Abstract
The aim of this study was to compare the success of first-attempt tracheal intubation in pediatric patients >1-year old performed using video versus direct laryngoscopy and compare the frequency of tracheal intubation–associated events and desaturation among these patients.
Prospective observational cohort study conducted in an Academic pediatric tertiary emergency department. We compared 50 children intubated with Mcgrath Mac video laryngoscope (VL group) and an historical series of 141 children intubated with direct laryngoscopy (DL group). All patients were aged 1 to 18 years.
The first attempt success rates were 68% (34/50) and 37.6% (53/141) in the VL and DL groups (P < .01), respectively. There was a lower proportion of tracheal intubation–associated events in the VL group (VL, 31.3% [15/50] vs DL, 67.8% [97/141]; P < .01) and no significant differences in desaturation (VL, 35% [14/50] vs DL 51.8% [72/141]; P = .06). The median number of attempts was 1 (range, 1–5) for the VL group and 2 (range, 1–8) for the DL group (P < .01). Multivariate logistic regression showed that video laryngoscope use was associated with higher chances of first-attempt intubation with an odds ratio of 4.5 (95% confidence interval, 1.9–10.4, P < 0.01).
Compared with direct laryngoscopy, VL was associated with higher success rates of first-attempt tracheal intubations and lower rates of tracheal intubation–associated events.
Keywords: emergency medicine, laryngoscope, laryngoscopy, pediatrics, tracheal intubation
1. Introduction
Tracheal intubation remains a key skill in pediatric emergencies. However, it is less frequently required and technically more difficult to perform in children than in adults.[1] Since the invention of the laryngoscope in 1895, the preferred method for intubation has been direct laryngoscopy (DL).[2] Pediatric intubation is a safe procedure in the hands of experienced providers and in controlled situations such as anesthesia for elective surgery, with first-attempt intubation successful in almost all cases, and few episodes of tracheal intubation–associated events. In a retrospective study comprising 1070 children aged 3 to 12 years intubated with rapid sequence intubation for elective anesthetic procedures, the first-attempt intubation success rate was 98.3% (1042/1070).[3]
Tracheal intubation performed outside the operating room may not be as safe as intubations performed inside the operating room. A review of an intubation registry that included 15 pediatric intensive care units included 1715 intubations with the first-attempt intubation success observed in 1066 cases (62.2%); tracheal intubation–associated events were observed in 20% of the intubations, including severe events in 6%.[4] Although pediatric intensive care intubations are a relative proxy to pediatric emergency department intubations, tracheal intubation is considered a significantly risky procedure due to the following reasons: presence of severe illness or injury, patient's insufficient fasting, and the relative inexperience of the providers performing the intubations.[1] Upon reviewing the national intubation registry of 17 pediatric emergency departments in Japan, Goto et al found that 293 intubations in children aged <18 years during a 4-year period had a first-attempt intubation success rate of 60%.[5] Similar studies in Australia, the United States, and Korea have shown first-attempt intubation success rates of 52% to 78%.[5–8] At the Instituto da Criança in Brazil, Sukys et al reviewed a registry of 94 patients intubated in the emergency department using rapid sequence intubation and found that only 37 tracheal intubations were successful in the first attempt (39%). This lower rate can be explained in part by the hospital patient population, with no trauma patients and 78% of children with underlying diseases, most of them severe, and also by the relative inexperience of professionals attempting intubation, most of them second-year residents.[9]
In the last decade, video laryngoscopy (VL) was considered as an alternative to DL. The video laryngoscope allows the indirect visualization of the glottis using a camera on the blade that provides a better view of the patient's airway on a video screen, also allowing better ability to coach trainees to improve their performance in intubation.[10] Its use has been progressively increasing in the pediatric intensive care units.
