Abstract
Background
Lockdown has been one of the major worldwide strategies to control the spread of coronavirus disease 2019 (COVID-19). Its consequences on the well-being of individuals needs to be better understood. The objective of this work was to evaluate the impact of lockdown on the well-being of a general population and the factors associated with this potential impairment of well-being in a population that has been only lightly affected by COVID-19 such as in Reunion island, an overseas French department.
Methods
An online survey was proposed to the population of Reunion Island between the 35th and 54th days of lockdown relative to pre- and per-lockdown periods. Well-being was measured by the 5-item World Health Organization Well-Being Index, with some questions about sleep habits (Pittsburgh questionnaire), weekly physical activity (IPAQ), health, and lifestyle.
Results
Four hundred volunteers answered the survey. They reported a 15.7% decrease in well-being (p < 0.001), accompanied by increased anxiety (p < 0.001), decreased weekly physical activity (p < 0.001), delayed and poorer quality sleep (p < 0.001). Multivariate logistical analysis showed that impairment in well-being during lockdown was independently associated with an increase in anxiety (odds ratio (OR): 4.77 (3.26–6.98), p < 0.001), decrease in weekly physical activity (OR: 0.58 (0.43–0.79), p < 0.001), and poor-quality sleep (OR: 0.29 (0.19–0.43), p < 0.001).
Conclusions
This study suggested an impairment in well-being during lockdown, associated with anxiety, lack of physical activity and sleep disruptions. Public policies must consider these factors as levers for improving the well-being of the population in order to effectively combat the spread of COVID-19.
Keywords: COVID-19, Lockdown, Well-being, Sleep, Physical activity, Anxiety
1. Introduction
In the absence of effective treatment for coronavirus disease 2019 (COVID-19), lockdown appeared as an effective strategy to control its spread [1]. The French government applied strict lockdown measures for 54 days, reducing the spread of the disease in France, COVID-19 hospitalizations and deaths [2]. Mental health problems are one of the main causes of disease burden in the world [3], and the lockdown has short- and long-term negative psychological effects [4]. It is therefore essential to know how to limit its deleterious effects.
People who were isolated for two weeks due to contact with MERS patients suffered from high rates of anxiety symptoms and anger during isolation, and showed mental health effects even at four to six months after removal from isolation.
Mental health could be defined as a state of well-being [5,6]. During COVID-19 lockdown, where daily rhythms are disrupted and freedom of movement and assembly are limited, physical inactivity [7], stress [8] and sleep disturbances [9] can be a source of mental discomfort. In France, freedom of movement has been limited to basic necessities, essential medical appointments, and professional travel that cannot be replaced by teleworking [10]. Individual outside physical activity (PA) was still possible within the limit of 1 h daily and within a maximum 1-km area around the home. A clear understanding of the impact of COVID-19 lockdown effects could provide a lever to improve the well-being and improve effectiveness of lockdown and public policies against COVID-19 spread.
Accordingly, the objective of this work was to investigate the impact of lockdown and its related factors on well-being in the general population. We hypothesized that sleep habits and weekly physical activity would contribute to well-being impairment during lockdown.
2. Methods
2.1. Study sample
An online survey was proposed to the adult population (age ≥ 18 y) of Reunion island between the 35th and 54th days of lockdown. Four hundred volunteers answered the online survey. This study was applied according to the rules of the French Data Protection Authority (CNIL) and all subjects gave their written informed consent to participate.
