Abstract
Context
Coronavirus disease 2019 (COVID-19) led to increased attention nationally on advance care planning.
Objectives
To describe the impact COVID-19 had on advance care planning based on changes in the calls to the West Virginia Center for End-of-Life Care (center) and in the volume and types of documents requested from and submitted to the center and its e-Directive Registry (registry).
Methods
A retrospective and observational analysis between January 1, 2020 and June 30, 2020 of calls to the center; advance directives downloaded from the center's Web site as well as mailed to the public and medical orders mailed to health care professionals on request to the center; and advance directives and medical orders submitted to the registry.
Results
The nature of calls changed to COVID-19-related topics, including confirmation of forms on the registry, urgent desire to initiate advance care planning, temporary rescindment of treatment-limiting forms, and questions on how to honor patients' wishes in advance directives and medical orders in light of their COVID-19 status. Also in the first six months of 2020, the center distributed more advance directives than it had during the same months in the last five years and more medical orders than it had in the preceding four years when there were no revisions to the medical order forms required by changes to the state law.
Conclusion
COVID-19 resulted in a new sense of urgency regarding advance care planning by West Virginians with increased attention to document their wishes and ensure that they were in the registry.
Key Words: COVID-19, advance care planning, medical orders, advance directives
Key Message
During the coronavirus disease 2019 pandemic, there was a new sense of urgency and interest in advance care planning in West Virginia resulting in calls and requests to the Center for End-of-Life Care to ensure that patients' wishes were accurately documented in its statewide registry so that they would be respected.
Introduction
In 2010, the West Virginia (WV) Center for End-of-Life Care (the center) created the WV e-Directive Registry (the registry), and in 2012, the registry became available online on the state's health information exchange portal, the West Virginia Health Information Network. This enabled Health Insurance Portability and Accountability Act-compliant and password-protected 24/7 access for treating health care providers to their patients' advance directives and medical orders in emergencies.
The subsequent coronavirus disease 2019 (COVID-19) pandemic heightened the awareness of health care providers and the public on end-of-life issues and prompted patients to engage in advance care planning.1, 2, 3, 4, 5 The purpose of this brief report is to describe the impact that COVID-19 had on advance care planning in WV during the first six months of 2020 including the peak of the pandemic shutdown. The impact is reflected by changes in the calls to the center and in the volume and types of documents requested from and submitted to the center and registry compared with data from the same months in the preceding six years.
Methods
Design and Setting
This is a retrospective and an observational analysis between January 1, 2020 and June 30, 2020 of advance directives and medical orders (do-not-resuscitate [DNR] and physician orders for scope of treatment [POST] forms) submitted to the registry and of advance directives and medical orders distributed by the center on request. The function of the registry and submission of forms to it have been previously described.6 , 7
Measurements
The following variables were analyzed: POST and DNR mailed to health care providers, advance directives mailed and downloaded from the center Web site, phone calls to the center, and forms submitted to the registry. The West Virginia University Institutional Review Board granted approval for registry-based research (#1208000278).
Results
The Center
Beginning January 2020, many WV residents and health care professionals began contacting the center with topics related to COVID-19. In the order of frequency with the most common first, calls to the center related to four main topics: confirmation of documents in the registry, urgent desire to initiate advance care planning, request for temporary rescindment of treatment-limiting forms, and patient-specific questions about how to honor patients' wishes in advance directives and medical orders in light of their COVID-19 status. Table 1 shows the frequency of consecutive voice mails per topic for 141 voice mails received during the 20-day period between March 20, 2020 and April 8, 2020. The 141 voice mails account for 26.4% of the total 534 voice mails received or calls placed by the center during March and April 2020. It is noteworthy that there were a disproportionate number of calls and voice mails to the center during these two months because the calls and voice mails represented 51% (534 of 1046) of the calls and voice mails for the six month period of the study. The 141 voice mails in Table 1 were selected based on available data at the time of the study (i.e., the voice mails from March 20, 2020 to April 8, 2020 were still available for retrospective data analysis) and are representative of the total calls received. Twenty-three of the voice mails were classified as other/irrelevant in Table 1 as they did not directly pertain to any of the topics (i.e., a death notice, wrong number, or wrong department) or could not be classified based on the caller not leaving a voice mail message.
Table 1.
