Abstract
Background
There is limited information on the clinical characteristics of patients with coronavirus disease 2019 (COVID-19) who are asymptomatic or have mild symptoms.
Methods
We performed a retrospective case series of patients with COVID-19 enrolled from February 22 to March 26, 2020. Forty cases of COVID-19 were confirmed using real-time reverse-transcription polymerase chain reaction among patients who underwent screening tests and were consecutively hospitalized at Ulsan University Hospital, Ulsan, Korea. The final follow-up date was May 19, 2020. All COVID-19 cases in Ulsan were included. Demographic and epidemiological information, comorbidities, clinical signs and symptoms, laboratory and radiologic findings, medications, treatments, outcomes, and main durations of patients with COVID-19 were compared according to supplemental oxygen requirement.
Results
Forty patients were included (median age, 30 years; interquartile range [IQR], 25–57 years; 58% female). Six (15%) patients required supplemental oxygen. The prevalence of asymptomatic severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) infection was 5% and that of presymptomatic infection was 13%. Cough, fever, myalgia, rhinorrhea or nasal congestion, and diarrhea were the screening criteria for diagnosing symptomatic and presymptomatic SARS-CoV-2 infections. Sputum production, chest discomfort, a large number of symptoms, abnormal procalcitonin and C-reactive protein levels, and abnormal chest X-ray or chest computed tomography findings were more common in patients requiring supplemental oxygen than in those not requiring supplemental oxygen. Overall mortality rate was 3% (1/40). Four patients (10%) were readmitted after testing positive by reverse-transcription polymerase chain reaction again. Incubation period was 5 days (IQR, 4–6 days), and the duration of viral shedding was 21 days (IQR, 14–28 days; maximum, 51 days).
Conclusion
The prevalence of asymptomatic SARS-CoV-2 infection was 5%, which is much lower than that previously reported. This finding suggests that careful interviews and follow-ups should be performed to identify SARS-CoV-2 infections. Cough, fever, myalgia, rhinorrhea or nasal congestion, and diarrhea are adequate screening criteria for covering all symptoms of SARS-CoV-2 infection. Further evaluation is required to create representative screening criteria for COVID-19.
Keywords: Prevalence, Asymptomatic, COVID-19, SARS-CoV-2, Korea
Graphical Abstract
INTRODUCTION
At the end of 2019, a novel coronavirus was identified as the cause of a cluster of pneumonia cases in Wuhan, China.1 It rapidly spread, resulting in an epidemic throughout China, followed by an explosion of cases in most countries worldwide. The World Health Organization (WHO) characterized coronavirus disease 2019 (COVID-19) as a pandemic.2 As of July 12, 2020, over 12 million confirmed cases including over 0.5 million deaths had been documented globally.3
The understanding of COVID-19 is continuously evolving. However, the known information focuses on inpatients with severe conditions or residents in specific environments, whereas information on asymptomatic patients or those with mild symptoms and residents in the community is limited.1,4,5,6,7
Ulsan is Korea's seventh-largest metropolitan city with over 1.1 million inhabitants. On February 22, 2020, the first confirmed case of COVID-19 was reported in Ulsan, and by April 26, there were 40 cases. Most COVID-19 patients in Ulsan had mild symptoms or were asymptomatic and were detected by screening individuals suspected of being exposed to severe acute respiratory syndrome coronavirus-2 (SARS-CoV2). For public health purposes, all COVID-19 cases confirmed in this city were admitted to a designated hospital, i.e., Ulsan University Hospital (UUH; Ulsan, Korea), regardless of the disease severity. Therefore, the evaluation of COVID-19 patients at UUH will likely provide information about mild or asymptomatic COVID-19 patients in the community.
We analyzed the clinical characteristics of all consecutively hospitalized COVID-19 patients at UUH.
METHODS
Study design
This retrospective case series was conducted at UUH, the largest teaching hospital in Ulsan.
Study patients
All patients were Korean residents of Ulsan and were diagnosed with COVID-19 by real-time reverse transcription-polymerase chain reaction (RT-PCR) for SARS-CoV-2. Among the 40 patients, 38 were confirmed at 10 screening centers in Ulsan and 2 at 2 screening centers in other cities and referred by the respective centers. The screening test for SARS-CoV2 was obligatory for families or those in close contacts with confirmed COVID-19 patients in Korea. Patients were admitted to UUH between February 22, 2020, and March 26, 2020. Clinical outcomes were monitored until May 19, 2020, the date when the last patient was discharged.
Data sources and variables
Demographic, clinical, and laboratory variables were collected from the clinical data warehouse platform in conjunction with the electronic medical records at the UUH Information of Clinical Ecosystem, and the authors manually reviewed these medical records. Additionally, we referred to epidemiological and clinical data identified by a preventive medicine specialist who interviewed the patients at the UUH and another source of epidemiological data for Ulsan. Transfers from UUH to a local hospital were merged and considered a single visit. Regarding patients who were readmitted during the study period, data from the first admission were considered. Data were collected on demographic characteristics (age, sex, occupation, education, and religion), epidemiological information, triage vitals (blood pressure, heart rate, temperature, respiratory rate, and peripheral oxygen saturation), comorbidities (hypertension, diabetes, dyslipidemia, cardiovascular disease, cancer, and hepatitis B infection), history of clinical signs and symptoms, laboratory and radiologic findings, medications (antiviral therapy and antimalarial therapy), treatments (continuous renal replacement therapy and invasive mechanical ventilation), outcomes (discharge, readmission, and mortality), and main durations (incubation period, symptom onset to hospital admission, viral shedding, and hospital stay). We calculated the Modified Early Warning Score (MEWS)8,9 and CURB-6510,11,12 pneumonia severity score. MEWS is based on systolic blood pressure, heart rate, respiratory rate, temperature, and consciousness, whereas CURB-65 is based on confusion, urea levels, respiratory rate, blood pressure, and ≥ 65 years. Fever was defined as a temperature of ≥ 37.5°C or subjective fever before admission and a temperature of ≥ 37.5°C in axillary measurements obtained after admission. Laboratory and radiologic findings were considered from the first test results available, typically within 24 hours of admission. When all symptoms and signs, radiologic findings, and laboratory findings of COVID-19 subsided and two consecutive negative results for SARS-CoV-2 infection were reported, the patient was considered recovered from COVID-19 and was discharged. If a patient had persistent positive SARS-CoV-2 test results and the other parameters were normalized, the patient was referred to a local hospital specified for Ulsan and hospitalized until negative results were obtained in two consecutive SARS-CoV-2 tests.
