Abstract
This report presents the details of a case of sight-threatening injury in the right eye of a 77-year-old man which was caused by the venom of the Asian giant hornet (Vespa mandarinia). The patient was not stung, rather the venom was sprayed into his eye. Although the injured eye was washed as a first aid treatment, persistent corneal defect, corneal endothelial decompensation, iris atrophy, pupil dilation, and mature cataract were observed and a hand movement visual acuity was recorded 8 weeks after the injury. Since a slight a-wave was detected in his electroretinogram (ERG) result after the corneal epithelial defect had healed, we performed cataract surgery and Descemet stripping automated endothelial keratoplasty (DSAEK). After the DSAEK, the cornea of the right eye became clearer; however, the visual acuity of his right eye did not improve. Fundus examination revealed branch retinal artery occlusion but no optic disc atrophy. ERG showed that the a-wave amplitude of the injured eye recorded after the surgery was almost half of that of the fellow eye. The iris atrophy and mature cataract show that the sprayed Vespa venom of the Asian giant hornet can permeate into the intraocular area even without stinging. Whether the venom directly affects retinal function is unclear, but the decreased a-wave of the injured eye shows that the venom caused damage of retinal function in some way. Irrigation of the anterior chamber as well as eye washing is needed as a first aid treatment in similar cases.
Keywords: Vespa mandarinia, Ocular injury, Sprayed venom, Bullous keratopathy, Electroretinogram
Introduction
Ocular injury caused by the sting of an insect of the Vespa species is a rare occurrence that can lead to sight-threatening complications including keratitis, bullous keratopathy, uveitis, iris atrophy, cataract, glaucoma, and optic neuritis [1, 2, 3, 4, 5]. These complications are mainly caused by the venom, which is a mixture of biological amines (histamine, serotonin, dopamine, noradrenaline), low-molecular-weight peptides, major protein subunits, and enzymes (hyaluronidase, phospholipase A, B) [6, 7], and the severity of the ocular injury depends on the depth of the stings [5, 8]. However, we recently treated a case of severe ocular injury by the venom of the Asian giant hornet (Vespa mandarinia); the patient was not stung, rather the venom was sprayed into his eye. This report presents the details of the case.
Case Report
A 77-year-old man, a bee feeder, was injured in his right eye by the sprayed venom of the Asian giant hornet (V. mandarinia; Fig. 1) in early October. His right eye was washed with physiological saline as a first aid treatment on the same day and treated with steroid and antibiotic eye drops by the nearest ophthalmologist; however, the corneal epithelial defect persisted, lenticular opacity increased, and pupil dilation occurred as the atrophy of the iris progressed. He was referred to the Cornea Service of Fujita Health University Bantane Hospital in late November of the same year for further management and treatment.
Fig. 1.
A bottle of Hachi-zake (hornet liquor), in which Asian giant hornets are soaked in brandy, that the patient brought for one of the authors (K.H.). This is drunk as a nourishing tonic.
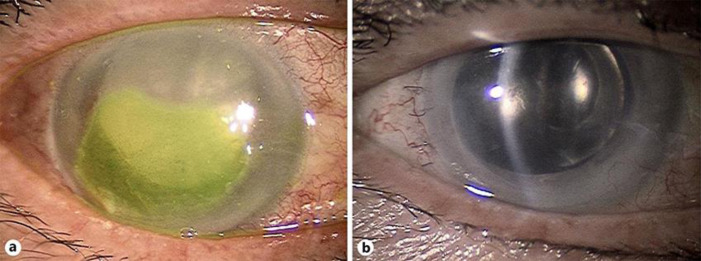
On initial examination, his best corrected visual acuity (decimal) was hand movement (uncorrectable) for the right eye and 0.7 (with 1.2 × +1.5 D) for the left eye. The intraocular pressure of the right eye could not be measured, whereas that of the left eye was 12 mm Hg. Epithelial edema with an epithelial defect of 8 × 4 mm was observed on the right cornea. The thickened cornea and the presence of folds of Descemet's membrane with pigmentary keratic precipitates suggested corneal endothelial decompensation (Fig. 2a). The iris of the right eye was depigmented and irregularly dilated. The fundus of the right eye could not be examined because of the hazy cornea and the presence of mature cataract.