2.2. Online survey
Responders were asked to answer all questions applying to himself/herself twice, when considering the last month before and during the lockdown. The 5-item World Health Organization Well-Being (WHO-5) index was proposed to participants to measure their subjective well-being. The overall WHO-5 score was rated from 0 (absence of well-being) to 100 (maximal well-being) [6]. This questionnaire has presented a good internal consistency, with a Cronbach coefficient alpha of 0.84 in the general population [11]. Six items of the Pittsburgh Sleep Quality Index (PSQI) were selected and included one question about sleep quality, one about sleep latency, and those about sleep duration, bedtime and morning awakening [12]. This questionnaire has shown an adequate internal consistency (Cronbach coefficient alpha of 0.69) [13]. Responders were also asked if they frequently felt anxious, using a scale ranging from never to always (including 6 levels). The level of PA during work and leisure was investigated using selected questions from the International Physical Activity Questionnaire (IPAQ) [14]. These questions evaluated the duration and frequency of moderate and intense PAs. Energy expenditure was assumed to correspond to 4 METs/min for moderate PA and 6 METs/min for intense PA [14,15]. Sociodemographic and lifestyle information were collected.
2.3. Statistical analyses
All statistical analyses were performed using Statview® software (SAS Institute, Inc., Cary, NC, USA).
Answers concerning the before and during lockdown periods were compared using two-sided Wilcoxon, two-sided repeated-measures analyses of variance (RM-ANOVA), or Pearson's two-sided χ2 test when appropriate. Effect size was calculated based on eta squared for the parametric variables, Cramer's V for the nominal variables, and the ratio z to the square root of the sample for the nonparametric variables.
Adjusted multivariate logistic regression analyses were performed to explain overall WHO-5 indexes in quartiles, expressed as odds ratio (OR) and using a 95% confidence interval (95%CI), including as independent variables: body mass index, work status under lockdown, age, sex, presence of chronic disease, changes in anxiety, sleep, and PA during lockdown. Significance was set at p < 0.05.
3. Results
Out of all responders (233 women, age: 29.8 ± 11.5 y), none of them reported being infected by COVID-19. A majority (362, 90.5%) were working or students before lockdown. During lockdown, 198 (61%) worked at home, 40 (11.0%) worked at their usual workplace, 15 (4.2%) worked at both, and 73 (20.2%) lost their activity. The majority of responders (393 subjects, 98.3%) reported a good health prior to lockdown. Sixty-eight responders reported having chronic diseases including respiratory, cardiovascular, cancer, or metabolic diseases.
