Abstract
Background:
CMS recently decided to produce private “healthcare disparities reports” that include dual eligibility (DE) as the sole stratifying variable used to assess pneumonia readmission disparities.
Research design:
We measure the relationship between DE status and readmissions, both with and without conceptually relevant social risk factors, including air pollution, severe housing problems, and food insecurity, using data from county- and hospital-level readmission rates, DE status, and social risk factors.
Results:
At the county level, the relationship between DE status and readmissions is partially confounded by at least three social risk factors. DE populations vary widely across hospitals, creating unequal between-hospital comparisons.
Conclusions:
Because of differences in the DE population, between-hospital comparisons could be misleading using a methodology that stratifies by DE only. We suggest viable alternatives to sole-factor stratification to properly account for social risk factors and better isolate quality differences that might yield readmission rate inequities.
Implications:
CMS's healthcare disparities reports provided to hospitals are limited by relying exclusively on DE proportion as the measure of social risk, undercutting the power of quality measurement and its related incentives to close or minimize healthcare inequities.
Keywords: dual eligibility, health equity, readmissions, social risk
1. Introduction
Although social risk factors (SRFs) have long been acknowledged by researchers to be major contributors to health and healthcare inequities,[1–3] until recently policymakers have been resistant to adopt quality measurement methodologies that account for social risk, despite its potentially confounding impact on measured quality differences. For example, the Centers for Medicare and Medicaid Services (CMS) had long prohibited the inclusion of sociodemographic status (SDS) in risk-adjustment specifications for quality measures, citing concern that such inclusion would “mask potential disparities or minimize incentives to improve the outcomes of disadvantaged populations.”[4]
In an important shift, after lengthy national debate and study that weighed the above concerns against the potential benefits of better accounting for inequity-promoting SRF differences,[5] in September of 2018 CMS sent hospitals private disparities reports that stratify pneumonia readmission rates by dual eligibility status (DE) in order to assess both “within hospital” disparities (How often do our DE patients readmit compared to our non-DE patients?) and to compare that hospital's readmissions gap to the national average disparity as a “between hospital” measure.[6] No rewards or penalties are associated with these reports and, beyond DE, no other SRF data are included in the analysis. In subsequent annual private reports, in addition to pneumonia, CMS provided DE-stratified readmission data for five additional conditions.
Given its strong correlation with poverty, itself an important predictor of health and health care outcomes,[5] using DE proportion as a proxy for other SRFs that might also influence readmission rates (e.g., access to transportation, level of social support, etc) has significant face validity. Furthermore, there is ample evidence that DE patients may receive poorer quality hospital care and that they are more likely than non-DE patients to readmit.[7,8]
However, the exclusive reliance on DE proportion as a proxy for all other SRFs is potentially problematic, particularly for between hospital comparisons. Such a juxtaposition assumes that DE patients across the country are identical in terms of their exposure to SRFs. That is, for CMS’ between-hospital comparison to be fair, DEs at every hospital being compared must face identical social challenges. If not, the methodology will likely unfairly penalize hospitals with more socially complex DE patients for factors unrelated to quality of care and, because DE is a proxy for so many diverse social risk factors, its use may not inform hospital based DE-specific interventions that address the salient mechanisms at play in a given community.
Figure 1 depicts how SRFs might partially confound the posited relationship between DE proportion and readmissions. We define a potentially confounding variable as one that both influences the outcome of interest (readmissions) and is correlated with the exposure of interest (in this case DE proportion). Given the positive correlations posited in Figure 1, in this instance any confounding would likely overestimate the relationship between DE proportion and readmissions.
Figure 1.
