Abstract
Evidence suggests that dissociation is associated with psychotic experiences, particularly hallucinations, but also other symptoms. However, until now, symptom-specific relationships with dissociation have not been comprehensively synthesized. This is the first prospectively registered (CRD42017058214) meta-analysis to quantify the magnitude of association between dissociative experiences and all symptoms of psychosis. MEDLINE, PsycINFO, PubMed, and Scopus databases were searched using exhaustive terms denoting dissociation and psychotic symptoms. We included both nonclinical (58 studies; 16 557 participants) and clinical (46 studies; 3879 patient participants) samples and evaluated study quality. Ninety-three eligible articles considering 20 436 participants were retained for analysis. There was a robust association between dissociation and clinical and nonclinical positive psychotic symptoms (r = .437; 95%CI: .386 −.486), with the observed effect larger in nonclinical studies. Symptom-specific associations were also evident across clinical and nonclinical studies, and included significant summary effects for hallucinations (r = .461; 95%CI: .386 −.531), delusions (r = .418; 95%CI: .370 −.464), paranoia (r = .447; 95%CI: .393 −.499), and disorganization (r = .346; 95%CI: .249 −.436). Associations with negative symptoms were small and, in some cases, not significant. Overall, these findings confirm that dissociative phenomena are not only robustly related to hallucinations but also to multiple positive symptoms, and less robustly related to negative symptoms. Our findings are consistent with proposals that suggest certain psychotic symptoms might be better conceptualized as dissociative in nature and support the development of interventions targeting dissociation in formulating and treating psychotic experiences.
Keywords: dissociation, psychosis, childhood trauma, meta-analysis
Introduction
The concept of dissociation has become a focus of considerable interest for the psychosis field over the past few years, with research examining its importance for the historical concept of schizophrenia,1 the prevalence of undiagnosed dissociative disorders in psychotic populations,2 the possibility of hybrid dissociative/psychotic disorders,3 and the role of dissociation in psychotic symptoms.4 The latter domain is the focus of this meta-analysis.
Dissociation has been defined by DSM-5 as “a disruption of and/or discontinuity in the normal integration of consciousness, memory, identity, emotion, perception, body representation, motor control, and behaviour.” 5(p291) Dissociation, and the dissociative disorders, are generally seen as resulting from traumatizing experiences; in recognition of this, dissociative symptoms are now formally recognized in other disorders typically seen as trauma-related, including borderline personality disorder and posttraumatic stress disorder.5 As trauma is increasingly seen as a causal risk factor in the development of psychosis, the relevance of dissociative experiences to psychosis is being explored with more vigor.6 Indeed, some have gone so far to suggest that certain psychotic symptoms, particularly auditory hallucinations and delusions of control or passive influence experiences, are better classified as dissociative than psychotic.3,7 The frequency with which the so-called first rank or Schneiderian symptoms are found in dissociative disorders lends weight to this argument.8 In turn, the concept of psychiatric disorders as discrete “disease entities” linked to distinct biological or genetic etiologies only present in those who meet criteria for specific conditions is increasingly contested.9 Considerable evidence further suggests that psychosis, like dissociative experiences, exists on a continuum with normal functioning and that its presentation cuts across diagnostic boundaries without being necessarily pathognomonic for any specific disorder.10
The concept of dissociation refers to a range of phenomena, including experiences encompassing various forms of “psychological detachment” (eg, depersonalization, derealization) as well as compartmentalization of mental experiences (eg, identity disturbances and dissociative amnesia).11 Significantly, meta-analytic studies have confirmed that dissociation is elevated in people with diagnoses in the schizophrenia-spectrum,12,13 suggesting that dissociation may be related to symptoms commonly observed in people who receive diagnoses of psychotic disorders. The association between auditory hallucinations and dissociation has attracted particular research attention, with a meta-analysis of 19 investigations reporting large associations between the two across both clinical and nonclinical populations.14 However, whilst the association with auditory hallucinations appears well-replicated, this does not imply that dissociation is uniquely associated with a greater predisposition to only report this symptom. In fact, research studies have found significant positive associations between dissociative experiences and both delusions4 and paranoia15 as well as respective subsyndromal psychotic-like symptoms in nonclinical samples.16 A significant relationship has also been reported, albeit less consistently, between dissociation and negative symptoms.17
Whilst recent meta-analytic evidence suggests the presence of considerable symptom overlap between diagnoses of schizophrenia spectrum disorders and dissociative disorders,18 no evidence synthesis to date has systematically examined the magnitude and consistency of the associations between discrete symptoms of psychosis and measures of dissociation. The value of investigating symptom-specific associations is especially pertinent due to the fact that different psychotic experiences may have distinct etiologies. Furthermore, clarifying these associations would be relevant to recent trends toward more symptom-specific and personalized targeted therapies for distressing psychotic symptoms.19
The primary aim of this meta-analysis was, therefore, to examine and synthesize associations between dissociation and the full range of psychosis symptomatology. A secondary aim was to assess the relationship between dissociation and psychosis symptomatology in both clinical and nonclinical populations and to report on the similarities and differences between them.