In a review of the intubation registries of 36 pediatric intensive care units between 2010 and 2015, a total of 8875 intubations were performed, 7947 (89.5%) with DL and 928 (10.5%) with VL. The odds ratio (OR) of video laryngoscope rate of use between 2011 and 2015 was 11.2 (95% confidence interval [CI], 3.2–38.9). The same study showed fewer tracheal intubation associated events with VL (adjusted OR, 0.57; 95% CI, 0.42–0.77; P < .001).[11]
There is a paucity of data regarding video laryngoscope use in the pediatric emergency department. Einsenberg et al reviewed a registry of 452 pediatric tracheal intubation procedures: 199 with VL (first-attempt intubation success rate, 72%) and 240 with DL (first-attempt intubation success rate, 71%) with no differences observed. The laryngoscopist initially attempted a direct visualization of the glottis using a C-MAC video laryngoscope (Karl Storz, Germany), whereas the video screen was used by a supervisor for real-time guidance.[12] Similarly, Kerrey et al used the C-MAC video laryngoscope as the first device for pediatric intubation with providers performing intubation with DL and a “copilot” attending physician watching the video screen. This strategy reached a first-attempt intubation success rate of 64% on a filmed intubation review.[13]
In 2015, the Emergency Department of the Instituto da Criança acquired a video laryngoscope (McGrath Mac Enhanced Direct Laryngoscope; Medtronic, United Kingdom).[14] This equipment was initially used for rescue tracheal intubation attempts for children aged >1 year.[15] Since the study conducted at this institution showed that there was room for improvement in terms of intubation success at this emergency department,[9] VL was introduced as the first option for intubation in children aged >1 year, and its use was assessed prospectively. Considering that the previous studies deemed VL as safe with expected clinical benefits, it was believed that it would be unethical to withhold VL from these patients; hence, a nonrandomized design was used.
1.1. Objectives
We hypothesized that video laryngoscope use would increase the first-attempt intubation success rate and decrease the episodes of desaturation and tracheal intubation associated events.
The primary objective was to compare the first-attempt intubation success rates of VL and DL. The secondary objectives were to compare the episodes of desaturation and tracheal intubation associated events between patients intubated using either method and to assess the safety of VL as the first choice for intubation of children aged >1 year.
2. Materials and methods
This was a prospective observational cohort study.
2.1. Participants and Setting
We prospectively recorded a total of 116 cases of intubations performed over a 23-month period (July 2016–May 2018). We also assessed the 5-year data of our local intubation registry, where a total of 248 registrations of intubated patients were recorded. We included all registered intubated patients aged older than 1 year but younger than 19 years. The exclusion criteria were as follows: patient's age was not within the established age limit, intubation method used was neither VL nor DL, patient's caregivers refused to provide informed consent, or a registration form was inadequately filled with insufficient information about patient's age or intubation method.
The study was conducted at the Emergency Department of the Instituto da Criança do Hospital das Clinicas da Faculdade de Medicina da Universidade de São Paulo in Brazil. This is an academically exclusive pediatric tertiary service that does not serve trauma patients.
Several months before the study, training measures were undertaken to prepare the interprofessional team including performing lectures, task training for physicians and fellows regarding the proper use of the video laryngoscope (McGrath Mac), and performing in situ simulations. All staff thus was familiar with video laryngoscope and trained in it to use as a rescue device. Starting in July 2016, the care teams were advised that all tracheal intubation procedures in children aged >1 year should be performed preferably with VL, where both professional intubating and supervisor looking at the screen. A number 1 blade was not available in the device used; hence, intubation in patients aged <1 year remained to be with DL. All intubations were registered immediately after the procedure.
Tracheal intubations at Instituto da Criança are performed with the presence of an attending physician who is the team leader and supervises the procedure, and a team is composed of a pediatric emergency fellow or a third-year resident of pediatrics, a second-year resident of pediatrics, a nurse, and a respiratory therapist. Rapid sequence intubation is used following a standard checklist unless there is a clear contraindication.[9] Historically, second-year pediatric residents at this institution perform tracheal intubation. In case of failure, the procedure is performed by the third-year resident, fellow, or attending physician, if deemed necessary. In case of a difficult airway, anesthesia attending physicians are required for assistance.
