Abstract
Background
Wuhan, the epicenter of the coronavirus disease 2019 outbreak, was locked down on January 23, 2020. We aimed to investigate the barriers to the physical prevention, negative attitudes, and anxiety levels.
Methods
A online cross-sectional survey was conducted with the people living in Wuhan between March 12th and 23rd, 2020.
Results
Of a total of 2411 complete responses, the mean and standard deviation for the total physical prevention barriers score was 19.73 (standard deviation ± 5.3; range 12−45) out of a possible score of 48. Using a cut-off score of 44 for the State-Trait Inventory score, 79.9% (95% confidence interval [CI]: 78.2−81.5) of the participants reported moderate to severe anxiety during the early phase of the outbreak, and 51.3% (95% CI 49.2−53.3) reported moderate to severe anxiety after the peak of coronavirus disease 2019 was over (during the study period). Comparing anxiety levels in the early phase of the outbreak and after the peak of the outbreak, 58.5% (95% CI 56.5−60.5) recorded a decreased anxiety. Females reported a higher likelihood of having decreased levels of anxiety than males (odds ratio = 1.78, 95% CI 1.48−2.14). Low negative attitudes score were associated with a higher decrease in anxiety (odds ratio = 1.59, 95% CI 1.33−1.89).
Conclusions
The attitudinal barriers to prevention of transmission of coronavirus disease 2019 are more prominent than physical prevention barriers after the peak of coronavirus disease 2019. High anxiety levels even after the peak warrant serious attention.
Key words: new coronavirus, physical, barriers, adherence, prevention
Introduction
Late December of 2019, an epidemic of coronavirus disease 2019 (COVID-19) spread rapidly from Wuhan, Hubei Province, China.1 , 2 Since then, the Chinese government has taken unprecedented public health measures to contain the outbreak. The epicenter has been under complete lockdown since January 23, 2020. In just 2 months after the lockdown of the epicenter and concerted efforts—including a combination of nationwide restrictions on movement, early detection and isolation—the new infection rate has started to decline and remains at a low level in China. On March 12, 2020, mainland China reported that the peak of the outbreak of COVID-19 in the country is over,3 hours after the World Health Organization declared the epidemic a pandemic.4 As of March 23, a total of 81,601 people had tested positive for coronavirus in mainland China, whereas the death toll rose to 3,276.5
Although mainland China has seen a slowing down in the COVID-19 infection and death rates, continuity in practices of infection prevention and control are needed to effectively curb and prevent the rebound of the outbreak. As effective COVID-19 treatments and the vaccine to prevent the novel coronavirus are yet to be available, the society at large should continue to sustain preventive practices to further contain the outbreak and prevent its re-emergence. In addition to physical prevention measures, addressing negative attitudes toward COVID-19 infection remains an important aspect of the management and control of the outbreak. The coronavirus outbreak has affected scores of global populations. The highly contagious and fatal cases have provoked considerable negative attitudes, such as embarrassment, social stigma, and discriminatory behavior against people with COVID-19 infection. Infectious disease negative attitudes have been recognized as major barriers to timely and effective health care or treatment-seeking.6 , 7 In addition, it may also affect the emotion and mental well-being of a person.8 Therefore, efforts to combat the new coronavirus should include addressing both the physical and the attitudinal barriers to adherence to precautions for preventing the transmission.
The COVID-19 pandemic is presenting a great challenge to the mental wellness of the people in China, especially in Wuhan which was placed under strict lockdown.9 Likewise, the pandemic also causes unprecedented mental health burden in the United States,10 United Kingdom,11 and many Western European countries.12, 13, 14 One of the early studies conducted in China assessing mental well-being during the early phase of the COVID-19 outbreak revealed that more than half of the public rated the psychological impact as moderate to severe.15 Nevertheless, the study was conducted in 194 cities throughout China, and information on the psychological well-being of people in the epicenter of the outbreak is currently lacking. The escalating outbreak that lasted for nearly 2 months before its peak was deemed to have caused deep-rooted psychological distress to the public, especially in the city of Wuhan. Now that the outbreak has ceased, it remains unclear what the extent of the consequences of the traumatic ordeals of COVID-19 on the public. Posttraumatic distress has been recognized as an important public health concern after a traumatic event, as it may cause various functional impairments, including a person's work ability and daily performance.16 , 17 The previous SARS outbreak evidenced serious consequences of long-term psychiatric morbidities among the survivors.18 Currently, there is no known information on the psychological aftermath of the COVID-19 outbreak either in the epicenter or in other cities outside the epicenter. There is an urgent need for the timely identification of people who are suffering from the psychological aftermath of the COVID-19 outbreak. A timely understanding of the mental well-being of the public is important to inform mental health interventions in response to this crucial need.
Given the aforementioned, a survey was conducted among the people living in Wuhan and aimed at investigating the barriers to preventive measures against COVID-19 infection, the negative attitudes toward COVID-19 infection, and their anxiety levels. As mental health may influence other aspects of everyday life, this study also investigates the association between anxiety levels, barriers in preventive measures, and negative attitudes toward COVID-19.
