Abstract
Importance:
Overuse of medical tests and treatments is an increasingly recognized problem across health systems; best practices for reducing overuse are not clear. Framing the problem in terms of the spectrum of potential patient harm is likely to be an effective strategy for clinician and patient engagement in efforts to reduce overuse, but the scope of negative effects of overuse on patients has not been well described.
Objective:
To generate a comprehensive conceptual map documenting the processes through which overused tests and treatments lead to multiple domains of negative effects on patients.
Design:
For map development: An iterative consensus process informed by structured review of the literature on overuse and input from a panel of 6 international experts. For map verification: Systematic analysis of case reports involving overused services, identified through literature review and relevant article collections.
Setting:
Searches of MedLine (PubMed interface), manual review of relevant journal collections
Main Outcome and Measures:
Creation of conceptual map, identification of domains of negative effects on patients, verification of map through case review.
Results:
Our conceptual map documents that overused tests and treatments and resultant downstream services generate six domains of negative effects on patients: Physical, Psychological, Social, Financial, Treatment Burden, and Dissatisfaction with Healthcare. Negative effects can result from overused services and from downstream services; they can also trigger further downstream services that in turn can lead to more negative effects, in an ongoing feedback loop. Case reports on overuse confirmed the processes and domains of our conceptual map. Cases also revealed strengths and weaknesses in published communication about overuse: they were dominated by physical effects, with other negative effects receiving far less attention.
Conclusions and Relevance:
This evidence based conceptual map clarifies the processes by which overused tests and treatments negatively affect patients; it also documents multiple domains of negative effects experienced by patients. The map will be useful for facilitating comprehensive communication about overuse, estimating harms and costs related to overused services, and informing health system efforts to reduce overuse.
INTRODUCTION
Medical overuse, the provision of health services for which potential harms exceed potential benefits, is increasingly recognized as a threat to both value and quality of care in health systems worldwide1,2. There is broad recognition by physicians3 and policymakers4 of the magnitude of overuse. Avoiding overuse is appealing in its promise to control costs while improving clinical outcomes. However, despite agreement regarding the need to reduce overuse and focused attention on the issue for more than 5 years5, there is little clarity on best approaches to reducing overuse, and success has been limited 6.
Overuse is often framed primarily as a problem of high cost and resource stewardship 7–9, which may limit the effectiveness of efforts to reduce it. While physicians recognize a professional responsibility to contain costs to the system, they also believe that their primary obligation is to provide the best care to the individual patient10,11. Patients themselves may also be suspicious of efforts to contain costs12. Framing overuse in terms of its impact on patients may be a more effective approach for generating both physician and patient buy-in13. Such efforts require an understanding of negative effects of overused services on patients14,15. However, harms of overuse have been poorly described, with overuse research focusing largely on documenting prevalence of overuse 16,17 and its drivers 18,19.
Experts have developed conceptual frameworks for understanding overuse, identifying research priorities, and engaging clinicians in reducing overuse20–23. However, while these frameworks have noted the importance of understanding potential patient harms, none has defined the scope of negative effects on patients or the processes by which negative effects occur. A conceptual map specifically focused on negative effects on patients and the processes through which overused services result in harms is needed. Such a map could inform clinician discussions of overuse with patients, facilitate health delivery system efforts to curb overuse, and optimize research describing negative effects of specific overused services.
We used a systematic, evidence-based approach to generate and verify a comprehensive conceptual map documenting the broad range of negative patient effects from overused tests and treatments. We took a patient-centered approach to the development of the map since the impact on patients is of primary importance to practicing physicians. In developing this conceptual map, we aimed to 1) capture the breadth of negative effects on patients, 2) describe the processes by which overused tests and treatments lead to negative effects. We used published case reports describing overuse to verify map domains and identify the types of negative effects emphasized in published cases of overuse.
METHODS
Literature Search
To develop a comprehensive conceptual map, we first conducted a structured review of the literature on overuse to identify all documented negative effects on patients. We defined overuse as the provision of medical services, including diagnostic tests, medications, and therapeutic interventions, for which the potential for harm exceeds the potential for benefit2.
We began by reviewing overuse studies known to the research team, recording all overused services and negative effects mentioned. We then conducted a broad literature search (see Appendix Figure, Terms used in the search) to identify additional studies documenting or discussing negative effects of overuse. One investigator (AT) reviewed all retrieved titles and abstracts (n=1222) and identified potentially relevant articles (n=212); a second investigator (DK) then reviewed abstracts from this pool and selected those that described an overused service and at least one negative effect on patients for inclusion and further review (n=140).
To capture data from these 140 articles, we followed an iterative process: We randomly selected a set of 25 articles and recorded all overused services and associated negative effects mentioned. We repeated this process until no additional negative effects emerged. We reached saturation after reviewing 2 sets of 25 (total 50 papers).
