Abstract
Purpose
To quantify the shrinking in outpatient and intravitreal injections’ volumes in a tertiary referral retina unit secondary to virus causing coronavirus disease 2019 (COVID-19).
Methods
In this retrospective cross-sectional study, we reviewed the charts of all patients who had a visit at a medical retina referral center during the Italian quarantine (from 9th of March 2020 to 3rd of May 2020). Number and characteristics of these data were compared with data from the same period in 2019 (from 9th of March 2019 to 3rd of May 2019).
Results
In the 2019 study period, there were 303 patients attending clinic (150 males, 153 females). In the 2020 study period, patients decreased to 75 (48 males, 27 females; P = 0.022 comparing gender prevalence between the two periods) with an overall reduction of 75.2%. Mean ± SD age was 71.4 ± 14.3 years (range 25–93 years) in the 2019 study period and 66.7 ± 13.1 years (range 32–91 years) in the 2020 study period (P = 0.005). The largest drop in outpatient volume was recorded in AMD patients (− 79.9%). Regarding the intravitreal treatments, there were 1252 injections in the 2019 period and 583 injections in the 2020 period (− 53.6% in injections). The drop in intravitreal treatments was larger in patients with posterior uveitis, retinal vein occlusion, and diabetes (− 85.7%, − 61.9%, and − 59.6%, respectively).
Conclusion
The volume of outpatient visits and intravitreal injections declined during the COVID-19 quarantine. The short- and long-term impacts are that routine in-person visits and intravitreal injections are expected to increase after the quarantine and, even more, after the pandemic.
Keywords: COVID-19, Retina, Intravitreal injections, Outpatient visits
Introduction
The severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2)—the virus causing coronavirus disease 2019 (COVID-19)—has been quickly infecting an increasing amount of people worldwide [1]. On March 11, 2020, the World Health Organization (WHO) has formally declared the COVID-19 outbreak as a pandemic. As a consequence, governments have established wide ranging control measures to reduce transmission of COVID-19 and thus to diminish pressure on health systems. Most countries initially adopted travel bans from specific locations (e.g., China), which was followed with the establishment of quarantine measures. As an example, the Italian government had placed the whole country under quarantine for 56 days (8 weeks, March 9, 2020 to May 3, 2020). People were forbidden from assembling in public places and were recommended to keep at least 1-m distance from each other, and restaurants, pubs, and shopping centers—except for pharmacies and food markets—were obligated to remain close. Moreover, a generalized shutdown of the Italian production system was imposed. Finally, people were restricted in movements except for necessity, work, and health circumstances.
The COVID-19 pandemic has drastically modified how outpatient care is given in healthcare practices. To reduce the chance of transmitting the virus to either patients or healthcare personnel, providers are deferring elective and preventive visits, and outpatient visits have been restricted to more urgent care [2–5]. Symmetrically, many patients are also postponing visits in order to avoid being exposed. Furthermore, adopted restrictions in traveling are also influencing both provider and patient behavior. Based on a survey done at Harvard University, while this reduction in outpatient volume has widely affected all medical and surgical specialties, the drop of in-person visits was overall larger among surgical specialties such as ophthalmology, which actually resulted as the most affected with a 79% decrease in the number of outpatient volume [6].
The COVID-19-related contraction in outpatient volume might have significant repercussions on the visual outcome of patients usually referring to retina units, as the number of injections and a failure to visit clinicians and undergo optical coherence tomography (OCT) were demonstrated to be associated with worse outcomes in patients with retinal disorders, including age-related macular degeneration (AMD) [7] and diabetic retinopathy [8].
The aim of this report was therefore to provide a quantification of the COVID-19-related drop in outpatient and intravitreal injections’ volume in a tertiary referral retina unit. More importantly, we examined patient characteristics and their associations with this decrease.