Method
Search Strategy
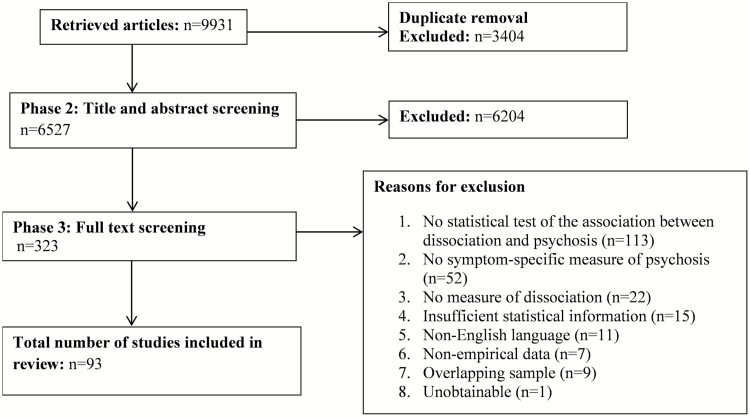
This review was conducted and reported according to PRISMA20 and its protocol registered on Prospero (CRD42017058214; for PRISMA guidelines, see supplementary table S1). MEDLINE, PsycINFO, PubMed, and Scopus were systematically searched using strings for dissociative and psychotic symptoms: (dissociat* OR depersonali* OR dereali* OR absorption OR multiple personalit*) AND (psychosis OR psychotic OR schizophren* OR hallucinat* OR voices OR visions OR delusion* OR paranoi* OR cognitive disorgani* OR positive symptoms OR negative symptoms OR first-rank symptoms OR Schneiderian). A hand-search of references and citations from eligible articles was also performed in order to identify additional studies. Primary searches were completed in April 2017 and updated in January 2020. Articles were subsequently assessed for eligibility based on screening of titles, abstracts, and full texts and only retained for review with consensus agreement from at least three reviewers. Details of the search and screening procedure are presented in figure 1.
Fig. 1.
Flow diagram of systematic search.
Inclusion and Validity
Studies meeting the following criteria were included for review: (1) published in English in a peer-reviewed journal, (2) use of self-report measures of dissociation, (3) use of self-report measures of psychotic symptoms, and (4) use of quantitative methods to report on the association between dissociative experiences and psychotic symptoms. Studies meeting these criteria were subsequently excluded if: (1) they were presented in a conference abstract or single case study format; (2) global scores of psychosis measures were provided rather than separate measures of positive and/or negative symptoms; (3) the study did not report sufficient statistical information to estimate effect sizes; and (4) there were overlapping participant samples. When multiple reports considered overlapping samples, we only included the report which provided a more precise estimate of the effects (ie, considered a larger sample size) or contained more complete statistical information to estimate relevant effects. No restrictions were placed on age or diagnostic status of participants, study design, or study start date.
Study quality was evaluated using relevant items from the Effective Public Health Practice Project tool21 (EPHPP). This is an instrument used to evaluate health research on the basis of study design and methodology, sample selection, and analytic methods and has demonstrated validity22 and inter-rater reliability.23 Studies were assessed by A.B. Oversight was provided by F.V., E.L., and S.B., with any queries or disagreements over scoring decisions resolved amongst these authors.
Data Extraction
Data extraction was conducted by the first two authors and systematically checked for accuracy by F.V. Information extracted from the primary studies was recorded on a standardized form and included general characteristics (eg, county, publication year), design, sample characteristics (eg, age, gender, diagnostic status), measures used to assess psychotic symptoms and dissociative experiences, the specific symptoms and subtypes of dissociation considered in the article, and statistical information to compute relevant effect sizes.
Effect Size Computation and Statistical Analysis
Analyses were conducted using CMA v.2. Results were pooled using a random-effects meta-analysis. Pearson’s r correlation coefficient was used as the primary metric, as effect sizes of the r-family were most commonly reported in the literature. When studies reported statistical information consistent with other families of effects (eg, d-family and binary effects), these were converted to effect sizes of the r family using computations methods outlined by Borenstein et al.24 To ensure that different study designs (ie, between-group and correlational) did not impact the findings, a subgroup analysis was conducted to contrast the magnitude of the aggregated correlational and between-group effects extracted from the primary studies. In all analyses, heterogeneity was assessed using the Q-test and the I2 statistic. Publication bias was also assessed through visual inspection of funnel plots and Egger’s tests. When evidence of publication or other selection bias was evident, analyses were followed with the trim-and-fill method to estimate the influence of potentially missing studies on summary effects.
The following analytic approach was taken. First, we summarized effects considering the relationship between dissociation and global symptom cluster measures (ie, positive, negative, and disorganization symptoms). These analyses were first conducted by including studies which reported effects for total symptom cluster measures (eg, PANSS positive symptom scores) as well as aggregated effect estimates in the case of studies that provided statistical information pertaining to specific symptoms within that cluster (ie, aggregated effects for studies reporting multiple correlation coefficients between dissociation and positive symptom measures, eg, hallucinations and delusions). These analyses were followed-up through multiple subgroup analyses, including: (1) comparison of clinical and nonclinical studies and (2) sensitivity analyses focusing on total symptom cluster measures (when sufficient numbers of studies were available). Secondly, for each cluster of symptoms, multiple meta-analyses were conducted to examine the association between dissociative experiences and specific symptoms of psychosis. Whenever the number of studies allowed it, we also explored the association between various psychosis symptoms and symptom clusters and specific subtypes of dissociation assessed by the Dissociative Experiences Scale25 (DES-II: ie, absorption, depersonalization/derealization, and amnesia).
Results
The search strategy resulted in 9931 articles. Following title/abstract screening, 323 studies were retained for full-text review, resulting in 93 included articles (see figure 1). A description of these studies is available in supplementary table S2 and effect sizes for individual studies included in the positive symptom, negative symptom, and disorganization analyses are presented in supplementary table S3.
Demographic Characteristics
The eligible studies comprised a total of 20 436 participants. Of these, 11 791 were women and 7627 were men, with a mean age of 27.07 years. Six studies did not specify gender and 19 did not specify age. In total, 58 presented data from nonclinical populations (n = 16 557) and 46 from patient groups (n = 3879).