Conceptual Map Development
Next, we sought to organize and categorize the negative effects identified through the literature search. To this end, we used an iterative consensus process: Initially each member of the research team independently reviewed the list of negative effects and grouped them into broader categories (e.g. short term, long term, physical, psychological, financial, etc.). The team then worked together to reach consensus on a set of categories capturing the range of overuse’s negative effects on patients.
We then used the categories to draft a conceptual map of overuse’s multiple negative effects on patients. The map aimed to capture the range of negative effects that can arise, as well as the relationships and feedback loops among overused services, negative effects, and downstream services. Again, we worked iteratively, making alterations to the general approach and visual presentation until reaching agreement.
We next obtained expert input to enhance the map’s comprehensiveness, clarity, and applicability. We recruited individuals from the U.S., Canada, and the U.K. with expertise in overuse research, implementation science, health services research, health economics, and clinical medicine. We conducted semi-structured interviews via WebEx with each expert to review the map and its potential applications. We used this feedback to refine the map on an ongoing basis. We reached saturation (with no further changes suggested) after interviewing six experts. After making minor graphic adjustments to the resulting map, we solicited additional comments and final approval from the same group of experts via email.
Conceptual Map Verification
Search Strategy to Identify Case Reports
To ensure applicability of our conceptual map to real-world patients, we collected published case descriptions describing overused services, processes of care related to overused services, and negative effects
We identified case descriptions illustrating the negative effects of overuse on patients by searching PubMed using the terms “Medical overuse” [Majr] and “case reports”. This process yielded 145 titles, which were reviewed by one author (DK) for relevance; 9 described a case with at least one negative effect from an overused service. We identified additional relevant cases by hand-searching article collections focused on overuse, including “Too Much Medicine” in The BMJ and “Teachable Moments” from the “Less is More” series in JAMA Internal Medicine. The search of article collections was performed by one author (BB) and checked by a second (DK). This search identified an additional 45 relevant cases, for a total of 54 case descriptions for inclusion in our analysis.
Coding of Case Descriptions
Using the QDA Miner Lite program, we coded all 54 relevant case descriptions. For each case we recorded the overused service, any resulting downstream services, and all negative effects. Overused services were classified by care site (inpatient, outpatient, emergency department), type (diagnostic vs. therapeutic), and category (laboratory testing, imaging, therapeutic procedure, medication, cardiac testing, catheter, other). Service classifications were performed by one investigator (BB) and verified by a clinician (DK). We recorded negative effects experienced by the index patient as well as theoretical or potential negative effects mentioned in the case descriptions but not necessarily experienced by the patient. All coding was done by one investigator (BB); a random 10% sample was also coded independently by a second investigator (DK). All differences in coding were resolved by discussion and consensus.
RESULTS
Conceptual map
The final conceptual map is shown in Figure 1. Overused services can lead to a cascade of downstream services. For example, a screening colonoscopy in an 80-year-old man can lead to a biopsy, hospitalization, and follow-up imaging tests. The overused service as well as downstream services can lead to negative effects. These negative effects can be short- or long-term, and short-term negative effects can become long-term. For example, a bowel perforation from colonoscopy may lead to chronic gastrointestinal symptoms.
Figure 1. Conceptual map.
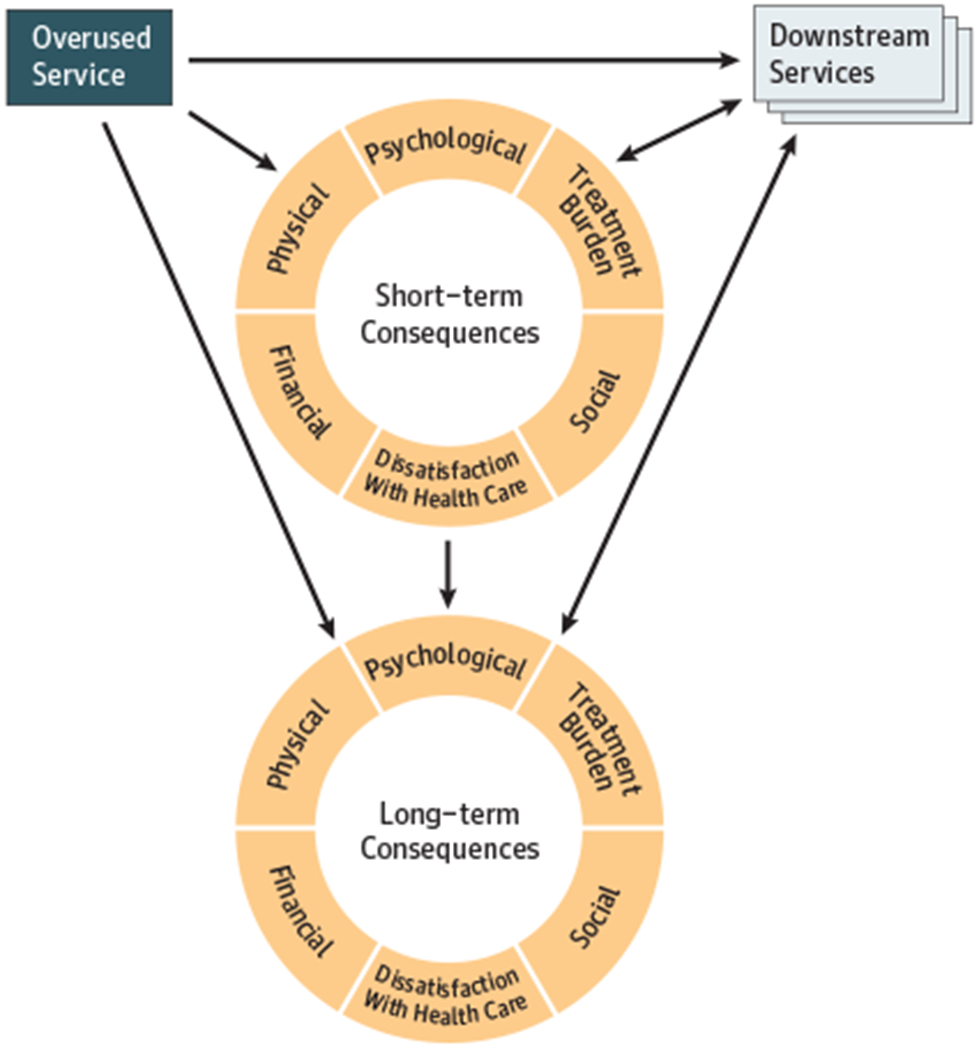