Real-time RT-PCR for SARS-CoV-2
During hospitalization, respiratory tract specimens including sputum and nasopharyngeal or oropharyngeal swab samples were collected to detect SARS-CoV-2 on different dates. After viral RNA extraction with the NX-48 viral nucleic acid extraction kit (Genolution, Seoul, Korea) in conjunction with Nextractor NX-48 (Genolution), real-time RT-PCR was performed using the PowerChek™ 2019-nCoV Real-Time PCR Kit (KogeneBiotech, Seoul, Korea) with the Bio-Rad CFX96 Deep Well Real-Time PCR Detection System (Bio-Rad, Hercules, CA, USA). This assay targets two genes (E: for Sarbecovirus screening and RdRp for confirmation of SARS-CoV-2), as suggested by the Korea Centers for Disease Control and Prevention and WHO.13
Symptoms and signs
We created a list of symptoms from previous COVID-19 studies.4,5,6,14,15 Patients were classified as symptomatic if they had fever, cough, sputum production, sore throat, myalgia, headache, chills, rhinorrhea or nasal congestion, chest discomfort, shortness of breath, fatigue, anorexia, diarrhea, nausea or vomiting, or dry mouth for the duration from suspected exposure to SARS-CoV-2 to hospital admission. Presymptomatic patients were defined as those who had no symptoms before admission but developed symptoms during admission. Asymptomatic patients were those who had no symptoms at any time for the duration from suspected exposure to SARS-CoV-2 to hospital discharge.
Main durations
The incubation period was estimated based on the date of estimated exposure to SARS-CoV-2 to the date of symptom onset. Patients who were asymptomatic or symptomatic without the exact dates of exposure to SARS-CoV-2 or symptom onset known were excluded from this analysis. The duration from symptom onset to hospital admission was analyzed in symptomatic patients. Patients who were asymptomatic, presymptomatic, or symptomatic without the exact date of symptom onset known were excluded. To estimate the duration of viral shedding, we defined the date of nucleic acid conversion as the median of the date of the last positive real-time RT-PCR test result and the date of the first negative real-time RT-PCR test because real-time RT-PCR was not performed daily. The test intervals ranged from 1 to 7 days according to patient conditions. Therefore, the duration of viral shedding was calculated by subtracting the date of symptom onset from the median of the date of the last positive real-time RT-PCR test result and the date of the first negative real-time RT-PCR test result. Patients who were asymptomatic or symptomatic without the exact date of symptom onset known were also excluded. Duration of hospital stay was calculated by subtracting the date of admission from the date of discharge. Concerning patients who were readmitted, the durations of viral shedding and hospital stay were defined according to the real-time RT-PCR result at the first admission.
Statistical analysis
The study subjects were grouped by whether supplemental oxygen was required. We present continuous variables as median and interquartile range (IQR) and categorical variables as counts (%). The medians of continuous variables were compared using the Mann–Whitney U test. Proportions for categorical variables were compared using Fisher's exact test. We used Stata (version 13; StataCorp, College Station, TX, USA) for these analyses. For unadjusted comparisons, a two-sided α-value of < 0.05 was considered statistically significant. These analyses were not adjusted for multiple comparisons; given the potential for type I error, the findings should be interpreted as exploratory and descriptive.
Ethics statement
The UUH Institutional Review Board (IRB) approved this study as minimal-risk research because it used data collected for routine clinical practice and waived the requirement for informed consent (IRB File No. 2020-03-030).
RESULTS
In this study, we included 40 patients (median age, 30 years [IQR, 25–57]; 58% female) (Table 1). Six (15%) patients required supplemental oxygen, which was supplied when peripheral oxygen saturation (SpO2) was < 90%. Among the six patients, five began receiving supplemental oxygen 1–14 days after admission and one began receiving supplemental oxygen on admission. The patients requiring supplemental oxygen were generally older (64 [IQR, 60–68] vs. 29 [IQR, 24–49] years) and more likely to have comorbidities (80% vs. 9%) than those not requiring supplemental oxygen. Further, 25 (63%) patients had been exposed to SARS-CoV-2, 4 (10%) had visited an endemic area in Korea, and 9 (23%) were imported cases. Three patients (8%) were febrile, two (5%) had a respiratory rate of > 20 breaths/min, and two (5%) had SpO2 levels of < 95% on admission.
