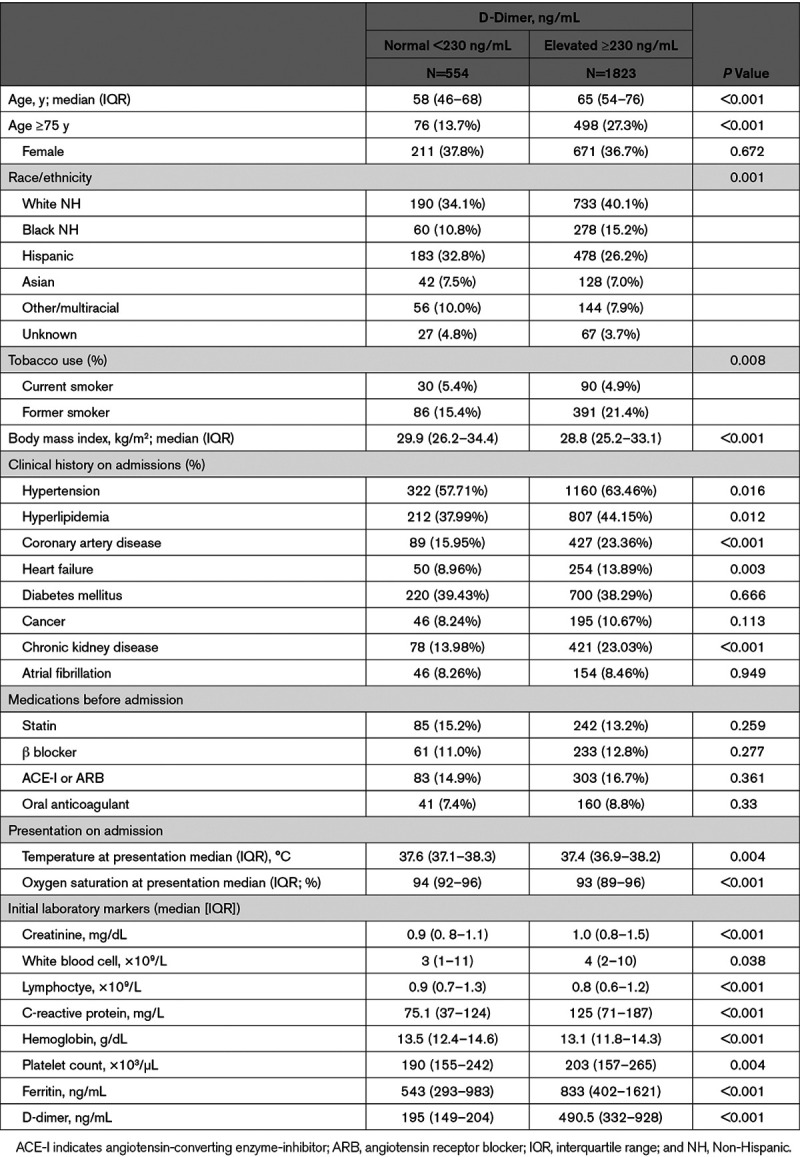
Compared with patients with a normal baseline D-dimer, patients with an elevated baseline D-dimer were older (median age, 65 [IQR=54–77] versus 58 [46–68] years; P<0.001) and had a lower body mass index (median [IQR], 28.8 [25.2–33.1] versus 29.9.0 [26.2–34.4]; P<0.001; Table 1). Comorbidities were more frequent among patients with an elevated D-dimer, including hypertension (63.5% versus 57.7%, P=0.016), hyperlipidemia (44.2% versus 38.0%, P=0.012), coronary artery disease (23.4% versus 16.0%, P=0.001), and chronic kidney disease (23.0% versus 14.0%, P<0.001). Cardiovascular medications were also more common in the elevated baseline D-dimer group. In terms of laboratory findings, patients with elevated baseline D-dimer had higher levels of median creatinine (1.0 [IQR=0.8–1.5] versus 0.9 [0.8–1.1], P<0.001), white blood cell count (4.0 [2.0–10] versus 3.0 [1.0–11], P<0.001), C-reactive protein (125 [71–187] versus 75.1 [37–124], P<0.001), platelet count (203 [157–265] versus 190 [155–242], P<0.001), ferritin (833 [402–1621] versus 543 [293–983], P<0.001), and lower levels of lymphoctyes (0.8 [0.6–1.2] versus 0.9 [0.7–1.3], P<0.001; Table 1).
