Small bowel (SB) capsule endoscopy (SBCE) is often perceived by both patients and physicians as a “lightweight,” noninvasive, comfortable procedure that is easily performed with little more than swallowing a pill and a glass of water. However, “easy to carry out” does not translate to ease of reading or interpretation. A SB capsule acquires thousands of images and generates a long video; however, clinically relevant findings are often seen in only a few frames. There is no way to direct or focus the camera, the capsule’s lens cannot be cleaned or luminal debris removed, and perhaps most importantly, the capsule cannot take tissue samples. Therefore, the rate of missed lesions in the SB has been quoted as high as 10 % 1 . Despite various SB imaging modalities offering similar diagnostic yield (DY) and miss rates, SBCE is one of the few endoscopic procedures open to immense scrutiny, as the data recorded are readily accessible for further on-demand review. This may expose clinicians to additional litigation but conversely, also provides a unique learning platform for new generations of SBCE readers. This is certainly fertile ground for virtual artificial neural network (ANN) training systems and even artificial intelligence (AI) diagnosis 2 . Currently, several different SBCE platforms exist. They differ in technical features and specifications such as size and weight, number and position of cameras, frame rate acquisition, and battery duration, as well as in several functions of proprietary reading software. In this editorial, we aim to provide general principles for SBCE reading, which are only partially addressed in recent technical reviews or guidelines 3 4 5 6 7 8 9 . We would also like to suggest tips and tricks to reduce common deficiencies in SBCE.
Reading capsule endoscopy: when and where
The following paragraph describes the SBCE video review process. It is crucial to point out that, as emphasized in several clinical guidelines 3 4 5 7 8 9 this is only one step of a complex diagnostic work-up. Before approaching any SBCE video, it is essential to be aware of clinical details about a patient, such as the duration of the clinical history, comorbidities, medications, and clinical presentation. Knowledge of these data allows for a thorough, focused, and fruitful SBCE revision process. It could be argued that knowing clinical data may introduce an anticipation bias, leading to overestimating the role of this procedure in the diagnostic work-up. However, knowledge of clinical data is crucial for a balanced evaluation of findings and meaningful SBCE conclusion.
Although there are obvious variations in anatomy, pathology, patient demographics, and technical specifications for each SBCE model, the capsule generally takes between 1.5 to 4 to 5 hours to cover the entire SB. This generates a video with a long run time and often prolonged sections of normal SB, which requires time, focused attention, and dedication to accurately evaluate and review 6 10 11 12 . It is a misconception that SBCE video reading is a simple task that can be undertaken as an activity performed in between other, more compelling clinical duties. In our opinion, SBCE reading should be afforded protected time and be performed as thoroughly and diligently as any other endoscopic activity. Experience can reduce SBCE reading time, however, the time allocated for review of one SBCE video should be at least 45 to 50 minutes even for an expert reader. This time slot includes short breaks, scheduled every 15 to 20 minutes, to maintain the reader’s focused attention during the reviewing process 10 11 12 .
It is fair to say that the SBCE reviewing process, especially in long and/or negative videos, can be monotonous and even tedious. However, the reader should remain vigilant to pick up even a single abnormal frame among thousands of normal frames. In our experience, the subconscious brain takes over to maximize performance, picking up subtle changes in texture or discoloration that under different circumstances, may not have been noted ( Fig. 1 ). A neutral background environment is suggested (i. e. quiet room, with adjustable/dimmable lights and possibly music) to assist concentration and minimize distraction 12 . Reading in a dim and quiet room may promote drowsiness, especially if the reading is performed at the end of a long working day. This reinforces the idea of identifying dedicated slots for SBCE reading, as a part of regular endoscopy activity. Seek advice from your occupational health team to create a proper environment, chair posture, and use of a computer monitor screen (over 21’’ is recommended), especially in high-volume services. A technique that may help to maintain focus is to keep a hand on the mouse, and a finger on the scroll wheel, as constant movements of the mouse and the fine-tuned control provided by the scroll wheel can help the reader remain constantly engaged with the video reading.
Fig. 1.
