Abstract
Background
Telehealth has been successfully implemented for the delivery of obstetrical care. However, little is known regarding the attitudes and acceptability of patients and providers in high-risk obstetrics and whether the implementation of a telehealth model improves access to care in nonrural settings.
Objective
This study aimed to describe patient and provider attitudes toward telehealth for the delivery of high-risk obstetrical care in a large healthcare system with both urban and suburban settings and to determine whether the implementation of a telehealth model improves patient adherence to scheduled appointments in this patient population.
Study Design
Two self-administered surveys were designed. The first survey was sent to all high-risk obstetrical patients who received a telehealth visit between March 1, 2020, and May 30, 2020. The second survey was designed for providers who participated in these visits. We also compared the attended, cancelled, and no-show visit rates before (March 1 to May 30, 2019) and after (March 1 to May 30, 2020) the telehealth implementation and telehealth vs in-person visits in 2020. We reviewed scheduled high-risk prenatal care appointments, diabetes mellitus education sessions, and genetic counseling and Maternal-Fetal Medicine consultations.
Results
A total of 91 patient surveys and 33 provider surveys were analyzed. Overall, 86.9% of patients were satisfied with the care they received and 78.3% would recommend telehealth visits to others. Notably, 87.8% of providers reported having a positive experience using telehealth, and 90.9% believed that telehealth improved patients’ access to care. When comparing patient and provider preference regarding future obstetrical care after experiencing telehealth, 73.8% of patients desired a combination of in-person and telehealth visits during their pregnancy. However, a significantly higher rate of providers preferred in-person than telehealth visits (56% vs 23%, P=.024, respectively). When comparing visits between 2019 and 2020, there was a significantly lower rate of no-show appointments (8.49% vs 4.61%, P<.001), patient-cancelled appointments (7.06% vs 4.96%, P<.001), and patient same-day cancellations (2.30% vs 1.35%, P<.001) with the implementation of telehealth. There was also a significantly lower rate of patient-cancelled appointments (3.82% vs 5.44%, P=.021) and patient same-day cancellations (0.60% vs 1.65%, P=.002) with those receiving telehealth visits than in-person visits in 2020.
Conclusion
The implementation of a telehealth model in high-risk obstetrics has the potential to improve access to high-risk obstetrical care, by reducing the rate of missed appointments. Both patients and providers surveyed expressed a high rate of satisfaction with telehealth visits and a desire to integrate telehealth into the traditional model of high-risk obstetrical care.
Key words: COVID-19, high-risk obstetrics, prenatal care, survey, telehealth
AJOG MFM at a Glance.
Why was this study conducted?
We sought to describe patient and provider attitudes toward telehealth use for the delivery of high-risk obstetrical care and to determine whether the implementation of a telehealth model improves patients’ adherence to scheduled appointments.
Key findings
Overall, 86.9% of patients and 87.8% of providers were satisfied with the use of telehealth for the care of high-risk obstetrical patients. When comparing outcomes of appointments in 2019 vs 2020, there was a significantly lower rate of no-show (8.49% vs 4.61%, P<.001) and cancelled appointments (7.06% vs 4.96%, P<.001) with the use of the telehealth model.
What does this add to what is known?
Patients and providers find telehealth an appropriate form of care for high-risk obstetrical patients. The incorporation of a telehealth model decreased the rate of missed and cancelled appointments, and patients expressed an interest in continuing telehealth appointments.