Table 1.
Patient Characteristics According to Baseline D-Dimer
Clinical Outcomes
During the course of hospitalization, 899 (37.8%) had critical illness, 620 (26.1%) required mechanical ventilation, 410 (17.2%) had a thrombotic event, and 871 (36.8%) had acute kidney injury. Compared with those with normal baseline D-dimer, individuals with elevated D-dimer were more likely to become critically ill (43.9% versus 18.5%; P<0.001) and more often required invasive mechanical ventilation (29.9% versus 13.9%, P<0.001). Thrombotic events (19.4% versus 10.2%, P<0.001) and acute kidney injury (42.4% versus 19.0%, P<0.001) were more common in the elevated D-dimer group (Figure 1; Table I in the Data Supplement). After adjustment for demographics, comorbidities, prior medications, and baseline laboratory values, elevated D-dimer was associated with higher odds of critical illness (OR, 2.4 [95% CI, 1.9–3.1], P<0.001), thrombotic events (OR, 1.9 [95% CI, 1.4–2.6]; P<0.001), and acute kidney injury (OR, 2.4 [95% CI, 1.9–3.1]; P<0.001). Rates of critical illness, thrombosis, and acute kidney injury increased with the level of D-dimer (Figure II in the Data Supplement), which remained significant after multivariable adjustment (Table 2). Individuals with a presenting D-dimer >2000 ng/mL had the highest risk of critical illness (65.4%), thrombotic event (36.9%), and acute kidney injury (58.7%). All adjusted models had c-indices >0.75, indicating reasonable discriminatory ability of the models. D-dimer trajectory by critical illness, thrombosis, and acute kidney injury are presented in Figure 2A through 2C. D-dimer levels generally peaked ≈5 days into hospitalization.
Figure 1.
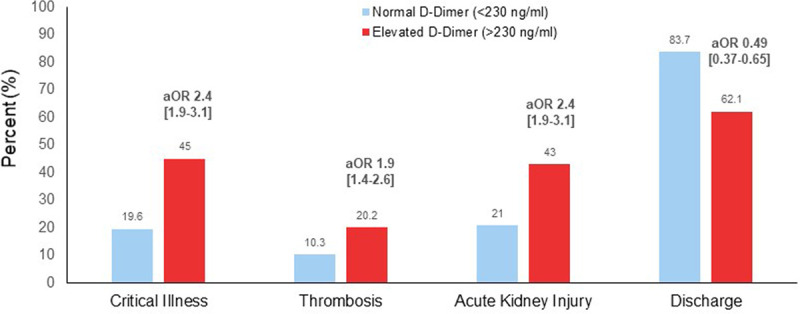
Baseline D-dimer measurements and adverse events. aOR indicates adjusted odds ratio.
Table 2.
Unadjusted and Adjusted OR for Patient Outcomes

Figure 2.
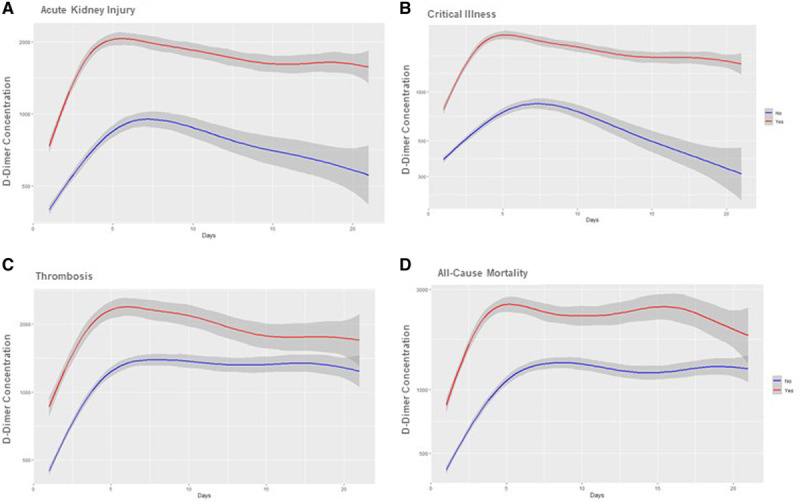
Trajectory of D-dimer during the first 21 d of hospitalization. Patients are stratified by (A) acute kidney injury, (B) critical illness, (C) thrombosis, and (D) all-cause mortality. The breakdown of thrombosis is: all thrombosis, n=410; deep venous thrombosis, n=103; pulmonary embolism, n=68; myocardial infarction, n=208; ischemic stroke, n=37; systemic embolism, n=22.