Quality Assessment
Results of the EPHHP quality ratings are presented in supplementary table S2. Most studies fell within the “moderate” rating (n = 43; 46.2%), with 33.3% rated “strong” (n = 31) and 20.4% “weak” (n = 19). Overall ratings reflected the methodological limitations typical of cross-sectional, correlational literature, namely limited control of confounding variables and selection bias.
Relationship Between Dissociation and Positive Symptoms
Global Positive Symptoms.
A random-effect meta-analysis of 98 effects found a robust association between clinical and nonclinical positive psychotic symptoms and dissociation, r = .437 (95%CI: .386 −.486). Heterogeneity analyses indicated that there was considerable statistical inconsistency, Q(97) = 3135.421, P < .001, I2 = 96.907; hence, caution should be taken when interpreting this summary effect. No influential cases were found, but the Egger’s test indicated possible bias, t(96) = 5.222, P < .001. The imputation of 12 hypothetically missing studies using the trim-and-fill method led to a marginal decrease in the summary effect, which remained of moderate magnitude: r = .402 (95%CI: .353 −.448).
A subgroup analysis comparing clinical (k = 42) and nonclinical studies (k = 51) indicated that the relationship between dissociation and positive symptoms was significantly larger in nonclinical (r = .475, 95%CI: .426 −.521) than clinical studies (r = .388, 95%CI: .311 −.459; Q(1) = 3.902, P = .048). Considerable heterogeneity was apparent in both subgroup analyses (I2 = 93.647% and 92.616%, respectively). There was no significant difference between correlational (r = .457, 95%CI: .420 −.492) and between-group effects (r = .337, 95%CI: .189 −.470) extracted from the primary studies (Q(1) = 2.821, P = .093).
We further examined associations between total positive symptoms and dissociation subtypes assessed by the DES-II. In this analysis, it was impossible to directly contrast the summary effect sizes pertaining to different subtypes due to nonindependence of the effects extracted from the primary studies. The analysis indicated that summary effects were generally similar in magnitude: absorption (k = 33; r = .460, 95%CI: .409 −.509), amnesia (k = 18, r = .357, 95%CI: .297 −.415), and depersonalization/derealization (k = 24, r = .405, 95%CI: .355 −.452).
A sensitivity analysis was conducted by restricting the above random-effect meta-analyses to studies that considered total measures of positive symptoms in clinical (eg, PANSS positive scale) and nonclinical samples (ie, total positive schizotypy measures like the SPQ). The results were largely comparable to those reported above. With 267 independent effects included for analysis, the summary effects for associations between positive symptoms and dissociation across clinical and nonclinical studies was r = .401 (95%CI: .305 −.489). There were high levels of heterogeneity, Q(26) = 384.884, P < .001, I2 = 93.246, but no evidence of publication bias was found (t(26) = 1.808, P = .171). The summary effect for the association between dissociative experiences and positive symptoms was substantially larger in nonclinical (k = 9, r = .511, 95%CI: .430 −.583) than clinical studies (k = 17, r = .331, 95%CI: .208 −.444; Q(1) = 6.530, P = .011). Subgroup analyses focusing on dissociation subtypes found moderate-to-large associations for absorption (k = 6; r = .473, 95%CI: .381 −.556) but only small associations for amnesia (k = 2, r = .178, 95%CI: −.043 −.382) and depersonalization/derealization (k = 5, r = .181, 95%CI: .019 −.334). These two findings may be related, as absorption experiences typically fall on the “normal” (nonclinical) end of the dissociation continuum.
Hallucinations.
A random-effect meta-analysis considering 50 effects found evidence of a robust but statistically heterogeneous association between hallucinatory experiences and dissociation: r = .461 (95%CI: .386 −.531), Q(49) = 2864.317, P < .001, I2 = 98.289. No influential cases were identified, and inspection of the funnel plot and the Egger’s test indicated no evidence of publication or other selection bias.
A subgroup analysis was carried out to contrast clinical (k = 18) with nonclinical studies (k = 30). After removing one potential outlier,26 the analysis indicated that the relationship between dissociation and hallucinatory experiences was equivalent across the two subgroups of studies: clinical, r = .432 (95%CI: .274 −.567) and nonclinical, r = .482 (95%CI: .416 −.543); Q(1) = 0.388, P = .534. A further subgroup analysis focusing on the DES-II dissociation subtypes indicated that summary affects were robust and significant in all cases: depersonalization/derealization (k = 20, r = .470, 95%CI: .416 −.521) followed by absorption (k = 23, r = .465, 95%CI: .394 −.531) and amnesia (k = 13, r = .388, 95%CI: .328 −.445).
An additional subgroup analysis was conducted to descriptively compare the effects obtained in studies considering hallucinations in different sensory modalities. These analyses could only be conducted for auditory (k = 15) and visual experiences (k = 4) due to a low number of studies that considered hallucinations in other domains. The findings indicated that the summary effects of auditory and visual hallucinations were r = .499 (95%CI: .413 −.575) and r = .476 (95%CI: .270 −.641), respectively.
Finally, a sensitivity analysis was conducted to clarify the results of these analyses by excluding effects extracted from 9 samples that used schizotypal measures of anomalous perception (which, although overlapping with hallucinatory experiences, considered a broader range of perceptual anomalies). After the exclusion of these studies, the random-effect meta-analysis of the remaining 41 effects found evidence of a robust but heterogeneous association between hallucinatory experiences and dissociation, with results comparable to those reported above; r = .453 (95%CI: .371 −.529), Q(40) = 1900.134, P < .001, I2 = 97.895. The results of subgroup analyses contrasting clinical and nonclinical studies as well as studies focusing on the DES-II dissociation subtypes were likewise comparable to those reported in our main analyses.
Delusions.
A random-effect meta-analysis with 30 effects found a moderate-to-large, but statistically heterogeneous, association between delusions and dissociation: r = .418 (95%CI: .370 −.464), Q(29) = 164.987, P < .001, I2 = 82.423. There was no evidence of potentially influential cases or publication bias.