All second-year residents are pediatric advanced life support-certified individuals and have undergone task training for intubation at the skill's laboratory during their emergency department rotation. They also participate regularly in simulations at the simulation center and in situ, all of which include airway management. However, different from fellows and attending physicians, the second-year residents were not familiar with VL before the study and did not practice intubation at operating room rotation. As a new practice after the introduction of VL, at the beginning of their rotation, residents were trained at the emergency department using a mastery learning approach.[16] Residents practiced with the device using a task trainer guided by an attending physician and were subsequently assessed using an intubation checklist elaborated by the authors. They were only allowed to intubate if they achieved mastery on this test (≥90% correct items in the checklist). If required, they were retrained until they mastered the procedure.
2.2. Outcomes
The primary outcome was the first-attempt intubation success rate. The secondary outcomes were the presence of desaturation defined as an oxygen saturation <80% during tracheal intubation in children with an initial oxygen saturation >90% after preoxygenation[17] and presence of tracheal intubation associated events. Based on several intubation studies, severe tracheal intubation–associated events included cardiac arrest, esophageal intubation with delayed recognition, emesis with aspiration, hypotension requiring intervention, laryngospasm, pneumothorax, pneumomediastinum, and direct airway injury. Nonsevere tracheal intubation–associated events included mainstream bronchial intubation, esophageal intubation with immediate recognition, emesis without aspiration, hypertension requiring therapy, epistaxis, dental or lip trauma, medication error, arrhythmia, and pain or agitation requiring additional medication or causing delay in intubation.[4]
2.3. Sample size
Two studies were used to estimate the sample size. Sukys et al showed a first-attempt intubation success rate of 39% (37/94) at the Emergency Department of the Instituto da Criança. Since the intubation process remained the same from this publication to immediately before the study, this was considered the basal intubation rate.[9] Kerrey et al's study, which reported a 64% (48/75) first-attempt intubation success rate using VL, was used to estimate the possible effect of this intervention, which was an increment of 25% from the first-attempt intubation success rate (64%–39%).[12] Considering a statistical power of 80%, significance of 95%, 2-tailed t test, and 94 cases in the first group, the 46 cases in the study group should demonstrate a 25% increase in the first-attempt intubation success rate.
2.4. Statistical methods
The data were treated according to the outcomes of the variables. For the continuous variables, the evaluation was performed using means (standard deviations) if the distribution was normal or using medians (variation or interquartile range) if the distribution was not normal. For the categorical variables, the evaluation was in percentage values. Missing or incomplete data were excluded from database.
Means or medians were compared using the Student t test or the Mann-Whitney U/Kruskal-Wallis test as appropriate. Categorical variables were compared using the χ2 test or Fisher exact test. Logistic regression models were performed to identify the independent variables associated with the first-attempt intubation success rate. In the multivariate analysis, we used as independent variables those that presented a level 20% of significance in the univariate analysis (VL, desaturation, second-year resident as professional intubating). All data were analyzed using the Statistical Package for the Social Sciences version 22.0. P values <.05 were considered statistically significant.
2.5. Ethics
Considering that intubation techniques are similar and VL was already used in the treatment for difficult airways before the study, the choice of recommending the VL as the first device was considered as a quality improvement initiative. Hence, consent was not required before intubation but was obtained for registration in this study. The Hospital das Clinicas da Faculdade de Medicina ethics review board approved this study (CAAE: 56983516.7.0000.0068).
3. Results
3.1. Participants
Fifty patients aged >1 year were intubated using VL during the study (the VL group), whereas a total of 141 patients were intubated using the DL group during the 5-year historical control. Cohort started on July 2016 and ended on May 2018 when the goal of intubating 46 patients using VL as first method programmed for analysis was achieved. Twenty-five patients in the prospective observational period were intubated with DL.
