Abstract
Summary
To investigate the cumulative incidence and mortality of COVID-19 and the prevalence of comorbidities such as diabetes, obesity and hypertension in regions with different altitude levels ranging from sea level to high altitude.
Methodology
Analytical study in which we correlated secondary data obtained from reports of the Ministry of Health and National Institute for Statistics and Informatic. The cumulative incidence and mortality of COVID-19 in 25 peruvian regions is reported, together with its relationnship with altitude levels during March-July 2020 using Pearsońs correlation. We also aiming to assess the prevalence of diabetes, obesity and hypertension with altitude according to the ENDES 2018 data using Gamma statistics.
Results
COVID-19 maintained an inverse correlation with higher rates in the coastal regions and lower rates with increasing altitude in the cumulative incidence (Pearson = −0.8, p < 0.000) and mortality (Pearson = −0.77, p < 0.000), adjusted gender and age. The prevalence of diabetes and obesity showed the same inverse correlation trend with altitude (Gamma p < 0.000) but not hypertension (Gamma p = 0.13)
Conclusions
The data in Peru it is suggested that physiological adaptation in a hypoxic environment at high altitude may protect persons from the severe impact of acute infection caused by SARS-CoV-2. The reduction in cumulative incidence and mortality rates with increasing altitude is the main finding. Possible mechanisms such as a decreased expression of angiotensin-converting enzyme 2 (ACE2) and a lower virulence because of a high altitude environment, may explain this epidemiological features. In addition, the lower prevalence of diabetes, obesity and hypertension may establish a protective epidemiology against these disease.
Keywords: COVID-19, Altitude, Incidence, Mortality, Prevalence, Diabetes, Hypertension, Obesity, ACE2, ENDES 2018
1. Introduction
A lethal form of pneumonia leading to severe acute respiratory syndrome (SARS-CoV-2) caused by a new coronavirus is a disease detected in December 2019 in the People's Republic of China, in Wuhan (Hubei province). This condition quickly spread to other Chinese provinces and all over the world with currently more than 24 million infected patients with nearly 900,000 deaths affecting 188 countries [1], [2], [3], [4]. Data presented at the CROI 2020 (Conference on Retroviruses and Opportunistic Infection) held in Boston, Massachusetts last March, showed that the clinical spectrum of pneumonia was mild to moderate cases, 80%; and 20% severe cases, leading to a 50% mortality rate in Intensive Care Units (ICU). Age, particularly being more than 80 years old, led to high mortality rates (16%), as well as comorbidities such as heart disease (10.5%), diabetes mellitus (7.3%), chronic respiratory disease (6.3%), high blood pressure (6%), and cancer (5.6%) amongst others [5], [6], [7], [8].
To date, mortality is mostly affecting the following countries: USA (172,000 deaths), Brazil (109,000 deaths), Mexico (57,000 deaths), India (52,000 deaths), UK (42,000 deaths), Italy (36,000 deaths), France (31,000 deaths), Spain (29,000 deaths), and Peru (27,000 deaths) [4].
The first case in Latin America was reported in Brazil (February 26, 2020), followed by Mexico (February 28, 2020), Chile and Argentina (March 3, 2020), and Peru on March 6, 2020. Case numbers and mortality rates are rapidly increasing in Brazil, Peru, Colombia and Chile, and nowadays these countries are the most severely affected by the pandemic in this region [9].
Peru is located in the western part of South America. Its western natural border is the Pacific Ocean; its other borders are Ecuador and Colombia in the north, Brazil in the east, and Bolivia and Chile in the southeast. Peruvian territory has many ecological floors: the coast at sea level where Lima, the capital city is located; the highlands, where there are some cities located higher than 3000 m above sea level, and the large Amazon rainforest bordering Ecuador, Colombia, Brazil, and Bolivia [10].
Cumulative incidence and mortality rates from COVID-19 occurring in this 32-million inhabitant country have a peculiar behavior according to its ecological areas. Lower numbers of COVID-19 cases have been observed in populations living at high altitude in the Andean region compared to coastal populations. This study analyzes the epidemiological features of COVID-19 infection according to altitude and the prevalence of diabetes mellitus, obesity and hypertension, conditions that may worsen its outcome.