A subgroup analysis comparing nonclinical (k = 17) and clinical studies (k = 12) found a significantly larger summary effect in nonclinical samples: r = .480 (95%CI: .428 −.529) and r = .297 (95%CI: .238 −.354); Q(1) = 21.750, P < .001, respectively. Subgroup analyses focusing on DES-II subtypes indicated that that the summary effects of absorption (k = 8, r = .402; 95%CI: .315 −.482) were somewhat larger than those of depersonalization/derealization (k = 6, r = .305, 95%CI: .236 −.371) and amnesia (k = 4, r = .195, 95%CI: −.090 −.384).
Only a minority of studies assessed associations between specific delusional beliefs (eg, grandiose, somatic, bizarre) and dissociation. There was also considerable heterogeneity in the type of beliefs considered in these studies, which precluded our ability to carry out more fine-grained analyses.
Paranoia.
After integrating 22 effects, the summary effect size for the relationship between dissociation and paranoia was r = .447 (95%CI: .393 −.499). Substantial statistical inconsistency was observed, Q(21) = 73.295, P < .001, I2 = 71.349, but there was no evidence of publication bias or studies exerting undue influence on these findings.
A subgroup analysis carried out to compare clinical (k = 8) and nonclinical studies (k = 13) found that the association between dissociative experiences and paranoia was largely comparable across the two groups: r = .416 (95%CI: .260 −.551) and r = .470 (95%CI: .423 −.515) respectively; Q(1) = .507, P = .476. Further subgroup analyses indicated that the summary effects for the DES-II dissociative subtypes were broadly comparable: absorption (k = 6; r = .426, 95%CI: .280 −.552), amnesia (k = 5, r = .401, 95%CI: .256 −.529), and depersonalization/derealization (k = 6, r = .427, 95%CI: .307 −.533).
Relationship Between Dissociation and Negative Symptoms
Global Negative Symptoms.
A meta-analysis considering 27 effects found a small and heterogeneous relationship between negative symptoms and dissociation: r = .138 (95%CI .065 −.209), Q(26) = 135.706, P < .001, I2 = 80.841. Visual inspection of the funnel plot and Egger’s test found no evidence of publication or other selection bias.
A subgroup analysis comparing clinical (k = 14) and nonclinical studies (k = 11) indicated that the relationship between dissociation and negative symptoms was significant in the nonclinical (r = .173, 95%CI: .101 −.242) but not the clinical samples (r = −.082, 95%CI: −.031 −.192). However, the differences in these summary effects were not significant: Q(1) = 1.827, P = .176. As only 1 study provided between-group effects, no subgroup analysis with correlational effects was conducted.
A sensitivity analysis was conducted on 13 studies that considered total measures of negative symptoms. These analyses indicated that the association between dissociative experiences and negative symptoms was not statistically significant: r = .0.084 (95%CI: −.025 −.191), Q(12) = 44.815, P = .129, I2 = 73.233.
To explore potential associations between dissociation and more specific negative symptoms, we combined effects pertaining to the following categories:
Reduced Emotional Experience and/or Expressiveness.
This analysis concerned a group of symptoms comprising anhedonia, flat/blunted/shallow/flattened affect, and emotional withdrawal. It included 11 effects and found a small and heterogeneous association between dissociative experiences and the symptoms under scrutiny: r = .128 (95%CI: .043 −.210), Q(10) = 36.529, P < .001, I2 = 72.624.
Lack of Motivation, Asociality, and Withdrawal.
This symptom category covered a lack of close relationships, poor rapport, desocialization, asociality, apathy, avolition, and lack of spontaneity. This random-effects meta-analysis considered 7 effects; a small but significant summary effect was observed: r = .190 (95%CI: .090 −.285), and heterogeneity was modest within these analyses: Q(6) = 12.394, P = .03, I2 = 55.793.
Cognitive Symptoms.
This cluster considered stereotyped thinking and difficulties in abstract thinking and attention. Only 3 effects were available for this analysis. A small summary effect was found: r = −.108 (95%CI: −.287 −.472) but heterogeneity statistics indicated substantial variation: Q(2) = 12.684, P < .001, I2 = 87.248.
Relationship Between Dissociation and Disorganization
A random-effects meta-analysis including 12 effects led to a moderate summary effect pertaining to associations between disorganization symptoms and dissociation: r = .346 (95%CI: .249 −.436). Statistical heterogeneity was substantial, Q(11) = 74.051, P < .001, I2 = 85.145, but there was no evidence of publication bias or influential effects. However, one investigation27 had an uncharacteristically negative and significant effect size. A sensitivity analysis was conducted by removing this study. The results were broadly comparable to those of the main analysis above: r = .382 (95%CI: .296 −.461), Q(10) = 52.051, P < .001, I2 = 81.099. As all studies provided data to compute correlational effects, no subgroup analysis of correlational and between-group effects was conducted.
A subgroup analysis comparing clinical (k = 5) and nonclinical (k = 6) studies indicated that the relationship between dissociation and disorganization was equivalent across the two samples: r = .348 (95%CI: .036 −.587) and r = .402 (95%CI: .337 −.463); Q-test(1) = .138, P = .710, respectively. There were no sufficient data to conduct subgroup analyses focusing on dissociation subtype, nor for total measures of disorganization.
Sensitivity Analyses for Study Quality
We conducted a final sensitivity analysis to evaluate the impact of including the 19 studies deemed methodologically weaker according to EPHHP ratings. Their exclusion had minimal impact on the overall findings of our meta-analyses focusing on positive symptoms, negative symptoms, and disorganization. In all cases, the summary effects and statistical heterogeneity statistics remained comparable to those reported in our main analyses.