Methods
Study Design and Participants
We conducted a cross-sectional, Web-based survey using an online questionnaire between March 12th and 23rd, 2020. The inclusion criteria were that the respondents were residents of Wuhan between the ages of 18 and 70 years.
Procedures
The researchers used the social network, WeChat (the most popular messaging app in China), to circulate the survey link to the residents of Wuhan. When participants completed the survey, they received a note to encourage them to disseminate the survey link to all their contacts. The participants were informed that their participation was voluntary, and consent was implied through their completion of the questionnaire. The questionnaire was developed in English and was then translated into Chinese. Local experts validated the content of the questionnaire, after which it was pilot-tested. The survey consisted of 3 sections, which assessed i) demographic background, ii) barriers to prevention measures, iii) negative attitude toward COVID-19, and iv) anxiety levels.
Barriers to Prevention Measures
The questions about preventive barriers consisted of 5 sections (12 items) that comprised questions about personal protection (4-item), cough etiquette (4-item), contact precautions (2-item), voluntary quarantine (1-item), and prompt reporting (1-item). The question queried participants' level of difficulties in practicing physical prevention measures. The response option was on a 4-point Likert scale, with the items scored as 1 (very easy), 2 (easy), 3 (difficult), or 4 (very difficult). The possible total physical prevention barriers score ranged from 4 to 48, with higher scores representing higher difficulty levels of physical prevention.
Negative Attitudes
Negative attitudes consisted of questions about feelings of fear, avoidance, keeping a secret, embarrassment, and stigma associated with COVID-19 (5-item). Optional answers were on a 4-point Likert scale, with the items scored as 1 (strongly disagree), 2 (disagree), 3 (agree), or 4 (strongly agree). The possible total negative attitudes score ranged from 4 to 20, with higher scores representing higher levels of negative attitudes.
Anxiety Levels
The 6-item state version of the State-Trait Anxiety Inventory (STAI-6) assessing anxiety levels that was used in this study was adapted from previous studies.19 , 20 The participants rated the frequency of experiencing 6 emotional states, namely being calm, tense, upset, relaxed, content, and worried, concerning the current COVID-19 outbreak. The participants were asked to rate their current level of anxiety (defined as anxiety levels after the peak) and their anxiety level during the early phase of the outbreak (during the first week of the lockdown). A 4-point scale was used (1 = not at all, 2 = somewhat, 3 = moderately, 4 = very much). The scores on the 3 positively worded items were reverse-coded. The total summed scores were prorated (multiplied by 20/6) to obtain scores that were comparable with those from the full 20-item STAI (giving a range from 20 to 80).20 A cut-off score of 44 was used to indicate moderate to severe symptoms.21 , 22 The differences in the level of anxiety levels were calculated. Participants were grouped into (1) having current anxiety levels lower than during the early phase of the outbreak—which was defined as having decreased anxiety levels—and (2) having current anxiety levels similar or higher than the early phase of the outbreak.
Statistical Analyses
The reliability of the physical and attitudinal preventive barrier items were evaluated by assessing the internal consistency of the items representing the scores. The 12 items for physical and 5 items for attitudinal preventive barrier scores had a reliability (Cronbach's α) of 0.870 and 0.889, respectively. The reliability computed for STAI-6 items in the assessment of anxiety levels after the peak and in the early phase of the outbreak were 0.778 and 0.833, respectively. Multivariable logistic regression analysis, using a simultaneous forced-entry method, was used to determine the demographic factors influencing physical prevention barriers and negative attitudes. The influence of physical prevention barriers and negative attitudes on the decrease in anxiety level comparing after the peak with the early phase of the outbreak was also examined using multivariable logistic regression analysis. Odds ratios (ORs), 95% confidence intervals (95% CIs), and P values were calculated for each independent variable. All statistical analyses were performed using the Statistical Package for the Social Sciences, version 20.0 (IBM Corp., Armonk, NY). The level of significance was set at P < 0.05.
Ethical Approval
The study protocol was approved by the Research Ethics Committee of the Fujian Medical University. Respondents were informed that their participation was voluntary, and consent was implied on the completion of the questionnaire.
Results
A total of 2411 complete responses were received. As shown in the first and second column of Table 1 , slightly over half of the participants were females (55.6%), and the highest educational level was university (51.3%). Slightly over 1 one-third (37.2%) of the participants were aged 31–50 years. Distribution by income groups shows that most of the participants were earning an average monthly income below CNY50,000 (43.5%) and between CNY50,000 and 120,000 (31.9%).
Table 1.