Methods
In this retrospective cross-sectional study, the authors reviewed the charts of all patients who had a visit at the “medical retina and imaging” unit of San Raffaele hospital (Milan, Italy) during the Italian quarantine (from 9th of March 2020 to 3rd of May 2020). Number and characteristics of these data were compared with data from the same period in 2019 (from 9th of March 2019 to 3rd of May 2019). Written informed consent was obtained from all subjects, and it was approved by the San Raffaele Ethics Committee. The study adhered to the tenets of the Declaration of Helsinki and Health Insurance Portability and Accountability Act.
All enrolled patients had a complete ophthalmologic evaluation, including the assessment of best corrected visual acuity (BCVA) and dilated fundus examination.
Statistical calculations were performed using Statistical Package for Social Sciences (version 20.0, SPSS Inc., Chicago, IL, USA).
To detect departures from normal distribution, a Shapiro-Wilk’s test was performed for all variables. Means and standard deviation (SD) were computed for all quantitative variables. Continuous variables were compared by conducting a Student’s t test for independent variables. Statistical significance of the differences between groups for qualitative variables was assessed using Fisher’s exact test. A P value < 0.05 was determined to be statistically significant.
Results
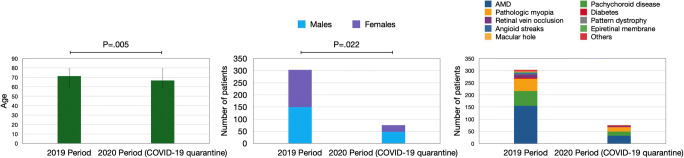
In the 2019 study period, there were 303 patients attending our clinic (150 males, 153 females). In the 2020 study period, patients decreased to 75 (48 males, 27 females (P = 0.022 comparing gender rates between the two periods) overall reduction of 75.2%). Clinical and demographic characteristics of enrolled patients are presented in Table 1 and Fig. 1. Mean ± SD age was 71.4 ± 14.3 years (range 25–93 years) in the 2019 study period and 66.7 ± 13.1 years (range 32–91 years) in the 2020 study period (P = 0.005). Mean ± SD visual acuity was 0.3 ± 0.5 LogMAR in the 2019 cohort and 0.3 ± 0.5 LogMAR in the 2020 cohort (P = 0.663).
Table 1.
Characteristics of patients undergoing in-person visits during the study periods
| Characteristic | 2019 period | 2020 period (COVID-19 quarantine) | Change |
|---|---|---|---|
| Number of patients, n (%) | 303 (100.0%) | 75 (100.0%) | − 75.2% |
| Gender, n (%) | 150 (49.5%) males, 153 (50.5%) females | 48 (64.0%%) males, 27 (36.0%) females | – |
| Mean age, mean ± SD | 71.4 ± 14.3 | 66.7 ± 13.1 | – |
| Main disease, n (%) | |||
| AMD | 155 (51.1%) | 32 (42.7%) | − 79.9% |
| Pachychoroid disease | 61 (20.1%) | 17 (22.7%) | − 60.7% |
| Pathologic myopia | 50 (16.5%) | 18 (24.0%) | − 49.6% |
| Diabetes | 5 (1.7%) | 2 (2.7%) | − 60.0% |
| Retinal vein occlusion | 13 (4.3%) | 4 (5.3%) | − 69.2% |
| Pattern dystrophy | 2 (0.7%) | 0 (0.0%) | − 100.0% |
| Angioid streaks | 4 (1.3%) | 0 (0.0%) | − 100.0% |
| Epiretinal membrane | 4 (1.3%) | 0 (0.0%) | − 100.0% |
| Macular hole | 2 (0.7%) | 0 (0.0%) | − 100.0% |
| Others | 7a (2.3%) | 2b (2.7%) | − 71.4% |
aMultiple evanescent white dot syndrome (n = 1), Irvine–Gass syndrome (n = 1), Sorsby macular dystrophy (n = 1), macular telangiectasia type 2 (n = 1), punctate inner choroidopathy (n = 1), optic nerve astrocytoma (n = 1), idiopathic macular neovascularization (n = 1)
bIdiopathic macular neovascularization (n = 1), punctate inner choroidopathy (n = 1)
n number of patients, SD standard deviation, AMD age-related macular degeneration
Fig. 1.