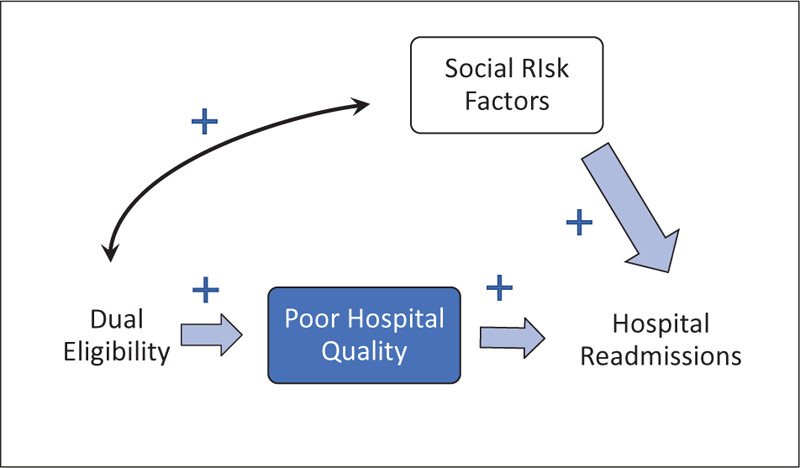
Potentially confounded relationship between dual eligibility and hospital readmissions.
This paper seeks to examine the validity and potential pitfalls of relying exclusively on DE proportion as an SRF proxy. Using county-level SRF data, we first measured the relationship between DE proportion, SRFs, and readmission rates to understand whether the relationship between DE and readmissions was confounded by SRFs. We then examined variation in hospitals’ patients’ county of residence and the distribution of SRFs within those counties to better understand if any observed confounding might impact the between-hospital comparisons in CMS’ disparities reports.
2. Methods
2.1. Hospital data
We collected hospital-wide readmission rates from the July 2018 release of Hospital Compare,[9] which measures risk-adjusted readmission rates based on all hospital discharges from July 1, 2016 to June 30, 2017. The readmission rates are measured as the risk-adjusted percent (from 0% to 100%) of patients that return to the hospital during the 30 days after discharge after an inpatient hospital stay. Only Medicare fee-for-service (FFS) patients over the age of 65 are included in the measurement. Risk adjustment accounts for some patient clinical characteristics, comorbidities, and previous medical histories.
To measure each hospital's dual eligible patient population, we computed the percent of unique inpatient discharges that were flagged as dually eligible for Medicare and Medicaid from the 2016 Medicare Standard Analytic Files (SAF), including the 100% inpatient and denominator files. Using the patient's county of residence from the same source, we computed hospital-level patient SRF rates. Hospitals with fewer than 25 discharges from dual eligible patients were removed from all analysis.
2.2. County data
We collected county-level data from the County Health Rankings and Roadmaps database[10] on air pollution, housing problems, and food insecurity. These three SRFs were chosen based on the available literature as factors that might impact a patient's readmission rate.[11–13] Air Pollution is defined as the average daily density of fine particulate matter in micrograms per cubic meter (PM2.5) and was collected by the Environmental Public Health Tracking Network in 2012. The severe housing problems rate was collected by Comprehensive Housing Affordability Strategy (CHAS) from 2010 to 2014 and is defined as the percentage of households with one or more of the following housing problems:
-
1.
housing unit lacks complete kitchen facilities,
-
2.
housing unit lacks complete plumbing facilities,
-
3.
household is severely overcrowded or
-
4.
household is severely cost burdened.
Food insecurity was derived from the Mind the Meal Gap project, the result of 2015 survey data using the Core Food Insecurity Model.
We also used county-level Medicare readmission rate and DE status for comparison in our results. As in the hospital-level analysis above, readmission measures 30-day post discharge hospital revisit rates from CMS. These data were derived from Medicare's Public Use File (PUF) Geographic Variation File.[14]
2.3. Models
To summarize the strength of the relationship between variables and to establish whether SRFs potentially confound the county-level relationship between DE proportion and readmission rates, we first correlated housing problems, air pollution, and food insecurity with county-level readmission rates and DE proportion. We calculated correlation coefficients, using a t-test for calculating statistical significance.