Fig. 2.
a Anterior segment findings of the injured eye under diffuse illumination at the patient's first visit. The cornea is hazy with stromal and epithelial edema and persistent corneal epithelial defect (stained by fluorescein). The pupil is dilated, and mature cataract can be seen. b Four months after DSAEK. Depigmented iris with dilated pupil indicates past history of severe iritis. DSAEK, Descemet stripping automated endothelial keratoplasty.
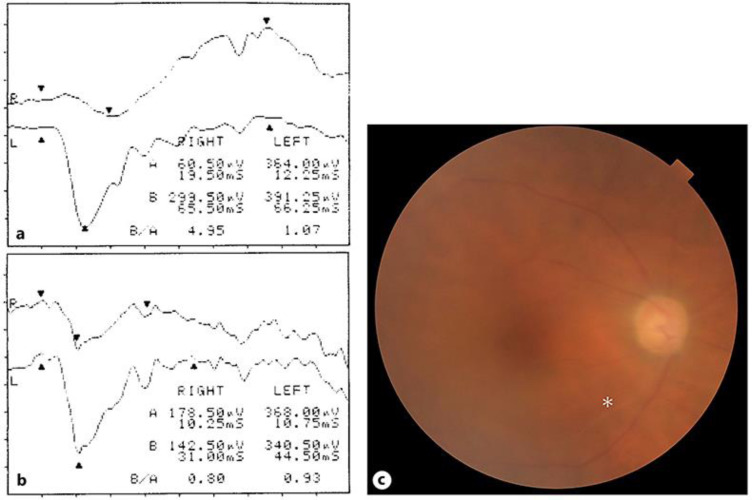
Detectable electroretinogram (ERG) waveforms recorded 3 months after the first visit, when the corneal epithelial defect had healed, suggested that the residual retinal function had some potential for visual improvement after cataract surgery. However, the amplitude was decreased (60.50 μV for the right eye and 364.00 μV for the left eye) and the implicit time was delayed (19.50 ms for the right eye and 12.25 ms for the left eye) in the a-wave (Fig. 3a). Since the corneal edema with epithelial bulla remained after phacoemulsification and aspiration and intraocular lens implantation, corneal endothelial transplantation (Descemet stripping automated endothelial keratoplasty [DSAEK]) was performed on the right eye about 1 year after the injury.
Fig. 3.
a ERG recorded before the cataract surgery. The ERG of the right eye shows a reduced amplitude and prolonged implicit time in the a-wave compared with that of the left eye. b ERG of the right eye 4 months after DSAEK. Improvement is seen in the amplitude and the implicit time due to the improved transparency of the ocular media. c Fundus photograph taken 4 months after DSAEK. Though the image of the fundus is hazy because of the residual corneal stromal edema, the color of the retina looks normal and there are no signs of atrophy in the optic disc, but a ghost vessel can be seen in the lower temporal area (asterisk). DSAEK, Descemet stripping automated endothelial keratoplasty; ERG, electroretinogram.
After DSAEK, the cornea of the right eye became clearer, even though the stromal edema remained (Fig. 2b). His vision got better subjectively, but the visual acuity of his right eye did not improve. The ERG results recorded after phacoemulsification and aspiration and intraocular lens implantation plus DSAEK (Fig. 3b) showed an increased amplitude and faster implicit time of the a-wave compared with that recorded before the surgery; however, the a-wave amplitude after the surgery was almost half of that of the fellow eye. Fundus examination revealed branch retinal artery occlusion (Fig. 3c, asterisk), but optic disc atrophy was not observed.