Of the 79 residents eligible to intubate, 59 different second-year residents attempted intubation in patients older than 1 year. Although the use of VL was recommended for tracheal intubation in patients aged >1 year, the attending physician made the final decision and sometimes chose DL. This occurred more frequently at the beginning of the observation, with increasing adherence to VL in the end. In the first 6 months, the proportions of direct and VL were 62.5% and 37.5%, respectively. In the last 6 months, the proportions of direct and VL were 18.2% and 81.8%, respectively.
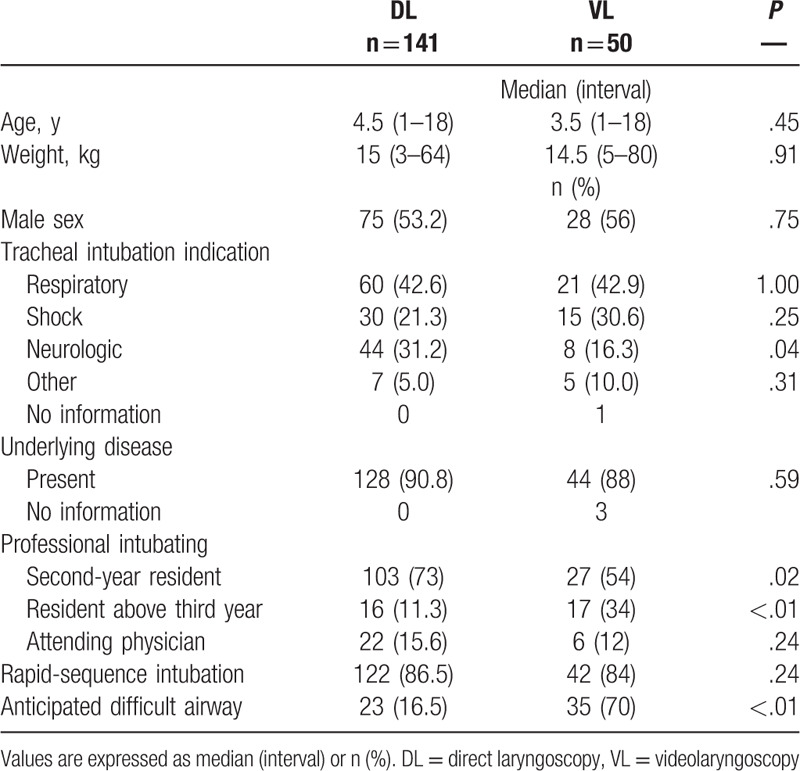
3.2. Baseline data
The baseline demographic data are summarized in Table 1. Both groups showed no significant difference in age, weight, sex, or indication for intubation due to respiratory disease or shock, underlying illness, or use of rapid-sequence intubation. Significant differences were observed in the following: indication for intubation due to neurological diseases more often observed in the DL group than in the VL group, a higher proportion of second-year residents intubating in the DL group than in the VL group, and a higher incidence of anticipated difficult airway in the VL group than in the DL group.
Table 1.
Baseline data.
3.3. Outcomes
Table 2 summarizes the main results. There was a significant difference in the first-attempt intubation success rate between the 2 groups, favoring the VL group. No differences were observed in tracheal intubation success rate with up to 3 attempts. A statistically significant difference was observed in the proportion of tracheal intubation associated events between the 2 groups, but not desaturation. The median number of attempts was 1 (1–5) in the VL group and 2 (1–8) in the DL group (P < .01, Kruskal-Wallis test).
Table 2.
Comparison of direct laryngoscopy and videolaryngoscopy groups.