D-Dimer and All-Cause Mortality
Among the 2377 hospitalized patients with COVID-19, 608 (25.6%) died or were discharged to hospice, 1652 patients (69.5%) were discharged, and the rest (117 [4.9%]) remained hospitalized. Unadjusted mortality was higher among patients with versus without elevated baseline D-dimer (548 [29.9%] versus 60 [10.8%]; OR, 3.5 [95% CI, 2.7–4.7]; P<0.001) as shown in Figure 3. The multivariable adjusted odds ratio showed a significantly higher odds of death in patients with elevated D-dimer than in those without (OR, 2.1 [95% CI, 1.6–2.9]; P<0.001). Mortality increased in association with the level of D-dimer (Figure 3). The association between elevated D-dimer and mortality was consistent across multiple subgroups, including age, sex, body mass index, hypertension, atrial fibrillation, and kidney disease (Figure III in the Data Supplement). Individuals with a presenting D-dimer >2000 ng/mL had the highest risk of all-cause mortality (48.3%). D-dimer trajectory by all-cause mortality is presented in Figure 2D.
Figure 3.
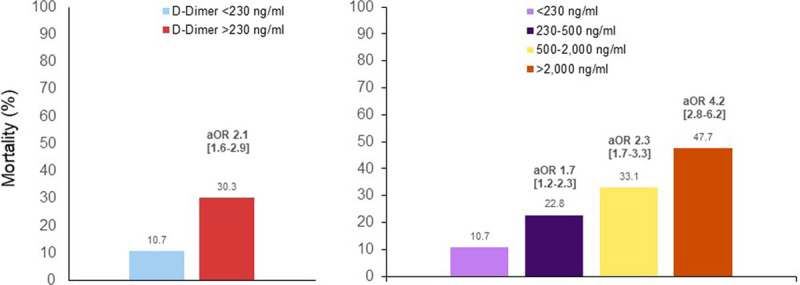
Baseline D-dimer measurements and all-cause mortality. All-cause mortality is defined as death or transfer to inpatient hospice. aOR indicates adjusted odds ratio.
Peak D-Dimer and Clinical Outcomes
Individuals with the highest peak D-dimer concentrations had the highest risk of critical illness, thrombotic events, acute kidney injury, and mortality (Figure IV in the Data Supplement). Among 301 (12.7%) individuals with a peak D-dimer >10 000 ng/mL, critical illness was present in 86.1%, thrombotic events in 39.5%, and acute kidney injury in 80.8%, and in-hospital mortality was 60.5% (Table II in the Data Supplement).
Discussion
Among 2377 adults hospitalized with COVID-19 at 4 hospitals within a large health system in New York City, 1823 (76%) had evidence of elevated D-dimer above the laboratory-specific upper limit of normal at hospital presentation and 2049 (86%) had an elevated D-dimer at any point during the hospitalization before discharge. Outcomes of patients with elevated D-dimer at the time of admission were particularly poor, with 45% critically ill, 20% with thrombosis, and 43% with acute kidney injury. D-dimer level was independently associated with these outcomes after multivariable adjustment for demographics, clinical characteristics, and other biomarkers that we have previously shown are associated with adverse outcomes.1 In contrast, individuals without an elevated D-dimer at presentation were more likely to be discharged without developing a critical illness. This is the first report to (1) demonstrate a robust association between elevated D-dimer, measured at admission and during hospitalization, and critical illness and mortality after covariate adjustment, (2) provide associations between D-dimer and other important clinical outcomes, such as thrombosis and acute kidney injury, and (3) analyze the relationship between level of D-dimer and trajectory with the frequency of adverse clinical events.