Bar charts showing comparisons between outpatient volumes in the 2019 and 2020 study periods. (Left) Error-bar chart displaying study cohorts’ ages in the two study groups. The height of the bars corresponds to the mean value, while the error bars represent the standard deviation (SD) of the data. Groups’ ages significantly differ between groups (P = 0.005). (Middle and right) Stacked bar charts showing the contribution of different sub-groups to each separate category in the two study periods. (Middle) The difference in gender prevalence was statistically significant (P = 0.022) between the two groups. (Right) The largest drop in outpatient volume was recorded in AMD patients (− 79.9%)
These cohorts were divided into subgroups according to the ocular disorder affecting patients. In our retinal clinic, most patients were affected by AMD (155 and 32 patients, in the 2019 and 2020 study periods, respectively). Importantly, in a post hoc analysis considering only disorders affecting at least 5 patients in the 2019 study period, the largest drop in outpatient volume was recorded in AMD patients (− 79.9%). Conversely, the smallest decrease in outpatient volume was documented in patients with pathologic myopia (− 49.6%).
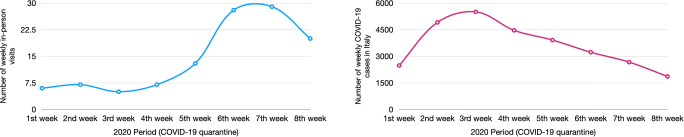
Figure 2 displays the weekly volume of outpatient visits during the COVID-19 quarantine in 2020, relative to the weekly incidence of new confirmed cases of COVID-19 in Italy. The number of in-person visits was higher in the last 3 weeks of quarantine, as compared with the previous weeks. Inversely, the incidence of COVID-19 cases tended to be descending in the last 4 weeks of quarantine.
Fig. 2.
Weekly volume of outpatient visits during the COVID-19 Italian quarantine in 2020 (left), relative to the weekly incidence of new COVID-19 cases (right). The number of in-person visits was higher in the last 3 weeks of quarantine. Inversely, the incidence of COVID-19 cases tended to be descending in the last 4 weeks of quarantine
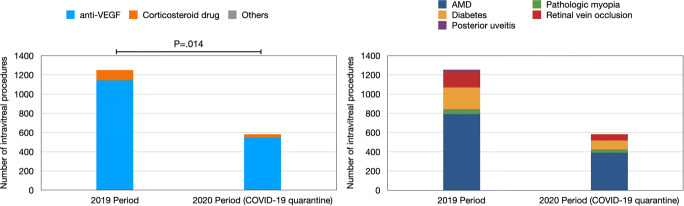
Regarding the intravitreal treatments, there were 991 patients (1252 injections) undergoing procedures in the 2019 period and 457 patients (583 injections) having therapy in the 2020 period (− 53.9% and − 53.6% reductions in number of patients and injections, respectively) (Table 2, Fig. 3). No differences in terms of age (P = 0.878) and gender prevalence (P = 1.0) were detected between the two groups.
Table 2.