Table 1. Baseline characteristics of the COVID-19 patients on admission.
| Characteristics | All patients (n = 40) | Supplemental | P value | |||
|---|---|---|---|---|---|---|
| Oxygen not required (n = 34) | Oxygen required (n = 6) | |||||
| Age, yr | 30 (25–57) | 29 (24–49) | 64 (60–68) | < 0.001 | ||
| Range | 0.002 | |||||
| ≤ 29 | 17 (43) | 17 (50) | 0 | |||
| 30–64 | 19 (47) | 16 (47) | 3 (50) | |||
| ≥ 65 | 4 (10) | 1 (2) | 3 (50) | |||
| Sex | 1.000 | |||||
| Female | 23 (57) | 19 (56) | 4 (67) | |||
| Male | 17 (43) | 15 (44) | 2 (33) | |||
| BMI, kg/m2 (n = 36) | 23.2 (21.5–26.5) | 23.2 (21.5–26.6) | 23.2 (21.8–25.2) | 0.945 | ||
| Range | 1.000 | |||||
| Normal, < 22.9 | 15 (42) | 13 (42) | 2 (40) | |||
| Overweight, 23.0–24.9 | 10 (28) | 9 (29) | 1 (20) | |||
| Obese, ≥ 25.0 | 11 (30) | 9 (29) | 2 (40) | |||
| Occupation | 0.453 | |||||
| Professionals | 3 (8) | 2 (6) | 1 (17) | |||
| Clerks | 8 (20) | 7 (21) | 1 (17) | |||
| Service workers | 4 (10) | 4 (12) | 0 | |||
| Sales workers | 2 (5) | 2 (6) | 0 | |||
| Craft workers | 3 (8) | 3 (9) | 0 | |||
| Housewives | 8 (20) | 5 (15) | 3 (50) | |||
| Students | 8 (20) | 8 (24) | 0 | |||
| Inoccupation | 4 (10) | 3 (9) | 1 (17) | |||
| Education, yr | 0.007 | |||||
| ≤ 9 | 4 (10) | 1 (3) | 3 (50) | |||
| 10–12 | 13 (33) | 11 (32) | 2 (33) | |||
| ≥ 13 | 23 (57) | 22 (65) | 1 (17) | |||
| Religion | 0.570 | |||||
| Christianity | 8 (20) | 7 (21) | 1 (17) | |||
| Buddhism | 6 (15) | 4 (12) | 2 (33) | |||
| Atheism | 14 (35) | 12 (35) | 2 (33) | |||
| Shincheonjia | 12 (30) | 11 (32) | 1 (17) | |||
| Exposure to source of transmission | 0.216 | |||||
| Linked to Shincheonjib | 25 (63) | 21 (62) | 4 (66) | |||
| Attendee | 12 (30) | 12 (35) | 0 | |||
| Attendee's family | 13 (33) | 9 (26) | 4 (66) | |||
| Recently visited Daeguc | 4 (10) | 3 (9) | 1 (17) | |||
| Linked to imported cases | 9 (23) | 8 (24) | 1 (17) | |||
| Othersa | 2 (5) | 2 (6) | 0 | |||
| Systolic blood pressure, mmHg | 135 (120–146) | 135 (119–148) | 137 (131–142) | 0.895 | ||
| Diastolic blood pressure, mmHg | 86 (78–89) | 86 (78–89) | 81 (77–86) | 0.271 | ||
| Heart rate, beats/min | 90 (81–98) | 90 (80–98) | 89 (82–96) | 0.940 | ||
| ≥ 100 | 7 (18) | 6 (18) | 1 (17) | 0.721 | ||
| Temperature, °C | 36.5 (36.3–36.8) | 36.4 (36.3–36.8) | 36.6 (36.4–37.0) | 0.311 | ||
| ≥ 37.5 | 3 (8) | 2 (6) | 1 (17) | 0.394 | ||
| Respiratory rate, breaths/min | 20 (18–20) | 20 (18–20) | 19 (18–20) | 0.704 | ||
| > 20 | 2 (5) | 1 (3) | 1 (17) | 0.281 | ||
| SpO2, % (n = 39) | 98 (97–99) | 98 (98–99) | 96 (94–96) | 0.004 | ||
| < 95% | 2 (5) | 0 | 2 (33) | 0.020 | ||
| MEWS | 0.410 | |||||
| 1 | 31 (77) | 27 (79) | 4 (66) | |||
| 2 | 5 (13) | 4 (12) | 1 (17) | |||
| 3 | 4 (10) | 3 (9) | 1 (17) | |||
| CURB-65d | 0.208 | |||||
| 0 | 22 (55) | 19 (56) | 3 (50) | |||
| 1 | 17 (42) | 15 (44) | 2 (33) | |||
| 2 | 1 (3) | 0 | 1 (17) | |||
| Smoking | 0.284 | |||||
| Never | 35 (87) | 31 (91) | 4 (67) | |||
| Formal | 4 (10) | 2 (6) | 2 (33) | |||
| Current | 1 (3) | 1 (3) | 0 | |||
| Alcohol consumption, g/wk | 1.000 | |||||
| < 100 | 36 (90) | 30 (88) | 6 (100) | |||
| ≥ 100 | 4 (10) | 4 (12) | 0 | |||
| Comorbidities | ||||||
| Any | 7 (18) | 3 (9) | 4 (80) | < 0.001 | ||
| Hypertension | 2 (5) | 0 | 2 (33) | 0.019 | ||
| Type 2 diabetes | 2 (5) | 0 | 2 (33) | 0.019 | ||
| Dyslipidemia | 5 (13) | 1 (3) | 4 (67) | 0.001 | ||
| Cardiovascular disease | 1 (3) | 0 | 1 (17) | 0.150 | ||
| Malignancy | 1 (3) | 0 | 1 (17) | 0.150 | ||
| Hepatitis B infection | 1 (3) | 1 (3) | 0 | 1.000 | ||
Data are presented as median (interquartile range) or number (%).
COVID-19 = coronavirus disease 2019, BMI = body mass index, SpO2 = peripheral oxygen saturation, MEWS = modified early warning score.
aTwo patients had contact with an individual suspected with COVID-19; bAn offshoot Christian new religious movement established in Korea; cThe center of Korea's coronavirus outbreak; dCURB-65 is a community-acquired pneumonia severity score based on confusion, urea levels (> 7 mmol/L), respiratory rate (≥ 30 breaths/min), blood pressure (systolic blood pressure < 90 mmHg or diastolic blood pressure ≤ 60 mmHg), and age (≥ 65 years).
