Abstract
Anti–thyroid peroxidase antibody (TPO-Ab), which is the known cause of autoimmune thyroid disease, enhances proinflammatory cytokine responses. Since low-grade inflammation is a known risk factor for atherosclerosis, a normal range of TPO-Ab (TPO-Ab negative) could be positively associated with atherosclerosis among participants with normal thyroid function. However, no study reported the association between normal range of TPO-Ab and atherosclerosis among eu-thyroid participants. A cross-sectional study was conducted with 1165 Japanese individuals with normal thyroid function (ie, normal range of free triiodothyronine [free T3] and free thyroxine [free T4]), aged 40 to 74 years, who participated in an annual health checkup in 2014. Among the study population, 115 were diagnosed as having atherosclerosis. A normal range value of TPO-Ab titer is revealed to be positively associated with atherosclerosis; sex, age, thyroid function (free T3 and thyroid-stimulating hormone), and known cardiovascular risk factor adjusted odds ratio and 95% confidence interval of atherosclerosis for logarithmic values of TPO-Ab was 2.23 (1.11, 4.47). When we limited the analysis to participants with normal levels of thyroid-stimulating hormone, this association became slightly stronger (2.65 [1.27,5.51]). Among the eu-thyroid general population, a normal range of TPO-Ab titer is revealed to be positively associated with atherosclerosis. Even though a TPO-Ab titer is not clinically relevant and is not associated with autoimmune thyroid disease, it could influence endothelial remodeling including atherosclerosis.
Keywords: anti-thyroid peroxidase antibody, atherosclerosis, normal thyroid function, thyroid hormone
1. Introduction
Auto-antibody such as an anti–thyroid peroxidase antibody (TPO-Ab), which is a known cause of autoimmune thyroid disease,[1] is reported to be present in low concentrations in the peripheral blood of healthy individuals.[2,3] Since TPO-Ab enhances pro-inflammatory cytokines[4] that play an important role in the progression of atherosclerosis,[5,6] a normal range of TPO-Ab titer could be positively associated with atherosclerosis among healthy participants (with normal thyroid function) as a result of low-grade inflammation.
A previous control study reported that the carotid intima-media thickness (CIMT) value of subclinical hypothyroidism subjects is significantly higher than that of normal control subjects.[7] Even if low-grade inflammation, not subclinical hypothyroidism, is to blame for the association between TPO-Ab and atherosclerosis, a normal range of TPO-Ab titer could be positively associated with atherosclerosis among eu-thyroid participants. Furthermore, this positive association could be observed even if the analysis is limited to participants with a normal range of thyroid-stimulating hormone (TSH) (excluding the influence of subclinical hypothyroidism).
Therefore, we hypothesized that independent of known confounding factors, a normal range of TPO-Ab titer is significantly positively associated with atherosclerosis among the eu-thyroid population and this association could also be observed even if there was limited analysis among participants without subclinical hypothyroidism (normal range of TSH).
To clarify the associations between normal range of TPO-Ab titer and atherosclerosis, we conducted a cross-sectional study of 1165 Japanese individuals with normal thyroid function (ie, normal range of free triiodothyronine [free T3] and free thyroxine [free T4]), aged 40 to 74 years, who participated in an annual health checkup in 2014.
2. Materials and methods
2.1. Study population
The methods that relate to the present risk survey including thyroid function have been described elsewhere.[8]
We ensured that participants understood the objective of the study and informed consent was obtained. This study was approved by the Ethics Committee of Nagasaki University Graduate School of Biomedical Sciences (project registration number 14051404).
The study population comprised 1883 Japanese individuals between the ages of 40 and 74 years from the Saza town in the western part of Japan who underwent an annual medical checkup in 2014, as recommended by the Japanese government.
To avoid the influence of thyroid disease, subjects with a history of thyroid disease (n = 60), subjects without thyroid function data such as TSH, free T3, and free T4 (n = 17), and subjects with an abnormal free T3 (normal range: 2.1–4.1 pg/mL) and free T4 (normal range: 1.0–1.7 ng/dL) range were excluded (n = 77).
Additionally, subjects without body mass index (BMI) data (n = 1), blood pressure data (n = 1), and TPO-Ab data (n = 294) were excluded. Furthermore, subjects with an abnormal range of TPO-Ab (normal range: <16 IU/mL) (n = 268) were excluded.