Coagulation abnormalities are increasingly recognized in hospitalized patients with COVID-19, including increased D-dimer, elevated fibrinogen, and increasing prothrombin time. While the most typical finding in patients with COVID-19 and a prothrombotic state is an increased D-dimer concentration,15 the level of D-dimer at presentation and its trajectory during the course of hospitalization is largely unknown. In a series of patients with COVID-19 across mainland China, elevated D-dimer (>500 ng/mL) on admission was present in 260 (46%) of 560 patients.23 A report of 172 patients from Wuhan, China noted that 32%, 26%, and 42% had a baseline D-dimer ≤500, >500 to ≤1000, and >1000 ng/mL, respectively.18 Most studies reporting on D-dimer do not report the proportion of individuals with abnormal D-dimer (>upper limit of normal) nor do they characterize different D-dimer cutoffs. This is the first report to examine the D-dimer trajectory during hospitalization.
Abnormalities in D-dimer in patients with COVID-19 is associated with an increased risk of critical illness and death.4,5,18 A meta-analysis of 18 studies with 3682 patients noted a higher D-dimer in patients with severe versus nonsevere infection.16 In a subgroup of 4 studies that reported critical illness (n=1218) and death (n=795), there was a 2-fold and 4-fold higher risk with of critical illness and death, respectively, among patients with D-dimer ≥500 versus <500 ng/mL.16 In one study of 191 patients from Wuhan, China with 54 deaths, Zhou et al18 found that D-dimer >1000 ng/mL at baseline was associated with an 18-fold increased risk of mortality after multivariable adjustment. However, because of the limited sample size and wide CIs, much uncertainty remains around this association.
D-dimer can only be generated when there is formation and degradation of cross-linked fibrin, provides a global marker of activation of the coagulation and fibrinolysis, and is therefore reflective of enhanced thrombotic activity.11 In fact, several pathological reports demonstrate massive amounts of micro and macro thrombi in multiple vascular beds in COVID-19.24,25 There is also evidence to suggest that D-dimer may not only be a marker of hypercoagulability and a prothrombotic state but may participate in pathogenesis. Fibrin degradation products induce acute pulmonary dysfunction and have a direct procoagulant effect. Infusion of purified human fragment D into rabbits induces pulmonary capillary leakage and hypoxemia.26 Fragment D also increases platelet aggregation and prostaglandin synthesis, activates complement, and induces chemotaxis of neutropenia.27
Our results boost the scientific rationale for clinical trials to reduce thrombotic risk and adverse outcomes. Patients with COVID-19 are at heightened risk for both arterial and venous thrombotic events.4,5 Cohort studies suggest that the incidence of thromboembolic complications in patients with COVID-19 ranges from 11% to 35%.15 A retrospective study done in China that included 449 hospitalized critically ill COVID-19 patients showed a lower mortality in patients who received prophylactic heparin >7 days than in patients not receiving anticoagulant treatment.28 Based on the limited data available, the International Society of Thrombosis and Hemostasis recommends a universal strategy of routine prophylactic dosed anticoagulation with unfractionated heparin or low-molecular weight heparin, after careful assessment of bleeding risk.29 A retrospective study of 109 patients hospitalized with severe COVID-19 infection found a high incidence of thromboembolic events despite VTE prophylaxis.30 A retrospective analysis of 2773 hospitalized patients with COVID-19 found no benefit of high-dose anticoagulation; however, a subgroup analysis in subjects treated with mechanical ventilation suggested a potential benefit with high-dose anticoagulation.31 Of note, patients infected with COVID-19 treated with anticoagulation are experiencing significant bleeding complications as well.32 The optimal strategy to prevent adverse clinical events is being studied in the ACTIV-4 (Accelerating COVID-19 Therapeutic Interventions and Vaccines-4) Antithrombotic Trial (URL: http://www.clinicaltrials.gov). Unique identifier: NCT04359277) among hospitalized patients with COVID-19 with elevated D-dimer.