2. Material and methods
This study has an analytical design, using secondary data of cumulative cases and mortality from COVID-19, obtained from reports issued by the Peruvian Ministry of Health (MINSA) from March to July 2020, the date on which the quarantine ended. Emphasis was placed on the occurrence of COVID-19 cases and mortality according to altitude levels in 25 Peruvian regions. Death COVID definition was made by using the ICD-10 code (U07.1 or U07.2 or B34.X or J97.X) or by written diagnosis (“COVID”, “Coronavirus”, “SARS CoV-2”) [11], [12].
Secondary data of the last Peruvian National Demographics and Health Survey (ENDES 2018) was explored regarding the prevalence of obesity, diabetes mellitus, and hypertension according to altitude: <1000 m above sea level (masl), 1000–3000 masl and >3000 masl. This is a representative survey, and 32,950 weighted cases were considered in subjects over 18 years old [13].
The data was analyzed using SPSS Statistics 25 Software and Pearson's correlation between COVID-19 cumulative incidence and mortality rates according to altitude. The average altitude of each region was used. The prevalence of obesity, diabetes mellitus, and high blood pressure was calculated according for 1000, 3000 and >3000 masl. Gamma statistics was used for measuring this correlation. Cumulative incidence was expressed as the case rate (cases × 1000 inhabitants) and mortality was expressed as deaths × 1000 inhabitants. The reference population for all estimates was obtained from the projected population for year 2020 according to the National Institute of Statistics and Informatics (INEI) [14].
3. Results
Table 1 describes the cumulative cases in the 25 Peruvian regions, ordered according to ascending altitude. The values found on the coast at sea level in cities such as Lima (20.87/1000) and Callao (19.20/1000) were descending to regions located at >3000 masl such as Apurimac (2.27/1000) and Puno (2.04/1000).
Table 1.
COVID-19 cases × 1000 inhabitants and Altitude in Peruvian Regions. March – July 2020.
| Region | Altitude (m) | Populationa | COVID casesb | COVID cases × 1000 |
|---|---|---|---|---|
| Peru | 32,625,948 | 423,611 | 12.98 | |
| Callao | 7 | 1,129,854 | 21,695 | 19.20 |
| Tumbes | 8 | 251,521 | 4329 | 17.21 |
| Lambayeque | 38 | 1,310,785 | 11,575 | 8.83 |
| Lima | 92 | 10,628,470 | 221,772 | 20.87 |
| Loreto | 123 | 1,027,559 | 11,901 | 11.58 |
| Ica | 291 | 975,182 | 13,475 | 13.82 |
| Madre de Dios | 305 | 173,811 | 3627 | 20.87 |
| Ucayali | 310 | 589,110 | 10,279 | 17.45 |
| San Martin | 500 | 899,648 | 9202 | 10.23 |
| Piura | 606 | 2,047,954 | 21,578 | 10.54 |
| Moquegua | 1197 | 192,740 | 3212 | 16.66 |
| Amazonas | 1330 | 426,806 | 6222 | 14.58 |
| La Libertad | 1572 | 2,016,771 | 15,877 | 7.87 |
| Arequipa | 1754 | 1,497,438 | 14,997 | 10.02 |
| Tacna | 1901 | 370,974 | 3020 | 8.14 |
| Ayacucho | 1999 | 668,213 | 4013 | 6.01 |
| Cajamarca | 2273 | 1,453,711 | 7121 | 4.90 |
| Huanuco | 2406 | 760,267 | 6904 | 9.08 |
| Ancash | 2607 | 1,180,638 | 12,412 | 10.51 |
| Junín | 2830 | 1,361,467 | 8156 | 5.99 |
| Apurimac | 3024 | 430,736 | 979 | 2.27 |
| Pasco | 3112 | 271,904 | 2032 | 7.47 |
| Cusco | 3149 | 1,357,075 | 4881 | 3.60 |
| Huancavelica | 3359 | 365,317 | 1821 | 4.98 |
| Puno | 3744 | 1,237,997 | 2,531 | 2.04 |
Projected population 2020 according to the National Institute of Statistics and Informatics (INEI).
Covid cases according to the Peruvian Ministry of Health until July 31, 2020.