2.2. Data collection and laboratory measurements
In order to accurately obtain clinical data during medical examination, interviewers were trained specially. Body weight and height were measured with an automatic body composition analyzer (BF-220; Tanita, Tokyo, Japan) and BMI (kg/m2) was calculated. Systolic blood pressure and diastolic blood pressure were recorded at rest.
A fasting blood sample was collected. HbA1c, triglycerides (TG), and high-density lipoprotein cholesterol (HDLc) levels were also measured using standard procedures at SRL, Inc. (Tokyo, Japan)[9]; HbA1c and TG levels were measured by the enzyme method while the HDLc level was measured by the direct method. TSH, free T3, free T4, and TPO-Ab were measured by standard procedures at the LSI Medience Corporation (Tokyo, Japan)[10]; TSH, free T3, and free T4 were measured by chemiluminescence immunoassay, and TPO-Ab was measured by electrochemiluminescence immunoassay.
A normal range of TPO-Ab (+) was defined as below 16 IU/mL.[10] Maximum values for the left and right common carotid arteries of the CIMT were calculated with an semiautomated digital edge-detection software (Intimascope; MediaCross, Tokyo, Japan) following a protocol that has been described in detail elsewhere.[11] The higher values of the right and left CIMT not including plaque measurements were then calculated, and the maximum CIMT value was then used for analysis. Since a previous study reported the normal CIMT value as <1.1 mm, we defined atherosclerosis as CIMT ≥ 1.1 mm.[12]
2.3. Statistical analysis
Characteristics of the study population were expressed as mean ± standard deviation except for preference history (current smoker and daily drinker), TPO-Ab, and TSH. The preference history was expressed as a percent value. Since TPO-Ab and TSH showed a skewed distribution, the characteristics of this study population were expressed as median (the first quartile, the third quartile), followed by logarithmic transformation. The differences among potential variables regarding atherosclerosis status were calculated. Differences between the mean values or proportional values of the monitored characteristics were analyzed in relation to atherosclerosis. Significant differences were evaluated using Student t-test for continuous variables and the χ2 test for proportional data.
Logistic regression models were used to calculate odds ratios (ORs) and 95% confidence intervals (CIs) to determine the association between TPO-Ab and atherosclerosis. Three adjustment models were used. The first model (model 1) was adjusted only for sex and age; the second model (model 2) further included the potential confounding factors that were directly associated with thyroid function, namely, TSH (μIU/mL) and free T3 (pg/mL). The last model (model 3) was further adjusted for potential confounding factors that were indirectly associated with thyroid function, such as BMI (kg/m2), systolic blood pressure (mm Hg), smoking status (current, former, and never), drinking status (daily, often, and non), TG (mg/dL), HDLc (mg/dL), and HbA1c (%). We also made an analysis limited to subjects within a normal range of TSH to avoid the influence of subclinical hypothyroidism. Furthermore, for sensitivity analysis, we made a sex-specific analysis.
All statistical analyses were performed with the SAS system for Windows (version 9.4: SAS Inc, Cary, NC). Values of P < 0.05 were regarded as statistically significant.
3. Results
3.1. Characteristics of the study population with atherosclerosis
In this study, 1165 subjects with a mean age of 60.6 years (standard deviation, 9.1; range 40–74) were enrolled.
Among the study population, 115 were diagnosed as having atherosclerosis.
The characteristics of the study population by atherosclerosis status are shown in Table 1.
Table 1.
Characteristics of the study population.
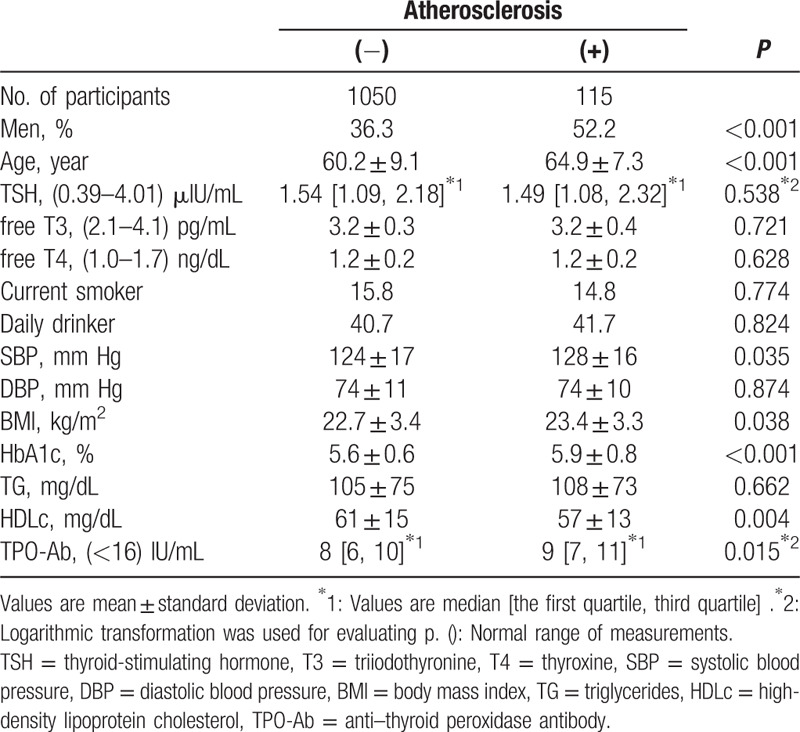
Compared to subjects without atherosclerosis, those with atherosclerosis show a higher prevalence in men and higher values of age, systolic blood pressure, BMI, HbA1c, and TPO-Ab while lower value of HDLc.