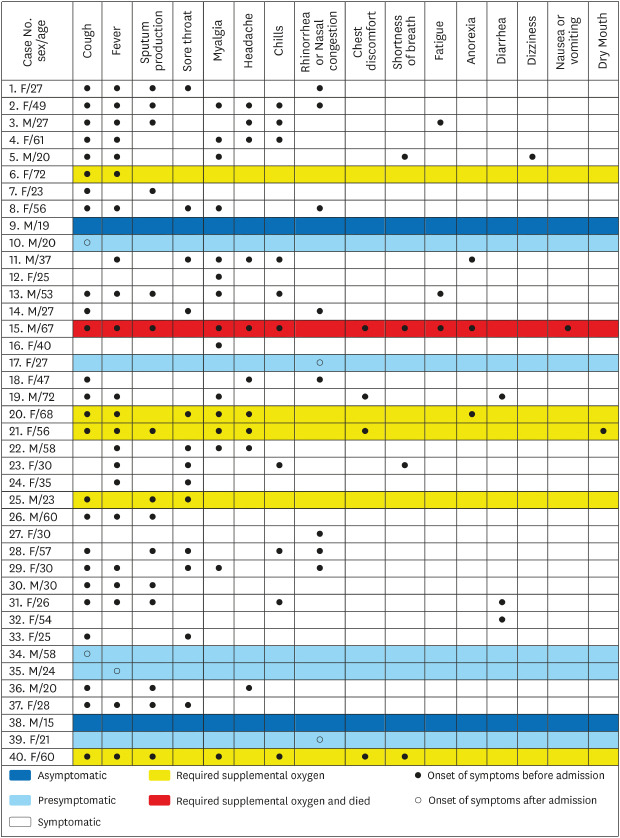
Signs and symptoms
Table 2 and the Fig. 1 summarize patient signs and symptoms. Among the 40 patients, 33 (83%) were symptomatic, 5 (13%) were presymptomatic, and 2 (5%) were asymptomatic. The most common symptoms were cough (68%) and fever (55%). Sputum production, sore throat, headache, chills, chest discomfort, shortness of breath, fatigue, anorexia, dizziness, and dry mouth existed with cough or fever. Conversely, myalgia, rhinorrhea or nasal congestion, or diarrhea was the only symptom in five patients. Sputum production and chest discomfort were more common in patients requiring supplemental oxygen than in those not requiring supplemental oxygen (83% vs. 32% for sputum production and 50% vs. 3% for chest discomfort, respectively). More symptoms were present in patients requiring supplemental oxygen than in those not requiring supplement oxygen (7 [IQR, 3–7] vs. 3 [IQR, 1–5]).
Table 2. Patient symptoms for the entire duration from suspected exposure to SARS-CoV-2 to hospital discharge.
| Symptoms | All patients (n = 40) | Supplemental | P value | ||
|---|---|---|---|---|---|
| Oxygen not required (n = 34) | Oxygen required (n = 6) | ||||
| Cough | 27 (68) | 21 (62) | 6 (100) | 0.152 | |
| Fevera | 22 (55) | 17 (50) | 5 (83) | 0.197 | |
| Sputum production | 16 (40) | 11 (32) | 5 (83) | 0.029 | |
| Sore throat | 14 (35) | 13 (38) | 1 (17) | 0.399 | |
| Myalgia | 15 (38) | 11 (32) | 4 (67) | 0.174 | |
| Headache | 11 (28) | 8 (24) | 3 (50) | 0.319 | |
| Chills | 11 (28) | 9 (27) | 2 (33) | 1.000 | |
| Rhinorrhea or nasal congestion | 9 (23) | 9 (27) | 0 | 0.306 | |
| Chest discomfort | 4 (10) | 1 (3) | 3 (50) | 0.008 | |
| Shortness of breath | 4 (10) | 2 (6) | 2 (33) | 0.100 | |
| Fatigue | 3 (8) | 2 (6) | 1 (17) | 0.394 | |
| Anorexia | 3 (8) | 1 (3) | 2 (33) | 0.054 | |
| Diarrhea | 3 (8) | 3 (9) | 0 | 1.000 | |
| Dizziness | 1 (3) | 1 (3) | 0 | 1.000 | |
| Nausea or vomiting | 1 (3) | 0 | 1 (17) | 0.150 | |
| Dry mouth | 1 (3) | 0 | 1 (177) | 0.150 | |
| No. of symptoms | 3 (1–6) | 3 (1–5) | 7 (3–7) | 0.026 | |
| Symptom status | 0.691 | ||||
| Symptomatic | 33 (83) | 27 (79) | 6 (100) | ||
| Presymptomatic | 5 (13) | 5 (15) | 0 | ||
| Asymptomatic | 2 (5) | 2 (6) | 0 | ||
Data are presented as number (%) or number (interquartile range).
SARS-CoV-2 = severe acute respiratory syndrome coronavirus-2.
aFever was measured as a temperature of ≥ 37.5°C or subjective fever before admission and a temperature of ≥ 37.5°C in axillary measurements after admission.
Fig. 1. Symptoms of the 40 COVID-19 patients.
COVID-19 = coronavirus disease 2019, F = female, M = male.
Laboratory and radiologic findings
Abnormal procalcitonin and C-reactive protein (CRP) levels were more commonly observed in patients requiring supplemental oxygen than in those not requiring supplemental oxygen (Table 3). The patient who died had the highest procalcitonin and CRP levels. Six (15%) patients had abnormal findings on chest X-ray or computed tomography, and patients requiring supplemental oxygen were more likely to have abnormal findings than those not requiring supplemental oxygen (5/6 [83%] vs. 1/34 [3%]).