Discussion
This is the first meta-analysis to systematically summarize and evaluate the magnitude of the associations between dissociative experiences and all symptoms of psychosis, and the findings support the existence of a robust and well-replicated relationship. Indeed, while the majority of literature examining links between dissociation and psychosis has primarily focused on hallucinations, the current analyses suggest that dissociative phenomena are robustly related to multiple positive symptoms and appear to be related to higher disorganization. Conversely, associations with negative symptoms were of considerably smaller magnitude and, in some cases, were nonsignificant. Furthermore, the effects considered in our review were observed across both clinical and nonclinical samples (although with differences in overall magnitude), indicating that dissociation may be an important factor underlying vulnerability to psychotic experiences across the continuum of psychosis.
Firstly, our review replicates and expands previous meta-analytic findings suggesting significant links between dissociation and auditory hallucinations.14 It also indicates that dissociation is linked to hallucinations across multiple sensory modalities and that the association with visual hallucinations is of comparable strength to that of auditory. The link between dissociation and hallucinatory experiences was additionally of similar size in both clinical and nonclinical studies. Some authors have argued that this association calls for a radical shift in the way such symptoms are conceptualized by researchers and clinicians, in that hallucinations amongst psychosis patients may be better conceived as “traumatic in origin and dissociative in kind.” 4(p521) However, others have backed more cognitive perspectives; for example, that dissociation could make individuals more prone to hallucinations by increasing confusion between inner and outer experiences,28 or that heightened states of dissociation may interact with preexisting cognitive vulnerabilities (such as source monitoring biases affecting the capacity to correctly identify the source of internally and externally generated events29).
This review also indicates that dissociative experiences present large associations with paranoia and delusions. Similarly, it identified significant links with symptoms of disorganization, although these were of a somewhat smaller magnitude relative to positive symptoms. One possible explanation for these associations is trauma-related, in that paranoia and delusions may arise from flashbacks which are not recognized as such.30 These experiences, which are consistent with models of traumatic memory,31 would typically be associated with powerful feelings of depersonalization/derealization that could subsequently drive the development of delusions and other psychotic symptoms.32 In this regard, future primary and secondary research could usefully elucidate such links by examining the relationship between psychotic and dissociative phenomena in those with a history of trauma exposure relative to those without.
Our analyses also corroborate findings from previous empirical studies that suggest the magnitude of associations between dissociative phenomena and negative symptoms is less robust than for positive symptoms. When focusing on specific groups of negative symptoms (cognitive symptoms, reduced emotional experience/expressiveness, and lack of motivation, asociality, and withdrawal), we observed small but statistically significant relationships. We note, however, that the number of studies considering negative symptoms is relatively sparse and characterized by high heterogeneity in the specific symptoms examined. Although our grouping of negative symptoms is consistent with existing proposals regarding their underlying dimensional structure (eg, in terms of diminished motivation and expression33), we were limited by the small number of diverse symptoms examined in the primary studies. There is an ongoing debate around the exact underlying structure of negative symptoms,34 and concerns remain regarding the risk of conflating their assessment with extraneous complaints such as depression or medication side effects. This has the potential of biasing the accurate estimation of the relationship between negative symptoms and dissociation (as well as other psychological and neurocognitive constructs), highlighting the need for further assessment innovation and future research to corroborate these findings. There are no clear models that posit a mechanism linking dissociation to negative symptoms, and indeed patients with dissociative identity disorder are often clinically distinguished from psychotic patients by an absence of negative symptoms.
Overall, our findings support proposals that certain psychotic symptoms might be better conceptualized as dissociative in nature.4 They are also consistent with evidence suggesting common etiological underpinnings between dissociation and symptoms of psychosis. In this respect, dissociation is common in individuals who have endured potentially traumatizing events35 and the risk for, and severity of, psychotic symptoms has been overwhelmingly linked to similar traumatic exposures.36,37 Furthermore, meta-analytic evidence suggests that dissociation in people with mental health difficulties, including psychosis, is associated with histories of childhood trauma,38 while multiple studies suggest dissociation is a well-replicated mediator of the link between childhood adversity and psychotic symptoms.39 However, it should be noted that our meta-analysis did not consider the potential role played by peritraumatic dissociation in the etiology of psychotic experiences. This remains an under-researched topic that could be addressed in future investigations.
In terms of different dissociation subtypes, our analyses found no striking differences in their respective associations with symptoms of psychosis, although in some analyses absorption appeared to be more linked to psychotic-like experiences in nonclinical samples. However, an important caveat should be noted: our evidence synthesis only considered the bivariate associations between dissociative and psychotic symptoms. It is, therefore, not possible to establish with high confidence whether symptom-specific associations might exist between psychotic experiences and dissociation, or between psychotic experiences and specific dissociative subtypes. Multivariate analyses accounting for covariation between different psychotic and dissociative experiences might be better placed to answer such questions. When these analyses have been conducted in primary research studies, some have reported alleged symptom-specific effects (eg, in the case of auditory hallucinations) whilst others have found no strong support for dissociation exclusively impacting individual symptoms.40
The difference observed in multiple analyses regarding the relatively larger association between dissociative and psychotic symptoms in nonclinical rather than clinical samples might be explained by several factors. Notably, as patients are likely to be more symptomatic than nonclinical participants, it is possible that studies conducted on clinical samples present restricted variance which might impact the magnitude of effects extracted from these studies. However, a further complication that should be considered when appraising our findings is the comparability of assessment measures typically used in clinical investigations, such as the PANSS, and the various schizotypy measures employed by nonclinical studies (many of which are highly heterogeneous in terms of the experiences they intend to capture). Whilst it is widely accepted that psychosis exists on a continuum with non-pathological experiences and traits, it could be argued that certain phenomena considered in the nonclinical literature (eg, paranoid ideation) may not be fully comparable with their clinical counterparts (eg, persecutory delusions). It, therefore, remains a possibility that the larger effects observed in our nonclinical analyses might reflect fundamental differences in the constructs assessed by different measures.