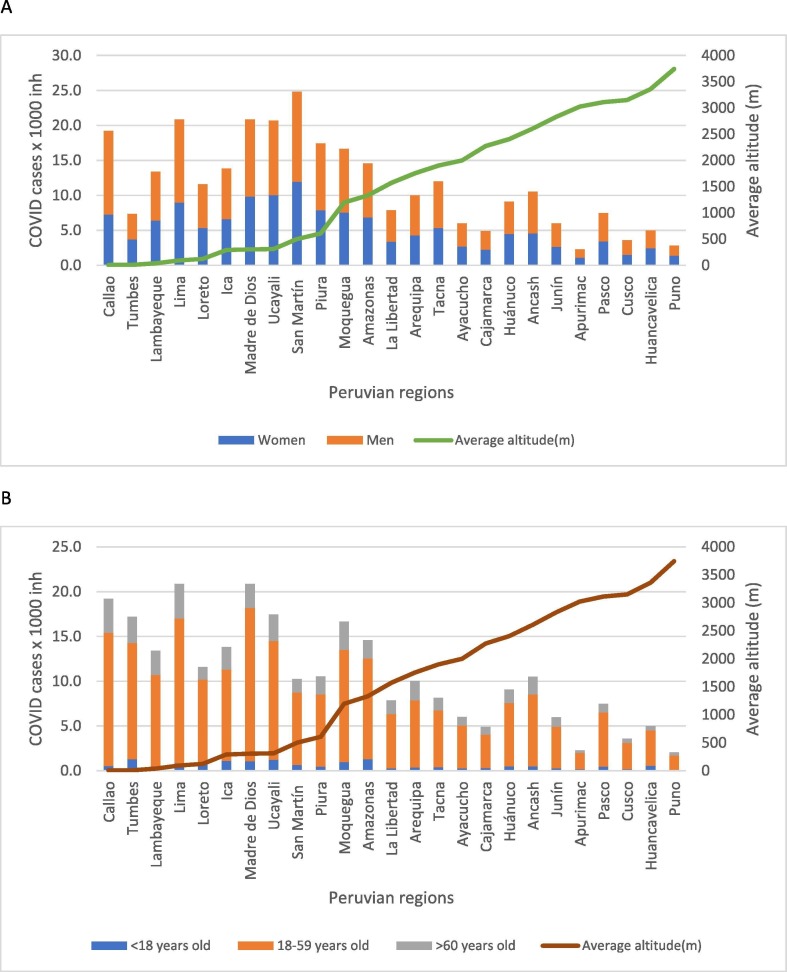
Fig. 1 shows an inverse correlation between altitude and cumulative cases of COVID-19/1000 inhabitants. Pearson’s statistics shows a highly significant association (Pearson = −0.8, p < 0.000) adjusted to gender and age (Table 3).
Fig. 1.
COVID-19 Cases × 1000 and Altitude in Peruvian regions. Mar-Jul 2020. A. Adjusted for gender. Women (Pearson correlation = −0.77, p = 0.000); Men (Pearson correlation = −0.77, p = 0.000). B. Adjusted for Age. < 18 years old (Pearson correlation − 0.66, p = 0.000); 18–59 years old (Pearson correlation = −0.84, p = 0.000); >60 years old (Pearson correlation = −0.81, p = 0.000).
Table 3.
Pearson correlation COVID 19 cases and deaths by gender and age according altitude average i .
| COVID Cases |
COVID Deaths |
|||
|---|---|---|---|---|
| Pearson correlation | p | Pearson correlation | p | |
| Total | −0.80 | 0.000 | −0.77 | 0.000 |
| Gender | ||||
| Women | −0.77 | 0.000 | −0.70 | 0.000 |
| Men | −0.77 | 0.000 | −0.76 | 0.000 |
| Age | ||||
| <18 years old | −0.66 | 0.000 | −0.53 | 0.005 |
| 18–59 years old | −0.84 | 0.000 | −0.79 | 0.000 |
| >60 years old | −0.81 | 0.000 | −0.75 | 0.000 |
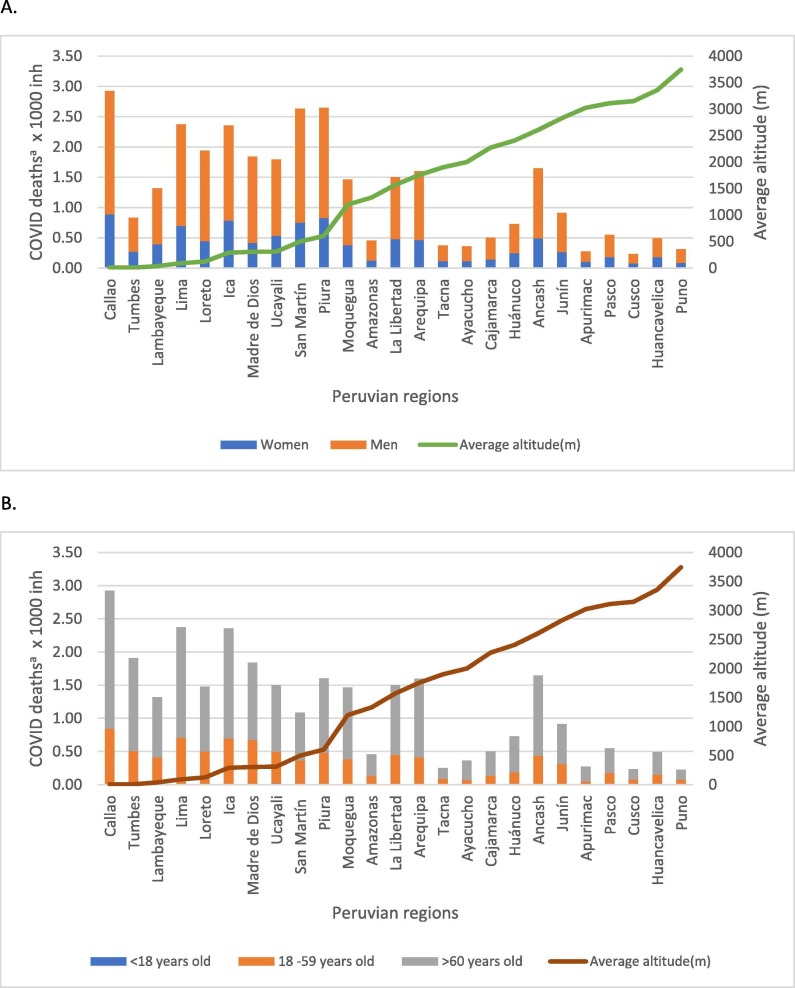
Table 2 describes a progressively inverse relationship for mortality and altitude levels in the 25 studied regions. At sea level, Callao 2.93/1000 and Lima (2.37/1000). In high altitude, Cusco (0.24/1000) and Puno (0.23/1000)
Table 2.
COVID-19 Mortality × 1000 and Altitude in Peruvian regions March -July 2020.