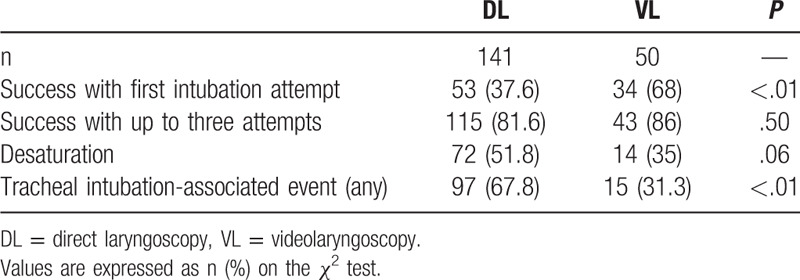
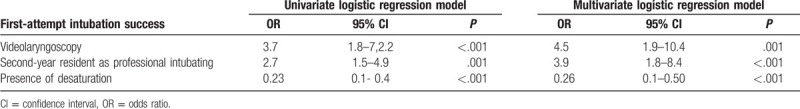
Table 3 summarizes the results of the multivariate logistic regression analysis. Considering all cases, we observed a positive association between tracheal intubation in the first attempt and VL (OR = 4.5; 95% CI, 1.8–7.0; P < .01) and second-year residents (OR = 3.9; 95% CI, 1.8–8.4; P < .01), whereas the presence of desaturation was presented as a reduced OR for first-attempt intubation (OR = 0.26; 95% CI, 0.1–0.50; P < .01).
Table 3.
Association between variables and first-attempt intubation success in univariate and multivariate logistic regression models.
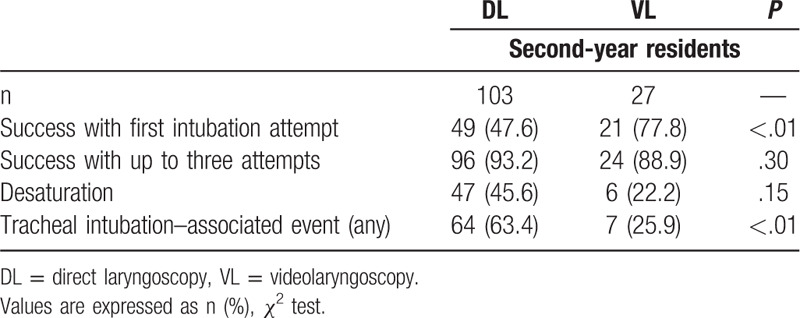
Considering that only second-year residents were trained with the mastery learning approach and that they were usually the first ones to attempt intubation, an analysis was performed to separate these specific groups (DL—second-year residents vs VL—second-year residents). The results of this ancillary analysis are summarized in Table 4 and are similar to the main population.
Table 4.
Comparison of direct laryngoscopy and videolaryngoscopy groups (second-year residents).
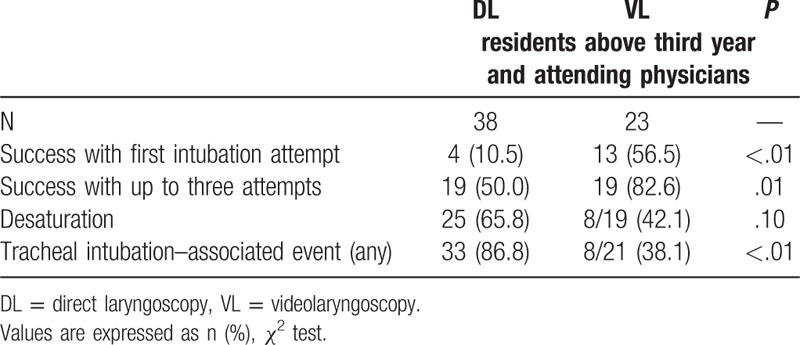
Analysis was also performed with the more experienced providers, who practiced VL with the task trainers but did not receive the mastery learning training (VL non- second-year residents and DL non- second-year residents). The results of this analysis are summarized in Table 5. Results are consistent with the main population, but in this group, there was a difference in the tracheal intubation success rate with up to 3 attempts between the 2 groups. The fact that the first-attempt intubation success rate is lower in this population most likely reflects the fact that the most experienced providers are the first to manage difficult airway in this hospital only in cases of anticipated airway difficulties or in the absence of second-year residents, which seldomly occurs.
Table 5.
Comparison of direct laryngoscopy and videolaryngoscopy groups (residents above third year and attending physicians).