Limitations
D-dimer levels were not routinely collected in all individuals; patients without any D-dimer level collected were excluded, and patients with worsening disease may have had D-dimers checked more frequently. Nonetheless, 85% of all subjects hospitalized had at least one D-dimer level measured, and associations between baseline D-dimer and outcomes were robust even after adjustment for demographics, clinical characteristics, baseline medications, and initial laboratory results. Moreover, a standardized admission laboratory protocol was only established about 2 weeks into the epidemic, resulting in missing D-dimer data for earlier patients, especially those who were less acutely ill. However, missing D-dimer was not associated with clinical events.1 Second, although critical illness, acute kidney injury, and mortality were objective end points, thrombotic events were based on diagnoses assigned by treating physicians and were not independently adjudicated. The impact of ascertainment bias or diagnostic suspicion bias is unknown. Third, it is possible that the observed associations between D-dimer and outcomes are confounded by yet-to-be-determined factors; however, we adjusted our analysis for established and novel risk factors. Furthermore, we found comparable and robust odds ratios in and across risk groups, including low and high cardiovascular risk groups. Finally, only in-hospital events were captured in this analysis. We did not assess the association between D-dimer and subsequent cardiovascular events after hospital discharge.
Conclusions
D-dimer levels were independently associated with a higher risk of critical illness, thrombosis, acute kidney injury, and all-cause mortality among patients with COVID-19, independent of previously identified risk factors. The present study provides additional support that COVID-19 is a coagulopathic condition with D-dimer representing a direct link between COVID-19 infection and adverse outcomes.
Sources of Funding
Funding from this project was supported in part by the NYU CTSA (New York University Clinical and Translational Science Award) grant UL1TR001445, from the National Center for Advancing Translational Sciences (NCATS). Dr Berger is funded, in part, by the National Heart and Lung Blood Institute of the National Institutes of Health (R01HL139909 and R35HL144993).
Disclosures
None.
Supplementary Material
Footnotes
Nonstandard Abbreviations and Acronyms
- ACE-I
- angiotensin-converting enzyme-inhibitor
- COVID-19
- coronavirus disease 2019
- IQR
- interquartile range
- PROTECT
- Prophylactic versus Therapeutic Anticoagulation Trial
- VTE
- venous thromboembolism
For Sources of Funding and Disclosures, see page 2546.
The Data Supplement is available with this article at https://www.ahajournals.org/doi/suppl/10.1161/ATVBAHA.120.314872.
References
- 1.Petrilli CM, Jones S, Yang J, Rajagopalan H, O’Donnell L, Chernyak Y, Tobin KA, Cerfolio RJ, Francois F, Horwitz LI. Factors associated with hospital admission and critical illness among 5279 people with coronavirus disease 2019 in New York City: prospective cohort study. BMJ. 2020;369:m1966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Guo T, Fan Y, Chen M, Wu X, Zhang L, He T, Wang H, Wan J, Wang X, Lu Z. Cardiovascular implications of fatal outcomes of patients with coronavirus disease 2019 (COVID-19). JAMA Cardiol. 