Physical Prevention Barriers and Negative Attitudes by Demographics (N = 2411)
| Covariates | N (%) | Univariate analysis |
Multivariable analysis |
Univariate analysis |
Multivariable analysis |
||
|---|---|---|---|---|---|---|---|
| High prevention physical barriers score (18–45) (n = 1250) | P value | OR (95% CI) score 18–45 vs. low score | High negative attitudes score 11–20 (n = 1348) | P value | OR (95% CI) high score vs. low score | ||
| Age group (y) | |||||||
| 18–30 | 761 (31.6) | 500 (65.7) | 1.87 (1.42–2.46)∗∗∗ | 430 (56.5) | Reference | ||
| 31–50 | 897 (37.2) | 446 (49.8) | P < 0.001 | 1.21 (0.96–1.51) | 454 (50.6) | P < 0.001 | 0.87 (0.69–1.09) |
| 51–70 | 753 (31.2) | 304 (40.4) | Reference | 464 (61.6) | 1.53 (1.17–1.99)∗∗ | ||
| Gender | |||||||
| Male | 1070 (44.4) | 659 (61.6) | P < 0.001 | 1.55 (1.29–1.86) | 672 (62.8) | P < 0.001 | 1.42 (1.19–1.71)∗∗∗ |
| Female | 1341 (55.6) | 591 (44.1) | Reference | 676 (50.4) | Reference | ||
| Highest educational level | |||||||
| Secondary school and below | 442 (18.3) | 215 (48.8) | 0.94 (0.71–1.24) | 237 (53.6) | |||
| High school | 731 (30.3) | 316 (43.2) | P < 0.001 | 0.80 (0.64–1.00) | 402 (55.0) | 0.347 | |
| University | 1238 (51.3) | 719 (58.1) | Reference | 709 (57.3) | |||
| Occupational category | |||||||
| Health professional | 81 (3.4) | 34 (42.0) | Reference | 45 (55.6) | Reference | ||
| Food handling workers/farmers | 217 (9.0) | 115 (53.0) | 1.54 (0.88–2.68) | 140 (64.5) | 1.36 (0.80–2.32) | ||
| Industrial workers | 615 (25.5) | 388 (63.1) | 2.48 (1.50–4.08)∗∗ | 409 (66.5) | 1.37 (0.84–2.21) | ||
| Office workers | 546 (22.6) | 293 (53.7) | P < 0.001 | 1.70 (1.04–2.80)∗ | 259 (47.4) | P < 0.001 | 0.67 (0.41–1.09) |
| Housewife/Retiree | 783 (32.5) | 328 (41.9) | 1.95 (1.18–3.23)∗∗ | 432 (55.2) | 0.93 (0.57–1.51) | ||
| Students | 169 (7.0) | 92 (54.4) | 1.45 (0.82–2.56) | 63 (37.3) | 0.47 (0.27–0.81)∗∗ | ||
| Average annual household income (CNY) | |||||||
| <50,000 | 1049 (43.5) | 444 (42.4) | Reference | 570 (54.3) | Reference | ||
| 50,000–120,000 | 769 (31.9) | 409 (53.2) | P < 0.001 | 1.52 (1.23–1.86)∗∗∗ | 389 (50.6) | P < 0.001 | 0.99 (0.82–1.22) |
| >120,000 | 593 (24.6) | 397 (66.9) | 2.01 (1.56–2.60)∗∗∗ | 389 (65.6) | 1.79 (1.40–2.28)∗∗∗ | ||
| Locality | |||||||
| Urban | 1865 (77.4) | 884 (47.4) | P < 0.001 | Reference | 1015 (54.4) | P < 0.001 | Reference |
| Suburban/Rural | 546 (22.6) | 366 (67.2) | 2.12 (1.70–2.65) | 333 (61.0) | 1.23 (0.99–1.52) | ||
∗P < 0.05, ∗∗P < 0.01, ∗∗∗P < 0.001.
OR = odds ratio; CI = confidence interval.
Figure 1 shows the responses of the level of difficulty in adherence to physical prevention measures. On the whole, the proportion of very difficult/difficult responses was very low for all the physical prevention items except for wearing eye protection (55.6%). The second highest reported physical prevention barrier was to avoid proximity with other people (16.3%). Figure 2 shows the responses for the level of agreement with negative attitudes. It is shown that a relatively higher proportion reported negative attitudes toward COVID-19 than those toward physical prevention barriers. Over half reported strongly agree/agree with regard to avoidance behavior (56.2%), followed by embarrassment (39.9%) and fear (38.8%).
Figure 1.
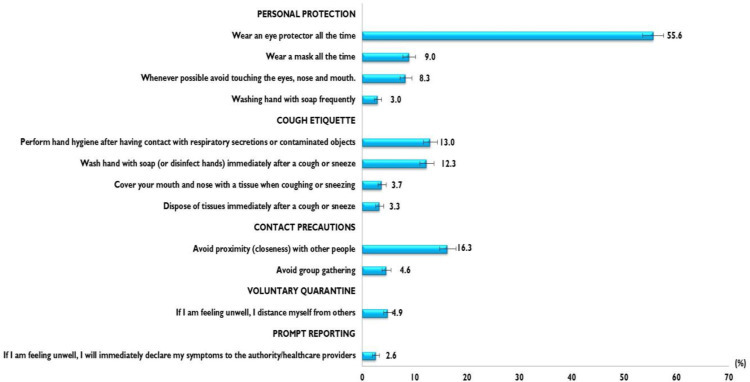
Proportion of Very Difficult/Difficult Responses in Adherence to Physical Prevention Measures (N = 2411)
Figure 2.