The conceptual map demonstrates that an overused service can lead directly to short- and/or long-term negative effects on patients across six domains. Overused services and negative effects can also lead to downstream services that themselves can lead to negative effects.
Negative effects fall into several domains, as detailed in Table 1:
‘Physical effects’ refer to temporary or permanent pain, injury, illness, or impairment. A short-term physical effect in this case could be pain from the procedure or discomfort from the bowel prep. A long-term physical effect could be disability from a procedural complication.
‘Psychological effects’ refer to negative emotions, mood symptoms, or psychiatric disorders. For example, patients may experience short-term anxiety from awaiting biopsy test results. In the long-term, patients could experience major depression related to a disability from a procedural complication.
‘Treatment burden’ refers to the workload patients must perform to manage health conditions. In the short-term, this might involve traveling to multiple appointments for overused and downstream services. In the long-term, this can involve managing chronic health conditions that arise as complications of overused procedures.
‘Social effects’ involve disruption of relationships or altered social identity or status due to a medical condition. In the short-term, this might involve a loss of ability to participate in social activities due to recovery from the procedure. In the long-term, this might involve loss of social networks due to ongoing physical problems caused by overuse.
‘Financial effects’ refer to monetary costs to patients from medical care. In the short-term, this can involve lost wages from time away from work. In the long-term, this can involve bankruptcy from ongoing medical costs.
‘Dissatisfaction with healthcare’ refers to unhappiness with or mistrust of health care services or providers. In the short-term, the patient might be frustrated with the health care provider for recommending a colonoscopy that was not clinically appropriate. In the long-term, the patient might come to mistrust health care providers in general for fear they will provide inappropriate care.
Table 1.
Domains of negative effects of overuse on patient
| Negative Effect Domain | Description | Examples |
|---|---|---|
| Physical | Temporary or permanent pain, injury, illness, or impairment32 | Procedural complications, disability, adverse drug effects, death |
| Psychological | Negative emotions, mood symptoms, or psychiatric disorders | Anxiety, stress, major depression, self-identification in the sick role |
| Treatment Burden | The workload patients must perform to manage health conditions 33–36 | Understanding and implementing disease management strategies, time traveling to and attending appointments |
| Social | Disruption of relationships, altered social identity or status due to a medical condition | Loss of ability to participate in family or other social networks, social labeling and stigma due to diagnosis |
| Financial | Monetary costs, including direct medical (treatment expenses), direct non-medical (non-medical expenses incurred while obtaining treatment), and indirect (lost productivity37 | Medical bills, travel costs, lost wages |
| Dissatisfaction with Healthcare | Unhappiness with or mistrust of health care services or providers38 | Frustration with clinical encounter, erosion of faith in clinician integrity and competence |
Any of these negative effects, particularly physical and psychological ones, can lead to yet more downstream services, creating a feedback loop in the overuse cascade. For example, complications from an unnecessary procedure could trigger additional treatments, which in turn could cause additional negative effects, leading to yet more treatments, and so on.
Map verification and characteristics of case descriptions
We verified applicability of our map using published case descriptions about overuse; we also used our map to assess the extent to which case descriptions document the full range of negative effects on patients. Fifty-four case descriptions described a total of 63 overused services. Nearly all case descriptions (49 [91%]) described the overuse cascade, with an average of 4.2 downstream services identified per case and 227 downstream services mentioned in total. Figure 2 illustrates two examples of the overuse cascade from case descriptions.
Figure 2. Examples of the overuse cascade.