To test whether each SRF is independently correlated with readmission after controlling for dual eligible status, we compare two county-level models predicting county-level readmission rates. In regression Model 1, we regressed DE against readmission rates, using ordinary least squares (OLS). For Model 2, also in Table 2, we used the same specification from Model 1 but added a vector of three county-level SRFs, including air pollution levels, severe housing problems rate, and food insecurity rate. Positive coefficients in Model 2 for our three SRF variables will confirm that those variables independently correlate with readmission even after controlling for DE status. The difference between dual eligible proportion's coefficient size between Model 1 and 2 estimates the size of SRFs’ attenuation effects on DE's impact on readmission. In each Model 1 and 2, we calculated model fit statistics (Adjusted-R2) and statistical significance using robust standard errors.
Table 2.
Relationship between dual eligibility and readmission rates before and after adding SRF controls.

To contrast the dual eligible patients’ level of SRF exposure, we aggregated DE patient data to the hospital level, using the patient's county of residence to estimate the SRF exposure level. The technique, described below, served to rank hospitals from lowest to highest average SRF exposure of hospitals’ dual eligible patients for each factor. We took the following steps for each SRF:
-
1.
Extracted inpatient claims-level data with patient county of residence for only those patients who were dually eligible
-
2.
Assigned each patient the SRF characteristics of their county of residence. For example, a patient that lived in a county with a severe housing problems rate of 10% had all their discharge assigned a value of 10%.
-
3.
Removed hospitals with fewer than 25 dual eligible patients
-
4.
Calculated hospital-level exposure by averaging across the county of residence for all dual-eligible discharges.
-
5.
Ranked all hospitals by exposure rate for each SRF.
-
6.
Computed minimum, maximum, median, 25th percentile, and 75th percentile hospital exposure rates for each SRF across hospitals.
The result represents average SRF exposure of each hospital's dual eligible patients and rank based on the average county where their dual eligible patients reside. Differences in the range of SRF exposure for dual eligible patients measured the extent to which SRF confounding affects a between-hospital comparison model. We then related the differences to the potential confounding effect found in our previous models.
3. Results
3.1. Section 1. Is the county-level relationship between DE proportion and readmission rates confounded by SRFs?
Air pollution, housing instability, and food insecurity are all statistically significantly positively correlated to both DE proportion and readmission rates and can thus be considered potential confounders of the relationship between DE proportion and readmission rates at the county level (Table 1). The next exhibit tests whether this potential confounding can be considered actual confounding.
Table 1.
Correlation coefficients between SRFs and readmission rates.
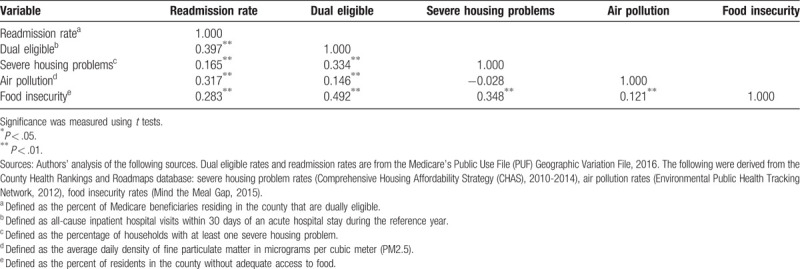
Table 2 presents results of regressing county-level readmission rates on county-level DE proportion both excluding SRFs (Model 1) and including SRFs (Model 2). Model 1 establishes that at the county level, a one percent increase in a county's proportion of dually eligible residents is related to a 0.13 increase in the county's readmission rate (or 0.13 readmissions per 100 discharges), statistically significant at the P < .01 level.
When SRF data are included in Model 2, the relationship between DE and readmissions is attenuated: the coefficient for DE proportion decreases by 22%, indicating that at the county level DE proportion is partially confounded by the included social factors. [15] We also find that each SRF included in the model had a statistically significant coefficient in the expected direction, implying that differences in SRFs would be expected to correspond to differences in readmission rates. Furthermore, the inclusion of SRF variables increases the proportion of explained county-level variance (R2) in readmission rates by 61%, suggesting Model 2 is a better fit.