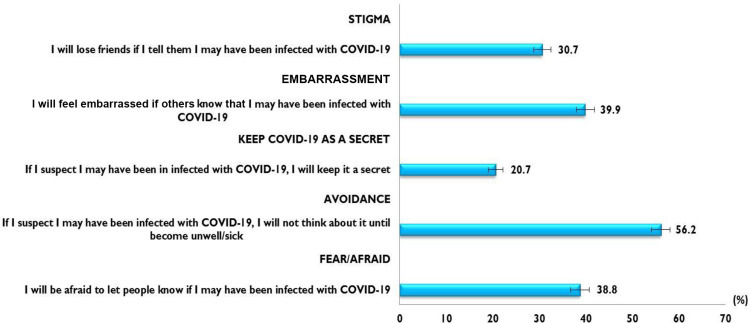
Proportion of Strongly Agree/Agree on Negative Attitudes (N = 2411).
The mean and standard deviation for the total physical prevention barriers score was 19.73 (standard deviation ± 5.3; range 12–45) out of a possible score of 48. The median was 18 (interquartile range: 14.0–23.0). The physical prevention barriers scores were categorized as a score of 18−45 or 12−17, based on the median split; as such, a total of 1250 (51.8%; 95% CI 49.8–53.9) were categorized as having a score of 18–45 and 1161 (48.2%; 95% CI 46.1–50.2) were categorized as having a score of 12−17. Table 1 shows the multivariable logistic regression analysis of demographic characteristics associated with having a higher score in physical prevention barriers. The age group 18−30 years reported a significantly higher likelihood of having high physical prevention barriers score than those aged 51−70 years (OR = 1.87; 95% CI [1.42–2.46]). Participants on an average annual income > CNY130,000 (OR = 2.01; 95% CI 1.56–2.60) and CNY50,000–120,000 (OR = 1.52; 95% CI 1.23–1.86) reported a higher likelihood of having a higher physical prevention barriers score than those earning < CNY50,000. Among all the occupation categories, industrial workers followed by housewife/retired reported the highest proportion of a high physical prevention barriers score.
The mean and standard deviation for the total negative attitudes score was 11.5 (standard deviation ± 4.1; range 5–20) out of a possible score of 20. The median was 11.0 (interquartile range: 9.0–14.0). The negative attitude scores were categorized as a score of 11–20 or 5–10, based on the median split; as such, a total of 1348 (55.9%; 95% CI 53.9–57.9) were categorized as having a score of 11–20, and 1063 (44.1%; 95% CI 42.1–46.1) had a score of 5–10. Table 1 shows the multivariable logistic regression analysis of demographic characteristics associated with having a higher score in negative attitudes. The age group 51−70 years reported a significantly higher likelihood of having high negative attitude scores than those aged 18−30 years (OR = 1.53; 95% CI [1.17–1.99]). Males reported higher negative attitudes scores than females (OR=1.42, 95% CI 1.19−1.71). Participants on an average annual income >CNY130,000 (OR = 1.79; 95% CI 1.40–2.28) reported a higher likelihood of having a negative attitudinal barrier score than those of <CNY50,000.
Using a cut-off score of 44 for the STAI score, a total of 79.9% (n = 1926) (95% CI 78.2−81.5) of the participants reported moderate to severe anxiety during the early phase of the outbreak, and a total of 51.3% (n = 1236) (95% CI 49.2−53.3) of the participants reported moderate to severe anxiety during the current moment. Table 2 shows the prevalence of moderate to severe anxiety during the early phase and after the peak of the COVID-19 outbreak. During the early phase of the outbreak, a higher proportion of females reported having moderate to severe anxiety than males. A prominent increase in the proportion with moderate to severe anxiety was observed with the increase in educational levels for both the early phase and after the peak of the outbreak. Participants of average annual income < CNY50,000 and those residing in urban localities reported the highest proportion, with moderate to severe anxiety. In total, 41.4% (95% CI 39.5–43.5) recorded current anxiety scores similar or higher than the score during the early phase of the outbreak, whereas 58.5% (95% CI 56.5−60.5) recorded current anxiety levels lower than during the early phase of the outbreak. Table 3 shows the multivariate analysis of factors associated with a reduced level of anxiety. Females reported a higher likelihood of having decreased levels of anxiety than males (OR = 1.78, 95% CI 1.48–2.14). Having lower negative attitudes score was associated with a higher decrease in anxiety (OR = 1.59, 95% CI 1.33–1.89). The 31−50 years age group, participants whose average annual income was CNY50,000–120,000 and office workers reported the highest likelihood of having a decreased anxiety level.
Table 2.