Table 3. Laboratory and radiologic findings of the COVID-19 patients upon hospital admission.
| Findings | Normal range | All patients (n = 40) | Supplemental | P value | |||
|---|---|---|---|---|---|---|---|
| Oxygen not required (n = 34) | Oxygen required (n = 6) | ||||||
| Laboratory findings | |||||||
| Blood routine | |||||||
| White blood cells, ×109/L | 4.0–10.1 | 4.4 (4.0–6.5) | 4.5 (4.0–6.4) | 4.3 (4.0–6.7) | 0.880 | ||
| Neutrophils, ×109/L | 1.8–7.7 | 2.9 (2.4–4.2) | 2.9 (2.3–4.0) | 2.9 (2.8–4.7) | 0.519 | ||
| Lymphocytes, ×109/L | 0.9–4.0 | 1.3 (0.9–1.7) | 1.4 (1.0–1.8) | 1.0 (0.8–1.3) | 0.233 | ||
| Platelets, ×109/L | 140–440 | 196 (152–267) | 203 (150–279) | 176 (167–201) | 0.306 | ||
| Hemoglobin, g/L | 12–16 | 13.9 (13.2–15.9) | 14.0 (13.1–16.2) | 13.8 (13.3–13.8) | 0.185 | ||
| Coagulation function | |||||||
| Prothrombin time, sec | 9.3–13.2 | 11.4 (10.9–11.8) | 11.5 (11.1–11.8) | 10.7 (10.3–11.0) | 0.019 | ||
| Activated partial thromboplastin time, sec | 21.0–39.4 | 27.7 (18.8–32.2) | 28.0 (20.9–33.0) | 22.0 (18.0–25.1) | 0.233 | ||
| Albumin, g/dL | 3.5–5.0 | 4.5 (4.2–4.8) | 4.7 (4.3–4.8) | 3.9 (3.8–4.1) | 0.001 | ||
| AST, U/L | 0–41 | 19 (19–29) | 19 (18–27) | 25 (26–34) | 0.019 | ||
| ALT, U/L | 15–40 | 23 (14–35) | 21 (13–35) | 32 (15–33) | 0.532 | ||
| Total bilirubin, mg/dL | 0.1–1.2 | 0.3 (0.3–0.5) | 0.4 (0.3–0.5) | 0.3 (0.2–0.4) | 0.324 | ||
| BUN, mg/dL | 8–20 | 10.8 (8.9–14.5) | 11.0 (9.0–14.1) | 9.4 (7.2–15.3) | 0.532 | ||
| Creatinine, mg/dL | 0.6–1.5 | 0.75 (0.64–0.91) | 0.78 (0.64–0.89) | 0.67 (0.63–0.98) | 0.747 | ||
| Glucose, mg/dL | 70–110 | 106 (93–122) | 101 (90–112) | 127 (113–180) | 0.006 | ||
| Infection-related biomarkers | |||||||
| Procalcitonin, ng/mL, > 0.05 (n = 39) | ≤ 0.05 | 9 (23) | 4 (12) | 5 (83) | < 0.001 | ||
| CRP, mg/dL, > 0.5 | 0–0.5 | 10 (25) | 4 (12) | 6 (100) | < 0.001 | ||
| Radiologic findings | < 0.001 | ||||||
| Abnormal chest X-ray and CT | - | 6 (15) | 1 (3) | 5 (83) | |||
| Bilateral lung | - | 4 (10) | 0 | 4 (66) | |||
| Unilateral lung | - | 2 (5) | 1 (3) | 1 (17) | |||
| Normal | - | 34 (85) | 33 (97) | 1 (17) | |||
Data are presented as median (interquartile range) or number (%).
COVID-19 = coronavirus disease 2019, AST = aspartate aminotransferase, ALT = alanine aminotransferase, BUN = blood urea nitrogen, CRP = C-reactive protein, CT = computed tomography.
Treatments and clinical outcomes
Treatments and clinical outcomes of the 40 patients are summarized in Table 4. Thirty-nine (98%) patients (i.e., all except one pregnant female) received antiviral therapy (lopinavir/ritonavir). Further, eight (20%) patients received antimalarial therapy (hydroxychloroquine). Patients requiring supplemental oxygen were more likely to receive antimalarial therapy than those not requiring supplemental oxygen (4/6 [67%] vs. 2/34 [6%]). One patient received continuous renal replacement therapy and invasive mechanical ventilation but eventually died. Among the 40 patients, 39 were discharged after recovery and 1 died, corresponding to a mortality rate of 3% (1/40). Four patients (10%) were readmitted during the study period after receiving positive real-time RT-PCR test results again, including two patients with mild symptoms and two asymptomatic patients. The median duration from discharge to readmission was 25 days (IQR, 12–35).
Table 4. Treatment and clinical outcomes of the COVID-19 patients.
| Outcomes | All patients (n = 40) | Supplemental | P value | ||
|---|---|---|---|---|---|
| Oxygen not required (n = 34) | Oxygen required (n = 6) | ||||
| Treatment | |||||
| Antiviral therapya | 39 (98) | 33 (97) | 6 (100) | 1.000 | |
| Antimalarial therapyb | 8 (20) | 2 (6) | 4 (67) | < 0.001 | |
| CRRT | 1 (3) | 0 | 1 (17) | 0.150 | |
| IMV | 1 (3) | 0 | 1 (17) | 0.150 | |
| Clinical outcomes | |||||
| Discharged | 39 (97) | 34 (100) | 5 (83) | 0.150 | |
| Died | 1 (3) | 0 | 1 (17) | 0.150 | |
| Readmission | 4 (10) | 4 (12) | 0 | 1.000 | |
Data are presented as number (%).