The apparent corneal edema in the right eye began 7 months after DSAEK, and the cornea became hazy with signs of neovascularization 1 year after DSAEK. Since no significant improvement in visual acuity was recorded after DSAEK, probably due to the damage in retinal function, we decided not to perform a second DSAEK.
Discussion
The Vespa species are widely distributed in the tropical and temperate zones of the eastern Asian area. V. mandarinia is the largest insect of the Vespa species, with a body length of 30 and 40 mm, and has the most toxic venom of the hymenopteran insects [9]. They build nests in wooden caves or underground in the suburbs, and to defend their nests against intruders, they attack not only by stinging but by spraying venom from their stingers [10]. The larva of the Vespa insect is an edible and valuable source of protein in the mountainous region of central Japan, and in some areas of Japan, the imagoes are soaked in spirits for medical liquor (Hachi-zake) (Fig. 1). Therefore, the worst natural enemies of Vespa species are humans and bears, which also eat larvae. For these enemies, their attack is mainly aimed at glossy black targets, including a human's head, a bear's nose, and the corneas of these mammals. The toxicity of the venom is strongest in the autumn season (September and October in Japan) when the insects start nesting and parenting, and the occurrence of sting injuries is highest in this season. With the expansion of human residential areas, the chances of getting closer to the nesting area of the Vespa species and the incidence of these ocular injuries will get higher.
Ocular trauma caused by the Vespa species occurs not only when the insect stings the victim but also if the venom is sprayed. The severity of an ocular injury caused by the venom of an insect of the Vespa species varies depending on the depth of the invasion of the toxin; therefore, the visual prognosis is relatively better if the venom is sprayed into the eye without stinging [11]. In the present case, however, persistent corneal epithelial defect, corneal endothelial decompensation, iris atrophy and pupil dilation, mature cataract, and damage to the retina and optic nerve were all observed in the injured eye even though the venom was sprayed into the eye without stinging. We could not obtain information about the pH of Vespa venom from the literature, but as it contains small peptides represented by wasp kinin and some nonenzymatic proteins with neurotoxic effects have a relatively low molecular weight [6, 7, 9, 10], some toxic agents may easily permeate from the cornea into the intraocular area. Since the toxicity of the insect venom is strongest in the autumn season, anterior chamber irrigation, not just eye washing [11, 12], should have been performed first in this case.
After the cataract surgery and DSAEK, the visual acuity of the injured eye did not improve, even though transparency should be guaranteed after these procedures. This is probably due to the neurotoxic effect of the venom [9], which may have penetrated from the cornea to the ocular sensory system, or as is shown in Figure 3c, another toxic mechanism worked to obstruct the retinal vessels. It is believed that surgical removal of mature cataract and corneal opacity may lead to improvement of the ERG waveform [13]. However, the branch retinal artery occlusion and/or toxic effect caused retinal damage, resulting in a lower a-wave amplitude compared with the fellow eye.
In conclusion, the present case was one of an ocular injury caused by the sprayed venom of V. mandarinia. Despite the eye washing administered as first aid treatment, persistent corneal epithelial defect, corneal endothelial decompensation, iris atrophy and pupil dilation, mature cataract, and damage to the retina and optic nerve occurred and led to visual loss. The Vespa venom can permeate into intraocular area even without stinging; in similar cases, irrigation of the anterior chamber should be considered as first aid treatment in addition to eye washing.
Statement of Ethics
This study was approved by the Research Ethics Committee of Fujita Health University and complies with the Declaration of Helsinki guidelines. Written informed consent was obtained from the patient for the surgery and for reporting the clinical course of his case.
Conflict of Interest Statement
The authors have no conflict of interest to declare.
Funding Sources
This work was supported by a grant from the Fujita Gakuen Research Fund and a Alcon Japan Research grant.
Author Contributions
K. Hirano followed up the patient, performed DSAEK, and mainly wrote the manuscript. A. Tanikawa analyzed the recorded ERG and contributed to the statements on retinal findings and function; he also provided critical advice during preparation of the manuscript.