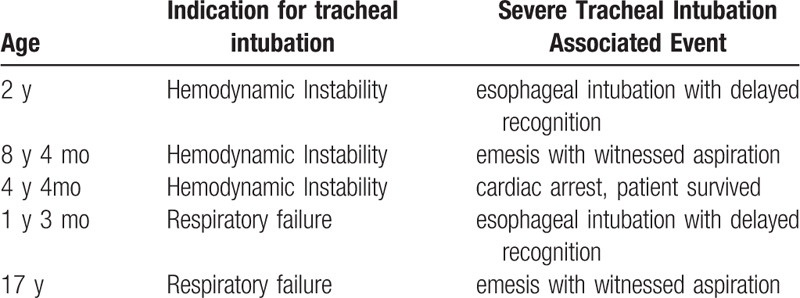
Of the 15 tracheal intubation associated events registered in the VL group, 5 were classified as severe. Table 6 details these events.
Table 6.
Severe tracheal intubation associated events.
4. Discussion
In this study, a 68% first-attempt intubation success rate using VL suggests an 80% improvement in success rate, which is higher compared to that of the historical series. This result is consistent with that of the study by Kerrey et al,[13] who also used VL in a pediatric emergency department and reported a 64% first-attempt intubation success rate. Additionally, this rate is close to and sometimes exceeds to the rates of several pediatric emergency departments worldwide with a range of 52% to 78%[5–8] and from the database of 15 pediatric intensive care units with a 62.2% first-attempt intubation success rate.[4] Furthermore, this rate suggests an improved intubation success with the use of VL at the Instituto da Criança.
Differences in the success rate of intubation with up to 3 attempts were not observed. The 86% rate is similar to that of the previous study at the same emergency department, which reported an 87% success rate with DL in up to 3 attempts.[9] Other studies reported success with up to 2 attempts. Kerrey et al reported a total of 90.7% of patients intubated with up to 2 attempts using VL.[13] In a multicenter registry of pediatric intensive care units, Lee et al reported an 84% success rate with up to 2 attempts using mostly DL.[18]
Significantly lower tracheal intubation–associated events in the study were observed compared with the events in the historical series. Although it is not possible to attribute this finding to the use of VL alone considering that differences were observed in patient population and laryngoscopists in the 2 groups, it certainly played a crucial role since the physical structure, rapid sequence intubation protocol, and health care staff did not change significantly during this period. However, it is important to note that even the proportion observed after the intervention (31.1%) is higher compared to the proportion observed in the registry of the 15 pediatric intensive care units in the United States, which has a 20% tracheal intubation associated events rate. Although intensive care intubations are not directly comparable, these rates suggest that there is still room for improvement in intubation safety in the emergency department.
There were no statistically significant differences between the 2 groups in desaturation. The 35% to 52% desaturation rate is high. In a study evaluating 2080 intubations for respiratory failure, the desaturation rate was 16.2% with 1 intubation attempt and 56% with ≥3 intubation attempts.[18] Considering the association between hypoxemia and tracheal intubation associated events,[17] the high desaturation rate partly explains the high proportion of tracheal intubation associated events.
Since second-year residents had more intensive training with VL compared to the other residents and fellows, it is possible that part of their superior performance was due to the training rather than the introduction of VL. However, an increase in the success rate was observed for patients intubated by more experienced professionals as well, which suggests a benefit in performance not related to training. Although this analysis was performed based on experience, the statistical design of the study was not powered to detect a significant difference between subgroups. It is important to note that there was a shift in tracheal intubation from second-year residents to more experienced professionals in the prospective phase which could have influenced the results to be more in favor of the VL group. This seems to be a universal tendency, with a higher proportion of intubations performed by fellows from pediatric intensive care units in the United States over the past decade.[19]
An added benefit of using VL was the increased team situational awareness acquired by having a shared view of the airway visualization using the video laryngoscope, increasing the physician's confidence in supervising the resident's performance. This benefit was already noted in other pediatric studies using VL[13] and is probably beneficial in discussing the increased acceptance of VL over time. Optimizing intubation conditions by training, processes, or equipment is specifically important considering the low frequency and high acuity of intubations in the emergency department[21] considering that in this study sample, not all second-year residents were exposed to emergency department intubations.