Introduction
The term “high-risk pregnancy care” is used to describe a mother, fetus, or both who are at higher risk of pregnancy or delivery complications. These patients typically require very close follow-up and a multidisciplinary approach to care.1 In March 2020, the coronavirus disease 2019 (COVID-19) pandemic severely affected New York City and its surrounding suburbs. Because in-person visits became a potential source of exposure and concern for patients and providers, many institutions accelerated their efforts to expand their telehealth offerings. In support, Centers for Medicare and Medicaid Services broadened the access to Medicare telehealth services on a temporary and emergency basis under the 1135 waiver authority and Coronavirus Preparedness and Response Supplemental Appropriations Act.2 A description of how telehealth can be tailored to high-risk obstetrical care during the pandemic has been reported.3
Telehealth has been successfully implemented for the delivery of obstetrical care in rural areas of the United States.4 Satisfaction surveys from patients and providers involved with telehealth in these rural settings have been positive, especially for low-risk obstetrical patients,5 , 6 Since the onset of the COVID-19 pandemic, providers in an urban setting have described telehealth as a potential means to provide obstetrical care.7
However, little is known regarding the attitudes and acceptability of patients and providers toward telehealth high-risk obstetrics. Furthermore, telehealth may not be as highly valued in urban or suburban settings compared with rural settings, because access to specialty care is typically not limited by distance.
Our aim was to describe patient and provider attitudes toward telehealth for the delivery of high-risk obstetrical care in a large healthcare system with both urban and suburban settings. We also sought to determine whether the implementation of a telehealth model improved patient adherence to scheduled appointments in this patient population.
Materials and Methods
Survey
We conducted a cross-sectional survey of all high-risk obstetrical patients who received a telehealth visit between March 1, 2020, and May 30, 2020, at 4 sites within the Northwell Health system. Subjects were identified by reviewing the electronic medical record (EMR) and determining the providers and patients who participated in telehealth visits for high-risk prenatal care appointments, diabetes mellitus education sessions, genetic counseling, and Maternal-Fetal Medicine (MFM) consultations.
Secondary to the COVID-19 pandemic, Northwell Health encouraged the transition of scheduled ambulatory patient visits to telehealth visits. The Division of Maternal-Fetal Medicine chose to implement telehealth for most scheduled high-risk prenatal care appointments, diabetes mellitus education sessions, genetic counseling, and MFM consultations. Telehealth visits were defined as visits completed via 2-way audio-audio or 2-way video-audio connection. In those receiving high-risk prenatal visits via telehealth, blood pressure cuffs were provided (but not Doptones). In-person visits were coordinated when a physical or ultrasound examination was required and scheduled at a minimum of every 6 weeks. Telehealth visits were performed every 1 to 3 weeks depending on the patient’s active high-risk conditions and comorbidities. All telehealth visits were conducted at the same time as in-person visits would have been conducted and not outside of normal office hours. During the pandemic, physician remuneration between virtual and physical encounters was the same.
Two surveys were created by the research team members, 1 for patients and 1 for providers. Each survey consisted of 2 components—1 multiple choice section obtaining either patient demographics or provider information and a second section to evaluate attitudes and satisfaction using a Likert scale. The patient survey had a total of 11 Likert scale questions, and the provider survey had a total of 5 Likert scale questions. Both surveys concluded with a question to evaluate the preferred optimal number of telehealth visits to be incorporated for future prenatal care. The surveys were reviewed by the research team to determine face and content validity. We excluded any patients with an invalid email. The survey responses were anonymous, and the rate of surveys opened was not available.
The surveys were distributed via email through the Research Electronic Data Capture (REDCap). The survey included a cover letter stating the purpose of the study and contact information. Follow-up reminders for survey completion were sent 1 and 2 weeks after the first contact.
We identified all genetic consultations, diabetes mellitus education sessions, MFM consultations, and high-risk prenatal care visits between March 1, 2019, and May 30, 2019, when only occasional telehealth visits were conducted, and between March 1, 2020, and May 30, 2020, after the transition to a telehealth model of care. The visits were then divided into the 3 categories based on data recorded in the Sorian appointment application system— attended appointment, no show, and cancelled appointment. Within the cohort of cancelled appointments, we determined whether visits were cancelled by the patient or the provider and whether they were cancelled on the same day of their scheduled appointment. We also identified the patients’ location of residency within these cohorts.