Another potential limitation of the literature considered in this review relates to the possible comorbidity between psychotic and dissociative disorders. Few studies formally assessed the presence of comorbid dissociative diagnoses when investigating the association between psychotic experiences and dissociation, yet there is some suggestion that undiagnosed dissociative disorders are not uncommon in psychotic populations.41 Future investigations may attempt to clarify the impact of comorbidity by applying diagnostic interviews such as the Structured Clinical Interview for DSM-5 Dissociative Disorders.42 It should also be noted that medication status may have confounded results via patients exhibiting antipsychotic side effects (eg, memory problems, detachment, affective flattening) that could be mistaken for dissociation during the assessment.43 We were additionally unable to conduct dissociation subtype analyses within groups (clinical vs nonclinical) yet some studies have suggested, for example, that different subtypes of dissociation were related to hallucinations in clinical vs nonclinical voice hearers.44
Several other caveats should also be considered when interpreting our findings. Although the analyses found no substantial evidence of publication or other forms of selection bias, our search strategy was limited to peer-reviewed English-language studies and it is possible that certain relevant studies might have been overlooked. As mentioned previously, the bivariate approach may also have masked more subtle differences in the relationship between dissociation and specific psychotic symptoms. Furthermore, our meta-analysis could not directly contrast the effects between dissociation and specific symptoms as the same studies often examined multiple psychotic experiences within the same sample. Additional methodological and statistical developments in meta-analysis and aggregate analysis of individual participant datasets (eg, network analysis, meta-analytic structural equation modeling, and independent patient data meta-analysis) might enable future evidence syntheses to estimate such effects with greater precision. Although subgroup analyses were conducted to account for the most important methodological and clinical variances between the studies included in this review, the summary effects reported should still be interpreted cautiously in light of the statistical heterogeneity detected in most of our analyses.
Finally, the findings bear several implications for clinical practice. Research into the development of psychological interventions for psychosis has recently moved toward devising and evaluating more targeted treatments in order to improve the effect sizes of generic cognitive-behavioral therapies (which traditionally focused on a range of different psychotic symptoms simultaneously). Future meta-analyses may help refine the issue of whether the relationship between dissociation and psychotic experience varies across different diagnostic groups. However, the current review suggests that the role played by dissociation in the maintenance of presenting difficulties should be carefully evaluated in the context of targeted therapies for voices, delusional beliefs, and other psychotic symptoms for which a strong link with dissociation was observed. As dissociation often represents a consequence of adversity exposure, trauma-focused therapies could also represent a meaningful treatment option for many people with psychotic and dissociative experiences. The adaptation of protocols used to treat dissociation likewise represents a promising area of intervention development for psychosis. For example, reconceptualizing voices as dissociated parts of the self and using dialogical approaches to improve relationships between hearer and voice is one instance of applying techniques developed in the dissociation field amongst psychosis populations.45 Such an intervention is currently undergoing controlled evaluation amongst patients with schizophrenia spectrum diagnoses (ISRCTN45308981), and if effective could represent a treatment advance that encapsulates the considerable clinical and conceptual overlap between dissociation and psychosis. In this respect, therapeutic approaches derived from dialogical principles may also have applicability beyond auditory hallucinations; a tradition notably begun by Laing’s46 characterization of schizophrenia as the “divided self,” and expanded by the work of theorists such as Lysaker et al47 who posit that issues of self-diminishment in psychosis can be addressed via psychotherapy that focuses on developing a coherent internal narrative.
Ultimately, our findings raise the issue of whether different psychotic symptoms do in fact have distinct etiologies. The strong association between dissociation and different types of positive symptoms suggests that they may have similar causal factors. Evidence suggests that substantial overlaps exist in biological and socio-environmental risks across diagnostic categories and specific symptoms48 and accordingly there has been a move toward transdiagnostic therapies.49–51 Nonetheless, there are likely to be a myriad of risk and resilience factors for each symptom and the relative importance of each is liable to vary from person to person, highlighting the importance of developing individualized formulations to help understand the development of distressing symptoms within the context of psychological therapies.
Funding
E.L. is funded by a National Institute for Health Research (NIHR) Postdoctoral Fellowship Scheme (PDF-2017-10-050) for this research project. This article presents independent research funded by the NIHR: the views expressed are those of the author and not necessarily those of the NHS, the NIHR, or the Department of Health and Social Care.
Supplementary Material
Acknowledgment
The authors have declared that there are no conflicts of interest in relation to the subject of this study.