Proportion of Moderate to Severe Anxiety Level During the Early Phase of Outbreak and After the Peak (N = 2411)
| Covariates | Early phase of outbreak |
After the peak |
|---|---|---|
| Score ≥44 % (95% CI) n = 1926 | Score>44 % (95% CI) n = 1236 | |
| Age group (y) | ||
| 18–30 | 33.0 (30.9–35.1) | 36.2 (33.6–39.0) |
| 31–50 | 37.2 (35.0–39.4) | 33.1 (30.5–35.8) |
| 51–70 | 29.9 (27.8–32.0) | 30.7 (28.1–33.3) |
| Gender | ||
| Male | 43.7 (41.4–45.9) | 48.9 (46.1–51.8) |
| Female | 56.3 (54.1–58.6) | 51.1 (48.2–53.9) |
| Highest educational level | ||
| Secondary school and below | 19.5 (17.7–21.3) | 20.6 (18.3–22.9) |
| High school | 27.9 (25.9–30.0) | 29.9 (27.4–32.6) |
| University | 52.6 (50.3–54.8) | 49.5 (46.7–52.3) |
| Occupational category | ||
| Health professional | 3.5 (2.8–4.5) | 3.6 (2.6–4.7) |
| Food handling workers/farmers | 9.3 (8.1–10.7) | 10.9 (9.2–12.8) |
| Industrial workers | 27.0 (25.0–29.0) | 33.3 (30.7–36.0) |
| Office workers | 22.1 (20.3–24.0) | 16.2 (14.2–18.4) |
| Housewife/Retiree | 31.5 (29.4–33.6) | 30.2 (27.6–32.8) |
| Students | 6.5 (5.4–7.7) | 5.8 (4.6–7.3) |
| Average annual household income (CNY) | ||
| <50,000 | 41.9 (39.7–44.1) | 43.7 (40.9–46.5) |
| 50,000–120,000 | 31.4 (29.3–33.5) | 27.8 (25.3–30.4) |
| >120,000 | 26.7 (24.7–28.7) | 28.5 (26.0–31.1) |
| Locality | ||
| Urban | 75.6 (73.7–77.6) | 73.0 (70.4–75.4) |
| Sub-urban/Rural | 24.4 (22.4–26.3) | 27.0 (24.6–29.6) |
CI = confidence interval.
Table 3.
Factors Associated With a Decrease in STAI Score (N = 2411)
| Covariates | N (%) | Univariate analysis |
Multivariable analysis |
|
|---|---|---|---|---|
| Decrease in STAI score† (n = 1411) | P value | OR (95% CI) | ||
| Age group (y) | ||||
| 18–30 | 761 (31.6) | 375 (49.3) | 0.70 (0.54–0.92)∗∗ | |
| 31–50 | 897 (37.2) | 595 (66.3) | P < 0.001 | 1.30 (1.03–1.64)∗ |
| 51–70 | 753 (31.2) | 441 (58.6) | Reference | |
| Gender | ||||
| Male | 1070 (44.4) | 516 (48.2) | P < 0.001 | Reference |
| Female | 1341 (55.6) | 895 (66.7) | 1.78 (1.48–2.14)∗∗∗ | |
| Highest educational level | ||||
| Secondary school and below | 442 (18.3) | 272 (61.5) | ||
| High school | 731 (30.3) | 422 (57.7) | 0.362 | |
| University | 1238 (51.3) | 717 (57.9) | ||
| Occupational category | ||||
| Health professional | 81 (3.4) | 46 (56.8) | Reference | |
| Food handling workers/farmers | 217 (9.0) | 133 (61.3) | 1.37 (0.80–2.35) | |
| Industrial workers | 615 (25.5) | 251 (40.8) | 0.64 (0.39–1.04) | |
| Office workers | 546 (22.6) | 387 (70.9) | P < 0.001 | 1.68 (1.02–2.76)∗ |
| Housewife/Retiree | 783 (32.5) | 488 (62.3) | 1.09 (0.66–1.78) | |
| Students | 169 (7.0) | 106 (62.7) | 1.64 (0.93–2.89) | |
| Average monthly household income (CNY) | ||||
| <50,000 | 1049 (43.5) | 596 (56.8) | 0.95 (0.74–1.21) | |
| 50,000–120,000 | 769 (31.9) | 512 (66.6) | P < 0.001 | 1.40 (1.09–1.79)∗∗ |
| >130,000 | 593 (24.6) | 303 (51.1) | Reference | |
| Locality | ||||
| Urban | 1865 (77.4) | 1111 (59.6) | 0.054 | |
| Sub-urban/Rural | 546 (22.6) | 300 (54.9) | ||
| Physical prevention score | ||||
| Score 12–17 | 1161 (48.2) | 698 (60.1) | 0.126 | |
| Score 18–45 | 1250 (51.8) | 713 (57.0) | ||
| Negative attitudes score | ||||
| Score 5–10 | 1063 (44.1) | 713 (67.1) | P < 0.001 | 1.59 (1.33–1.89)∗∗∗ |
| Score 11–20 | 1348 (55.9) | 698 (51.8) | Reference | |
∗P < 0.05, ∗∗P < 0.01, ∗∗∗P < 0.001.
CI = confidence interval; OR = odds ratio; STAI = State-Trait Anxiety Inventory.
Decrease in STAI score—STAI score after peak < STAI score early phase of outbreak.
Discussion
To our knowledge, this study is the first investigation aimed at preventive measures, attitudes, and anxiety levels of the public in Wuhan, the epicenter, after the peak of COVID-19, and the findings could offer an insight into the strategies required to effectively address prevention gaps and the provision of emergency psychological intervention.