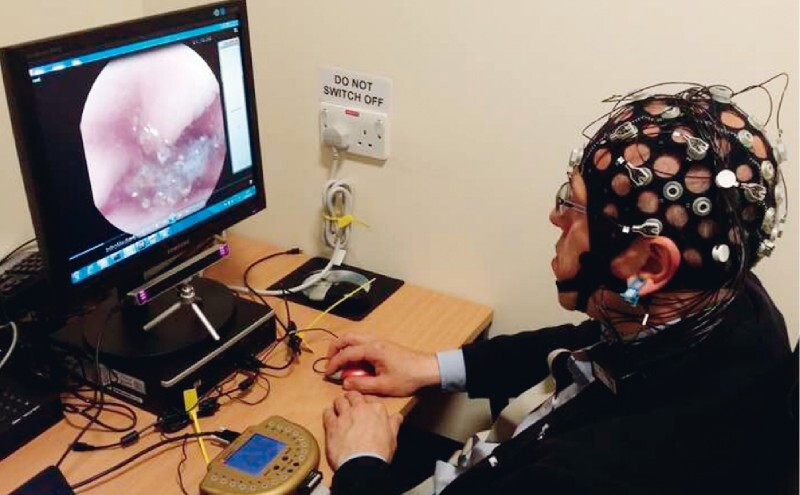
Author's unpublished work/data on eye tracking/electroencephalogram recording concentration during SBCE reading.
Basics of review & important steps in SB capsule endoscopy reading
The first step in SBCE evaluation is a quick overview of the entire video. This can be done using specifically designed, automated fast-reading modes (e. g. QuickView, TOP 100, OmniMode, Duoview etc.) 13 14 15 or manual scrolling through the video at a high frame rate (near the maximum available frame rate), the latter of which is our personal preference. This first phase is to quickly identify possible areas of interest for further detailed review, to identify key anatomical landmarks (namely the pylorus and ileocecal valve) and more importantly to gain vital clinical information quickly in relevant circumstances, e. g. investigation of gastrointestinal bleeding. Landmarking is fundamental for assessment of SB cleansing, confirmation of complete SB exploration, and lesion localization for application of standardized scoring. Following landmarking, we recommend proceeding directly to SB assessment. It is important to highlight a common issue with review speed: the capsule often resembles a “bullet train” in the proximal SB 16 , where it has been clearly demonstrated that both vascular and neoplastic lesions are most frequently located 17 , and slows down when passing though the distal SB. Therefore, regardless of the capsule model, we recommend decreasing the frame rate to 6 to 8 frames/second when inspecting the proximal SB. According to the reading protocol proposed by the European Society of Gastrointestinal Endoscopy 6 the frame rate can be increased when in the mid-distal SB. However, we suggest that readers avoid high frame rates (e. g. 16–20 frames/sec) in almost every SB segment, otherwise identification of minimal changes may be impossible even for an expert reader.
Use of dual-frame review for most frontal-view capsules has been widely adopted 6 , but novice readers may wish to continue using the single frame mode or adopting a more personal style, should they wish, especially if it allows them to focus and enjoy the review. When reviewing the SB, we strongly advise saving any relevant findings to create a case library that can be reviewed quickly and easily; ( Fig. 2 ). The second review should focus on comparing the saved thumbnails and relevant short video sections. Due to the propulsive activity of the SB, capsules often move bi-directionally, therefore, the same lesion or anomaly may appear several times; running through the library may also help estimate the number and location of findings. Each selected thumbnail should be compared with software-embedded Atlas images and with results of previous studies performed in the same center. The relevant ones should be annotated using dedicated classification or scoring systems (e. g. Niv score, Lewis score, CECDAI [Capsule Endoscopy Crohnʼs Disease Activity Index](, Saurin classification, SPICE [smooth, protruding lesion index on capsule endoscopy] score) 18 19 20 21 . The overall clinical evaluation of a SB video and report results from the combined evaluation of annotated thumbnails. Before finalizing the report, we suggest systematically checking the stomach and the colon, even if the capsule system in use is not designed for other gastrointestinal segments, as obvious gastric and colonic lesions overlooked on initial gastroscopy and colonoscopy may be discovered in 7 % to 15 % (up to 30 % in some reports) of patients 22 . This is particularly important in cases where evaluation of the SB is negative.