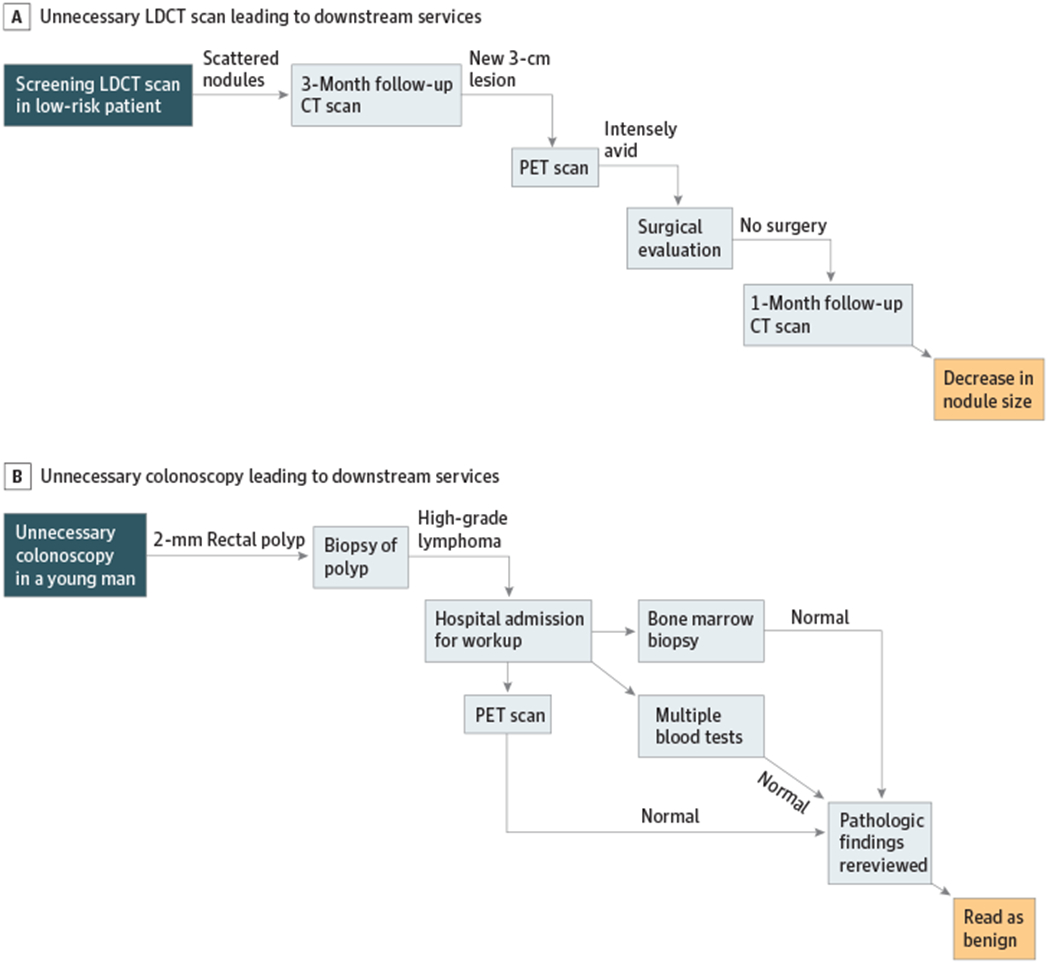
Case examples in which an abnormal result of an unnecessary test leads to a series of downstream services. These services may represent appropriate responses to abnormal findings or may include additional unnecessary services or medical errors, leading to negative effects on patients.
Panel A: Unnecessary screening low-dose CT scan (overused service) revealed scattered nodules. This finding led to a 3-month follow-up scan, which then led to a PET scan, a surgical evaluation, and ultimately another follow-up scan.
Panel B: Unnecessary colonoscopy revealed a polyp; biopsy was initially misread as high-grade lymphoma, which precipitated hospital admission with bone-marrow biopsy, PET scan, and multiple blood tests. Ultimately the biopsy was re-reviewed and findings were reclassified as benign.
The cases described an average of 3.2 negative effects per case. All cases identified at least one short-term negative effect. However, only one case reported a long-term negative effect. Most case descriptions (61%) demonstrated the overuse cascade feedback loop in which negative effects led to additional downstream services, which in turn led to more negative effects.
All domains from our conceptual map were represented in case descriptions. Across cases, physical effects predominated (69%), followed by psychological effects (16%) and treatment burden (9%). Financial effects (3%) and dissatisfaction with healthcare (2%) were rarely described. Only one case mentioned social effects. Table 2 provides examples of negative effects in each domain from cases in our sample.
Table 2.