Characteristics of patients treated intravitreally during the study periods
| Characteristic | 2019 period | 2020 period (COVID-19 quarantine) | Change |
|---|---|---|---|
| Treated patients | |||
| Number of patients, n (%) | 991 (100.0%) | 457 (100.0%) | − 53.9% |
| Gender, n (%) | 469 (47.3%) males, 522 (52.7%) females | 227 (%) males, 230 (%) females | – |
| Mean age, mean ± SD | 71.1 ± 11.7 | 72.0 ± 12.7 | – |
| Performed procedures | |||
| Total number of intravitreal procedures, n (%) | 1252 (100.0%) | 583 (100.0%) | − 53.6% |
| Drug, n (%) | |||
| anti-VEGF | 1143 (91.3%)a | 551 (94.5%)d | − 51.7% |
| Corticosteroid medication | 107 (8.5%)b | 32 (5.5%)e | − 70.1% |
| Others | 2 (0.2%)c | 0 | − 100.0% |
| Main disease, n (%) | |||
| AMD | 791 (63.2%) | 392 (67.2%) | − 50.4% |
| Myopia | 51 (4.1%) | 33 (5.7%) | − 35.3% |
| Diabetes | 228 (18.2%) | 92 (15.8%) | − 59.6% |
| Retinal vein occlusion | 168 (13.4%) | 64 (11.0%) | − 61.9% |
| Posterior uveitis | 14 (1.2%) | 2 (0.3%) | − 85.7% |
aBevacizumab (n = 0), ranibizumab (n = 621), aflibercept (n = 522)
bDexamethasone implant (Ozurdex®) (n = 97), fluocinolone acetonide implant (Iluvien®) (n = 10)
cOcriplasmin (Jetrea®) (n = 1), rituximab (n = 1)
dBevacizumab (n = 385)*, ranibizumab (n = 82), aflibercept (n = 84)
eDexamethasone implant (Ozurdex®) (n = 32)
n number of patients or eyes, SD standard deviation, VEGF vascular endothelial growth factor, AMD age-related macular degeneration
*After September 2019, bevacizumab becomes the only reimbursable drug in Lombardy—i.e., where this study was conducted—for patients with neovascular AMD
Fig. 3.
Bar charts showing comparisons between intravitreal injections’ volumes in the 2019 and 2020 study periods. Stacked bar charts showing the contribution of different sub-groups to each separate category in the two study periods. (Left) The type of medication was different in terms of prevalence between the two study groups (P = 0.014) with a largest drop in corticosteroid injections during the 2020 study period. (Right) The largest reduction in intravitreal treatments was recorded in patients with posterior uveitis, retinal vein occlusion, and diabetes (− 85.7%, − 61.9%, and − 59.6%, respectively)
Of note, while the COVID-19 pandemic has caused a wide shrinking in intravitreal treatments, this drop was larger for corticosteroid intravitreal injections (− 70.1%) than for anti-VEGF treatments (− 51.7%, P = 0.014 in the comparison between the two study periods). Finally, during quarantine, the drop in intravitreal treatments was larger in patients with posterior uveitis, retinal vein occlusion, and diabetes (− 85.7%, − 61.9%, and − 59.6%, respectively), as compared with patients with AMD and myopia (− 50.4% and − 35.3%).
Discussion
In this report we investigated the contraction in outpatient volume and intravitreal injections in a referral retina unit during the COVID-19 Italian quarantine. Overall, we demonstrated that the COVID-19 pandemic significantly shrank both the in-person visit and intravitreal procedure volumes.
This shrinking in outpatient volume may be related to different factors.
First, ophthalmology teams have adopted new ways of working to minimize risk to patients and staff at the same time as optimizing treatment and care of ocular disorders. In details, ophthalmology departments conceived risk-stratification guidelines to decide if patients needed to be visited in-person or could be deferred [2, 3]. Such guidelines were also consequent to shortages of personal protective equipment (PPE) and absence of well-established protocols that might reduce personnel risk. Also, COVID-19 infections among health workers have been dramatically contracting the numbers of available staff.
Second, patients were also limited in traveling between regions and this may have limited their capability to attend visits and intravitreal treatments.
Third, many patients also postponed visits as fears of exposure to COVID-19 are causing people to avoid hospital help. This was confirmed by our analysis demonstrating a relative increase in outpatient volume in the last three weeks of quarantine, which was also characterized by a significant reduction in COVID-19 weekly new cases.