Fig. 2.
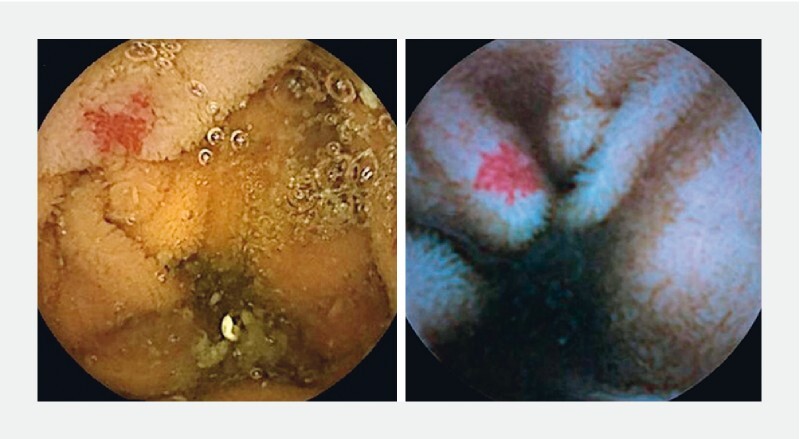
SBCE images of an angiectasia under white light (left; PillCamSB3) and Blue Mode reading (right; PillCamSB2).
In addition, we suggest a “think twice” policy in negative SB exams; we recommend that the same reviewer, or where possible, a second, more experienced reviewer, repeat the complete review process. Last but not least, standardization is required and every report should contain quantifiable information. For this purpose, we suggest following the SAVER acronym; Specification of protrusions (i. e. SPICE score for masses/bulges) 18 , Assessment of a lesions (especially angiectasias) bleeding potential (i. e. through the Saurin score) 19 , eValuation of inflammatory activity (e. g. by Lewis or CECDAI cores) 20 21 , Estimate of location of important lesions 23 , and Recording of bowel/image cleanliness ( Table 1 ) 24 .
Table 1. SAVER acronym for memory aid for capsule endoscopy report checklist.
| S | PICE any protrusion(s); Girelli index (mass of bulge) |
| A | ssess lesion(s) potential for bleeding (Saurin Score) |
| V | aluate inflammation (Lewis score or CECDAI) |
| E | estimate the location of important lesion(s)/finding(s) (Li score) |
| R | ecord image & overall video cleanliness |
SPICE, smooth, protruding lesion index on capsule endoscopy; CECDAI, Capsule Endoscopy Crohn's Disease Activity Index.
How to shorten video reading times
Because SBCE reading is time-consuming, several options have been evaluated to save time without compromising lesion detection rate. The more obvious way to shorten reading time is to simply increase the reading frame rate. However, the impact of this approach on lesion detection is still unclear. While some studies have demonstrated low miss rates, we believe that increasing reading frame speed may lead to diagnostic error. Capsule manufacturers have introduced different software image analysis systems to automatically select or highlight relevant images and eliminate sequential images which are similar and redundant 13 14 15 . These systems can reduce reading time by up to 50 % with a very low diagnostic miss rate; in our opinion, although they cannot substitute for a thorough video reading, they might represent a valid form of support. Similarly, automatic systems for selection of frames containing blood (or red areas) have been developed, which may show some promise in patients with suspected small bowel bleeding, but relevant frames can still be missed. Currently, we cannot rely heavily on these tools in the SBCE reading process. In addition, because capsule images are not of high resolution when compared to conventional endoscopes, any image enhancement tool (e. g. Fujinon Intelligent Chromo Endoscopy-FICE, and Blue Mode for PillCam, Augmented Live-body Image Color spectrum Enhancement-ALICE for Mirocam, Advanced Color Enhancement-ACE for CapsoCam etc.,) is welcome 25 . Currently available image enhancement tools seem to allow for slightly more accurate characterization of observed lesions, but they do not significantly improve the detection rate of clinically relevant lesions.