COVID-19 = coronavirus disease 2019, CRRT = continuous renal replacement therapy, IMV = invasive mechanical ventilation.
aLopinavir/ritonavir, 400 mg/100 mg for 1 week; bHydroxychloroquine, 400 mg for 5 days.
The main durations related to COVID-19 are shown in Table 5. The median incubation period was 5 days (IQR, 4–6) for 25 patients in whom the exact dates of exposure to SARS-CoV-2 and symptom onset were known. The baseline characteristics of the two patient groups (included vs. excluded) evaluated for the estimation of the incubation period are shown in Supplementary Table 1. No imported patients knew the exact date of exposure to SARS-CoV-2 and thus were excluded from the estimation of incubation period.
Table 5. Main durations of COVID-19.
| Duration | All patients | Supplemental | P value | ||||
|---|---|---|---|---|---|---|---|
| Oxygen not required | Oxygen required | ||||||
| Median (IQR) | No. of patients | Median (IQR) | No. of patients | Median (IQR) | No. of patients | ||
| Incubation period,a day | 5 (4–6) | 25 | 5 (4–6) | 22 | 6 (4–9) | 3 | 0.643 |
| Symptom onset to admission,b day | 5 (2–8) | 31 | 5 (2–8) | 26 | 6 (5–9) | 5 | 0.333 |
| Duration of viral shedding,c day | 21 (14–28) | 36 | 20 (13–27) | 31 | 22 (21–29) | 5 | 0.507 |
| Duration of hospital stay,d day | 22 (16–27) | - | 21 (16–24) | - | 28 (20–32) | - | 0.029 |
COVID-19 = coronavirus disease 2019, IQR = interquartile range, RT-PCR = reverse transcription-polymerase chain reaction.
aTwo asymptomatic patients and 13 symptomatic patients without the exact date of exposure to SARS-CoV-2 or symptom onset known were excluded; bTwo asymptomatic patients, five presymptomatic patients, and two symptomatic patients without the exact date of symptom onset known were excluded; cDuration was calculated by subtracting the date of symptom onset from the median of the date of the last positive real-time RT-PCR test result and the date of the first negative real-time RT-PCR test result. Two asymptomatic patients and two symptomatic patients without the exact date of symptom onset known were excluded; dDuration was calculated by subtracting the day of admission from the day of discharge.
The median duration from symptom onset to hospital admission was 5 days (IQR, 2–8). The median duration from symptom onset to undergoing PCR test was 3 days (IQR, 1–7) and that to obtaining PCR result was 1 day (IQR, 0–1) (Supplementary Table 2). Thirty-nine (98%) patients were admitted to the hospital within 1 day after receiving positive real-time RT-PCR results. The median duration of viral shedding was 21 days (IQR, 14–28), with the maximum duration being 51 days. The median duration of hospital stay was 22 days (IQR, 16–27).
DISCUSSION
In this retrospective case series of 40 COVID-19 patients admitted to a hospital, only 2 (5%) were asymptomatic and 5 (13%) were presymptomatic. Although this study investigated COVID-19 patients at one hospital, all cases that developed in a metropolitan city of Korea were included; these cases had characteristics similar to those of other COVID-19 patients in Korea.16,17 COVID-19 patients in this study were slightly younger than those in Korea in general (43% vs. 34% aged ≤ 29 years and 18% vs. 24% aged ≥ 60 years).16 However, females accounted for 58% of the patients (57.6% for all patients with COVID-19 in Korea). The mortality rate was 3% (1/40), which is similar to the 2.3% reported for all patients with COVID-19 in Korea. As of June 20, 2020, the incidence of SARS-CoV-2 infection in Ulsan was 4.6/100,000 people, which is the same as the median value reported in 17 provinces and major cities of Korea (range, 1.1–238.2/100,000 people).17
The patients requiring supplemental oxygen were older and more likely to have comorbidities than those not requiring supplemental oxygen. The patient who died required supplemental oxygen, was 67 years old, and had cardiovascular disease. This suggests that age and comorbidities are risk factors for poor prognosis.5,6
Among the 40 patients in this study, 2 (5%) had asymptomatic SARS-CoV-2 infection. Thirty-three (83%) were symptomatic and five (13%) were presymptomatic. Park et al.18 reported the epidemiology of the COVID-19 outbreak at a call center in Korea. Among 97 patients, 4 (4%) remained asymptomatic after 14 days of quarantine, which is similar to the 5% reported in our study. Arons et al.19 reported that the prevalence of asymptomatic infection was 6% (3/48) in residents at a skilled nursing facility in Washington, US, which was similar to the prevalence in the present study. They used 14 symptoms to define symptomatic infections, which were also similar to the 16 symptoms included in the present study. By contrast, many other studies reported much higher prevalence of asymptomatic infection than our study, and they tended to use fewer symptoms to define symptomatic infections.20,21,22,23 An Italian study reported that 42% of infections were asymptomatic when only fever and cough were considered symptoms.21 In an Icelandic population screening,20 43% of patients were asymptomatic. However, the authors noted that symptoms almost certainly developed later in some of the asymptomatic patients. Hence, the actual prevalence of asymptomatic infections is likely to be < 43%. Regarding female admitted for delivery in New York city, the asymptomatic infection rate was 88%, which was much higher than that observed in the present study.22 In that study, the authors considered symptomatic cases to have fever and other symptoms of COVID-19 but did not provide information about the other symptoms. In a study of Greek citizens evacuated from three European countries, asymptomatic infection rate was 88%.23 The subjects were asked in-flight to complete a paper form with clinical information and received written instructions to report any new symptoms by telephone. The authors did not include symptoms other than fever and cough. Thus, symptoms were likely underestimated in that study. In a review, Oran and Topol24 reported that asymptomatic SARS-CoV-2 infections accounted for 40%–45% of all infections. However, there were no records of the articles used in their review to confirm whether atypical symptoms such as anorexia, diarrhea, and nausea were evaluated.24 A COVID-19 infection survey in England published in July 2020 reported that 67% of patients were asymptomatic. However, symptoms were self-reported rather than clinically diagnosed and instances wherein the questions related to symptoms were not answered were defined as asymptomatic.25 Given these findings, the real prevalence of asymptomatic SARS-CoV-2 infection may be much lower than those reported in previous studies and is associated with the definition of a symptomatic infection and the number of symptoms used to define symptomatic. Therefore, careful history taking with the appropriate number of symptoms is required to diagnose COVID-19.