| Region | Altitude (m) | Populationa | COVID deathsb | COVID deaths × 1000 |
|---|---|---|---|---|
| Peru | 32,625,948 | 51,789 | 1.59 | |
| Callao | 7 | 1,129,854 | 3305 | 2.93 |
| Tumbes | 8 | 251,521 | 490 | 1.95 |
| Lambayeque | 38 | 1,310,785 | 1727 | 1.32 |
| Lima | 92 | 10,628,470 | 25,233 | 2.37 |
| Loreto | 123 | 1,027,559 | 1522 | 1.48 |
| Ica | 291 | 975,182 | 2297 | 2.36 |
| Madre de Dios | 305 | 173,811 | 320 | 1.84 |
| Ucayali | 310 | 589,110 | 890 | 1.51 |
| San Martin | 500 | 899,648 | 976 | 1.08 |
| Piura | 606 | 2,047,954 | 3278 | 1.60 |
| Moquegua | 1197 | 192,740 | 282 | 1.46 |
| Amazonas | 1330 | 426,806 | 195 | 0.46 |
| La Libertad | 1572 | 2,016,771 | 3029 | 1.50 |
| Arequipa | 1754 | 1,497,438 | 2393 | 1.60 |
| Tacna | 1901 | 370,974 | 94 | 0.25 |
| Ayacucho | 1999 | 668,213 | 242 | 0.36 |
| Cajamarca | 2273 | 1,453,711 | 728 | 0.50 |
| Huánuco | 2406 | 760,267 | 554 | 0.73 |
| Ancash | 2607 | 1,180,638 | 1944 | 1.65 |
| Junín | 2830 | 1,361,467 | 1245 | 0.91 |
| Apurimac | 3024 | 430,736 | 118 | 0.27 |
| Pasco | 3112 | 271,904 | 149 | 0.55 |
| Cusco | 3149 | 1,357,075 | 319 | 0.24 |
| Huancavelica | 3359 | 365,317 | 180 | 0.49 |
| Puno | 3744 | 1,237,997 | 279 | 0.23 |
Projected population 2020 according to the National Institute of Statistics and Informatics (INEI).
Covid deaths according to the National System of Deaths (SINADEF) of the Peruvian Ministry of Health from March 1st until July 31st, 2020. Death COVID definition by CIE 10 code (U07.1 or U07.2 or B34.X or J97.X) or by written diagnosis (“COVID”, “Coronavirus”, “SARS CoV-2”).