Negative effects of overuse. Case examples in each domain.
| Negative Effect Domain | Example | |
|---|---|---|
| Clinical scenario | Negative effect | |
| Physical | Unnecessary CT angiography showed CAD, which led to coronary angiography and ultimate 3-vessel coronary artery bypass graft surgery (CABG)39 | Heart failure as a complication of the CABG |
| Psychological | Unnecessary thrombophilia testing after a provoked DVT, with “abnormal” findings that were not clinically meaningful40 | Significant worry about passing rare disorders on to her children |
| Treatment burden | Overly tight control of type 2 diabetes with insulin led to multiple episodes of hypoglycemia and related anxiety41 | Sense of being overwhelmed, inability to fully engage in care |
| Social | Unnecessary hospitalization for arthritis in an elderly woman27 | Prolonged inpatient rehab stay with removal from usual enjoyable social activities |
| Dissatisfaction with healthcare | Unnecessary FFP for an asymptomatic supratherapeutic INR led to a severe transfusion reaction42 | Patient was distressed by the reaction and openly questioned the need for the transfusion |
| Financial | An elderly man was taking over 50 dietary supplements as recommended by his physician43 | Annual out of pocket cost of $36,000, despite limited income |
Physical effects were depicted with greater detail than other effects and often dominated case reports. Physical problems were typically described at length in precise clinical language:
[The patient] presented with acute-onset confusion, word-finding difficulty, and short-term memory defects.7
He pulled out his urinary catheter, causing severe trauma evidenced by profuse gross hematuria.24
In contrast, psychological effects were often described only briefly or in passing, using vague, non-clinical terms (“worry,” “feeling overwhelmed,” “emotional distress,” “increased patient concern”). Dissatisfaction with healthcare was also frequently depicted in elusive or equivocal language, as patients “expressed regret” or “wondered what good, if any, had come of all the testing.” Similarly, most mentions of financial impact were imprecise: A few cases specified dollar amounts (as in the example in Table 2), but more often costs to patients were described in abstract terms (“higher costs,” “additional costs,” “excess cost”). Descriptions of treatment burden were especially unclear: Many cases, for example, mentioned that patients had experienced excess hospitalization during the overuse cascade, but few explicitly identified this as a negative effect or burden on the patient. In most cases, treatment burden was implied, not explicit.
DISCUSSION
We used a systematic, evidence-based, expert-informed approach to develop a conceptual map of negative effects of medical overuse on patients. Our map captures the breadth of negative effects on patients by defining multiple domains of potential negative effects and describes the process of the overuse cascade through which patients are affected25,26. Our review of published cases documenting negative effects of an overused service reinforced both the domains of our map and the importance of the overuse cascade in the process through which overused services ultimately harm patients. While our map may represent negative effects from any health service, even needed care, it is unique in its focus on overuse and its potential for enhancing understanding of overuse.
Our review of published cases confirmed the domains of negative effects that emerged from the systematic review and expert panel process. In addition, while they may not reflect the true prevalence or severity of specific types of harms, published cases offered important insights into clinician thinking about negative effects of overused services. Though all domains were mentioned in the cases, nearly all identified negative effects were short-term, with physical problems dominating descriptions. The focus on short-term effects is not surprising. Many physicians, particularly hospitalists, follow patients for only a short time and may lack knowledge of long-term outcomes. In addition, short-term negative effects are easier to attribute to a specific overused service compared to long-term effects, whose origin may become obscured over time.
The emphasis on physical effects is likely related to several factors. First, cases published in the medical literature are authored by clinicians and reflect the clinician perspective and/or understanding of the patient experience, which may be limited. Physical effects, particularly short-term effects, are easiest for clinicians to recognize and describe, especially when they are severe27. However, negative effects in other domains should also be recognized given that they are common and can substantially impact patient well-being. For example, in the US, high out of pocket costs are increasingly recognized as a toxic “side effect” of all care. Incurring debt as a result of unneeded care is of particular concern28 but may be unrecognized by physicians and was rarely mentioned in case descriptions. Further, being diagnosed with a health condition is associated with anxiety and depression29,30. Overused services that result in labeling with a new “diagnosis” (even if that diagnosis does not impact physical health) can similarly lead to psychological distress, though it may not be apparent to treating clinicians. Moreover, treatment burden and social disruption occur routinely but are generally unmentioned by patients and unappreciated by their clinicians as they seem outside the realm of clinical medicine. These non-physical negative effects are important to consider when weighing or conveying the value of avoiding unnecessary services.
The process used to develop this conceptual map has some limitations. First, after searching the literature on overuse we reviewed a random sample of papers; other domains may have emerged with comprehensive review. However, no other domains emerged in our case reviews and expert interviews and our domains are similar to those developed to categorize patient harms in other clinical contexts31. Second, we engaged with six experts in the field when designing the conceptual map, and it is possible that talking to more experts or different experts may have led us in a different direction. Further, we may have missed published case reports of overused services with negative effects, as they are difficult to identify, though we used a systematic process for locating cases. Moving forward, eliciting patient perspectives on the relative importance of negative effects in each domain will further enhance the applicability of our conceptual map.