The study protocol was reviewed and approved by the Northwell Health Institutional Review Board. All data were stored in the REDCap. Descriptive statistics were generated for demographics and satisfaction toward telehealth services. The reliability of the surveys was measured by internal consistency Cronbach α, which in turn measures how well each item correlates with other items in the scale. Cronbach α of >0.70 is considered as an acceptable internal consistency reliability. Differences in appointment rates before and after the implementation of telehealth were analyzed using chi-square test for categorical variables and Fisher exact test when the expected cell frequency was ≤5. P<.05 was considered statistically significant.
Results
Survey responses
After the review of the EMR, 1115 individual patients were identified having a telehealth visit, and 261 patients were excluded secondary to invalid email address. In total, 851 surveys were distributed and 91 patient surveys were returned (response rate of 10.6%). The demographics and characteristics of the patients who responded are presented in Table 1 . Age groups were evenly distributed and more than half of the respondents identified themselves as nonwhite.
Table 1.
Patient demographics
| Demographic | Value |
|---|---|
| Age, y | |
| <24 | 2 (2.2) |
| 25–29 | 23 (14.3) |
| 30–34 | 29 (31.9) |
| 35–39 | 35 (38.5) |
| .≥40 | 12 (13.2) |
| Race | |
| White | 41 (45.1) |
| Hispanic or Latin American | 17 (18.7) |
| Black or African American | 11 (12.1) |
| Asian | 21 (23.1) |
| Native Hawaiian or Pacific Islander | 1 (1.1) |
| Other | 4 (4.4) |
| Highest level of education | |
| Less than high school | 1 (1.1) |
| High school | 20 (22.2) |
| Bachelor’s degree | 38 (42.2) |
| Master’s degree | 31 (34.4) |
| Insurance | |
| Medicaid | 20 (22.0) |
| Employer-provided health insurance | 58 (63.7) |
| Private | 12 (13.2) |
| None | 1 (1.1) |
| Type of visit | |
| High-risk prenatal visit | 15 (16.4) |
| Maternal-Fetal Medicine consultation | 35 (38.5) |
| Genetic counseling | 11 (12.1) |
| Diabetes mellitus education | 51 (56.0) |
| Number of telehealth visits | |
| 1 visit | 33 (36.7) |
| 2 visits | 25 (27.8) |
| ≥3 visits | 32 (35.6) |
| Type of visit | |
| Telephone contact only (audio) | 17 (18.95) |
| Web camera (video and audio) | 31 (34.4) |
| Both | 42 (46.7) |
Values are presented as number (percentage).
Jeganathan et al. Telehealth in high-risk obstetrical patients. AJOGMFM 2020.
Patient survey responses are noted in Figure 1 . Overall, 86.9% of patients were satisfied with the care they received and 78.3% would recommend telehealth visits to others. Notably, 84.7% of patients found the process of connecting to their appointment easy and 92.9% felt their privacy was secure. Patients reported being able to visualize their doctor in 70.3% of cases just as well as if the appointment was in person. A conclusion cannot be made on blood pressure cuff use at home because 71% marked not applicable.
Figure 1.
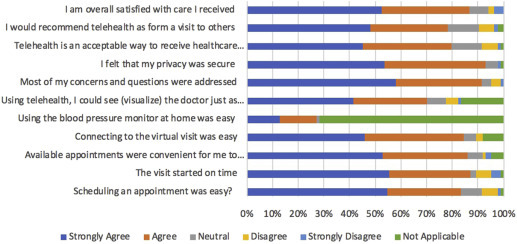
Patient survey responses on telehealth use in high-risk pregnancy care
This figure represents the degree of agreement with 11 survey statements designed to determine the attitudes toward telehealth for high-risk pregnancy care on a 5-point Likert scale.
Jeganathan et al. Telehealth in high-risk obstetrical patients. AJOG MFM 2020.