3.2. Atherosclerosis in relation to anti–thyroid peroxidase (TPO-Ab)
Independent from thyroid function and known cardiovascular risk factors, among the eu-thyroid population, a normal range of TPO-Ab revealed to be positively associated with atherosclerosis (Table 2). The ORs and 95% CIs of atherosclerosis for logarithmic values of TPO-Ab are 2.19 (1.11, 4.33) for model 1, 2.18 (1.10, 4.32) for model 2, and 2.23 (1.11, 4.47) for model 3.
Table 2.
ORs and 95% CIs for atherosclerosis in relation to TPO-Ab among the eu-thyroid population.
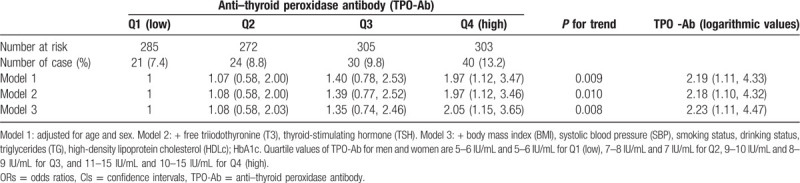
For sensitivity, our analysis was sex-specific. Among men, although no significant association was observed, there was a positive tendency between TSH and atherosclerosis. In women, a significant positive association between TSH and atherosclerosis was observed. The fully adjusted ORs and 95% CIs of atherosclerosis for logarithmic values of TPO-Ab were 1.62 (0.59, 4.48) for men and 2.88 (1.09, 7.57) for women, respectively.
3.3. Atherosclerosis in relation to anti–thyroid peroxidase (TPO-Ab) limited to subjects within the normal range of thyroid-stimulating hormone (TSH)
When we limited analyses to subjects within the normal range of TSH, the positive association between TPO-Ab (logarithmic values) and atherosclerosis became slightly stronger (Table 3). The corresponding values were 2.60 (1.27, 5.34) for model 1, 2.58 (1.26, 5.30) for model 2, and 2.65 (1.27, 5.51) for model 3.
Table 3.
ORs and 95% CIs for atherosclerosis in relation to TPO-Ab among the eu-thyroid population limited to a normal range of TSH.
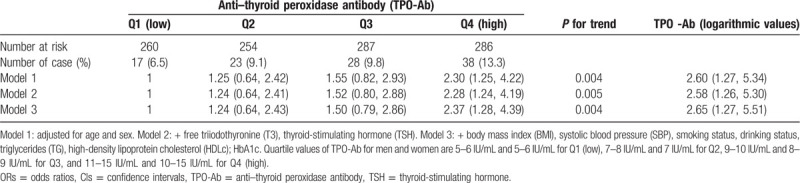
For sensitivity analysis, we also made sex-specific analysis among subjects within the normal range of TSH. Similar associations were observed for both men and women. In women, a significant positive association between TSH and atherosclerosis was observed. The fully adjusted ORs and 95% CIs of atherosclerosis for logarithmic values of TPO-Ab were 1.84 (0.63, 5.38) for men and 3.57 (1.31, 9.73) for women, respectively.
4. Discussion
The major findings of the present study in the eu-thyroid general population are that, independent of known confounding factors, a normal range of TPO-Ab titer is significantly positively associated with atherosclerosis. And this positive association became slightly stronger when the analysis is limited to participants with a normal range of TSH.