The analysis revealed a decrease in overall WHO-5 score by 15.7% (Table 1 ), greater anxiety scores, and significant changes in sleep habits during lockdown: the responders went to bed later, fell asleep later and woke up later in the morning. They also reported longer night sleep with more frequent and longer naps, but with a decrease in sleep quality. There was an increase in time spent in the sitting position, a decrease in weekly PA, a slight decrease in moderate weekly PA, and a higher decrease in intense weekly PA.
Table 1.
Changes in anxiety, weekly physical activity, sleep habits and quality before and during COVID-19 lockdown.
| Before Lock-down |
During Lock-down |
Difference | Effect size | P | |||
|---|---|---|---|---|---|---|---|
| Mean | Standard deviation | Mean | Standard deviation | ||||
| 5-WHO well-being index (/100) | 70.9 | 17.0 | 55.2 | 21.0 | −15.7 | 0.30 | <0.001 |
| Sleep duration (h) | 7.5 | 1.2 | 7.8 | 1.7 | −0.3 | 0.04 | <0.001 |
| Bedtime (h) | 22.5 | 1.0 | 24.2 | 1.9 | −1.7 | 0.49 | <0.001 |
| Morning awakening (h) | 6.7 | 1.6 | 8.7 | 2.2 | 2.0 | 0.45 | <0.001 |
| Nap duration (min) | 1.2 | 0.6 | 1.7 | 0.9 | 0.5 | 0.29 | <0.001 |
| Overall physical activity (METs-min/week) | 2466 | 1853 | 1788 | 1558 | −678 | 0.14 | <0.001 |
| Moderate physical activity (METs-min/week) | 709 | 621 | 614 | 589 | −95 | 0.03 | <0.001 |
| Intense physical activity (METs-min/week) |
1757 |
1507 |
1174 |
1261 |
−583 |
0.16 |
<0.001 |
| Median |
Interquartile range |
Median |
Interquartile range |
Difference |
Effect size |
p |
|
| Sitting time (h) | 4.5 | 3.0 | 7.5 | 8.0 | 3.0 | 0.58 | <0.001 |
| Sleep latency (min) | 20 | 30 | 30 | 45 | 10 | 0.54 | <0.001 |
| n | % | n | % | Difference |
Effect size | p | ||
|---|---|---|---|---|---|---|---|---|
| n | % | |||||||
| Nap frequency | ||||||||
| never | 184 | 46.0 | 185 | 46.2 | 1 | 0.2 | 0.36 | <0.001 |
| sometimes | 195 | 48.8 | 155 | 38.8 | −40 | −10.0 | ||
| Everyday | 21 | 5.2 | 60 | 15.0 | 39 | 9.8 | ||
| Anxiety | ||||||||
| Never | 80 | 20.0 | 55 | 13.8 | −25 | −6.2 | 0.36 | <0.001 |
| sometimes | 202 | 50.5 | 200 | 50.0 | −2 | −0.5 | ||
| Often | 99 | 24.8 | 113 | 28.2 | 14 | 3.4 | ||
| Always | 19 | 4.7 | 32 | 8.0 | 13 | 3.3 | ||
| Sleep quality | ||||||||
| very bad | 8 | 2.0 | 101 | 25.2 | 93 | 23.2 | 0.22 | <0.001 |
| fairly bad | 82 | 20.5 | 120 | 30.0 | 38 | 9.5 | ||
| fairly good | 230 | 57.5 | 92 | 23.0 | −138 | −34.5 | ||
| Very good | 80 | 20.0 | 87 | 21.8 | 7 | 1.8 | ||
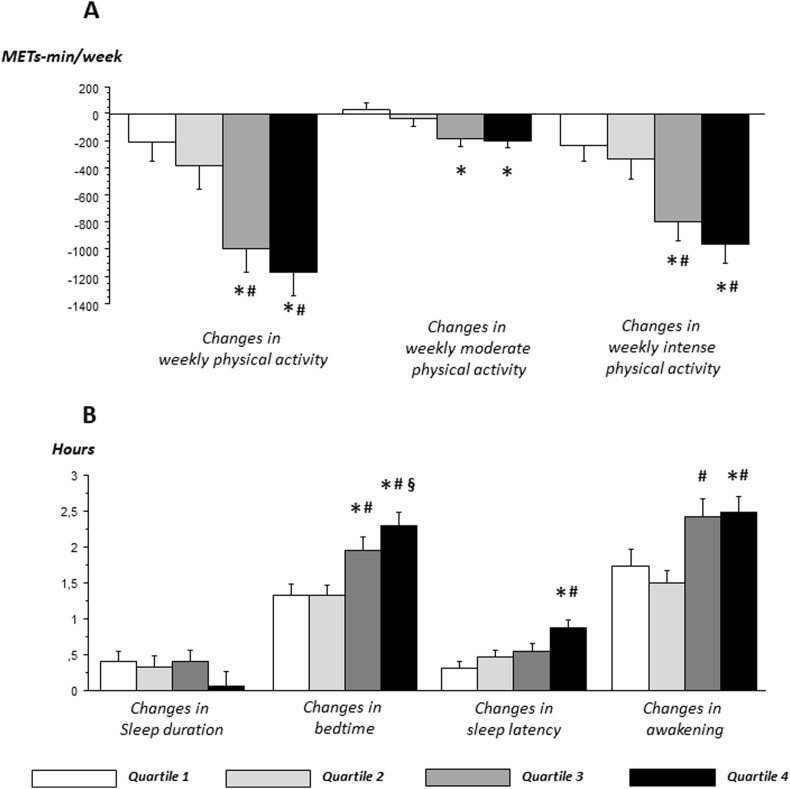
Those reporting the highest decrease in well-being (fourth and third quartiles) also reported the highest decrease in their total (p < 0.05), moderate (p < 0.05) and intense (p < 0.05) weekly PAs (Fig. 1 A). They also reported the greatest impairments in anxiety (p < 0.05), sleep quality (p < 0.05), bedtime (p < 0.05), sleep latency (p < 0.05), and morning awakening (p < 0.05) (Fig. 1B). Adjusted multivariate logistical analyses revealed that the impairment in well-being in those individuals was independently associated with age, a reduction in weekly PA, an increase in anxiety, and a poor sleep quality (Table 2 ).