We investigated 16 symptoms of SARS-CoV-2 infection and found that cough and fever were the most common symptoms and that many other symptoms developed in addition to fever or cough. For example, sputum production always developed with cough and shortness of breath always developed with fever. Conversely, myalgia, rhinorrhea or nasal congestion, or diarrhea developed without cough or fever in some patients. Hence, cough, fever, myalgia, rhinorrhea or nasal congestion, and diarrhea were the screening criteria used to detect all cases of symptomatic and presymptomatic SARS-CoV-2 infections. Further studies with varied study populations are required to determine screening criteria with representative symptoms of COVID-19. Sputum production, chest discomfort, and the number of symptoms were associated with requiring supplemental oxygen in univariate analyses. Multivariate analyses are required to confirm whether sputum production, chest discomfort, and a large number of symptoms can predict poor prognosis of COVID-19.
This study has several advantages. First, data were collected from manual medical record reviews and an electronic health record database, thus providing more detailed patient information. Second, we used varied data sources including epidemiological and clinical data identified by a preventive medicine specialist who interviewed all patients, resulting in highly qualified and sufficient information. Finally, we monitored all patients including readmitted patients until they were discharged. Therefore, it was possible to perform continued observation of the natural course of COVID-19.
However, this study has several limitations. First, given the limited number of cases, it was difficult to compare variables using multivariable-adjusted methods. Second, we could only estimate the incubation period for 63% (25/40) of the patients and could not estimate it for the imported cases. The uncertainty of the exact dates might have affected our assessment. Third, we did not have information about the loss of taste or smell as symptoms of COVID-9.26 There was limited information on the loss of taste or smell as symptoms of COVID-9 in February and March, 2020 when most patients with COVID-19 in this study were hospitalized. Hence, patients’ history of taste or smell was not taken at admission. If loss of taste or smell was included in our screening criteria, the prevalence of asymptomatic SARS-CoV-2 infection might have been < 5% in the present study. Finally, we only investigated the presence of symptoms and did not consider the severity of symptoms. Hence, if a symptom is mild, the clinical importance of the symptom is not clear.
In this case series, we found that the prevalence of asymptomatic SARS-CoV-2 infection was 5%, which is much lower than those previously reported. This finding suggests that the careful investigation of symptom history and follow-up should be performed to detect SARS-CoV-2 infections. Cough, fever, myalgia, rhinorrhea or nasal congestion, and diarrhea were the screening criteria used to cover all symptoms of SARS-CoV-2 infection. Further evaluation with varied study populations is required to create representative screening criteria for COVID-19.
ACKNOWLEDGMENTS
We thank Jae-Bum Jun, Jong-Joon Ahn, Tae-Hoon Lee, Yang-Jin Jegal, Seung-Won Ra, Hyeon-Hui Kang, Kwang-Won Seo, and Byung-Ju Kang (Department of Internal Medicine, Ulsan University Hospital, Ulsan, Korea) for the contribution to the management of patients with COVID-19 at Ulsan University Hospital.
Footnotes
Disclosure: The authors have no potential conflicts of interest to disclose.
- Conceptualization: Jeong TH, Park C.
- Data curation: Park C.
- Formal analysis: Jeong TH, Lee SH.
- Investigation: Ock M.
- Methodology: Jeong TH, Park C, Son JS, Jeon YG.
- Software: Jeong TH.
- Writing - original draft: Jeong TH.
- Writing - review & editing: Park C, Ock M, Lee SH, Son JS, Jeon YG.
SUPPLEMENTARY MATERIALS
Baseline characteristics of the patients stratified by inclusion for the estimation of incubation period
Durations from symptom onset to admission in COVID-19 patients
References
- 1.Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395(10223):497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organization. Coronavirus disease (COVID-19): situation report-51. [Updated 2020]. [Accessed March 22, 2020]. https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200311-sitrep-51-covid-19.pdf.
- 3.World Health Organization. Coronavirus disease (COVID-19): situation report-61. [Updated 2020]. [Accessed July 12, 2020]. https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200620-covid-19-sitrep-152.pdf?sfvrsn=83aff8ee_4.