TPO-Ab is one of the known factors that cause an autoimmune thyroid disease that results in hypothyroidism. Since hypothyroidism is reported to be associated with atherosclerosis progression,[13] levels of TPO-Ab titer could be positively associated with atherosclerosis by indicating a low level of thyroid function. Moreover, a previous cross-sectional study reported that not only subjects with overt hypothyroidism but also subclinical hypothyroidism showed significantly higher CIMT than normal control subjects.[7] Therefore, subclinical hypothyroidism, which is associated with TPO-Ab, could be associated with atherosclerosis, as increased CIMT which is an established risk factor for cardiovascular disease.[14] Even so, a previous cross-sectional study of subclinical hypothyroidism reported that the presence of TPO-Ab does not appear to correlate with cardiovascular disease.[15] These studies indicate that the presence of low levels of thyroid function, rather than the presence of TPO-Ab, could be associated with atherosclerosis.
However, in the present study, we found a significant positive association between a normal range of TPO-Ab titer and atherosclerosis among the eu-thyroid population.
Hashimoto disease is one of the known major autoimmune thyroid diseases. Endothelial dysfunction, which is evaluated by flow-mediated arterial dilation, is observed among eu-thyroid patients with Hashimoto's thyroiditis.[16] TPO-Ab is found to be a significant factor associated with endothelium-dependent arterial dilation.[16] Therefore, even if the thyroid hormones are within the normal range, having TPO-Ab-positive endothelium might be a disadvantage.
In the present study, we found further evidence that even with a normal range of TPO-Ab titer (TPO-Ab negative), the TPO-Ab titer is positively associated with atherosclerosis among the eu-thyroid general population with a normal TSH range. This finding indicates that the atherosclerosis risk for higher values of TPO-Ab within the normal range is not caused by thyroid function abnormality.
A previous study indicated that thyroid peroxidase induced the release of proinflammatory cytokines such as tumor necrosis factor alpha (TNF-α) and interferon-γ (IFN-γ) from phagocytic cells and T-cell responses to thyroid peroxidase are promoted by TPO-Ab.[4] Since TNF-α and IFN-γ are known contributing factors for the progress of atherosclerosis,[5,6] low-grade inflammation might determine the positive association between TPO-Ab and atherosclerosis.
Clinical implication for present study is that, even with a normal TPO-Ab titer range, participants with higher TPO-Ab could possess a higher risk of atherosclerosis progression possibly by indicating low-grade inflammation. Furthermore, participants with atherosclerosis could have higher TPO-Ab even among eu-thyroid populations.
4.1. Limitations
Potential limitations of the present study warrant consideration. Even though low-grade inflammation may have influenced our results, we could not evaluate the degrees of inflammation. Further epidemiological investigations using data of pro-inflammatory cytokines such as those related to TNF-α and IFN-γ are thus needed. Additionally, since this was a cross-sectional study, we could not establish any causal relationships.
4.2. Future directions
To clarify the causality of the association between normal range of TPO-Ab and atherosclerosis, longitude studies are need to be conducted.
5. Conclusion
In conclusion, a normal TPO-Ab range was found to be significantly positively associated with atherosclerosis in eu-thyroid participants and in those participants with normal TSH range. These findings are considered to be valuable for clarifying the association of a normal TPO-Ab range with the presence of atherosclerosis.
Acknowledgments
We are grateful to Ms. Keiko Yamaoka, Ms. Kaori Yamamura, and staff from Saza town office for their outstanding support.
Author contributions
Conceptualization: Yuji Shimizu, Naomi Hayashida.
Data curation: Yuji Shimizu, Yuko Nabeshima-Kimura, Shin-Ya Kawashiri, Yuko Noguchi, Yasuhiro Nagata, Takahiro Maeda, Naomi Hayashida.
Formal analysis: Yuji Shimizu, Yuko Nabeshima-Kimura, Yuko Noguchi, Naomi Hayashida.
Investigation: Yuji Shimizu, Yuko Nabeshima-Kimura, Shin-Ya Kawashiri, Yuko Noguchi, Yasuhiro Nagata, Takahiro Maeda, Naomi Hayashida.
Methodology: Yuji Shimizu, Yuko Nabeshima-Kimura, Yuko Noguchi, Naomi Hayashida.
Project administration: Yuji Shimizu, Takahiro Maeda, Naomi Hayashida.
Supervision: Yuji Shimizu, Takahiro Maeda, Naomi Hayashida.