This study has the following limitations. First, it was conducted in a single center. Because this is a specialized service with a population distinct from other hospitals due to the absence of trauma patients and the high proportion of children with comorbidities and an anticipated difficult airway, results should be interpreted with caution. However, the results may be beneficial for pediatric tertiary academic hospitals, which care for children with acute illness and chronic health conditions. Second, the wide age range of the study population makes the real clinical benefit of VL harder to assess. The fact that intubations of patients aged <1 year were excluded in this study is a potential confounder as this is the population most vulnerable to intubation challenges. Of note, during the study, 58 patients aged <1 year were intubated in the emergency department using DL, with only 16 successful intubations in the first attempt (27.5%), which shows a potential clinical benefit of VL in this age group. The higher proportion of anticipated difficult airway in the VL group was most likely an over-estimation related to the excessive emphasis on difficult airway assessment during resident training, rather than from population heterogeneity. Although this fact could lead to a possible selection bias, results show that the main determinant of adherence to recommendation of using VL in all intubations was time, with progressive acceptance of VL regardless of difficult airway status. The high proportion of anticipated difficult airway favors VL because a video laryngoscope is a rescue device recommended for use in cases of difficult airway.[20]
Considering the heterogeneity of devices available on the market, it is important to highlight that the results obtained with the McGrath Mac may not be necessarily applicable to other equipment because tracheal intubation technique may vary depending on the device. Third, this study used an observational design. Success might have been altered by factors other than VL, although the significant differences observed make this unlikely. Considering the relative rarity of tracheal intubations in the pediatric emergency department, a single-center randomized study would be challenging. Furthermore, considering the team's perception of the advantages of VL, it was ethically complex to restrict its use. Finally, the use of intubation recording as a data collection tool is a limitation because registered outcomes are often more favorable than other outcomes, such as reviews of patient films or parameters measured using a multiparametric monitor.[8] Nevertheless, considering the insufficient studies in this specific population, results are relevant to the current knowledge of the subject and may justify future multicenter randomized studies.
In conclusion, a higher first-attempt intubation success rate was obtained with VL compared to DL in an academic pediatric tertiary emergency depatment. Additionally, the tracheal intubation associated event rate was lower in VL than in DL. This effect was consistent regardless of the professional experience. These results suggest that VL may be considered as a safe first choice for the intubation of pediatric patients in the emergency department.
Author contributions
TC, AR and CS designed the study. VC trained residentes with videolaryngoscopy, and collected data. SF planned and carried out statistical analysis. TC wrote manuscript. All authors revised and approved final manuscript.
Glossary
Abbreviations: CI = confidence interval, DL = direct laryngoscopy, OR = odds ratio, VL = videolaryngoscopy.