Ultimately, we believe that although SBCE is a highly technical tool, the most effective way to shorten reading times while maintaining accuracy and effectiveness is strictly linked to reader competency. Although expertise in upper and lower gastrointestinal endoscopy is necessary prerequisite 9 26 27 , SBCE has specific technical features that make it different from other endoscopy techniques (e. g. underwater view, non-distended lumen, tangential non-adjustable view, back-and-forth capsule movements etc.). Therefore, even experienced endoscopists still require dedicated training. However, SBCE training is currently not standardized, differing widely between countries and institutions 26 27 and the definition of competency has not yet been universally established. Several clinical researchers have evaluated the number of SBCE procedures needed to obtain reading privileges. The Korean Gut Study Group and the American Society for Gastrointestinal Endoscopy define 10 and 25 SBCE readings, respectively, as thresholds for defining competency 9 ; however, more recent well-designed studies using SBCE assessment tools conclude that basic competency can be obtained after 20 to 25 supervised videos. Advanced competency may require a more comprehensive training curriculum. Experience is a relative point in SBCE reading, and further exposure to a larger volume of reviewed SBCEs not only reduces reading time but also improves identification of subtle mucosal changes. However, even more important than a threshold number of SBCEs for achieving and maintaining competency is participation in a dedicated SB multidisciplinary working group. Only through continuous collaboration with specialists who perform other dedicated SB diagnostics or therapeutics can SBCE readers improve their ability to evaluate the lesions identified, for example, in estimating size and location. Ideally, SBCE readers should also be involved in device-assisted enteroscopy procedures (or at least see some of them). This helps to bridge the gap between wired and wireless endoscopy, ensuring a continuous reappraisal process that eventually improves SBCE reading. Participating in dedicated meetings in which findings or cases can be discussed with experts or in a peer-to-peer setting may also be helpful in maintaining competency.
Table 2 lists 10 tips and tricks for an effective capsule endoscopy reading process.
Table 2. Ten tips and tricks for an effective SBCE reading.
| 1. | Get your training sorted! Achieving competency before starting SBCE reading is mandatory and maintaining proficiency thereafter is vital |
| 2. | Avoid CE reading if you are tired; it is a long and tough process requiring focused attention |
| 3. | Avoid CE reading in between other gastrointestinal procedures or tasks; instead, set up dedicated reading slots (45–60 min each) |
| 4. | Set up an inspiring and dedicated SBCE reading environment, i. e. quiet room with dimmable lights, big-sized screen etc. |
| 5. | Collect as much clinical data as possible before SBCE reading; you are not just describing findings; you are also participating in a diagnostic process |
| 6. | Follow a predefined sequence; pre-reading, landmarking, findings & clips selection and reporting; don’t forget to check gastrointestinal segments outside the SB |
| 7. | Slow down, whether you are an expert or a novice reader, and consider a slower reading speed in the proximal SB. Avoid high (e. g. 18–20 fps) speeds |
| 8. | Be proactive; move through the video and compare images or findings to other videos, online resources or in-print libraries |
| 9. | Set up a SB multidisciplinary team and whenever possible compare your findings with the results of other diagnostic procedures (e. g. device-assisted enteroscopy, surgery, radiology imaging). It is critical to reappraise both morphology and clinical relevance of SBCE findings |
| 10. | Enjoy reading CE or relinquish the task |
SBCE, small bowel capsule endoscopy; CE: capsule endoscopy.
Conclusion
In light of recent advances, and the unique nature of SBCE, we can expect an acceleration in technology. AI systems offer the ability to extract only relevant points of interest from the thousands of images generated and provide a preliminary report – much like current electrocardiogram machines 28 . Until that time, training and expert guidance remain the cornerstone for competent clinical evaluation of SBCE videos.
Acknowledgement
The authors thank Dr. Alex Robertson for the thorough language review and essential editorial support.
Footnotes
Competing interests Dr. Pennazio has received honoraria from Olympus and Medtronic. Dr. Toth has received honoraria and/or travel support from Olympus, Medtronic, Norgine and Ambu. Dr. Koulaouzidis has received material support for research from SynMed UK, IntroMedic and Aquilant; he also received the 2011 ESGE-Given Imaging Ltd research grant. He has received honoraria and/or travel support from Dr Falk Pharma, Jinshan, Ferring Pharmaceuticals UK and Norgine and has been on the advisory boards for Dr Falk Pharma UK, Tillotts Pharma, IntroMedic. Dr Koulaouzidis also is cofounder of AJM Med-i-Caps.