Importantly, our report demonstrated a significant reduction in average age among patients undergoing visits during the 2020 COVID-19 quarantine, as compared with the same period in 2019. Furthermore, among patients who presented during the COVID-19 period from March 9 through May 3, 2020, the prevalence of AMD was lower than among those who presented during the pre–COVID-19 period (from March 9 through May 3, 2019). Taken our results together, we may conclude that outpatient care in older patients, who are more likely affected by AMD, was more significantly impacted by the COVID-19 pandemic. The latter finding was presumably related to a higher frequency of visits’ postponements in older patients who are known to be at higher risk for severe illness from COVID-19 [9]. Of note, our analysis was limited in that we were not able to appropriately investigate the reduction in outpatient volume among patients with retinal vascular disorders (e.g., diabetic retinopathy), as these patients usually refer to another unit in the same department (“retinal vascular disorder” unit). However, we thought that the safest strategy was to compare the outcome volume within the same unit in order to have a better comprehension of the true change between periods. Interestingly, we also found a relative higher decrease in outpatient volume in female patients than in males. The latter finding is somewhat surprising assuming that COVID-19 tends to affect men more severely than it does to women [9]. These results might be secondary to the fact that women have a higher frequency of visits’ postponement as they are more worried about the spread of the infection than men, as suggested by recent surveys on British [10] and Australian [11] citizens. Finally, visual acuities were similar in the two periods, this suggesting that a lower vision was not a determining factor for patients to attend visits.
Although quarantine measures are limited in time, the COVID-19 pandemic could last about 2 years. For this reason, efforts to reduce shrinking in outpatient volume are underway. First, administrators have been relocating ophthalmology teams and services away from departments caring for patients with COVID-19. This may reduce patients’ fears of exposure to COVID-19. In addition, patients’ care has been partially switched to online or phone consultations. However, essential examination elements such as visual acuity assessment, ophthalmoscopy, and OCT can be assessed only in person. Work has been done to execute these investigations remotely, but is not set for application.
In our study, we also evaluated the decrease in intravitreal injections’ volume during the COVID-19 quarantine. Our analysis involved all those patients undergoing intravitreal injections, regardless of the unit they were referred (e.g., “retina” unit, “retinal vascular disorders” unit, “uveitis” unit, etc.). We demonstrated a significant decrease in number of intravitreal injections during the COVID-19 period from March 9 through May 3, 2020. More importantly, the decline in intravitreal injections was larger for patients with retinal vascular disorders (e.g., diabetes and retinal vein occlusions) and for corticosteroid medications. Taking into consideration that patients with diabetes and cardiovascular comorbidities are at higher risk of worse outcomes with COVID-19, these results confirm that the decrease in ophthalmology care is more accentuated within fragile patients. Furthermore, patients with diabetic retinopathy were also demonstrated to have a worse therapy compliance compared with AMD patients [12]. The latter finding might have been accentuated during the COVID-19 pandemic. Finally, eyes under corticosteroid medications do not usually experience sudden visual changes and therefore may less likely require prompt treatments.
Limitations of this study include the analysis of a single community setting in northern Italy, which to date is one of the most affected regions worldwide. Future studies will investigate the impact of COVID-19 pandemic in areas where the diffusion of this disease remains low. Furthermore, although it is reasonable to expect an increase in outpatients’ volume at the end of quarantine, we did not evaluate this aspect. However, clinics adopted different protocols after quarantine and therefore we thought the safest approach to describe the reduction in outpatient volume during this period was to compare it with the same period in the previous year.
In conclusion, in a tertiary referral retina unit, the volume of outpatient visits and intravitreal injections declined during the Covid-19 quarantine. The short- and long-term impacts are that routine in-person visits and intravitreal injections are expected to increase after the quarantine and, even more, after the pandemic. Therefore, ophthalmology clinics should be ready for a “rebound” effect. More importantly, future longitudinal studies will be designed to clarify the impact of this contraction on patients’ outcomes.
Funding
No funding was received for this research.