A total of 85 surveys were mailed out to providers and 33 provider surveys were returned (response rate of 38.8%). Attending physicians, fellows, and residents represented 60.3% of all responses, and nonphysicians including nurse practitioners, nurse midwifes, dietitians, and genetic counselors represented 39.7%. Provider responses are presented in Figure 2 . There were no significant differences between physician and nonphysician responses. Overall, 87.8% of providers liked using telehealth and 90.9% believed that telehealth improved patients’ access to care.
Figure 2.
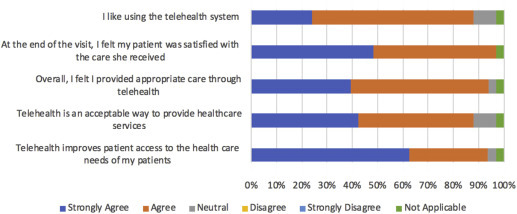
Provider survey responses on telehealth use in high-risk pregnancy care
This figure represents the degree of agreement with 5 survey statements designed to determine the attitudes toward telehealth for high-risk pregnancy care on a 5-point Likert scale.
Jeganathan et al. Telehealth in high-risk obstetrical patients. AJOG MFM 2020.
Figure 3 compares patients’ and providers’ preferences for future obstetrical care after experiencing telehealth. Notably, 73.8% of patients desired a mixture of both in-person and telehealth; however, there was a significantly higher rate of providers who preferred in-person than telehealth visits (56% vs 23%, P=.024, respectively).
Figure 3.
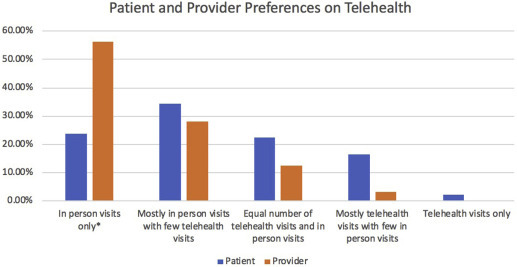
Patient and provider preferences on telehealth
This figure represents what the patient and provider prefer for future high-risk obstetrical care after experiencing telehealth visits. The asterisk indicates P<.05.
Jeganathan et al. Telehealth in high-risk obstetrical patients. AJOG MFM 2020.
Among the patient responses, the 11-Likert scale questions highly correlated with the total satisfaction (r, 0.846; 95% confidence interval [CI], 0.720–892). Likewise, the 5-Likert scale provider response also highly correlated with the total satisfaction (r, 0.947; 95% CI, 0.630–0.984).
Outcome of scheduled appointment
A total of 5734 appointments were scheduled between March 1, 2019, and May 30, 2019. Of the 5494 visits scheduled between March 1, 2020, and May 30, 2020, 1850 (33.7%) were telehealth appointments. Owing to the inability to determine the type of visit, 36 visits were excluded from March 2019 to May 2019 and 378 visits were excluded from March 2020 to May 2020. The remaining appointments stratified by the type of visit and identified as “attended,” “no show,” “cancelled,” “cancelled by patient,” and “cancelled by patient on the same day of the visit” are presented in Table 2 .
Table 2.
Outcomes of scheduled appointments in 2019 vs 2020
| Appointments | 2019 | 2020 | P value |
|---|---|---|---|
| High-risk prenatal visits | |||
| Attended | 905 | 625 | .093 |
| No show | 127 | 54 | <.001 |
| Cancelled | 122 | 194 | <.001 |
| Patient cancelled | 33 | 39 | .076 |
| Patient cancelled on the same day | 16 | 19 | .209 |
| Genetic counseling | |||
| Attended | 722 | 578 | .483 |
| No show | 93 | 34 | <.001 |
| Cancelled | 147 | 164 | .002 |
| Patient cancelled | 109 | 52 | .007 |
| Patient cancelled on the same day | 34 | 13 | .033 |
| Diabetes mellitus education | |||
| Attended | 1519 | 1673 | .835 |
| No show | 183 | 94 | <.001 |
| Cancelled | 232 | 505 | <.001 |
| Patient cancelled | 142 | 69 | <.001 |
| Patient cancelled on the same day | 48 | 21 | <.001 |
| MFM consultation | |||
| Attended | 946 | 420 | <.001 |
| No show | 81 | 54 | .402 |
| Cancelled | 88 | 398 | <.001 |
| Patient cancelled | 118 | 94 | .854 |
| Patient cancelled on the same day | 33 | 16 | .123 |
| All visits | |||
| Attended | 4092 | 3296 | <.001 |
| No show | 484 | 236 | <.001 |
| Cancelled | 589 | 1261 | <.001 |
| Patient cancelled | 402 | 254 | <.001 |
| Patient cancelled on the same day | 131 | 69 | <.001 |
| Total visits | 5698 | 5116 |
MFM, Maternal-Fetal Medicine.