References
- 1.Lewis B S, Eisen G M et al. A pooled analysis to evaluate results of capsule endoscopy trials. Endoscopy. 2005;37:960–965. doi: 10.1055/s-2005-870353. [DOI] [PubMed] [Google Scholar]
- 2.Leenhardt R, Vasseur P, Li C et al. CAD-CAP Database Working Group. A neural network algorithm for detection of GI angioectasia during small-bowel capsule endoscopy. Gastrointest Endosc. 2019;89:189–194. doi: 10.1016/j.gie.2018.06.036. [DOI] [PubMed] [Google Scholar]
- 3.Pennazio M, Spada C, Eliakim R et al. Small-bowel capsule endoscopy and device-assisted enteroscopy for diagnosis and treatment of small-bowel disorders: European Society of Gastrointestinal Endoscopy (ESGE) Clinical Guideline. Endoscopy. 2015;47:352–376. doi: 10.1055/s-0034-1391855. [DOI] [PubMed] [Google Scholar]
- 4.Yamamoto H, Ogata H, Matsumoto T et al. Clinical Practice Guideline for Enteroscopy. Dig Endosc. 2017;29:519–546. doi: 10.1111/den.12883. [DOI] [PubMed] [Google Scholar]
- 5.Gerson L B, Fidler J L, Cave D R et al. ACG Clinical Guideline: Diagnosis and Management of Small Bowel Bleeding. Am J Gastroenterol. 2015;110:1265–1287. doi: 10.1038/ajg.2015.246. [DOI] [PubMed] [Google Scholar]
- 6.Rondonotti E, Spada C, Adler S et al. Small-bowel capsule endoscopy and device-assisted enteroscopy for diagnosis and treatment of small-bowel disorders: European Society of Gastrointestinal Endoscopy (ESGE) Technical Review. Endoscopy. 2018;50:423–446. doi: 10.1055/a-0576-0566. [DOI] [PubMed] [Google Scholar]
- 7.Enns R A, Hookey L, Armstrong D et al. Clinical practice guidelines for the use of video capsule endoscopy. Gastroenterology. 2017;152:497–514. doi: 10.1053/j.gastro.2016.12.032. [DOI] [PubMed] [Google Scholar]
- 8.Oliva S, Thomson M, de Ridder L et al. Endoscopy in Pediatric Inflammatory Bowel Disease: A Position Paper on Behalf of the Porto IBD Group of the European Society for Pediatric Gastroenterology, Hepatology and Nutrition. J Pediatr Gastroenterol Nutr. 2018;67:414–430. doi: 10.1097/MPG.0000000000002092. [DOI] [PubMed] [Google Scholar]
- 9.ASGE . Faigel D O, Baron T H, Adler D G. ASGE guideline: guidelines for credentialing and granting privileges for capsule endoscopy. Gastrointest Endosc. 2005;61:503–505. doi: 10.1016/s0016-5107(04)02781-6. [DOI] [PubMed] [Google Scholar]
- 10.Lo S. How should we do capsule endoscopy reading? Tech Gastroint Endosc. 2006;8:146–148. [Google Scholar]
- 11.Barkin J A, Barkin J S. Video capsule endoscopy teaching, reading and troubleshooting. Gastrointest Clin N Am. 2017;27:15–27. doi: 10.1016/j.giec.2016.08.002. [DOI] [PubMed] [Google Scholar]
- 12.Lewis S B. How to read capsule endoscopy images. Gastrointest Clin N Am. 2004;14:11–26. doi: 10.1016/j.giec.2003.11.001. [DOI] [PubMed] [Google Scholar]
- 13.Freitas M, Arieira C, Carvalho P B et al. Simplify to improve in capsule endoscopy - top 100 is a swift and reliable evaluation tool for the small bowel inflammatory activity in Crohnʼs disease. Scand J Gastroenterol. 2020;55:408–413. doi: 10.1080/00365521.2020.1745880. [DOI] [PubMed] [Google Scholar]
- 14.Saurin J C, Lapalus M G, Cholet F et al. Can we shorten the small-bowel capsule reading time with the “Quick-view” image detection system. Dig Liver Dis. 2012;44:477–581. doi: 10.1016/j.dld.2011.12.021. [DOI] [PubMed] [Google Scholar]