In general, the study participants had a good level of physical prevention measures even though the peak of the COVID-19 was declared over. A large proportion had difficulty in using eye-protection, which could have been because of difficulties in obtaining face shields or goggles. Of important highlight, this study did not investigate the underlying reasons for barriers in prevention. A review of global literature reported that among the reasons for barriers in prevention were lack of safety commitment from the public, poor safety culture, lack of proper communication between the health authority and public, and lack of resources for implementing public health and social measures.23 On a positive note, the evidence of current good physical prevention practices may be one of the reasons leading to the continuous decline in infection rates since the day the country announced that the peak of COVID-19 was over. It must also be noted that the demographic disparities found in preventive measures found in this study have many important lessons for policies that seek to address social inequities in disease emergence. In the study, compared with older age participants, the younger age participants present higher barriers to physical prevention. It is thus imperative to enlighten the younger people to enhance their prevention practices despite evidence showing that the elderly and people with underlying diseases are susceptible to infection and prone to serious outcomes.24 Appropriate risk communication is important to enhance sustainable prevention practices. Risk communication that includes informing young people that although COVID-19 generally involves mild infections among healthy young adults, nevertheless in comparison to seasonal influenza, evidence indicates that the risk of death in COVID-19 among young adults is higher than for seasonal influenza.25 Appropriate risk communication is essential and perhaps may trigger higher preventive measures among the younger people. In this study, compelling evidence and the implication of higher barriers in prevention practices among the income group CNY50,000−120,000 and industrial workers warrant further investigation.
Of important note, the study found a relatively higher proportion expressed negative attitudes toward COVID-19 infection. This implies that attitudinal barriers are more prominent than physical prevention barriers. A prominent negative attitude—avoidance behavior—found in this study implies the importance of encouraging the cultivation of timely and appropriate health-seeking attitudes when one is suspected of having been infected with COVID-19. It is equally important to note that cognitive avoidance also contributes to a delay in taking precautions to prevent the spread of COVID-19. Also noteworthy is that the second most prominent negative attitudes after cognitive avoidance were embarrassment and fear of being known to have COVID-19 infection, whereby both were reported by over one-third of the study participants. Likewise, fear and embarrassment were found to deter seeking medical care in other infectious diseases such as Hepatitis B infection and HIV.24 , 26 Equally essential to note is the findings of significant differences in negative attitudes according to demographics. In contrast to physical prevention measures, the older adults in this study demonstrated higher negative attitudes toward COVID-19. In this study, males and participants from higher income groups also tend to demonstrate higher negative attitudes toward COVID-19, which provides important population-level information to address socioeconomic factors that drive attitude disparities.
The finding that nearly 80% of respondents reported moderate to severe anxiety during the early phase of the outbreak evidences the enormous mental health impact of the COVID-19 infection on the public in Wuhan. On the whole, participants rated lower anxiety levels after the country had declared the peak of the COVID-19 pandemic over, with approximately half reporting moderate to severe anxiety. Further, 40% of participants still showed a reduction in anxiety levels despite the peak of the epidemic being over. This implies that the COVID-19 outbreak is still spurring fear on a societal level and likewise found in the previous SARS and Ebola outbreak.18 , 27 Findings from this study imply the posttraumatic distress associated with the COVID-19 outbreak deserves special attention. In the case of the Ebola outbreak, a study revealed that anxiety and depression were still prevalent after 1 year of the outbreak, especially among those who had been in quarantine and witnessed death associated with the disease.27 Therefore, the findings of this study suggest the importance of continuous monitoring of the impact on public mental health and to identify those who are experiencing chronic mental distress and subsequently provide long-term management, especially for complicated traumatic distress cases.
It should also be worth noting that the female gender, along with having positive attitudes toward COVID-19, were 2 strong predictors of a decrease in anxiety levels. Despite females having the highest proportion of moderate to severe anxiety during the early phase of the COVID-19 outbreak, compared with their male counterparts, the females reported a higher likelihood of having a reduced anxiety after the peak of the COVID-19 pandemic was over. This perhaps implies that females are able to recuperate emotionally more quickly than males. More importantly, this study also found that a more positive attitude toward COVID-19 infection is associated with a reduction in anxiety levels, which again emphasizes the importance of tackling negative attitudes in the control and management of COVID-19 after the peak of the outbreak. Tackling stigma and discrimination requires a multilevel approach—amongst others, these should involve public information campaigns to educate and inform the community, interventions focused on cultivating positive views and the provision of helpful coping strategies.28 Moreover, there has been a suggestion that public mental health interventions should be formally integrated into public health preparedness and plans.29 A recent published report emphasized the importance of consultation-liaison psychiatry (CLP) in management of psychiatric manifestations associated to the COVID-19 pandemic.30 It was reported that the CLP was first established in China after liberation in 1949; however, the CLP–type services are not well developed.31 Thus, there is a need to enhance CLP services in China by initiating training programs and research in various medical institutes to provide good mental healthcare during the COVID-19 pandemic.