In conclusion, our evidence-based conceptual map clarifies the processes by which overuse of medical services negatively affects patients and identifies the domains of negative effects. It represents an important addition to existing frameworks designed to codify the process of overuse. As efforts to reduce overuse move forward, our conceptual map can be useful at all levels: facilitating individual clinician communication with patients, enabling accurate estimates of the costs of overuse in economic analyses, and informing broader health system efforts to curb overuse.
Supplementary Material
Figure 3.
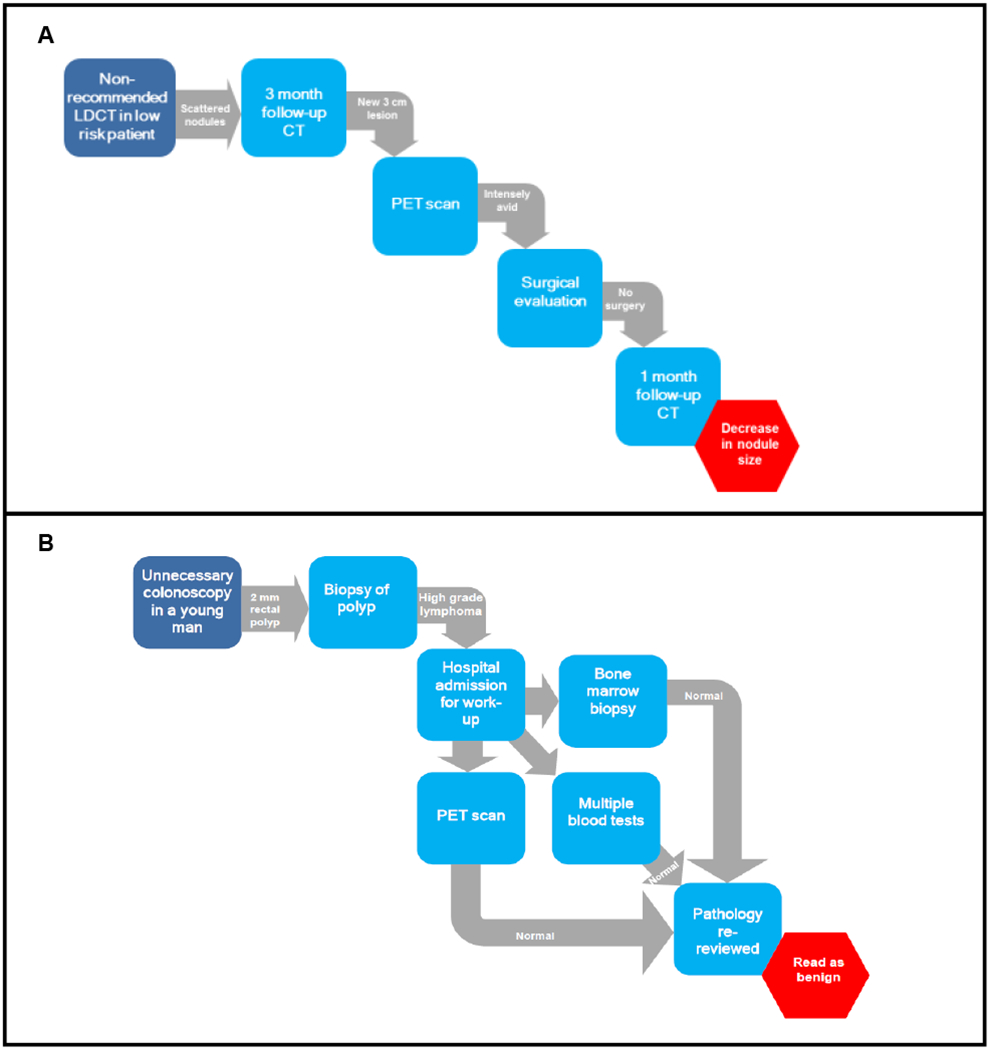
Examples of the overuse cascade
Key Points.
Question:
What is the scope of negative effects on patients from overused medical tests and treatments?
Findings:
We developed an evidence-based conceptual map of negative effects of overuse that defined six domains: Physical, Psychological, Social, Financial, Treatment Burden, and Dissatisfaction with Healthcare. Negative effects in these domains can result directly from overused services and indirectly from downstream services. Negative effects themselves can also lead to additional downstream services.
Meaning:
Clarifying the breadth of potential negative effects of overuse on patients and the processes that can lead to them can inform efforts to understand and reduce overuse.
Acknowledgments:
The authors wish to thank our expert panel: Andrew Briggs, Teresa Damush, Dan Morgan, Hsien Seow, and Saul Weingart. In addition, we thank Antonio DeRosa for assistance with literature searches and Chris Kaeser for design assistance.
All authors report no relevant conflicts of interest. DK participated in study design, data collection and analysis, and drafted the manuscript. SC participated in study design and data collection and manuscript editing, BB participated in data collection and manuscript editing, SK participated in study design and manuscript editing, AT participated in data collection and manuscript editing, and ALS participated in study design, data collection, and manuscript editing.