- 15.Gomes C, Pinho R, Ponte A et al. Evaluation of the sensitivity of the Express View ® in the Mirocam capsule endoscopy software . Scand J Gastroenterol. 2020;55:371–375. doi: 10.1080/00365521.2020.1734650. [DOI] [PubMed] [Google Scholar]
- 16.Worsoe J, Fynne L, Gregersen T et al. Gastric transit and small bowel transit time and motility assessed by a magnet tracking system. BMC Gastroenterol. 2011;29:145. doi: 10.1186/1471-230X-11-145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Davie M, Yung D E, Douglas S et al. Mapping the distribution of small bowel angioectasias. Scand J Gastroenterol. 2019;54:597–602. doi: 10.1080/00365521.2019.1608293. [DOI] [PubMed] [Google Scholar]
- 18.Girelli C M, Porta P, Colombo E et al. Development of a novel index to discriminate bulge from mass on small bowel capsule endoscopy. Gastrointest Endosc. 2011;74:1067–1074. doi: 10.1016/j.gie.2011.07.022. [DOI] [PubMed] [Google Scholar]
- 19.Saurin J C, Delvaux M, Vahedi K et al. Clinical impact of capsule endoscopy compared to push enteroscopy: 1-year follow-up study. Endoscopy. 2005;37:318–323. doi: 10.1055/s-2005-861114. [DOI] [PubMed] [Google Scholar]
- 20.Gralnek I M, Defranchis R, Seidman E et al. Development of a capsule endoscopy scoring index for small bowel mucosal inflammatory change. Aliment Pharmacol Ther. 2008;27:146–154. doi: 10.1111/j.1365-2036.2007.03556.x. [DOI] [PubMed] [Google Scholar]
- 21.Gal E, Geller A, Fraser G et al. Assessment and validation of the new capsule endoscopy Crohnʼs disease activity index (CECDAI) Dig Dis Sci. 2008;53:1933–1937. doi: 10.1007/s10620-007-0084-y. [DOI] [PubMed] [Google Scholar]
- 22.Koffas A, Laskaratos F M, Epstein O. Non-small bowel lesion detection at small bowel capsule endoscopy: a comprehensive literature review. World J Clin Cases. 2018;6:901–907. doi: 10.12998/wjcc.v6.i15.901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Li X, Chen H, Dai J et al. Predictive role of capsule endoscopy on the insertion route of double-balloon enteroscopy. Endoscopy. 2009;41:762–766. doi: 10.1055/s-0029-1215009. [DOI] [PubMed] [Google Scholar]
- 24.Ponte A, Pinho R, Rodrigues A et al. Review of small-bowel cleansing scales in capsule endoscopy: A panoply of choices. World J Gastrointest Endosc. 2016;8:600–609. doi: 10.4253/wjge.v8.i17.600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Yung D E, Boal Carvalho P, Giannakou A et al. Clinical validity of flexible spectral imaging color enhancement (FICE) in small-bowel capsule endoscopy: a systematic review and meta-analysis. Endoscopy. 2017;49:258–269. doi: 10.1055/s-0042-122015. [DOI] [PubMed] [Google Scholar]
- 26.Read A J, Rice M D, Conjeevaram H S et al. A deeper look at the small bowel: training pathways in video capsule endoscopy and device-assisted enteroscopy. Dig Dis Sci. 2018;63:2210–2219. doi: 10.1007/s10620-018-5133-1. [DOI] [PubMed] [Google Scholar]
- 27.Koffas A, Laskaratos F M, Epstein O. Training in video capsule endoscopy: current status and unmet needs. World J Gastrointest Endosc. 2019;11:395–402. doi: 10.4253/wjge.v11.i6.395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Iakovidis D K, Koulaouzidis A. Automatic lesion detection in capsule endoscopy based on color saliency: closer to an essential adjunct for reviewing software. Gastrointest Endosc. 2014;80:877–883. doi: 10.1016/j.gie.2014.06.026. [DOI] [PubMed] [Google Scholar]