References
- 1. Moskowitz A, Heim G. Eugen Bleuler’s Dementia praecox or the group of schizophrenias (1911): a centenary appreciation and reconsideration. Schizophr Bull. 2011;37(3):471–479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Sar V, Taycan O, Bolat N, et al. Childhood trauma and dissociation in schizophrenia. Psychopathology 2010;43(1):33–40. [DOI] [PubMed] [Google Scholar]
- 3. van der Hart O, Witztum E. Dissociative psychosis: clinical and theoretical aspects. In: Moskowitz A, Dorahy MJ, Schäfer I, eds. Psychosis, Trauma and Dissociation: Evolving Perspectives on Severe Psychopathology. 2nd ed.London, UK: Wiley; 2019:307–319. [Google Scholar]
- 4. Moskowitz A, Read J, Farrelly S, Rudegeair T, Williams O. Are psychotic symptoms traumatic in origin and dissociative in kind? In: Dell PF, O’Neil JA, eds. Dissociation and the Dissociative Disorders: DSM-V and Beyond. New York, NY: Routledge/Taylor & Francis Group; 2009:521–533. [Google Scholar]
- 5. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders: DSM. 5th ed. Arlington, VA: American Psychiatric Publishing; 2013. [Google Scholar]
- 6. Moskowitz A, Heinimaa M, Van der Hart O. Defining psychosis, trauma and dissociation: historical and contemporary conceptions. In: Moskowitz A, Dorahy MJ, Schäfer I, eds. Psychosis, Trauma and Dissociation: Evolving Perspectives on Severe Psychopathology. 2nd ed.London, UK: Wiley; 2019:9–29. [Google Scholar]
- 7. Moskowitz A, Corstens D. Auditory hallucinations: psychotic symptom or dissociative experience? J Psychol Trauma. 2008;6:35–63. [Google Scholar]
- 8. Şar V, Öztürk E. Psychotic symptoms in dissociative disorders. In: Moskowitz A, Dorahy MJ, Schäfer I, eds. Psychosis, Trauma and Dissociation: Evolving Perspectives on Severe Psychopathology. 2nd ed.London, UK: Wiley; 2019:195–206. [Google Scholar]
- 9. Bentall RP. Madness Explained: Psychosis and Human Nature. London, UK: Penguin Books; 2003. [Google Scholar]
- 10. Reininghaus U, Böhnke JR, Chavez-Baldini U, et al. Transdiagnostic dimensions of psychosis in the Bipolar-Schizophrenia Network on Intermediate Phenotypes (B-SNIP). World Psychiatry. 2019;18(1):67–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Spiegel D, Lewis-Fernández R, Lanius R, Vermetten E, Simeon D, Friedman M. Dissociative disorders in DSM-5. Annu Rev Clin Psychol. 2013;9:299–326. [DOI] [PubMed] [Google Scholar]
- 12. Lyssenko L, Schmahl D, Bockhacker L, Vonderlin R, Bohus M, Kleindienst N. Dissociation in psychiatric disorders: a meta-analysis of studies using the dissociative experiences scale. Am J Psychiatry. 2018;175:37–46. [DOI] [PubMed] [Google Scholar]
- 13. O’Driscoll C, Laing J, Mason O. Cognitive emotion regulation strategies, alexithymia and dissociation in schizophrenia, a review and meta-analysis. Clin Psychol Rev. 2014;34(6):482–495. [DOI] [PubMed] [Google Scholar]
- 14. Pilton M, Varese F, Berry K, Bucci S. The relationship between dissociation and voices: a systematic literature review and meta-analysis. Clin Psychol Rev. 2015;40:138–155. [DOI] [PubMed] [Google Scholar]
- 15. Justo A, Risso A, Moskowitz A, Gonzalez A.. Schizophrenia and dissociation: its relation with severity, self-esteem and awareness of illness. Schizophr Res. 2018;197:170–175. [DOI] [PubMed] [Google Scholar]
- 16. Giesbrecht T, Merckelbach H, Kater M, Sluis AF. Why dissociation and schizotypy overlap: the joint influence of fantasy proneness, cognitive failures, and childhood trauma. J Nerv Ment Dis. 2007;195(10):812–818. [DOI] [PubMed] [Google Scholar]
- 17. Ross CA, Keyes B. Dissociation and schizophrenia. J Trauma Dissociation. 2004;5:69–83. [Google Scholar]
- 18. Renard SB, Huntjens RJ, Lysaker PH, Moskowitz A, Aleman A, Pijnenborg GH. Unique and overlapping symptoms in schizophrenia spectrum and dissociative disorders in relation to models of psychopathology: a systematic review. Schizophr Bull. 2016;43(1):108–121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Thomas N. What’s really wrong with cognitive behavioral therapy for psychosis? Front Psychol. 2015;6:323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Moher D, Liberati A, Tetzlaff J, Altman DG; PRISMA Group Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009;339:b2535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Thomas H. Quality assessmenttool for quantitative studies: effective public health practice project https://www.nccmt.ca/knowledge-repositories/search/14. Accessed August 10 2017.