Fig. 1.
Relationship between physical activity, sleep and individual well-being during COVID-19 lockdown. A) Changes in reported overall, moderate and intense physical activities according to well-being quartiles. Energy expenditure is assumed to be a combination of 4 METs/min for moderate physical activity and 6 METs/min for intense physical activity. B) Changes in reported bedtime, sleep duration, and time of awakening according to well-being quartiles. It is interesting to note the close relationship between well-being, physical activity and sleep patterns: individuals who reported an alteration in their well-being are those who also reported a reduction in their physical activity and a delay and lengthening of their sleep.∗: p < 0.05 in comparison with first quartile, #: p < 0.05 in comparison with second quartile and §: p < 0.05 in comparison with third quartile.
Table 2.
Odds ratios (OR) for change in well-being with the COVID-19 containment according to WHO-5 score quartiles (95% confidence interval, 95% CI).
| Crude OR (95%CI) | p | Adjusted OR (95%CI) | p | ||
|---|---|---|---|---|---|
| Age | 1st quartile | 1 | – | 1 | – |
| 2nd quartile | 1.02 (1.00–1.04) | 0.114 | 1.02 (0.98–1.05) | 0.367 | |
| 3rd quartile | 1.04 (1.02–1.07) | <0.001 | 1.04 (1.01–1.08) | 0.020 | |
| 4th quartile | 1.07 (1.04–1.10) | <0.001 | 1.07 (1.02–1.12) | 0.003 | |
| Changes in bedtime | 1st quartile | 1 | – | 1 | – |
| 2nd quartile | 1.18 (0.82–1.70) | 0.381 | 0.90 (0.71–1.12) | 0.336 | |
| 3rd quartile | 1.30 (0.94–1.81) | 0.113 | 1.09 (0.88–1.36) | 0.424 | |
| 4th quartile | 1.60 (1.18–2.18) | 0.002 | 1.17 (0.92–1.50) | 0.205 | |
| Changes in sleep duration | 1st quartile | 1 | – | 1 | – |
| 2nd quartile | 0.99 (0.84–1.18) | 0.950 | 1.08 (0.84–1.38) | 0.549 | |
| 3rd quartile | 1.01 (0.85–1.18) | 0.965 | 1.15 (0.92–1.44) | 0.222 | |
| 4th quartile | 0.87 (0.74–1.03) | 0.104 | 1.06 (0.83–1.35) | 0.610 | |
| Changes in sleep latency | 1st quartile | 1 | – | 1 | – |
| 2nd quartile | 0.95 (0.79–1.16) | 0.630 | 1.00 (0.99–1.01) | 0.678 | |
| 3rd quartile | 1.20 (1.01–1.42) | 0.035 | 1.00 (0.99–1.00) | 0.275 | |
| 4th quartile | 1.39 (1.19–1.64) | <0.001 | 1.00 (0.99–1.01) | 0.449 | |
| Changes in sleep quality | 1st quartile | 1 | – | 1 | – |
| 2nd quartile | 0.60 (0.46–0.79) | <0.001 | 0.58 (0.41–0.81) | 0.001 | |
| 3rd quartile | 0.43 (0.33–0.57) | <0.001 | 0.40 (0.28–0.57) | <0.001 | |
| 4th quartile | 0.29 (0.21–0.40) | <0.001 | 0.29 (0.19–0.43) | <0.001 | |
| Changes in physical activity | 1st quartile | 1 | – | 1 | – |
| 2nd quartile | 0.74 (0.59–1.94) | 0.011 | 0.72 (0.55–0.94) | 0.015 | |
| 3rd quartile | 0.68 (0.55–0.85) | <0.001 | 0.68 (0.52–0.89) | 0.005 | |
| 4th quartile | 0.57 (0.46–0.71) | <0.001 | 0.58 (0.43–0.79) | <0.001 | |
| Changes in anxiety | 1st quartile | 1 | – | 1 | – |
| 2nd quartile | 1.65 (1.27–2.14) | <0.001 | 1.90 (1.38–2.63) | <0.001 | |
| 3rd quartile | 2.31 (1.75–3.05) | <0.001 | 2.95 (2.09–4.17) | <0.001 | |
| 4th quartile | 3.61 (2.68–4.86) | <0.001 | 4.77 (3.26–6.98) | <0.001 |
Adjustment for sex, age, body mass index, chronic disease, and work status during lockdown, plus all variables presented in the Table. It can be noted that age, physical activity, sleep quality and anxiety since lockdown are independently associated with impairment of individual well-being.