Fig. 2 shows an inverse correlation between altitude and COVID-19 mortality × 1000 inhabitants. Pearson's statistics shows a highly significant association (Pearson = −0.77p < 0.000), adjusted to gender and age (Table 3).
Fig. 2.
COVID-19 Deaths × 1000 inh and Altitude in Peruvian regions. March -July 2020. A. Adjusted for gender. Women (Pearson correlation = −0.70, p = 0.000); Men (Pearson correlation = −0.76, p = 0.000). B. Adjusted for Age. < 18 years old (Pearson correlation − 0.53, p = 0.005); 18–59 years old (Pearson correlation = −0.79, p = 0.000); >60 years old (Pearson correlation = −0.75, p = 0.000). aCovid deaths according to the National System of Deaths (SINADEF) of the Peruvian Ministry of Health from March 1st until July 31st, 2020. Death COVID definition by CIE 10 code (U07.1 or U07.2 or B34.X or J97.X) or by written diagnosis (“COVID”, “Coronavirus”, “SARS CoV-2”).
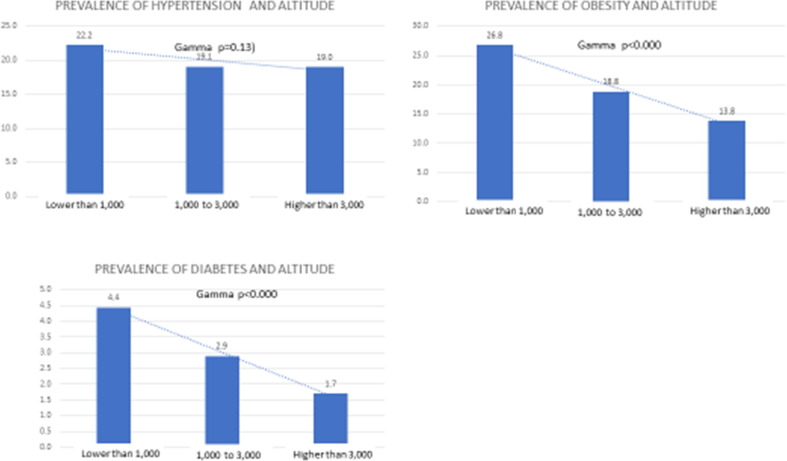
Fig. 3 shows an inverse correlation between altitude and the prevalence of diabetes, obesity and high blood pressure. Self-reported prevalence of diabetes decrease progressively from 4.4% (<1000 mals), 2.9% (1000–3000 mals) to 1.7% (>3000 mals). Obesity prevalence by BMI decreased from 26.8% (<1000 mmasl), 18.8 (1000–3000 mals) to 13.8% (>3000 mals). When applying Gamma statistics, associations for diabetes and obesity were significant (p = 0.000). The association for high blood pressure was marginal, 22.2% (<1000 masl), 19.1% (1000–3000 masl) to 19.0% (>3000 masl) (p = 0.13).
Fig. 3.
Source ENDES 2018.
4. Discussion
SARS-CoV-2, the causative agent of COVID-19 disease enters the respiratory tract cells, as well as the lung, heart, arteries and kidneys through angiotensin-converting enzyme 2 (ACE2). The main damage occurs in the pulmonary epithelium where ACE2 acts as a vasodilator agent, balancing the action of ACE1, which acts as a vasoconstrictor [15].
Under normal conditions the renin-angiotensin system (RAS) is regulated by a balance between ACE1 and ACE2 expression, but a study in rats exposed to hypoxic conditions equivalent to 4500 m altitude, showed increased ACE1 levels and reduced ACE2 expression in the target cells [16]. Experimentally, it has been shown that under hypoxic conditions, ACE1 is regulated by the hypoxia-inducible factor 1 (HIF-1) in human pulmonary artery smooth muscle cells (hPASMC), while ACE2 expression is markedly decreased [17].
Studies carried out during the first SARS-CoV epidemics in 2002 showed that the level of ACE2 expression in lung epithelial cells was positively correlated with the infection rate [18], [19], [20], [21].
Since under hypoxia experimental conditions the level of ACE2 expression is decreased, it may be inferred that persons living in high altitude exposed to chronic hypoxia also express reduced ACE2 levels in their lungs; and, therefore, they may be less susceptible to SARS-CoV-2 penetration in pulmonary cells; and, therefore, they might be less susceptible for acquiring COVID-19 infection.