No external funding was obtained specifically for this study but the work of Drs. Korenstein and Lipitz-Snyderman were supported in part by the NIH/NCI P30 CA008748 Cancer Center Support Grant. The funder had no role in the design of the study; the collection, analysis, and interpretation of the data; or approval of the finished manuscript.
References
- 1.Brownlee S, Chalkidou K, Doust J, et al. Evidence for overuse of medical services around the world. Lancet. 2017;390(10090):156–168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chassin MR, Galvin RW. The urgent need to improve health care quality. Institute of Medicine National Roundtable on Health Care Quality. JAMA. 1998;280(11):1000–1005. [DOI] [PubMed] [Google Scholar]
- 3.Lyu H, Xu T, Brotman D, et al. Overtreatment in the United States. PloS One. 2017;12(9):e0181970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rich EC, Lake TK, Valenzano CS, Maxfield MM. Paying the doctor: evidence-based decisions at the point-of-care and the role of fee-for-service incentives. J Comp Eff Res. 2013;2(3):235–247. [DOI] [PubMed] [Google Scholar]
- 5.Berwick DM, Hackbarth AD. Eliminating waste in US health care. JAMA. 2012;307(14):1513–1516. [DOI] [PubMed] [Google Scholar]
- 6.Rosenberg A, Agiro A, Gottlieb M, et al. Early Trends Among Seven Recommendations From the Choosing Wisely Campaign. JAMA Intern Med. 2015;175(12):1913–1920. [DOI] [PubMed] [Google Scholar]
- 7.Chamberlain E, DiVeronica M, Segura R. When Medical Care Leads to Harm--Difficulty Finding Words: A Teachable Moment. JAMA Intern Med. 2015;175(8):1271–1272. [DOI] [PubMed] [Google Scholar]
- 8.Mukerji G, Weinerman A, Schwartz S, Atkinson A, Stroud L, Wong BM. Communicating wisely: teaching residents to communicate effectively with patients and caregivers about unnecessary tests. BMC Med Educ. 2017;17(1):248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wolfson D, Santa J, Slass L. Engaging physicians and consumers in conversations about treatment overuse and waste: a short history of the choosing wisely campaign. Acad Med. 2014;89(7):990–995. [DOI] [PubMed] [Google Scholar]
- 10.Buist DS, Chang E, Handley M, et al. Primary Care Clinicians’ Perspectives on Reducing Low-Value Care in an Integrated Delivery System. Perm J. 2016;20(1):41–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Tilburt JC, Wynia MK, Sheeler RD, et al. Views of US physicians about controlling health care costs. JAMA. 2013;310(4):380–388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Schleifer D, Rothman DJ. “The ultimate decision is yours”: exploring patients’ attitudes about the overuse of medical interventions. PloS One. 2012;7(12):e52552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Liao JM, Schapira MS, Navathe AS, Mitra N, Weissman A, Asch DA. The Effect of Emphasizing Patient, Societal, and Institutional Harms of Inappropriate Antibiotic Prescribing on Physician Support of Financial Penalties: A Randomized Trial. Ann Intern Med. 2017;167(3):215–216. [DOI] [PubMed] [Google Scholar]
- 14.Grady D, Redberg RF. Less is more: how less health care can result in better health. Arch Intern Med. 2010;170(9):749–750. [DOI] [PubMed] [Google Scholar]
- 15.Hicks LK. Reframing overuse in health care: time to focus on the harms. J Oncol Pract. 2015;11(3):168–170. [DOI] [PubMed] [Google Scholar]
- 16.Chan KS, Chang E, Nassery N, Chang HY, Segal JB. The state of overuse measurement: a critical review. Med Care Res Rev. 2013;70(5):473–496. [DOI] [PubMed] [Google Scholar]
- 17.Korenstein D, Falk R, Howell EA, Bishop T, Keyhani S. Overuse of health care services in the United States: an understudied problem. Arch Intern Med. 2012;172(2):171–178. [DOI] [PubMed] [Google Scholar]
- 18.Colla CH, Kinsella EA, Morden NE, Meyers DJ, Rosenthal MB, Sequist TD. Physician perceptions of Choosing Wisely and drivers of overuse. Am J Manag Care. 2016;22(5):337–343. [PubMed] [Google Scholar]
- 19.Kachalia A, Berg A, Fagerlin A, et al. Overuse of testing in preoperative evaluation and syncope: a survey of hospitalists. Ann Intern Med. 2015;162(2):100–108. [DOI] [PubMed] [Google Scholar]