3.2. Section 2. Comparison of the average SRF exposure across hospitals’ dual eligible patients
Figure 2 shows that hospitals’ DE patients’ SRF exposure (the blue box-and-whisker plot) varies greatly across US hospitals. For all three SRFs included in the current analysis, the range of hospitals’ DE-patients’ SRF exposure is nearly as wide as the range of SRF exposure across US counties themselves. Thus, some hospitals have dual eligible patients that live almost exclusively in counties with the highest exposure to social risk as defined, while other hospitals care for DE patients with minimal SRF exposure.
Figure 2.
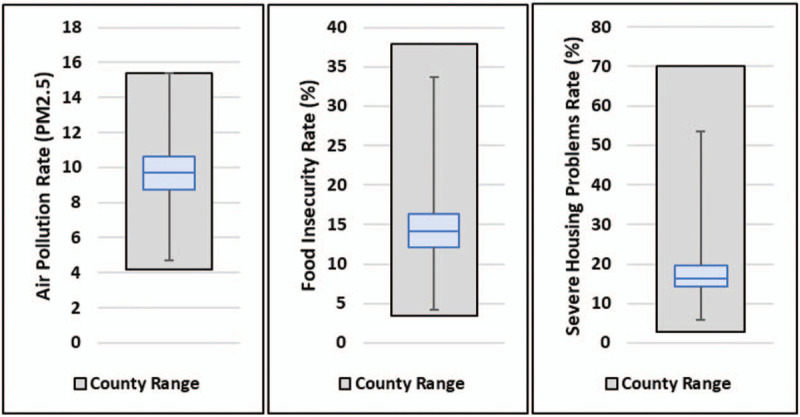
Range of average SRF exposure of hospitals’ dual eligible patients. Authors’ analysis of County Health Rankings and Roadmaps database (county range) and Medicare claims data, 2016. Upper whisker—maximum hospital (highest exposure). Lower whisker—minimum hospital (lowest exposure). Horizontal blue line = median hospital. Blue box: 25th to 75th percentile hospital.
Importantly, the interquartile range is narrow for each SRF: hospitals from the 25th to the 75th percentile tend to be only a few points apart in terms of their DE-patients’ SRF exposure. However, our regression coefficients demonstrate that even a small increase in SRFs can translate to a meaningful increase in readmissions. For example, a one-unit increase in the air pollution rate, which is about half of the interquartile range, corresponds to an additional 0.52 patients readmitted per 100 discharges.
4. Discussion
4.1. Summary of findings
Our results show that at the county level, the relationship between the proportion of DE residents and readmission rates is partially confounded by conceptually relevant SRFs such as air quality, housing instability, and food insecurity. Furthermore, our analyses demonstrate that not all DE patients are homogenous in terms of their SRF exposure. Thus, CMS’ current methodology comparing one hospitals’ readmissions gap to all others’ is limited by between-hospital differences in the social complexity of DE patients. Should CMS eventually use the current methodology to reward or penalize hospitals for their gaps (or lack thereof), hospitals treating patients with greater social complexity are very likely to be unfairly penalized for non-quality related neighborhood factors.
Thus, while CMS’ emergent use of quality measurement to address healthcare inequities is laudable insofar as it raises awareness and moves towards an incentive structure focused on narrowing such avoidable gaps, the chosen methodology hamstrings these efforts by reducing relevant SRFs to a single factor—DE proportion—that is correlated with confounding variables to which DE populations are exposed to varying degrees.
4.2. Implications for policy
There are alternatives. In the short term, one way CMS could ensure apples-to-apples comparisons in their between hospital measure is to sub-stratify by an SRF exposure variable. In this scenario, CMS could specify a conceptual model that isolates SRFs particularly relevant for a quality indicator (such as air quality for pneumonia readmissions) and then compare hospitals whose DE patients experience similar exposure to those SRFs. This would allow sub-strata specific positive deviant hospitals to be identified and studied so that effective practices could be disseminated and implemented by hospitals treating similar DE populations.