Significant quartiles are shown in bold.
4. Discussion
The current study sought to study the effect of lockdown on the mental health of the Reunion island population. Our results suggested a deep impairment in well-being during lockdown, associated with several independent factors including age, anxiety, lack of PA and disrupted sleep.
Mental health has both positive and negative dimensions: the positive dimension refers to notions of well-being and coping skills; while the negative one includes psychological distress and psychiatric disorders [6]. Thus, mental health is not considered as only the absence of depression/anxiety symptoms but also as some degree of psychological well-being [11]. Moreover, a subjective definition of well-being has the quality of being correlated with both economic [5] and neurobiological aspects [16]. Studying mental well-being by the WHO-5 index is a strategy for understanding what individuals experience. Two thresholds are considered: a threshold ≤50 is used to detect patients suffering from depression and a change in threshold of 10 points on the WHO-5 scale marks a clinical change [6]. Here, a major decrease in the WHO-5 scores seemed to appear during lockdown in Reunion (Fig. 1A), exceeding these thresholds were 131 (32%) responders who reported a WHO-5 score ≤50 (vs. 77 (19%) before lockdown). Accordingly, a recent Chinese study showed that COVID-19 lockdown affected the psychological health of the population in Hubei province, including more depression, anxiety and impaired well-being [17]. More generally, previous studies on isolation have shown short- and long-term negative psychosocial effects [4], mainly following isolation in response to severe acute respiratory syndrome in 2003. Consistent with COVID-19 lockdown observations, these studies mainly described a high prevalence of various symptoms of psychological distress and negative responses, including fear, sadness, emotional disturbance, depression, stress, low mood, irritability, or anger [4]. In the long term, these subjects were at risk to report anxiety, alcohol abuse or dependency and post-traumatic stress symptoms [18].
Sedentary behaviors expose populations to well-known risks related to insufficient PA, including cardiovascular or psychological risks [19]. Here, we observed that responders reported a decrease in their weekly overall, moderate and intense PAs (Fig. 1B); which was also independently correlated with a deterioration in their well-being (Table 1). These results are consistent with two recent studies about COVID-19 lockdown in Portugal [20] and Belgium [21], in which both reported a decrease in energy expenditure during COVID-19 lockdown. We can therefore think that the lack of PA is a determining factor in the well-being under lockdown.
Sleep habits were previously proposed as lifestyle factors that could be an important component of mental health during lockdown [22]. We observed that most individuals reported longer and shifted sleeps. This shift in the sleep habits was associated with impaired well-being in our study (Fig. 1C, Table 1). This result is consistent with longitudinal, transversal or experimental studies revealing that reduced or disrupted sleep is a risk factor for depression and anxiety [23]. Changes in the duration or timing of light exposure, the lack of PA, and absence or disruptions of socioprofessional synchronizers have the potential to desynchronize circadian rhythms, affect mood [24], and finally contribute to the impairment of well-being. Thus, it is reasonable to suppose that disruption of circadian rhythms would contribute to impairment in sleep quality and well-being.