2020;5:1–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bangalore S, Sharma A, Slotwiner A, Yatskar L, Harari R, Shah B, Ibrahim H, Friedman GH, Thompson C, Alviar CL, et al. ST-segment elevation in patients with COVID-19 - a case series. N Engl J Med. 2020;382:2478–2480 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Klok FA, Kruip MJHA, van der Meer NJM, Arbous MS, Gommers DAMPJ, Kant KM, Kaptein FHJ, van Paassen J, Stals MAM, Huisman MV, et al. Incidence of thrombotic complications in critically ill ICU patients with COVID-19. Thromb Res. 2020;191:145–147 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cui S, Chen S, Li X, Liu S, Wang F. Prevalence of venous thromboembolism in patients with severe novel coronavirus pneumonia. J Thromb Haemost. 2020;18:1421–1424 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Batlle D, Soler MJ, Sparks MA, Hiremath S, South AM, Welling PA, Swaminathan S; COVID-19 and ACE2 in Cardiovascular, Lung, and Kidney Working Group. Acute kidney injury in COVID-19: emerging evidence of a distinct pathophysiology. J Am Soc Nephrol. 2020;31:1380–1383. doi: 10.1681/ASN.2020040419 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Yaghi S, Ishida K, Torres J, Grory BM, Raz E, Humbert K, Henninger N, Trivedi T, Lillemoe K, Alam S, et al. SARS2-CoV-2 and stroke in a New York healthcare system [published correction appears in Stroke. 2020 Aug;51(8):e179]. Stroke. 2020;51:2002–2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bilaloglu S, Aphinyanaphongs Y, Jones S, Iturrate E, Hochman J, Berger JS. Thrombosis in hospitalized patients with COVID-19 in a New York City health system [published online July 20, 2020]. JAMA. doi: 10.1001/jama.2020.13372. https://jamanetwork.com/journals/jama/fullarticle/2768715 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chen N, Zhou M, Dong X, Qu J, Gong F, Han Y, Qiu Y, Wang J, Liu Y, Wei Y, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020;395:507–513. doi: 10.1016/S0140-6736(20)30211-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Adam SS, Key NS, Greenberg CS. D-dimer antigen: current concepts and future prospects. Blood. 2009;113:2878–2887. doi: 10.1182/blood-2008-06-165845 [DOI] [PubMed] [Google Scholar]
- 11.Weitz JI, Fredenburgh JC, Eikelboom JW. A test in context: D-dimer. J Am Coll Cardiol. 2017;70:2411–2420. doi: 10.1016/j.jacc.2017.09.024 [DOI] [PubMed] [Google Scholar]
- 12.Bockenstedt P. D-dimer in venous thromboembolism. N Engl J Med. 2003;349:1203–1204. doi: 10.1056/NEJMp030084 [DOI] [PubMed] [Google Scholar]
- 13.Naik RP, Wilson JG, Ekunwe L, Mwasongwe S, Duan Q, Li Y, Correa A, Reiner AP. Elevated D-dimer levels in African Americans with sickle cell trait. Blood. 2016;127:2261–2263. doi: 10.1182/blood-2016-01-694422 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kabrhel C, Mark Courtney D, Camargo CA, Jr, Plewa MC, Nordenholz KE, Moore CL, Richman PB, Smithline HA, Beam DM, Kline JA. Factors associated with positive D-dimer results in patients evaluated for pulmonary embolism. Acad Emerg Med. 2010;17:589–597. doi: 10.1111/j.1553-2712.2010.00765.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Levi M, Thachil J, Iba T, Levy JH. Coagulation abnormalities and thrombosis in patients with COVID-19. Lancet Haematol. 2020;7:e438–e440. doi: 10.1016/S2352-3026(20)30145-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Shah S, Shah K, Patel SB, Patel FS, Osman M, Velagapudi P, Turagam MK, Lakkireddy D, Garg J. Elevated D-Dimer Levels are Associated with Increased Risk of Mortality in COVID-19: A Systematic Review and Meta-Analysis. https://www.medrxiv.org/content/10.1101/2020.04.29.20085407v1. Accessed May 5, 2020.