References
- [1].Mittiga MR, Geis GL, Kerrey BT, et al. The spectrum and frequency of critical procedures performed in a pediatric emergency department: implications of a provider-level view. Ann Emerg Med 2013;61:263–70.. [DOI] [PubMed] [Google Scholar]
- [2].Hirsch NP, Smith GB, Hirsch PO. Alfred Kirstein. Pioneer of direct laryngoscopy. Anaesthesia 1986;41:42–5.. [DOI] [PubMed] [Google Scholar]
- [3].Gencorelli FJ, Fields RG, Litman RS. Complications during rapid sequence induction of general anesthesia in children: a benchmark study. Paediatr Anaesth 2010;20:421–4.. [DOI] [PubMed] [Google Scholar]
- [4].Nishisaki A, Turner DA, Brown CA, et al. A National Emergency Airway Registry for children: landscape of tracheal intubation in 15 PICUs. Crit Care Med 2013;41:874–85.. [DOI] [PubMed] [Google Scholar]
- [5].Goto T, Gibo K, Hagiwara Y, et al. Factors associated with first-pass success in pediatric intubation in the emergency department. West J Emerg Med 2016;17:129–34.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Choi HJ, Je SM, Kim JH, et al. The factors associated with successful paediatric endotracheal intubation on the first attempt in emergency departments: a 13-emergency-department registry study. Resuscitation 2012;83:1363–8.. [DOI] [PubMed] [Google Scholar]
- [7].Long E, Sabato S, Babl FE. Endotracheal intubation in the pediatric emergency department. Paediatr Anaesth 2014;24:1204–11.. [DOI] [PubMed] [Google Scholar]
- [8].Kerrey BT, Rinderknecht AS, Geis GL, et al. Rapid sequence intubation for pediatric emergency patients: higher frequency of failed attempts and adverse effects found by video review. Ann Emerg Med 2012;60:251–9.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Sukys GA, Schvartsman C, Reis AG. Evaluation of rapid sequence intubation in the pediatric emergency department. J Pediatr (Rio J) 2011;87:343–9.. [DOI] [PubMed] [Google Scholar]
- [10].Pouppirt NR, Foglia EE, Ades A. A video is worth a thousand words: innovative uses of videolaryngoscopy. Arch Dis Child Fetal Neonatal Ed 2018;103:F401–2.. [DOI] [PubMed] [Google Scholar]
- [11].Grunwell JR, Kamat PP, Miksa M, et al. Trend and outcomes of video laryngoscope use across PICUs. Pediatr Crit Care Med 2017;18:741–9.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Eisenberg MA, Green-Hopkins I, Werner H, et al. Comparison between direct and video-assisted laryngoscopy for intubations in a pediatric emergency department. Acad Emerg Med 2016;23:870–7.. [DOI] [PubMed] [Google Scholar]
- [13].Kerrey BT, Mittiga MR, Rinderknecht AS, et al. Reducing the incidence of oxyhaemoglobin desaturation during rapid sequence intubation in a paediatric emergency department. BMJ Qual Saf 2015;24:709. [DOI] [PubMed] [Google Scholar]
- [14].Giraudon A, Bordes-Demolis M, Blondeau B, et al. Comparison of the McGrath® MAC video laryngoscope with direct Macintosh laryngoscopy for novice laryngoscopists in children without difficult intubation: a randomised controlled trial. Anaesth Crit Care Pain Med 2017;36:261–5.. [DOI] [PubMed] [Google Scholar]
- [15].Ross M, Baxter A. Use of the new McGrath® MAC size-1 paediatric videolaryngoscope. Anaesthesia 2015;70:1217–8.. [DOI] [PubMed] [Google Scholar]
- [16].McGaghie William C, Issenberg Saul B, Barsuk Jeffrey H, et al. A critical review of simulation-based mastery learning with translational outcomes. Med Educ 2014;48:375–85.. [DOI] [PubMed] [Google Scholar]
- [17].Li S, Hsieh TC, Rehder KJ, et al. Frequency of desaturation and association with hemodynamic adverse events during tracheal Intubations in PICUs. Pediatr Crit Care Med 2018;19:e41–50.. [DOI] [PubMed] [Google Scholar]
- [18].Lee JH, Turner DA, Kamat P, et al. The number of tracheal intubation attempts matters! A prospective multi-institutional pediatric observational study. BMC Pediatr 2016;16:58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Gabrani A, Kojima T, Sanders RCJ, et al. Downward trend in pediatric resident laryngoscopy participation in PICUs. Pediatr Crit Care Med 2018;19:e242–50.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Apfelbaum JL, Hagberg CA, Caplan RA, et al. Practice guidelines for management of the difficult airway: an updated report by the American Society of Anesthesiologists Task Force on management of the difficult airway. Anesthesiology 2013;118:251–70.. [DOI] [PubMed] [Google Scholar]
- [21].Kerrey BT, Rinderknecht A, Mittiga M. High risk, low frequency: optimizing performance of emergency intubation for children. Ann Emerg Med 2017;70:783–6.. [DOI] [PubMed] [Google Scholar]