Taken together, these results suggest that measures and advice to promote PA at home or outside, as was the case in France (1 h/d and close to home), or advice on sleep hygiene could improve the well-being of populations during lockdown. Finally, it can be thought that improving the well-being of individuals during lockdown may allow them to better comply with the rules of the lockdown and may help to better fight against the spread of COVID-19.
There are several limitations of the present study. The relatively small sample size may limit to the generalizability of these results. However, these results are consistent with previously published studies [17,20,21]. The study population was relatively young, although age has been found to be an important factor in well-being impairment in this population. Thus, the possibility emerges that older populations may have a greater impairment in well-being than has been reported in the current study and previous ones. This issue needs to be explored in future work.
5. Conclusion
In an anxiety provoking context such as COVID-19 lockdown, limitation of PAs and sleep disturbances could contribute to an alteration in well-being, reaching clinical threshold in a large proportion of responders. The public policies put in place must consider these factors as levers for improving the well-being of the population in order to effectively combat the spread of COVID-19.
Authorship contribution statement
FC: Conceptualization, Investigation, Methodology, Data analysis, Writing original draft; MA: Conceptualization, Investigation, Methodology, Review & editing; TC: Conceptualization, Methodology, Review & editing; NT: Conceptualization, Methodology, Review & editing; NC: Conceptualization, Methodology, Review & editing; GD: Conceptualization, Methodology, Supervision, Review & editing.
Footnotes
None of the authors has any conflict of interest to disclose.
The ICMJE Uniform Disclosure Form for Potential Conflicts of Interest associated with this article can be viewed by clicking on the following link: https://doi.org/10.1016/j.sleep.2020.09.014.
Conflict of interest
The following is the supplementary data related to this article:
Multimedia component 1
References
- 1.Gregori D., Azzolina D., Lanera C. A first estimation of the impact of public health actions against COVID-19 in Veneto (Italy) J Epidemiol Community Health. 2020;74(10):858–860. doi: 10.1136/jech-2020-214209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Salje H., Tran Kiem C., Lefrancq N. Estimating the burden of SARS-CoV-2 in France. Science. 2020;369(6500):208–211. doi: 10.1126/science.abc3517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Whiteford H.A., Degenhardt L., Rehm J. Global burden of disease attributable to mental and substance use disorders: findings from the Global Burden of Disease Study 2010. Lancet Lond Engl. 2013;382:1575–1586. doi: 10.1016/S0140-6736(13)61611-6. [DOI] [PubMed] [Google Scholar]
- 4.Brooks S.K., Webster R.K., Smith L.E. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet Lond Engl. 2020;395:912–920. doi: 10.1016/S0140-6736(20)30460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Oswald A.J., Wu S. Objective Confirmation of Subjective Measures of Human Well-Being: Evidence from the U.S.A. Science. 2010;327:576–579. doi: 10.1126/science.1180606. [DOI] [PubMed] [Google Scholar]
- 6.Topp C.W., Østergaard S.D., Søndergaard S. The WHO-5 Well-Being Index: A Systematic Review of the Literature. Psychother Psychosom. 2015;84:167–176. doi: 10.1159/000376585. [DOI] [PubMed] [Google Scholar]
- 7.McMahon E.M., Corcoran P., O'Regan G. Physical activity in European adolescents and associations with anxiety, depression and well-being. Eur Child Adolesc Psychiatr. 2017;26:111–122. doi: 10.1007/s00787-016-0875-9. [DOI] [PubMed] [Google Scholar]
- 8.Malone C., Wachholtz A. The Relationship of Anxiety and Depression to Subjective Well-Being in a Mainland Chinese Sample. J Relig Health. 2018;57:266–278. doi: 10.1007/s10943-017-0447-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tang N.K.Y., Fiecas M., Afolalu E.F. Changes in Sleep Duration, Quality, and Medication Use Are Prospectively Associated With Health and Well-being: Analysis of the UK Household Longitudinal Study. Sleep. 2017;40 doi: 10.1093/sleep/zsw079. [DOI] [PubMed] [Google Scholar]
- 10.Épidémie Coronavirus (Covid-19) -Confinement : ce qui est interdit, ce qui est permis, service-public.fr. https://www.service-public.fr/particuliers/actualites/A13922 March 24th 2020.