On the other hand, a series of studies in accordance with our investigation, have shown that altitude exerts a protective effect for the development of diabetes, hypertension and obesity [22], [23], [24], [25], [26], comorbidities that may worsen the outcome of COVID-19.
Therefore, altitude would be an adverse ecological ambiental for SARS-CoV-2 infection where physiological factors secondary to hypoxia are combined with a low prevalence of diabetes, hypertension and obesity and minor posibilitie of becoming infected and for developing serious and fatal conditions.
There are various case series studies conducted during the COVID-19 pandemics supporting this hypothesis.
High altitude populations of Tibet located on the northern side of the Himalayas, above 4000 masl, showed that the impact of the disease on the Tibetan plateau was low compared to that reported in other Chinese regions [27]. Only 134 confirmed cases without any death were reported (Tibet, Qinghai and part of Sichuan) [28] compared to 74,283 cases and 2009 deaths reported by China in the first wave of the pandemics.
In Bolivia, a country located in the southern Andean part of South America, populations living in high altitude, such as La Paz (2400–4000 masl), Oruro (3735 masl), Potosi (4090 masl), and Chuquisaca (2810 masl) reported 54 COVID-19 cases in total compared to infection rates in Santa Cruz de la Sierra, the second largest province in Bolivia located at 400 m above sea level, which reported more than 100,000 COVID-19 cases up to July 2020 [29].
In Ecuador, located in the northern Andean part of South America, the pandemic as of April 7th, produced four times fewer COVID-19 cases in high-altitude areas (722), compared to near 100,000 cases in coastal regions. [30]
Data obtained in the present study, confirm the strong statistical significance of low cumulative incidence and mortality of COVID-19 in high altitude populations in relation to coastal populations from Peru during follow-up of cases from March 06th, when the first case was diagnosed, until July 31th, when a quarantine phase ended.
Table 1 and Fig. 1 show a reduction in the impact of COVID-19 with increasing altitude in the 25 regions studied. Lima (92masl) with 20.87 cases/1000 inhabitants and Puno (3744 masl), with 2.04 cases/1000 inhabitants were the extreme findings for this disease behavior. We also found that mortality rates were inversely related to altitude, as shown in Table 2 and Fig. 2 with high values in Callao (2.93/1000 inhabitants) at sea level, and very low values in high altitude regions such as Puno (0.23/1000 inhabitants) at 3744 masl, adjusted for age and gender.
Beside to the hypoxic environment, there are environmental factors that could also influence the virulence of SARS-CoV-2 at high altitude such as temperature, dry air, and high levels of ultraviolet (UV) light radiation. [31], [32], [33], [34].
In conclusion, our data show a decrease in the cumulative incidence and mortality rates from SARS-CoV-2 infection with increasing altitude, particularly in populations living over 3000 m above sea level. In addition, the lower prevalence of comorbidities such as obesity, diabetes mellitus, and hypertension in altitude, may establish a protective epidemiological trend against this disease.
Funding
That research was funded by the Diabetes, Hypertension and Lipids Unit (UDHYL) of the Universidad Peruana Cayetano Heredia.
Contributors
SNS was el author of idea and design of investigation
MEN-R and MY-A were the authors of the statistics and interpretation of results
AACH analized the secundaria data of ENDES 2018
SNS,MEN-R, MA-Y and AACH participated in the research and article preparation and approved the final article.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgment
The authors appreciate the technical and secretarial support of Edwin Arroyo and Nilda Ludeña from the Diabetes, Hypertension and Lipid Unit (UDHYL) of the Universidad Peruana Cayetano Heredia in preparing the manuscript.
References
- 1.Zhu N., Zhang D., Wang W., et al. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020 doi: 10.1056/NEJMoa2001017. published online Jan 24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Holshue M.L., DeBolt C., Lindquist S., et al. First case of 2019 novel coronavirus in the United States. N Engl J Med. 2020 doi: 10.1056/NEJMoa2001191. published online Jan 3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.https://gisanddata.maps.arcgis.com/apps/opsdashboard/index.html#/bda7594740fd40299423467b48e9ecf6
- 4.The Epidemiological Characteristics of an Outbreak of 2019 Novel Coronavirus Diseases (COVID-19) — China, 2020. The Novel Coronavirus Pneumonia Emergency Response Epidemiology Team, Chinese Center for Disease Control and Prevention. CCDC Weekly / Vol. 2 / No. 8 [PMC free article] [PubMed]
- 5.Huang C., Wang Y., Li X., et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chen N., Zhou M., Dong X., et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020;395:507–513. doi: 10.1016/S0140-6736(20)30211-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wang D., Hu B., Hu C. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA. 2020 doi: 10.1001/jama.2020.1585. published online Feb. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.WHO. Clinical management of severe acute respiratory infection when novel coronavirus (nCoV) infection is suspected. Jan 11, 2020. https://www.who.int/publications-detail/clinical-management-ofsevere-acute-respiratory-infection-when-novel-coronavirus-(ncov)infection-is-suspected (accessed Feb 8, 2020).