The long-term fix lies in developing robust national datasets of SRFs (at both patient and community levels) that can be used as adjustors for a given quality measure based on conceptual and empirical relationships since covariates relevant for pneumonia readmissions might not be as relevant for hip replacement readmissions. While some extant datasets might be leveraged for this, significant new investments will be needed to develop and align SRF data collection at the national level as well as within clinical records. The need for such a national data system that gathers comprehensive and valid demographic and social factor data has only increased as its absence has greatly hindered our nation's efforts to identify and intervene on health inequities laid bare by COVID-19.[16]
Although DE might be the only social risk factor variable for which there is enough data to produce national reports, and thus CMS has necessarily settled on what is currently feasible, we must acknowledge that it is conceptually, CMS has seemingly settled for what is currently feasible: using DE proportion as a universal proxy. This is conceptually unsound and runs the risk, should penalties eventually be tied to disparities gaps, of depriving safety net providers the resources needed to care for the most socially and clinically complex of patients.
4.3. Limitations
We relied on county-level data to explore the relationship between social risk and readmission rates. Community- or individual-level data, which are not nationally available, would be more precise and avoid the ecologic fallacy of drawing conclusions for individual patients based on population level data. However, as health inequities are population-level as opposed to individual- or patient-level dynamics, this limitation is somewhat mitigated. Additionally, our data were limited to hospital-wide readmissions information rather than targeting specific conditions like pneumonia readmissions, which as noted above may be responsive to different social factors.
5. Conclusion
While CMS’ efforts to provide hospitals with stratified analysis to identify quality and healthcare inequities is an important step forward in using measurement to close or minimize such gaps, the chosen method of using DE proportion to represent a complex, multifaceted relationship is far from an acceptable standard in large measure because it is not wholly valid. This present research supports the adoption of a more nuanced, evidence-based approach to account for social risk, either via simple sub-stratification by SRF exposure or, in a future state, via the inclusion in risk adjustment models of specific patient- and community-level SRFs that satisfy the definition of “confounder” provided above. By relying exclusively on DE proportion as the measure of social risk, we undercut the power of quality measurement and its related incentives to close or minimize healthcare inequities.
Author contributions
Both authors made substantial contributions to the design of the study, as well as hands-on analysis of the data, including interpretation and visualization. Drafting was the responsibility of both authors, each of which wrote large portions of the paper, and reviewed writing by the other. Both authors have given final approval for the published version and are accountable for all aspects of the work.
Correction
The author affiliations originally appeared as both authors having two affiliations. The first affiliation, Health Equity Policy, was incorrect and has since been removed.
In Table 1, the lettered footnotes were incorrectly assigned in column 1 and have since been corrected.
Footnotes
Association of American Medical Colleges, Washington, DC, USA.
Abbreviations: CHAS = Comprehensive Housing Affordability Strategy, CMS = Centers for Medicare and Medicaid Services, DE = dual eligibility, PM2.5 = particulate matter in micrograms per cubic meter, PUF = public use files, SAF = Standard Analytic Files, SRF = social risk factors.
How to cite this article: Alberti PM, Baker MC. Dual eligible patients are not the same: How social risk may impact quality measurement's ability to reduce inequities. Medicine. 2020;99:38(e22245).
The authors have no funding sources to disclose.
The authors have no conflicts of interest to disclose.
This study was exempt from ethical approval and review by an Institutional Review Board because it did not use identifiable human subjects data. Claim-level data was de-identified and subject to a data use agreement.
The datasets generated during and/or analyzed during the present study are publicly available.