Jeganathan et al. Telehealth in high-riskobstetrical patients. AJOG MFM 2020.
Differences between no-show rates, patient-cancelled appointments, and patient same-day cancelled appointments are shown in Figures 4, 5, and 6 , respectively. In 2020, after the implementation of telehealth, there was a lower rate of attended visits and total cancelled appointments compared with 2019. However, in 2020, overall, there was a significantly lower rate of no-show appointments (8.49% vs 4.61%, P<.001), patient-cancelled appointments (7.06% vs 4.96%, P<.001), and patient same-day cancellations (2.30% vs 1.35%, P<.001). This was true for all appointment types with the exception of the MFM consultations. There was no significant difference in no-show appointments, patient-cancelled appointments, or patient same-day cancellations for MFM consultations in 2020 compared with 2019.
Figure 4.
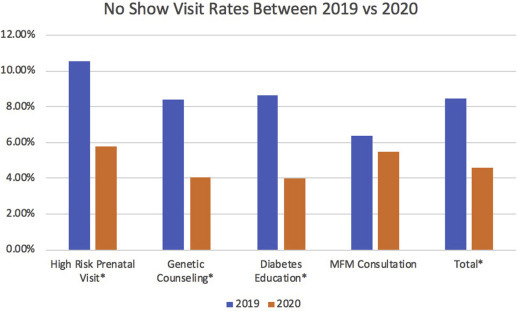
No-show visit rates between 2019 and 2020
This figure represents the proportion of no-show visits from March 1, 2019, to May 30, 2019, compared with March 1, 2020, to May 30, 2020. The asterisk indicates P<.05.
MFM, Maternal-Fetal Medicine.
Jeganathan et al. Telehealth in high-risk obstetrical patients. AJOG MFM 2020.
Figure 5.
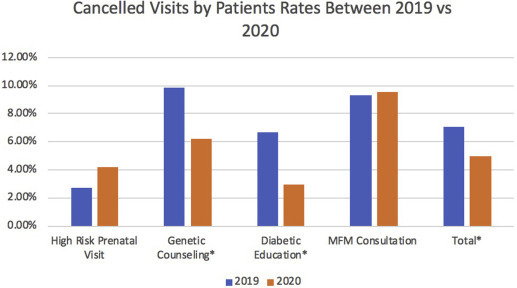
Cancelled visits by patient rates between 2019 and 2020
This figure represents the proportion of visits that were cancelled by patients between March 1, 2019, and May 30, 2019, compared with March 1, 2020, to May 30, 2020. The asterisk indicates P<.05.
MFM, Maternal-Fetal Medicine.
Jeganathan et al. Telehealth in high-risk obstetrical patients. AJOG MFM 2020.
Figure 6.
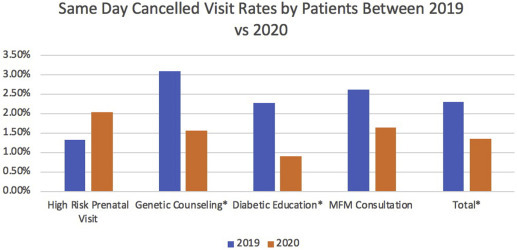
Same-day cancelled visit rates by patients between 2019 and 2020
This figure represents the proportion of visits that were cancelled by patients on the same day of their visit between March 1, 2019, and May 30, 2019, compared with March 1, 2020, to May 30, 2020. The asterisk indicates P<.05.