- 9.https://www.who.int/emergencies/diseases/novel-coronavirus-2019/technical-guidance/naming-the-coronavirus-disease-(covid-2019)-and-the-virus-that-causes-it (novel virus).
- 10.«Worldometers Peru». 2020. Consulted during 2020.
- 11.Situation Room for Health Operations Covid-19 of the Ministry of Health (MINSA) during the period from March 01 to July 31, 2020.
- 12.Covid deaths according to the National System of Deaths (SINADEF) of the Peruvian Ministry of Health from March 1st until July 31st, 2020.
- 13.National Demographic and Health Survey (ENDES) 2018. National Institute of Statistics and Informatics, Peru
- 14.National Institute of Statistics and Informatics (INEI). Peruvian population projected to 2020.
- 15.Lu R., Zhao X., Li J., Niu P., Yang B., Wu H., Wang W., Song H., Huang B., Zhu N., Bi Y., Ma X., Zhan F., Wang L., Hu T., Zhou H., Hu Z., Zhou W., Zhao L., Chen J., Meng Y., Wang J., Lin Y., Yuan J., Xie Z., Ma J., Liu W.J., Wang D., Xu W., Holmes E.C., Gao G.F., Wu G., Chen W., Shi W., Tan W. Genomic characterisation and epidemiology of 2019 novel coronavirus: implications for virus origins and receptor binding. Lancet. 2020;395(10224):565–574. doi: 10.1016/S0140-6736(20)30251-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hampl V., Herget J., Bibova J., Banasova A., Huskova Z., Vanourkova Z., et al. Intrapulmonary activation of the angiotensin-converting enzyme type 2/angiotensin 1–7/G-protein-coupled Mas receptor axis attenuates pulmonary hypertension in Ren-2 transgenic rats exposed to chronic hypoxia. Physiol. Res. 2015;64(1):25–38. doi: 10.33549/physiolres.932861. [DOI] [PubMed] [Google Scholar]
- 17.Dang Z., Su S., Jin G., Nan X., Ma L., Li Z., et al. Tsantan Sumtang attenuated chronic hypoxia-induced right ventricular structure remodeling and fibrosis by equilibrating local ACE-AngII-AT1R/ACE2-Ang1-7-Mas axis in rat. J. Ethnopharmacol. 2020;250 doi: 10.1016/j.jep.2019.112470. [DOI] [PubMed] [Google Scholar]
- 18.Zhang R., Wu Y., Zhao M., Liu C., Zhou L., Shen S., et al. Role of HIF-1alpha in the regulation ACE and ACE2 expression in hypoxic human pulmonary artery smooth muscle cells. Am. J. Physiol. Lung Cell Mol. Physiol. 2009;297(4):L631–L640. doi: 10.1152/ajplung.90415.2008. [DOI] [PubMed] [Google Scholar]
- 19.Jia H.P., Look D.C., Shi L., Hickey M., Pewe L., Netland J., et al. ACE2 receptor expression and severe acute respiratory syndrome coronavirus infection depend on differentiation of human airway epithelia. J. Virol. 2005;79(23):14614–14621. doi: 10.1128/JVI.79.23.14614-14621.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ren, L.L., Wang, Y.M., Wu, Z.Q., Xiang, Z.C., Guo, L., Xu, T., Jiang, Y.Z., Xiong, Y., Li, Y.J., Li, X.W., Li, H., Fan, G.H., Gu, X.Y., Xiao, Y., Gao, H., Xu, J.Y., Yang, F., Wang, X.M., Wu, C., Chen, L., Liu, Y.W., Liu, B., Yang, J., Wang, X.R., Dong, J., Li, L., Huang, C.L., Zhao, J.P., Hu, Y., Cheng, Z.S., Liu, L.L., Qian, Z.H., Qin, C., Jin, Q., Cao, B., Wang, J.W., 20Identification of a novel coronavirus causing severe pneumonia in human: a descriptive study. Chin. Med. J. (Engl.). https://doi.org/10.1097/CM9. 0000000000000722. [Epub ahead of print].