Writing – original draft: Yuji Shimizu
Glossary
Abbreviations: BMI = body mass index, CIMT = carotid intima-media thickness, CIs = confidence intervals, HDLc = high-density lipoprotein cholesterol, IFN-γ = interferon-γ, OR = odds ratios, SBP = systolic blood pressure, T3 = triiodothyronine, T4 = thyroxine, TG = triglycerides, TNF-α = tumor necrosis factor alpha, TPO-Ab = anti–thyroid peroxidase antibody, TSH = thyroid-stimulating hormone.
References
- [1].Carlê A, Laurberg P, Knudsen N, et al. Thyroid peroxidase and thyroglobulin auto-antibodies in patients with newly diagnosed overt hypothyroidism. Autoimmunity 2006;39:497–503.. [DOI] [PubMed] [Google Scholar]
- [2].Nielsen CH, Leslie RG, Jepsen BS, et al. Natural autoantibodies and complement promote the uptake of a self antigen, human thyroglobulin, by B cells and the proliferation of thyroglobulin-reactive CD4(+) T cells in healthy individuals. Eur J Immunol 2001;31:2660–8.. [DOI] [PubMed] [Google Scholar]
- [3].Jensen EA, Peterson PH, Blaabjerg O, et al. Establishment of reference distributions and decision values for thyroid antibodies against thyroid peroxidase (TPOAb), thyroglobulin (TgAb) and the thyrotropin receptor (TRAb). Clin Chem Lab Med 2006;44:991–8.. [DOI] [PubMed] [Google Scholar]
- [4].Nielsen CH, Brix TH, Leslie RG, et al. A role for autoantibodies in enhancement of pro-inflammatory cytokine responses to a self-antigen, thyroid peroxidase. Clin Immunol 2009;133:218–27.. [DOI] [PubMed] [Google Scholar]
- [5].Urschel K, Cicha I. TNF-α in the cardiovascular system: from physiology to therapy. International Journal of Interferon, Cytokine and Mediator Research 2015;7:9–25.. [Google Scholar]
- [6].Voloshyna I, Littlefield MJ, Reiss AB. Atherosclerosis and interferon-γ: new insights and therapeutic targets. Trends Cardiovasc Med 2014;24:45–51.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Saif A, Mousa S, Assem M, et al. Endothelial dysfunction and the risk of atherosclerosis in overt and subclinical hypothyroidism. Endocr Connect 2018;7:1075–80.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Shimizu Y, Nabeshima-Kimura Y, Kawashiri SY, et al. Anti-thyroid peroxidase antibody and thyroid cysts among the general Japanese population: a cross-sectional study. Environ Health Prev Med 2020;25:7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9]. Home page on SRL. Comprehensive inspection information (in Japanese). Available at: http://test-guide.srl.info/hachioji/ [access date August 13, 2020] [Google Scholar]
- [10].LSI Medience Corporation Information. Rinsyokensa Jugyo. 2017; 17-04. (in Japanese). Available at: https://www.medience.co.jp/information/pdf/17-04.pdf [access date August 13, 2020]. [Google Scholar]
- [11].Hara T, Takamura N, Akashi S, et al. Evaluation of clinical markers of atherosclerosis in young and elderly Japanese adults. Clin Chem Lab Med 2006;44:824–9.. [DOI] [PubMed] [Google Scholar]
- [12].Kawamori R, Yamasaki Y, Matsushima H, et al. Prevalence of carotid atherosclerosis in diabetic patients. Ultrasound high-resolution B-mode imaging on carotid arteries. Diabetes Care 1992;15:1290–4.. [DOI] [PubMed] [Google Scholar]
- [13].Ichiki T. Thyroid hormone and vascular remodeling. J Atheroscler Thromb 2016;23:266–75.. [DOI] [PubMed] [Google Scholar]
- [14].van den Oord SC, Sijbrands EJ, ten Kate GL, et al. Carotid intima-media thickness for cardiovascular risk assessment: systematic review and meta-analysis. Atherosclerosis 2013;228:1–1.. [DOI] [PubMed] [Google Scholar]
- [15].Wells BJ, Hueston WJ. Are thyroid peroxidase antibodies associated with cardiovascular disease risk in patients with subclinical hypothyroidism? Clin Endocrinol (Oxf) 2005;62:580–4.. [DOI] [PubMed] [Google Scholar]
- [16].Xiang GD, He YS, Zhao LS, et al. Impairment of endothelium-dependent arterial dilation in Hashimoto's thyroiditis patients with euthyroidism. Clin Endocrinol (Oxf) 2006;64:698–702.. [DOI] [PubMed] [Google Scholar]