This current study has several limitations that should be considered. The first pertains to the cross-sectional nature of the study. Thus, the direction of association between attitudes and anxiety levels cannot be identified through cross-sectional study. Future experimental studies are warranted to identify causal relationship between attitudes and anxiety levels. Second, the responses were based on self-report and may be subject to recall bias, self-reporting bias, and a tendency to report socially desirable responses. Of note, assessment of anxiety level during the early phase of the outbreak may be particularly susceptible to recall bias. Another study limitation is the use of an online survey distributed through the social media platform. The study is an open survey; hence, the denominator is not observable, and the response rate is unable to be calculated. Therefore, the current study may be affected by sampling bias. Therefore, the results should be interpreted with caution. Despite these limitations, the study data contribute tremendously to the understanding of public responses and anxiety levels, especially now that the epidemic is growing exponentially.
In conclusion, the current outbreak of the infectious COVID-19 disease has fuelled considerable negative attitudes, including avoidance, embarrassment, stigma, and fear. Study evidences attitudinal barriers to the prevention of the transmission of COVID-19 is more prominent than physical prevention barriers. Implementing educational interventions in reducing negative attitudes toward COVID-19 is crucial. Further, timely dissemination of authoritative pandemic information on the evolving epidemiology and risks is also crucial to alleviate negative attitudes and play an important role in alleviating public psychological pressure. The current study provides evidence that the public experienced heightened anxiety levels during the early phase of the COVID-19 outbreak. Nevertheless, although the proportion with moderate and high anxiety reduced, the fact that half of the public has moderate to severe anxiety levels after the peak of the COVID-19 outbreak is worrisome. Our findings identify the importance of tackling negative attitudes in reducing anxiety levels and provide insight that can be used to formulate psychological interventions to continuously improve the mental health of the people even after the peak of the COVID-19 epidemic is over. Since the COVID-19 pandemic is still ongoing, further longitudinal studies are needed to examine the persistence of anxiety in the aftermath of the COVID-19 pandemic in Wuhan. As the COVID-19 pandemic may lead to long-term mental health issues, helping people cope with their stress and continuous provision of social support are needed to improve their psychological well-being.This study has also raised an important need for continual assessment and address physical and attitudinal barriers to the prevention of COVID-19 in future studies to achieve sustainable elimination of the COVID-19 pandemic.
Footnotes
Conflicts of Interest: The authors declare no conflict of interest.
Funding: This study was supported by the Pilot Project of the Fujian Provincial Department of Science and Technology (No. 2020Y0005); Fujian Medical University's Rapid Response Funding Call for COVID-19 Related Research (No. 2020YJ003). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript. The authors would like to thank all participants of the study for their participation in the investigation.
Availability of Data and Material: All data for this study are available on reasonable request to corresponding author.
Author Contributions: LP.W., Y.L., and Z.H. planned the study. Y.L. obtained the data. LP.W. and H.A. performed the statistical analysis and data summarization. LP.W. drafted the manuscript. All authors discussed the results and contributed to the final manuscript.
References
- 1.Lu H., Stratton C.W., Tang Y.W. Outbreak of pneumonia of unknown etiology in Wuhan, China: the mystery and the miracle. J Med Virol. 2020;92:401–402. doi: 10.1002/jmv.25678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hui D.S., Azhar E.I., Madani T.A. The continuing 2019-nCoV epidemic threat of novel coronaviruses to global health - the latest 2019 novel coronavirus outbreak in Wuhan, China. Int J Infect Dis. 2020;91:264–266. doi: 10.1016/j.ijid.2020.01.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.XinhuaNet. China Says Its COVID-19 Peak is Over. 2020. http://www.xinhuanet.com/english/2020-03/12/c_138870547.htm Available from:
- 4.WHO Virtual Press Conference on COVID-19. 2020. https://www.who.int/docs/default-source/coronaviruse/transcripts/who-audio-emergencies-coronavirus-press-conference-full-and-final-11mar2020.pdf?sfvrsn=cb432bb3_2 Available from:
- 5.WHO Coronavirus Disease 2019 (COVID-19) Situation Report-63. 2020. https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200323-sitrep-63-covid-19.pdf?sfvrsn=b617302d_2 Available from:
- 6.Craig G.M., Daftary A., Engel N., O'Driscoll S., Ioannaki A. Tuberculosis stigma as a social determinant of health: a systematic mapping review of research in low incidence countries. Int J Infect Dis. 2017;56:90–100. doi: 10.1016/j.ijid.2016.10.011. [DOI] [PubMed] [Google Scholar]
- 7.Mak W.W., Cheung F., Woo J. A comparative study of the stigma associated with infectious diseases (SARS, AIDS, TB) Hong Kong Med J. 2009;15 Suppl 8:34–37. [PubMed] [Google Scholar]