- 17.Tang N, Li D, Wang X, Sun Z. Abnormal coagulation parameters are associated with poor prognosis in patients with novel coronavirus pneumonia. J Thromb Haemost. 2020;18:844–847. doi: 10.1111/jth.14768 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Z, Xiang J, Wang Y, Song B, Gu X, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395:1054–1062. doi: 10.1016/S0140-6736(20)30566-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chen T, Wu D, Chen H, Yan W, Yang D, Chen G, Ma K, Xu D, Yu H, Wang H, et al. Clinical characteristics of 113 deceased patients with coronavirus disease 2019: retrospective study. BMJ. 2020;368:m1091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ackermann M, Verleden SE, Kuehnel M, Haverich A, Welte T, Laenger F, Vanstapel A, Werlein C, Stark H, Tzankov A, et al. Pulmonary vascular endothelialitis, thrombosis, and angiogenesis in COVID-19. N Engl J Med. 2020;383:120–128 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wichmann D, Sperhake JP, Lütgehetmann M, Steurer S, Edler C, Heinemann A, Heinrich F, Mushumba H, Kniep I, Schröder AS, et al. Autopsy findings and venous thromboembolism in patients with COVID-19: a prospective cohort study. Ann Intern Med. 2020;173:268–277. doi: 10.7326/M20-2003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Levin A, Warnock DG, Mehta RL, Kellum JA, Shah SV, Molitoris BA, Ronco C; Acute Kidney Injury Network Working Group. Improving outcomes from acute kidney injury: report of an initiative. Am J Kidney Dis. 2007;50:1–4. doi: 10.1053/j.ajkd.2007.05.008 [DOI] [PubMed] [Google Scholar]
- 23.Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, He JX, Liu L, Shan H, Lei CL, Hui DSC, et al. ; China Medical Treatment Expert Group for Covid-19. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382:1708–1720. doi: 10.1056/NEJMoa2002032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.McGonagle D, O'Donnell JS, Sharif K, Emery P, Bridgewood C. Immune mechanisms of pulmonary intravascular coagulopathy in COVID-19 pneumonia. Lancet Rheumatol. 2020;2:e437–e445 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Menter T, Haslbauer JD, Nienhold R, Savic S, Hopfer H, Deigendesch N, Frank S, Turek D, Willi N, Pargger H, et al. Postmortem examination of COVID-19 patients reveals diffuse alveolar damage with severe capillary congestion and variegated findings in lungs and other organs suggesting vascular dysfunction [published online May 4, 2020]. Histopathology. doi: 10.1111/his.14134. https://onlinelibrary.wiley.com/doi/full/10.1111/his.14134 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Manwaring D, Curreri PW. Cellular mediation of respiratory distress syndrome induced by fragment D. Ann Chir Gynaecol. 1981;70:304–307 [PubMed] [Google Scholar]
- 27.Manwaring D, Curreri PW. Platelet and neutrophil sequestration after fragment D-induced respiratory distress. Circ Shock. 1982;9:75–80 [PubMed] [Google Scholar]
- 28.Tang N, Bai H, Chen X, Gong J, Li D, Sun Z. Anticoagulant treatment is associated with decreased mortality in severe coronavirus disease 2019 patients with coagulopathy. J Thromb Haemost. 2020;18:1094–1099 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Thachil J, Tang N, Gando S, Falanga A, Cattaneo M, Levi M, Clark C, Iba T. ISTH interim guidance on recognition and management of coagulopathy in COVID-19. J Thromb Haemost. 2020;18:1023–1026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Maatman TK, Jalali F, Feizpour C, Douglas A, II, McGuire SP, Kinnaman G, Hartwell JL, Maatman BT, Kreutz RP, Kapoor R, et al. Routine venous thromboembolism prophylaxis may be inadequate in the hypercoagulable state of severe coronavirus disease 2019 [published online May 27, 2020]. Crit Care Med. doi: 10.1097/CCM.0000000000004466. https://journals.lww.com/ccmjournal/FullText/2020/09000/Routine_Venous_Thromboembolism_Prophylaxis_May_Be.33.aspx [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Paranjpe I, Fuster V, Lala A, Russak AJ, Glicksberg BS, Levin MA, Charney AW, Narula J, Fayad ZA, Bagiella E, et al. Association of treatment dose anticoagulation with in-hospital survival among hospitalized patients with COVID-19. J Am Coll Cardiol. 2020;76:122–124. doi: 10.1016/j.jacc.2020.05.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Dogra S, Jain R, Cao M, Bilaloglu S, Zagzag D, Hochman S, Lewis A, Melmed K, Hochman K, Horwitz L, et al. Hemorrhagic stroke and anticoagulation in COVID-19. J Stroke Cerebrovasc Dis. 2020;29:104984 doi: 10.1016/j.jstrokecerebrovasdis.2020.104984 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