Compliance with ethical standards
Conflict of interest
Francesco Bandello is a consultant for Alcon (Fort Worth, Texas, USA), Alimera Sciences (Alpharetta, Georgia, USA), Allergan Inc. (Irvine, California, USA), Farmila-Thea (Clermont-Ferrand, France), Bayer Shering-Pharma (Berlin, Germany), Bausch And Lomb (Rochester, New York, USA), Genentech (San Francisco, California, USA), Hoffmann-La-Roche (Basel, Switzerland), Novagali Pharma (Évry, France), Novartis (Basel, Switzerland), Sanofi-Aventis (Paris, France), Thrombogenics (Heverlee, Belgium), and Zeiss (Dublin, USA). Giuseppe Querques is a consultant for Alimera Sciences (Alpharetta, Georgia, USA), Allergan Inc. (Irvine, California, USA), Amgen (Thousand Oaks, USA), Bayer Shering-Pharma (Berlin, Germany), Heidelberg (Germany), KBH (Chengdu, China), LEH Pharma (London, UK), Lumithera (Poulsbo, USA), Novartis (Basel, Switzerland), Sandoz (Berlin, Germany), Sifi (Catania, Italy), Sooft-Fidea (Abano, Italy), and Zeiss (Dublin, USA). The other authors have no disclosures.
Ethical approval
This article does not contain any studies with animals performed by any of the authors. All procedures performed in studies involving human participants were in accordance with the ethical standards of the (place name of institution and/or national research committee) and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Footnotes
This is part of a topical collection on Perspectives on COVID-19.
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72 314 cases from the Chinese Center for Disease Control and Prevention. JAMA. 2020;323(13):1239–1242. doi: 10.1001/jama.2020.2648. [DOI] [PubMed] [Google Scholar]
- 2.Parravano M, Borrelli E, Costanzo E, et al. Protect healthcare workers and patients from COVID-19: the experience of two tertiary ophthalmology care referral centers in Italy. Ophthalmol Ther Jun. 2020;9(2):231–234. doi: 10.1007/s40123-020-00251-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Borrelli E, Sacconi R, Querques L, et al. Taking the right measures to control COVID-19 in ophthalmology: the experience of a tertiary eye care referral center in Italy. Eye. 2020;34(7):1175–1176. doi: 10.1038/s41433-020-0880-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Corradetti G, Corvi F, Nguyen TV, Sadda SR. Management of neovascular age-related macular degeneration during the COVID-19 pandemia. Ophthalmol Retin. 2020;S2468-6530(20):30207–30204. doi: 10.1016/j.oret.2020.05.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Iovino C, Caporossi T, Peiretti E (2020) Vitreoretinal surgery tip and tricks in the era of COVID-19. Graefes Arch Clin Exp Ophthalmol. 10.1007/s00417-020-04800-x [DOI] [PMC free article] [PubMed]
- 6.Mehrotra A, Chernew M, Linetsky D, Cutler D (2020) The impact of the COVID-19 pandemic on outpatient visits: a rebound emerges https://www.commonwealthfund.org/publications/2020/apr/impact-covid-19-outpatient-visits. Accessed 12 Jul 2020
- 7.Holz FG, Tadayoni R, Beatty S, et al. Key drivers of visual acuity gains in neovascular age-related macular degeneration in real life: findings from the AURA study. Br J Ophthalmol. 2016;100(12):1623–1628. doi: 10.1136/bjophthalmol-2015-308166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gross JG, Glassman AR, Liu D, et al. Five-year outcomes of panretinal photocoagulation vs intravitreous ranibizumab for proliferative diabetic retinopathy: a randomized clinical trial. JAMA Ophthalmol. 2018;136(10):1138–1148. doi: 10.1001/jamaophthalmol.2018.3255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zhou F, Yu T, Du R, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395(10229):1054–1062. doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.(2020) COVID-19 research | MARCH. https://www.marchnetwork.org/research. Accessed 22 May 2020
- 11.(2020) COVID-19 and Canadians’ state of mind: worried, lonely, and expecting disruption for at least 2 to 3 months . https://abacusdata.ca/coronavirus-covid19-abacus-data-mood-polling/. Accessed 22 May 2020
- 12.Weiss M, Sim DA, Herold T, et al. Compliance and adherence of patients with diabetic macular edema to intravitreal anti-vascular endothelial growth factor therapy in daily practice. Retina. 2018;38(12):2293–2300. doi: 10.1097/IAE.0000000000001892. [DOI] [PubMed] [Google Scholar]