MFM, Maternal-Fetal Medicine.
Jeganathan et al. Telehealth in high-risk obstetrical patients. AJOG MFM 2020.
A comparison of telehealth appointments with in-person appointments outcomes in 2020 is presented in Table 3 . There was a significantly lower rate of appointments cancelled by patients for in-person visits than telehealth visits (5.44% vs 3.82%, P=.021). Telehealth visits also had a lower no-show rate; however, this difference was not statistically significant. There was no difference between the number of cancelled and no-show appointments between 2019 and 2020 when stratified by the location of patient residency (Table 4 ).
Table 3.
Outcomes of scheduled appointment comparing telehealth with in-person visits in 2020
| Appointments | Telehealth | In-person visits | P value |
|---|---|---|---|
| Attended | 1115 | 2181 | <.001 |
| No show | 60 | 176 | .214 |
| Cancelled | 252 | 1009 | <.001 |
| Patient cancelled | 57 | 197 | .021 |
| Patient cancelled on the same day | 9 | 60 | .003 |
Jeganathan et al. Telehealth in high-risk obstetrical patients. AJOGMFM 2020.
Table 4.
Outcomes of scheduled appointments in 2019 vs 2020 by location of residency
| Appointments | 2019 | 2020 | P value |
|---|---|---|---|
| No show | |||
| Queens | 170 | 88 | .737 |
| Brooklyn | 13 | 5 | .899 |
| Bronx | 3 | 0 | .225 |
| Manhattan | 4 | 1 | .539 |
| Nassau County | 138 | 50 | .095 |
| Suffolk County | 152 | 92 | .177 |
| New Jersey | 0 | 0 | - |
| Westchester County | 0 | 0 | - |
| Patient cancelled | |||
| Queens | 81 | 68 | .119 |
| Brooklyn | 15 | 7 | .512 |
| Bronx | 3 | 2 | .953 |
| Manhattan | 0 | 0 | - |
| Nassau County | 98 | 78 | .178 |
| Suffolk County | 203 | 99 | .076 |
| New Jersey | 1 | 0 | .426 |
| Westchester County | 1 | 0 | .426 |
| Cancelled on the same day | |||
| Queens | 32 | 24 | .251 |
| Brooklyn | 5 | 2 | .745 |
| Bronx | 2 | 1 | .308 |
| Manhattan | 0 | 0 | - |
| Nassau County | 38 | 22 | .758 |
| Suffolk County | 54 | 21 | .308 |
| New Jersey | 0 | 0 | - |
| Westchester County | 0 | 0 | - |
Jeganathan et al. Telehealth in high-riskobstetrical patients. AJOG MFM 2020.
Discussion
Principal findings
These results illustrate that patients and providers view telehealth as an acceptable way to deliver high-risk obstetrical care. Compared with the same time period in 2019, when telehealth visits were rare, the broad implementation of telehealth in 2020 markedly reduced the rate of missed appointments.
Results
Our findings show that, overall, patients are satisfied with telehealth as a mode of care for high-risk pregnancy. In regard to using technology, most patients felt that they were able to see their doctors as well as in person and felt their privacy was still secure through the visit. Patient’s also preferred future visits to include a combination of both telehealth and in-person visits. Both nonphysicians and physicians also felt they provided adequate care for the patients through telehealth.
When we compared the time period before and after telehealth was regularly incorporated into visits, there was a lower rate of patient no-show appointments and patient-cancelled appointments for high-risk prenatal visit, genetic counseling, and diabetes mellitus educations. There were lower rates of telehealth visits being cancelled by patients than in-person visits in the same time period.