- 8.Williams J., Gonzalez-Medina D., Le Q. Infectious diseases and social stigma. Appl Innov Tech. 2011;4:58–70. [Google Scholar]
- 9.Xiang Y.T., Yang Y., Li W. Timely mental health care for the 2019 novel coronavirus outbreak is urgently needed. Lancet Psychiatry. 2020;7:228–229. doi: 10.1016/S2215-0366(20)30046-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Purtle J. COVID-19 and mental health equity in the United States. Soc Psychiatry Psychiatr Epidemiol. 2020;55:969–971. doi: 10.1007/s00127-020-01896-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pierce M., Hope H., Ford T. Mental health before and during the COVID-19 pandemic: a longitudinal probability sample survey of the UK population. Lancet Psychiatry. 2020;7:883–892. doi: 10.1016/S2215-0366(20)30308-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kokou-Kpolou C.K., Megalakaki O., Laimou D., Kousouri M. Insomnia during COVID-19 pandemic and lockdown: prevalence, severity, and associated risk factors in French population. Psychiatry Res. 2020;290:113128. doi: 10.1016/j.psychres.2020.113128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.D'Agostino A., Demartini B., Cavallotti S., Gambini O. Mental health services in Italy during the COVID-19 outbreak. Lancet Psychiatry. 2020;7:385–387. doi: 10.1016/S2215-0366(20)30133-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Thome J., Coogan A.N., Fischer M., Tucha O., Faltraco F. Challenges for mental health services during the 2020 COVID-19 outbreak in Germany. Psychiatry Clin Neurosci. 2020;74:407. doi: 10.1111/pcn.13019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wang C., Pan R., Wan X. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int J Environ Res Public Health. 2020;17 doi: 10.3390/ijerph17051729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Iribarren J., Prolo P., Neagos N., Chiappelli F. Post-traumatic stress disorder: evidence-based research for the third millennium. Evid Based Complement Alternat Med. 2005;2:503–512. doi: 10.1093/ecam/neh127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lewis S.J., Arseneault L., Caspi A. The epidemiology of trauma and post-traumatic stress disorder in a representative cohort of young people in England and Wales. Lancet Psychiatry. 2019;6:247–256. doi: 10.1016/S2215-0366(19)30031-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mak I.W., Chu C.M., Pan P.C., Yiu M.G., Chan V.L. Long-term psychiatric morbidities among SARS survivors. Gen Hosp Psychiatry. 2009;31:318–326. doi: 10.1016/j.genhosppsych.2009.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hou W.K., Hall B.J., Canetti D., Lau K.M., Ng S.M., Hobfoll S.E. Threat to democracy: physical and mental health impact of democracy movement in Hong Kong. J Affect Disord. 2015;186:74–82. doi: 10.1016/j.jad.2015.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Marteau T.M., Bekker H. The development of a six-item short-form of the state scale of the Spielberger State-Trait Anxiety Inventory (STAI) Br J Clin Psychol. 1992;31:301–306. doi: 10.1111/j.2044-8260.1992.tb00997.x. [DOI] [PubMed] [Google Scholar]
- 21.Leung G.M., Ho L.M., Chan S.K. Longitudinal assessment of community psychobehavioral responses during and after the 2003 outbreak of severe acute respiratory syndrome in Hong Kong. Clin Infect Dis. 2005;40:1713–1720. doi: 10.1086/429923. [DOI] [PubMed] [Google Scholar]
- 22.Knight R.G., Waal-Manning H.J., Spears G.F. Some norms and reliability data for the state--trait anxiety inventory and the zung self-rating depression scale. Br J Clin Psychol. 1983;22(Pt 4):245–249. doi: 10.1111/j.2044-8260.1983.tb00610.x. [DOI] [PubMed] [Google Scholar]
- 23.Maqbool A., Khan N.Z. Analyzing barriers for implementation of public health and social measures to prevent the transmission of COVID-19 disease using DEMATEL method. Diabetes Metab Syndr. 2020;14:887–892. doi: 10.1016/j.dsx.2020.06.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Huang C., Wang Y., Li X. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kobayashi T., Jung S.M., Linton N.M. Communicating the risk of death from novel coronavirus disease (COVID-19) J Clin Med. 2020;9 doi: 10.3390/jcm9020580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kamen C., Arganbright J., Kienitz E. HIV-related stigma: implications for symptoms of anxiety and depression among Malawian women. Afr J AIDS Res. 2015;14:67–73. doi: 10.2989/16085906.2015.1016987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Jalloh M.F., Li W., Bunnell R.E. Impact of Ebola experiences and risk perceptions on mental health in Sierra Leone, July 2015. BMJ Glob Health. 2018;3:e000471. doi: 10.1136/bmjgh-2017-000471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.WHO The World Health Report. Promoting Mental Health. 2001. https://www.who.int/whr/2001/chapter4/en/index2.html Available from:
- 29.Dong L., Bouey J. Public mental health crisis during COVID-19 pandemic, China. Emerg Infect Dis. 2020;26:1616–1618. doi: 10.3201/eid2607.200407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Horn M., Granon B., Vaiva G., Fovet T., Amad A. Role and importance of consultation-liaison psychiatry during the COVID-19 epidemic. J Psychosom Res. 2020;137:110214. doi: 10.1016/j.jpsychores.2020.110214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ji J., Ye C. Consultation-liaison psychiatry in China. Shanghai Arch Psychiatry. 2012;24:124–130. doi: 10.3969/j.issn.1002-0829.2012.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]