- 21.Rothan H.A., Byrareddy S.N. The epidemiology and pathogenesis of coronavirus disease (COVID-19) outbreak. J. Autoimmun. 2020;102433 doi: 10.1016/j.jaut.2020.102433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Seclén S., et al. Prevalencia de obesidad, diabetes mellitus, hipertensión arterial e hipercolesterolemia como factores de riesgo coronario y cerebrovascular en población adulta de la costa, sierra y selva del Perú. Acta Medica Perú. 1999 Jul;17(1):8–12. [Google Scholar]
- 23.Segura L, Agusti R, J R. Factores de riesgo de las enfermedades cardiovasculares en el Perú. Estudio TORNASOL. Revista Peruana de Cardiologia Agosto 2006; XXXII(2).
- 24.Woolcott O.O., Castillo O.A., Gutiérrez C., Elashoff R.M., Stefanovski D., Bergman R.N. Inverse association between diabetes and altitude: a cross-sectional study in the adult population of the United States. Obes. Silver Spring Md. 2014;22(9):2080–2090. doi: 10.1002/oby.20800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Seclén S.N., Rosas M.E., Arias A.J., Huayta E., Medina C.A. Prevalence of diabetes and impaired fasting glucose in Peru: report from PERUDIAB, a national urban population-based longitudinal study. BMJ Open Diabetes Res. Care. 2015;3(1) doi: 10.1136/bmjdrc-2015-000110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Woolcott O.O., Gutierrez C., Castillo O.A., Elashoff R.M., Stefanovski D., Bergman R.N. Inverse association between altitude and obesity: a prevalence study among Andean and low-altitude adult individuals of Peru. Obes. Silver Spring Md. 2016 Apr;24(4):929–937. doi: 10.1002/oby.21401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lei Y., Huang X., Lang B., Lan Y., Lu J., Zeng F. Clinical features of imported cases of coronavirus disease 2019 in Tibetan patients in the Plateau area. Med Rxiv. 2020 doi: 10.1101/2020.03.09.20033126. [DOI] [Google Scholar]
- 28.Gelek L. Schools in Tibet to reopen as COVID-19 fears subside. Radio Free Asia. 2020 https://www.rfa.org/english/news/tibet/school-coronavirus-reopen03172020145324.html [Google Scholar]
- 29.Ministerio-de-Comunicación. COVID-19 Bolivia. Gaceta Oficial; 2020. https://www. comunicacion.gob.bo/?q=noticias.
- 30.Gobierno-de-la-Republica-de-Ecuador. Coronavirus Ecuador; 2020. https://coronavirusecuador.com.
- 31.Zubieta-Calleja G. Covid-19 Pandemia Essential Suggestions; 2020. https:// altitudecliniccom/blog/2020/03/covid-19-pandemia-essential-suggestions/.
- 32.Zubieta-Calleja G. Las ventajas de la radiación ultravioleta en el control del coronavirus en la altura. La razon; 2020. https://m.la-razon.com/sociedad/2020/04/05/las-ventajas-de-la-radiacion-ultravioleta-en-el-control-del-coronavirus-en-la-altura/.
- 33.Shanna Ratnesar-Shumate*, Gregory Williams, Brian Green, Melissa Krause, Brian Holland, Stewart Wood, Jordan Bohannon, Jeremy Boydston, Denise Freeburger, Idris Hooper, Katie Beck, John Yeager, Louis A Altamura, Jennifer Biryukov, Jason Yolitz, Michael Schuit, Victoria Wahl, Michael Hevey, Paul Dabisch. Simulated Sunlight Rapidly Inactivates SARS-CoV-2 on Surfaces . National Biodefense Analysis and Countermeasures Center, Operated by BNBI for the US Department of Homeland Security, Frederick, MD, 21702 The Author(s) 2020. Published by Oxford University Press for the Infectious Diseases Society of America. This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial.
- 34.Arias-Reyesa Christian, Zubieta-De-Uriosteb Natalia, Poma-Machicaoa Liliana, Aliaga-Raduana Fernanda, FavioCarvajal-Rodriguez Mathias Dutschmannc, Schneider-Gasserd Edith M., et al. Does the pathogenesis of SARS-CoV-2 virus decrease at high-altitude? Respiratory Physiology & Neurobiology. 2020;207 doi: 10.1016/j.resp.2020.103443. [DOI] [PMC free article] [PubMed] [Google Scholar]