- 20.Morgan DJ, Brownlee S, Leppin AL, et al. Setting a research agenda for medical overuse. BMJ. 2015;351:h4534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Morgan DJ, Leppin AL, Smith CD, Korenstein D. A Practical Framework for Understanding and Reducing Medical Overuse: Conceptualizing Overuse Through the Patient-Clinician Interaction. J Hosp Med. 2017;12(5):346–351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Nassery N, Segal JB, Chang E, Bridges JF. Systematic overuse of healthcare services: a conceptual model. Appl Health Econ Health Policy. 2015;13(1):1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Parchman ML, Henrikson NB, Blasi PR, et al. Taking action on overuse: Creating the culture for change. Healthc (Amst). 2017;5(4):199–203. [DOI] [PubMed] [Google Scholar]
- 24.Al-Abri M, Wong BM, Leis JA. A urinary catheter left in place for slightly too long: A teachable moment. JAMA Intern Med. 2015;175(2):163–163. [DOI] [PubMed] [Google Scholar]
- 25.Lipitz-Snyderman A, Korenstein D. Reducing Overuse-Is Patient Safety the Answer? JAMA. 2017;317(8):810–811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Mold JW, Stein HF. The cascade effect in the clinical care of patients. N Engl J Med. 1986;314(8):512–514. [DOI] [PubMed] [Google Scholar]
- 27.Brennan-Taylor MK. “Mom, You Have to Trust Me”. JAMA Intern Med. 2015;175(9):1441. [DOI] [PubMed] [Google Scholar]
- 28.Ubel PA, Abernethy AP, Zafar SY. Full disclosure--out-of-pocket costs as side effects. N Engl J Med. 2013;369(16):1484–1486. [DOI] [PubMed] [Google Scholar]
- 29.Cotter AR, Vuong K, Mustelin L, et al. Do psychological harms result from being labelled with an unexpected diagnosis of abdominal aortic aneurysm or prostate cancer through screening? A systematic review. BMJ. 2017;7(12):e017565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.de Ridder D, Geenen R, Kuijer R, van Middendorp H. Psychological adjustment to chronic disease. Lancet. 2008;372(9634):246–255. [DOI] [PubMed] [Google Scholar]
- 31.Harris RP, Sheridan SL, Lewis CL, et al. The harms of screening: a proposed taxonomy and application to lung cancer screening. JAMA Intern Med. 2014;174(2):281–285. [DOI] [PubMed] [Google Scholar]
- 32.Department of Health and Human Services, National Institutes of Health, National Cancer Institute. Common Terminology Criteria for Adverse Events (CTCAE) Version 4.03. https://evs.nci.nih.gov/ftp1/CTCAE/CTCAE_4.03/CTCAE_4.03_2010-06-14_QuickReference_8.5x11.pdf. Accessed December 15, 2017.
- 33.Gallacher KI, Montori VM, May CR, Mair FS. Treatment Burden and Multimorbidity. 2016. https://basicmedicalkey.com/treatment-burden-and-multimorbidity/. Accessed December 15, 2017.
- 34.Gallacher K, Jani B, Morrison D, et al. Qualitative systematic reviews of treatment burden in stroke, heart failure and diabetes - Methodological challenges and solutions. BMC Med Res Methodol. 2013;13(1):10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Opportunity Costs In Modern Medicine. Health Aff (Millwood). 1992;11(2):162–169. [DOI] [PubMed] [Google Scholar]
- 36.V-T T Burden of treatment: the work of being a patient. Minimally Disruptive Medicine. https://minimallydisruptivemedicine.org/2015/06/29/burden-of-treatment-the-work-of-being-a-patient/. Published June 29, 2015 Accessed November 3, 2017.
- 37.Direct Medical Costs In: Kirch W. (eds) Encyclopedia of Public Health. Springer Link Website; https://link.springer.com/referenceworkentry/10.1007/978-1-4020-5614-7_802. Accessed November 3, 2017. [Google Scholar]
- 38.Blendon RJ, Benson JM, Hero JO. Public Trust in Physicians — U.S. Medicine in International Perspective. N Engl J Med. 2014;371(17):1570–1572. [DOI] [PubMed] [Google Scholar]
- 39.Schmidt T, Maag R, Foy AJ. Overdiagnosis of coronary artery disease detected by coronary computed tomography angiography: A teachable moment. JAMA Intern Med. 2016;176(12):1747–1748. [DOI] [PubMed] [Google Scholar]
- 40.Gupta A, Sarode R, Nagalla S. Thrombophilia testing in provoked venous thromboembolism: A teachable moment. JAMA Intern Med. 2017;177(8):1195–1196. [DOI] [PubMed] [Google Scholar]
- 41.Rodriguez-Gutierrez R, Lipska KJ, McCoy RG. Intensive glycemic control in type 2 diabetes mellitus—a balancing act of latent benefit and avoidable harm: A teachable moment. JAMA Intern Med. 2016;176(3):300–301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Tummalapalli S, Qiu Y, Cho HJ. Anticoagulation reversal for supratherapeutic international normalized ratio: A teachable moment. JAMA Intern Med. 2017;177(6):869–870. [DOI] [PubMed] [Google Scholar]
- 43.Strewler A, Conroy R, Kao H. Approach to overuse of herbal and dietary supplements: A teachable moment. JAMA Intern Med. 2014;174(7):1033–1034. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