- 11.Bech P., Olsen L.R., Kjoller M. Measuring well-being rather than the absence of distress symptoms: a comparison of the SF-36 Mental Health subscale and the WHO-Five well-being scale. Int J Methods Psychiatr Res. 2006;12:85–91. doi: 10.1002/mpr.145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Buysse D.J., Reynolds C.F., Monk T.H. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28:193–213. doi: 10.1016/0165-1781(89)90047-4. [DOI] [PubMed] [Google Scholar]
- 13.Spira A.P., Beaudreau S.A., Stone K.L. Reliability and validity of the Pittsburgh Sleep Quality Index and the Epworth Sleepiness Scale in older men. J Gerontol A Biol Sci Med Sci. 2012;67:433–439. doi: 10.1093/gerona/glr172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Craig C.L., Marshall A.L., Sjöström M. International physical activity questionnaire: 12-country reliability and validity. Med Sci Sports Exerc. 2003;35:1381–1395. doi: 10.1249/01.MSS.0000078924.61453.FB. [DOI] [PubMed] [Google Scholar]
- 15.Ainsworth B.E., Haskell W.L., Herrmann S.D. 2011 Compendium of Physical Activities: a second update of codes and MET values. Med Sci Sports Exerc. 2011;43:1575–1581. doi: 10.1249/MSS.0b013e31821ece12. [DOI] [PubMed] [Google Scholar]
- 16.Urry H.L., Nitschke J.B., Dolski I. Making a life worth living: neural correlates of well-being. Psychol Sci. 2004;15:367–372. doi: 10.1111/j.0956-7976.2004.00686.x. ht. [DOI] [PubMed] [Google Scholar]
- 17.Ahmed M.Z., Ahmed O., Aibao Z. Epidemic of COVID-19 in China and associated Psychological Problems. Asian J Psychiatry. 2020;51:102092. doi: 10.1016/j.ajp.2020.102092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jeong H., Yim H.W., Song Y.-J. Mental health status of people isolated due to Middle East Respiratory Syndrome. Epidemiol Health. 2016;38 doi: 10.4178/epih.e2016048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Margaritis I., Houdart S., El Ouadrhiri Y. How to deal with COVID-19 epidemic-related lockdown physical inactivity and sedentary increase in youth? Adaptation of Anses' benchmarks. Arch Publ Health. 2020;78 doi: 10.1186/s13690-020-00432-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Antunes R., Frontini R., Amaro N. Exploring Lifestyle Habits, Physical Activity, Anxiety and Basic Psychological Needs in a Sample of Portuguese Adults during COVID-19. Int J Environ Res Publ Health. 2020;17 doi: 10.3390/ijerph17124360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Constandt B., Thibaut E., De Bosscher V. Exercising in Times of Lockdown: An Analysis of the Impact of COVID-19 on Levels and Patterns of Exercise among Adults in Belgium. Int J Environ Res Publ Health. 2020;17 doi: 10.3390/ijerph17114144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kokou-Kpolou C.K., Megalakaki O., Laimou D. Insomnia during COVID-19 pandemic and lockdown: Prevalence, severity, and associated risk factors in French population. Psychiatry Res. 2020;290:113128. doi: 10.1016/j.psychres.2020.113128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ben Simon E., Vallat R., Barnes C.M. Sleep Loss and the Socio-Emotional Brain. Trends Cognit Sci. 2020;24:435–450. doi: 10.1016/j.tics.2020.02.003. [DOI] [PubMed] [Google Scholar]
- 24.Rajaratnam S.M., Arendt J. Health in a 24-h society. Lancet Lond Engl. 2001;358:999–1005. doi: 10.1016/S0140-6736(01)06108-6. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Multimedia component 1