References
- [1].Dulin MF, Tapp H. Communities matter: the relationship between neighborhoods and health. N C Med J 2012;73:381–8.. [PubMed] [Google Scholar]
- [2].Robert Wood Johnson Foundation and University of Wisconsin Population Health Institute, Givens M, Gennuso K, Jovaag A, et al. 2017 County Health Rankings: Key Findings Report. 2017. [Google Scholar]
- [3].DeMilto L, Nakashian M. Using social determinants of health data to improve health care and health: a learning report; 2016. Available at: https://www.rwjf.org/en/library/research/2016/04/using-social-determinants-of-health-data-to-improve-health-care-.html. Accessed August 31, 2020. [Google Scholar]
- [4].Centers for Medicare & Medicaid Services, Department of Health and Human Services. Medicare program; hospital inpatient prospective payment systems for acute care hospitals and the long-term care hospital prospective payment system and fiscal year 2013 rates; hospitals’ resident caps for graduate medical education payment purposes; quality reporting requirements for specific providers and for ambulatory surgical centers. Proposed rule. Fed Regist 2012;77:27870–8192.. [PubMed] [Google Scholar]
- [5].National Quality Forum. Evaluation of the NQF trial period for risk adjustment for social risk factors final report; July 18, 2017. Available at: www.qualityforum.org/Publications/2017/07/Social_Risk_Trial_Final_Report.aspx. Accessed October 8, 2018. [Google Scholar]
- [6].Yale New Haven Health Services Corporation/Center for Outcomes Research & Evaluation (YNHHSC/CORE), Lloren A, Zhou G, Liu S, et al. Assessing Hospital Disparities for Dual Eligible Patients: Thirty-Day All-Cause Unplanned Readmission Following Pneumonia Hospitalization Measure. 2018;Available at: https://www.qualitynet.org/files/5e202c5256d6a100233eeb49?filename=2018_PN_MethodDryRunReport.pdf. Accessed October 8, 2018. [Google Scholar]
- [7].Inovalon. An Investigation of Medicare Advantage Dual Eligible Member-Level Performance on CMS Five-Star Quality Measures; 2015. Available at: http://www.inovalon.com/sites/default/files/documents/INV_Duals_Study_Report_(3%2026%2015)_v1%200%201.pdf. Accessed October 8, 2018. [Google Scholar]
- [8].Gu Q, Koenig L, Faerberg J, et al. The Medicare Hospital Readmissions Reduction Program: potential unintended consequences for hospitals serving vulnerable populations. Health Serv Res 2014;49:818–37.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Centers for Medicare & Medicaid Services, Department of Health and Human Services. Hospital Compare datasets; 2018. Available at: https://data.medicare.gov/data/hospital-compare. [Google Scholar]
- [10].University of Wisconsin Population Health Institute. County Health Rankings and Roadmaps; 2018. Available at: http://www.countyhealthrankings.org/. Accessed July 30, 2018. [Google Scholar]
- [11].Morakinyo OM, Mokgobu MI, Mukhola MS, et al. Health outcomes of exposure to biological and chemical components of inhalable and respirable particulate matter. Int J Environ Res Public Health 2016;13:592.Accessed July 30, 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Swinburne M, Garfield K, Wasserman AR. Reducing hospital readmissions: addressing the impact of food security and nutrition. J Law Med Ethics 2017;45: (1_suppl): 86–9.. [DOI] [PubMed] [Google Scholar]
- [13].Rollins C, Glass NE, Perrin NA, et al. Housing instability is as strong a predictor of poor health outcomes as level of danger in an abusive relationship: findings from the SHARE Study. J Interpers Violence 2012;27:623–43.. [DOI] [PubMed] [Google Scholar]
- [14].Centers for Medicare & Medicaid Services, Department of Health and Human Services. Medicare Geographic Variation Public Use File, 2018. Available at: https://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/Medicare-Geographic-Variation/GV_PUF.html. [Google Scholar]
- [15].Oxford university press, Rothman KJ. Epidemiology: An Introduction. 2012;Accessed July 30, 2018. [Google Scholar]
- [16].Alberti PM, Lantz PM, Wilkins CH, et al. Equitable Pandemic Preparedness and Rapid Response: Lessons from COVID-19 for Pandemic Health Equity, Journal of Health Politics. Policy and Law 2020. [DOI] [PubMed] [Google Scholar]