- 22. Thomas BH, Ciliska D, Dobbins M, Micucci S. A process for systematically reviewing the literature: providing the research evidence for public health nursing interventions. Worldviews Evid Based Nurs. 2004;1(3):176–184. [DOI] [PubMed] [Google Scholar]
- 23. Armijo-Olivo S, Stiles CR, Hagen NA, Biondo PD, Cummings GG. Assessment of study quality for systematic reviews: a comparison of the cochrane collaboration risk of bias tool and the effective public health practice project quality assessment tool: methodological research. J Eval Clin Pract. 2012;18(1):12–18. [DOI] [PubMed] [Google Scholar]
- 24. Borenstein M, Hedges LV, Higgins JPT, Rothstein HR.. Introduction to Meta-Analysis. West Sussex, UK: Wiley; 2009. [Google Scholar]
- 25. Carlson E, Putman F. An update on the dissociative experiences scale. Dissociation. 1993;6:16–27. [Google Scholar]
- 26. Longden E, House AO, Waterman MG. Associations between nonauditory hallucinations, dissociation, and childhood adversity in first-episode psychosis. J Trauma Dissociation. 2016;17(5):545–560. [DOI] [PubMed] [Google Scholar]
- 27. Tschoeke S, Steinert T, Flammer E, Uhlmann C. Similarities and differences in borderline personality disorder and schizophrenia with voice hearing. J Nerv Ment Dis. 2014;202(7):544–549. [DOI] [PubMed] [Google Scholar]
- 28. Allen JG, Coyne L, Console DA. Dissociative detachment relates to psychotic symptoms and personality decompensation. Compr Psychiatry. 1997;38(6):327–334. [DOI] [PubMed] [Google Scholar]
- 29. Varese F, Barkus E, Bentall RP. Dissociation mediates the relationship between childhood trauma and hallucination-proneness. Psychol Med. 2012;42(5):1025–1036. [DOI] [PubMed] [Google Scholar]
- 30. Moskowitz A, Montirosso R. Childhood experiences and delusions: Trauma, memory and the double bind. In: Moskowitz A, Dorahy MJ, Schäfer I, eds. Psychosis, Trauma and Dissociation: Evolving Perspectives on Severe Psychopathology (2nd ed.). London, UK: Wiley; 2019:117–140. [Google Scholar]
- 31. Brewin CR. Episodic memory, perceptual memory, and their interaction: foundations for a theory of posttraumatic stress disorder. Psychol Bull. 2014;140(1):69–97. [DOI] [PubMed] [Google Scholar]
- 32. Hardy A. Pathways from trauma to psychotic experiences: a theoretically informed model of posttraumatic stress in psychosis. Front Psychol. 2017;8:697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Blanchard JJ, Cohen AS. The structure of negative symptoms within schizophrenia: implications for assessment. Schizophr Bull. 2006;32(2):238–245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Strauss GP, Esfahlani FZ, Galderisi S, et al. Network analysis reveals the latent structure of negative symptoms in schizophrenia. Schizophr Bull. 2019;45(5):1033–1041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Dalenberg CJ, Brand BL, Gleaves DH, et al. Evaluation of the evidence for the trauma and fantasy models of dissociation. Psychol Bull. 2012;138(3):550–588. [DOI] [PubMed] [Google Scholar]
- 36. Varese F, Smeets F, Drukker M, et al. Childhood adversities increase the risk of psychosis: a meta-analysis of patient-control, prospective- and cross-sectional cohort studies. Schizophr Bull. 2012;38(4):661–671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Bailey T, Alvarez-Jimenez M, Garcia-Sanchez AM, Hulbert C, Barlow E, Bendall S. Childhood trauma is associated with severity of hallucinations and delusions in psychotic disorders: a systematic review and meta-analysis. Schizophr Bull. 2018;44(5):1111–1122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Rafiq S, Campodonico C, Varese F. The relationship between childhood adversities and dissociation in severe mental illness: a meta-analytic review. Acta Psychiatr Scand. 2018;138(6):509–525. [DOI] [PubMed] [Google Scholar]
- 39. Williams J, Bucci S, Berry K, Varese F. Psychological mediators of the association between childhood adversities and psychosis: a systematic review. Clin Psychol Rev. 2018;65:175–196. [DOI] [PubMed] [Google Scholar]
- 40. Pearce J, Simpson J, Berry K, Bucci S, Moskowitz A, Varese F. Attachment and dissociation as mediators of the link between childhood trauma and psychotic experiences. Clin Psychol Psychother. 2017;24(6):1304–1312. [DOI] [PubMed] [Google Scholar]
- 41. Ross CA, Keyes B. Clinical features of dissociative schizophrenia in China. Psychosis 2009;1:51–60. [Google Scholar]
- 42. Steinberg M. Advances in clinical assessment: the differential diagnosis of dissociative identity disorder and schizophrenia. In: Moskowitz A, Dorahy MJ, Schäfer I, eds. Psychosis, Trauma and Dissociation: Evolving Perspectives on Severe Psychopathology. 2nd ed.London, UK: Wiley; 2019:335–349. [Google Scholar]
- 43. Longden E, Read J. Assessing and reporting the adverse effects of antipsychotic medication: a systematic review of clinical studies, and prospective, retrospective, and cross-sectional research. Clin Neuropharmacol. 2016;39(1):29–39. [DOI] [PubMed] [Google Scholar]
- 44. Perona-Garcelán S, Bellido-Zanin G, Rodríguez-Testal JF, López-Jiménez AM, García-Montes JM, Ruiz-Veguilla M. The relationship of depersonalization and absorption to hallucinations in psychotic and non-clinical participants. Psychiatry Res. 2016;244:357–362. [DOI] [PubMed] [Google Scholar]
- 45. Moskowitz A, Mosquera D, Longden E. Auditory verbal hallucinations and the differential diagnosis of psychotic and dissociative disorders: historical, empirical and clinical perspectives. Eur J Trauma Dissociation. 2017;1:37–46. [Google Scholar]
- 46. Laing RD. The Divided Self. New York, NY: Penguin Books; 1978. [Google Scholar]
- 47. Lysaker PH, Lysaker JT, Lysaker JT. Schizophrenia and the collapse of the dialogical self: recovery, narrative and psychotherapy. Psychother Theory Res Pract Train. 2001;38:252–261. [Google Scholar]
- 48. Johnstone L, Boyle M, Cromby J, et al. The Power Threat Meaning Framework: Towards the Identification of Patterns in Emotional Distress, Unusual Experiences and Troubled or Troubling Behaviour, as an Alternative to Functional Psychiatric Diagnosis. Leicester, UK: British Psychological Society; 2018. [Google Scholar]
- 49. Mansell W, Harvey A, Watkins ER, Shafran R. Cognitive behavioral processes across psychological disorders: a review of the utility and validity of the transdiagnostic approach. Int J Cog Ther. 2008;1:181–191. [Google Scholar]
- 50. Gutner CA, Presseau C. Dealing with complexity and comorbidity: opportunity for transdiagnostic treatment for PTSD. Curr Treat Options Psychiatry. 2019;6(2):119–131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Hazell CM, Hayward M, Cavanagh K, Jones AM, Strauss C. Guided self-help cognitive-behaviour Intervention for VoicEs (GiVE): results from a pilot randomised controlled trial in a transdiagnostic sample. Schizophr Res. 2018;195:441–447. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.