- 4.Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, He JX, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382(18):1708–1720. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wang D, Hu B, Hu C, Zhu F, Liu X, Zhang J, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA. 2020;323(11):1061–1069. doi: 10.1001/jama.2020.1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chen N, Zhou M, Dong X, Qu J, Gong F, Han Y, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020;395(10223):507–513. doi: 10.1016/S0140-6736(20)30211-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Richardson S, Hirsch JS, Narasimhan M, Crawford JM, McGinn T, Davidson KW, et al. Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the New York City area. JAMA. 2020;323(20):2052–2059. doi: 10.1001/jama.2020.6775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Subbe CP, Kruger M, Rutherford P, Gemmel L. Validation of a modified Early Warning Score in medical admissions. QJM. 2001;94(10):521–526. doi: 10.1093/qjmed/94.10.521. [DOI] [PubMed] [Google Scholar]
- 9.Hu H, Yao N, Qiu Y. Comparing rapid scoring systems in mortality prediction of critical ill patients with novel coronavirus disease. Acad Emerg Med. 2020;27(6):461–468. doi: 10.1111/acem.13992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lim WS, van der Eerden MM, Laing R, Boersma WG, Karalus N, Town GI, et al. Defining community acquired pneumonia severity on presentation to hospital: an international derivation and validation study. Thorax. 2003;58(5):377–382. doi: 10.1136/thorax.58.5.377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lim WS, Baudouin SV, George RC, Hill AT, Jamieson C, Le Jeune I, et al. BTS guidelines for the management of community acquired pneumonia in adults: update 2009. Thorax. 2009;64 Suppl 3:iii1–iii55. doi: 10.1136/thx.2009.121434. [DOI] [PubMed] [Google Scholar]
- 12.Nguyen Y, Corre F, Honsel V, Curac S, Zarrouk V, Fantin B, et al. Applicability of the CURB-65 pneumonia severity score for outpatient treatment of COVID-19. J Infect. 2020;81(3):e96–8. doi: 10.1016/j.jinf.2020.05.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Corman VM, Landt O, Kaiser M, Molenkamp R, Meijer A, Chu DK, et al. Detection of 2019 novel coronavirus (2019-nCoV) by real-time RT-PCR. Euro Surveill. 2020;25(3):2000045. doi: 10.2807/1560-7917.ES.2020.25.3.2000045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.COVID-19 National Emergency Response Center, Epidemiology and Case Management Team, Korea Centers for Disease Control and Prevention. Early epidemiological and clinical characteristics of 28 cases of coronavirus disease in South Korea. Osong Public Health Res Perspect. 2020;11(1):8–14. doi: 10.24171/j.phrp.2020.11.1.03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kim ES, Chin BS, Kang CK, Kim NJ, Kang YM, Choi JP, et al. Clinical course and outcomes of patients with severe acute respiratory syndrome coronavirus 2 infection: a preliminary report of the first 28 patients from the Korean cohort study on COVID-19. J Korean Med Sci. 2020;35(13):e142. doi: 10.3346/jkms.2020.35.e142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Korea Centers for Disease Control & Prevention. Coronavirus disease-19, Republic of Korea. Cases in Korea. [Updated 2020]. [Accessed June 20, 2020]. http://ncov.mohw.go.kr/en/bdBoardList.do?brdId=16&brdGubun=161&dataGubun=&ncvContSeq=&contSeq=&board_id=
- 17.Korea Centers for Disease Control & Prevention. Coronavirus disease-19, Republic of Korea. Cases in Korea by city/province. [Updated 2020]. [Accessed June 20, 2020]. http://ncov.mohw.go.kr/en/bdBoardList.do?brdId=16&brdGubun=162&dataGubun=&ncvContSeq=&contSeq=&board_id=#header.
- 18.Park SY, Kim YM, Yi S, Lee S, Na BJ, Kim CB, et al. Coronavirus disease outbreak in Call Center, South Korea. Emerg Infect Dis. 2020;26(8):1666–1670. doi: 10.3201/eid2608.201274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Arons MM, Hatfield KM, Reddy SC, Kimball A, James A, Jacobs JR, et al. Presymptomatic SARS-CoV-2 infections and transmission in a skilled nursing facility. N Engl J Med. 2020;382(22):2081–2090. doi: 10.1056/NEJMoa2008457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gudbjartsson DF, Helgason A, Jonsson H, Magnusson OT, Melsted P, Norddahl GL, et al. Spread of SARS-CoV-2 in the Icelandic population. N Engl J Med. 2020;382(24):2302–2315. doi: 10.1056/NEJMoa2006100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lavezzo E, Franchin E, Ciavarella C, Cuomo-Dannenburg G, Barzon L, Del Vecchio C, et al. Suppression of a SARS-CoV-2 outbreak in the Italian municipality of Vo'. Nature. 2020;584(7821):425–429. doi: 10.1038/s41586-020-2488-1. [DOI] [PubMed] [Google Scholar]
- 22.Sutton D, Fuchs K, D'Alton M, Goffman D. Universal screening for SARS-CoV-2 in women admitted for delivery. N Engl J Med. 2020;382(22):2163–2164. doi: 10.1056/NEJMc2009316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lytras T, Dellis G, Flountzi A, Hatzianastasiou S, Nikolopoulou G, Tsekou K, et al. High prevalence of SARS-CoV-2 infection in repatriation flights to Greece from three European countries. J Travel Med. 2020;27(3):taaa054. doi: 10.1093/jtm/taaa054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Oran DP, Topol EJ. Prevalence of asymptomatic SARS-CoV-2 infection: a narrative review. Ann Intern Med. 2020;173(5):362–367. doi: 10.7326/M20-3012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Office for National Statistics. Coronavirus (COVID-19) infections in the community in England. [Updated July 2020]. [Accessed July 9, 2020]. https://www.ons.gov.uk/peoplepopulationandcommunity/healthandsocialcare/conditionsanddiseases/articles/coronaviruscovid19infectionsinthecommunityinengland/july2020.
- 26.Stokes EK, Zambrano LD, Anderson KN, Marder EP, Raz KM, El Burai Felix S, et al. Coronavirus disease 2019 case surveillance - United States, January 22-May 30, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(24):759–765. doi: 10.15585/mmwr.mm6924e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Baseline characteristics of the patients stratified by inclusion for the estimation of incubation period
Durations from symptom onset to admission in COVID-19 patients