Acknowledgement
We thank Dr. Masako Matsuura, MD, PhD for offering the chance to perform the DSAEK in Matsuura Eye Clinic (Ichinomiya, Aichi, Japan). We would also like to thank Editage (www.editage.com) for English language editing.
References
- 1.Gilboa M, Gdal-On M, Zonis S. Bee and wasp stings of the eye. Retained intralenticular wasp sting: A case report. Br J Ophthalmol. 1977 Oct;61((10)):662–4. doi: 10.1136/bjo.61.10.662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Arcieri ES, França ET, de Oliveria HB, De Abreu Ferreira L, Ferreira MA, Rocha FJ. Ocular lesions arising after stings by hymenopteran insects. Cornea. 2002 Apr;21((3)):328–30. doi: 10.1097/00003226-200204000-00019. [DOI] [PubMed] [Google Scholar]
- 3.Im JC, Kang YK, Park TI, Shin JP, Kim HK. Sympathetic ophthalmia after wasp sting. Korean J Ophthalmol. 2015 Dec;29((6)):435–6. doi: 10.3341/kjo.2015.29.6.435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kim JM, Kang SJ, Kim MK, Wee WR, Lee JH. Corneal wasp sting accompanied by optic neuropathy and retinopathy. Jpn J Ophthalmol. 2011 Mar;55((2)):165–7. doi: 10.1007/s10384-010-0912-z. [DOI] [PubMed] [Google Scholar]
- 5.Ono T, Iida M, Mori Y, Nejima R, Iwasaki T, Amano S, et al. Outcomes of bee sting injury: comparison of hornet and paper wasp. Jpn J Ophthalmol. 2018 Mar;62((2)):221–5. doi: 10.1007/s10384-018-0563-z. [DOI] [PubMed] [Google Scholar]
- 6.Habermann E. Bee and wasp venoms. Science. 1972 Jul;177((4046)):314–22. doi: 10.1126/science.177.4046.314. [DOI] [PubMed] [Google Scholar]
- 7.Edery H, Ishay J, Lass I, Gitter S. Pharmacological activity of oriental hornet (Vespa orientalis) venom. Toxicon. 1972 Jan;10((1)):13–25. doi: 10.1016/0041-0101(72)90085-2. [DOI] [PubMed] [Google Scholar]
- 8.Razmjoo H, Abtahi MA, Roomizadeh P, Mohammadi Z, Abtahi SH. Management of corneal bee sting. Clin Ophthalmol. 2011;5:1697–700. doi: 10.2147/OPTH.S26919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Abe T, Kawai N, Niwa A. Purification and properties of a presynaptically acting neurotoxin, mandaratoxin, from hornet (Vespa mandarinia) Biochemistry. 1982 Mar;21((7)):1693–7. doi: 10.1021/bi00536a034. [DOI] [PubMed] [Google Scholar]
- 10.Ono M, Terabe H, Hori H, Sasaki M. Insect signalling: components of giant hornet alarm pheromone. Nature. 2003 Aug;424((6949)):637–8. doi: 10.1038/424637a. [DOI] [PubMed] [Google Scholar]
- 11.Koh N, Chiba K, Kikuchi M, Senoo T, Chigusa Y. Case report of vesicular keratitis and cataract caused by bee venom without sting [Atarashii Ganka] J Eye. 2008;25((4)):549–52. [Google Scholar]
- 12.Nishiyama K, Totsuka S. Corneal stings of vespa [Nippon Ganka Kiyo] Folia Ophthalmol Jap. 1984;35((8)):1486–94. [Google Scholar]
- 13.Galloway NR. Electrophysiological testing of eyes with opaque media. Eye (Lond) 1988;2((Pt 6)):615–24. doi: 10.1038/eye.1988.114. [DOI] [PubMed] [Google Scholar]