Clinical implications
Current recommendations on the frequency of appointments for prenatal care in low-risk women are based on expert opinion.8 Since the start of the COVID-19 pandemic, alternative approaches have been proposed to minimize the number of in-person patient visits, thus decreasing the potential exposure and transmission of the virus.9 One survey of low-risk postpartum women found an increased desire for a more individualized plan of care, including the option of remote monitoring and telehealth medicine.10
Given the complexity of high-risk obstetrical care and often greater anxiety of this population, one might expect a reluctance to shift from in-person visits to telehealth. This study showed a broad acceptance of a telehealth model in this population. There was a high patient satisfaction rate in those receiving telehealth visits and an increased desire for future obstetrical care to include a mixture of both telehealth and in-person visits. This was in contrast to providers who preferred in-person visits only.
It is important to consider that for patients, in-person visits may pose a large burden that includes obtaining daycare, finding transportation, and taking time off from work. Previous studies have shown that telehealth improved access to care in rural settings. One recent study showed that telehealth visits decreased no-show rates compared with in-person visits during the COVID-19 pandemic, which may be attributed to the fear of in-person visits.7 Similar to Madden et al,7 in this study, when comparing the same time period 1 year before where only in-person visits were conducted, the implementation of telehealth decreased the rate of no shows and cancelled appointments. Interestingly, the only visit type that was not affected was MFM consultations. This may reflect a patient’s preference to speak in person with the physician their deeply personal concerns about their pregnancy. Even though access to care may be perceived as “easier” in urban settings owing to reduced geographic barriers, additional personal and social factors may play roles in the ability to attend visits, which supports the availability of alternative methods of visits to improve adherence.
Strengths and limitations
A strength of this study includes the use of a digital appointment system to record patient visits, which enabled an accurate assessment of the rates of attended and missed appointments between the 2 time periods. There was also a wide range of responder demographic factors, including those with diverse racial and ethnic backgrounds, which makes these survey results more characteristic of the general population than previous studies that included mostly responses from white women.
One of the main limitations of this study is the low survey response rate and the possibility that the results were influenced by sampling bias. The low response rate may be caused by the distribution of surveys through email rather than in person and stressors from the COVID-19 pandemic that might have hindered participation. The high rate of nonrespondents precludes the generalization of the results to the entire population of patients included in the study. Because our surveys were anonymous, we were unable to compare characteristics between respondents and nonrespondents. We were also unable to assess whether women had other virtual healthcare visits. Furthermore, given our sample size, we were unable to address certain patient demographics or visit characteristics that were predictive of satisfaction and dissatisfaction. The higher satisfaction rate may be attributed to the fact that this survey was conducted during the COVID-19 pandemic, when patients may not have wanted to appear for in-person visits. The surveys we used were also not validated because previous validated surveys did not reflect the range of questions we sought to answer.
Another limitation of the study is the high rate of cancelled visits initiated by provider offices during the 2020 time period, owing to the COVID-19 pandemic. These cancellations are attributable to extensive rescheduling that occurred owing to the conversion to telehealth visits or to coordinate in-person visits with other scheduled visits, such as ultrasound examinations. Because this study was completed during the COVID-19 pandemic, many patients remained at home, thus making telehealth adherence more feasible than if patients had occupational responsibilities. This may prevent application of these results to areas not significantly affected by the COVID-19 pandemic.
Research implications
One systematic review showed that the implementation of the telemedicine model in high-risk obstetrical patients reduced the need for visits for diabetes mellitus and hypertension without changing maternal or fetal outcomes. Most of the studies included in this review were conducted in high-income European countries and not generalizable to the population in the United States.11 Future studies are needed to assess the impact of a telehealth model of high-risk care on pregnancy outcomes in an ethnically diverse population such as ours. Future studies should also include a larger sample size and evaluate whether certain characteristics including demographics, distance from the hospital, mode of telehealth (video vs phone encounter), and duration of visits are associated with greater satisfaction. It will also be interesting to see whether attitudes toward telehealth remain as positive and compliance with visits remains as high as in this study, once stay at home orders have been lifted.
Conclusion
Although the COVID-19 pandemic has altered the way we care for patients, this has also required us to try innovative ways to continue to provide care for our high-risk obstetrical patients. In this study, telehealth has improved access to care and has achieved high marks for patient satisfaction and a desire to continue this model of care in the future.
Acknowledgments
We thank the Northwell Health COVID-19 Research Consortium for the support with the initiation of this project.
Footnotes
This paper is part of a supplement that represents a collection of COVID-related articles selected for publication by the editors of AJOG MFM without additional financial support.
The authors report no conflict of interest.
Cite this article as: Jeganathan S, Prasannan L, Blitz MJ, et al. Adherence and acceptability of telehealth appointments for high-risk obstetrical patients during the coronavirus disease 2019 pandemic. Am J Obstet Gynecol MFM 2020;2:100233.
References
- 1.Eunice Kennedy Shriver National Institute of Child Health and Human Development, U.S Department of Health and Human Services. High-risk pregnancy. 2018. www.nichd.nih.gov/health/topics/high-risk Available at:
- 2.Centers for Medicare & Medicaid Services Medicare telemedicine health care provider fact sheet. 2020. www.cms.gov/newsroom/fact-sheets/medicare-telemedicine-health-care-provider-fact-sheet?inf_contact_key=26769da722efe729dba2be1c4678cef6 Available at:
- 3.Aziz A., Zork N., Aubey J.J., et al. Telehealth for high-risk pregnancies in the setting of the COVID-19 pandemic. Am J Perinatol. 2020;37:800–808. doi: 10.1055/s-0040-1712121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lowery C., Bronstein J., McGhee J., Ott R., Reece E.A., Mays G.P. ANGELS and University of Arkansas for Medical Sciences paradigm for distant obstetrical care delivery. Am J Obstet Gynecol. 2007;196:534.e1–534.e9. doi: 10.1016/j.ajog.2007.01.027. [DOI] [PubMed] [Google Scholar]
- 5.Bhandari N.R., Payakachat N., Fletcher D.A., et al. Validation of newly developed surveys to evaluate patients’ and providers’ satisfaction with telehealth obstetric services. Telemed J E Health. 2020;26:879–888. doi: 10.1089/tmj.2019.0156. [DOI] [PubMed] [Google Scholar]
- 6.Pflugeisen B.M., Mou J. Patient satisfaction with virtual obstetric care. Matern Child Health J. 2017;21:1544–1551. doi: 10.1007/s10995-017-2284-1. [DOI] [PubMed] [Google Scholar]
- 7.Madden N., Emeruwa U.N., Friedman A.M., et al. Telehealth uptake into prenatal care and provider attitudes during the COVID-19 pandemic in New York City: a quantitative and qualitative analysis. Am J Perinatol. 2020;37:1005–1014. doi: 10.1055/s-0040-1712939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Riley L, Stark A. Preconception and antepartum care. Guidelines for perinatal care. 7th ed. Washington D.C: American Academy of Pediatrics and the American College of Obstetricians and Gynecologists 2012:95–168.
- 9.Boelig R.C., Saccone G., Bellussi F., Berghella V. MFM guidance for COVID-19. Am J Obstet Gynecol MFM. 2020;2:100106. doi: 10.1016/j.ajogmf.2020.100106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Peahl A.F., Novara A., Heisler M., Dalton V.K., Moniz M.H., Smith R.D. Patient preferences for prenatal and postpartum care delivery: a survey of postpartum women. Obstet Gynecol. 2020;135:1038–1046. doi: 10.1097/AOG.0000000000003731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.DeNicola N., Grossman D., Marko K., et al. Telehealth interventions to improve obstetric and gynecologic health outcomes: a systematic review. Obstet Gynecol. 2020;135:371–382. doi: 10.1097/AOG.0000000000003646. [DOI] [PMC free article] [PubMed] [Google Scholar]