Proposed Title Classification of Phone Calls to the Center During the COVID-19 Pandemic
| Topic | Number of Voice Mails Received | Representative Comment |
|---|---|---|
| Confirmation of documents in the registry | 97 |
|
| Urgent desire to initiate advance care planning | 12 |
|
| Request for temporary rescindment of treatment-limiting forms | 6 |
|
| Patient-specific questions about how to honor a patient's wishes in advance directives and medical orders in light of their COVID-19 status | 3 |
|
| Other/irrelevant | 23 |
|
COVID-19 = coronavirus disease 2019; DNR = do not resuscitate; MPOA = Medical Power of Attorney.
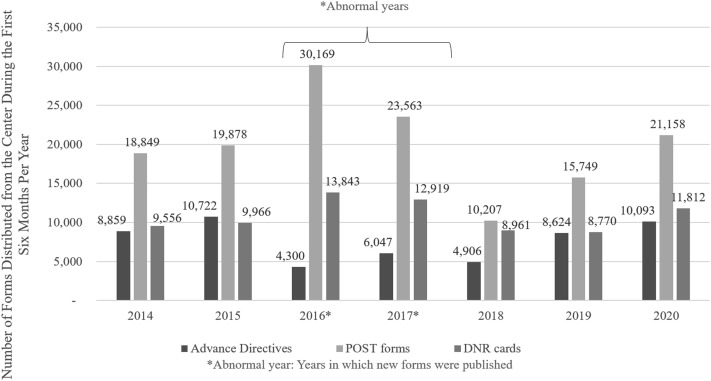
COVID-19-related concerns also resulted in a spike in advance care planning medical order form requests. Excluding the years of 2016 and 2017 when the center distributed revised DNR and POST forms because of changes in state law regarding signatory authority on medical orders of advanced practice registered nurses (2016) and physician assistants (2017),8 the center distributed more of these medical order forms in the first six months of 2020 than in the same months in 2014, 2015, 2018, and 2019 (Fig. 1 ). During March–June 2020, the center limited distribution of POST forms and DNR cards to 100 per mailing to conserve the center's supply during the pandemic when there might be delays in form production.
Fig. 1.
Distribution comparison by form type for the first six months of 2014–2020. POST = physician orders for scope of treatment; DNR = do not resuscitate.
In the first six months of 2020, the center distributed 10,093 advance directives, which were second only in number in the first six months in a seven-year period to 2015 when the center distributed 10,722 advance directives (Fig. 1) and the highest in the last five years.
Fig. 1 shows the comparison of distribution rates by form type (advance directives, POST forms, and DNR cards) for the first six months (June 1–June 30 per year) of the last seven years (2014–2020). The previous six years are shown to establish the average and range of distribution rates for typical years for comparison to 2020. The years of 2016 and 2017 were atypically high because new versions of the DNR and POST forms were released in those years. In past years, the center staff noted that form distribution rates were significantly higher in years when revised versions of the medical orders were released because of changes in state code.
The Registry
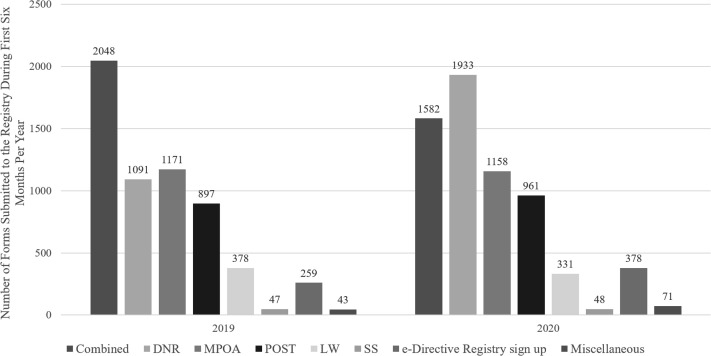
In the first six months of 2019, the registry received 5934 forms, including 2048 combined living will and Medical Power of Attorney forms, 1091 DNR cards, 1171 Medical Power of Attorney forms, 897 POST forms, and 378 living will forms.
During the first six months of 2020, the registry received 6471 forms, including 1582 combined living will and Medical Power of Attorney forms, 1933 DNR cards, 1158 Medical Power of Attorney forms, 961 POST forms, and 331 living will forms. Fig. 2 shows the comparison of submission rates by form type to the registry for the first six months of 2019 and 2020. Most remarkable is the 77.18% increase in DNR cards (1933 vs. 1091) received in the first six months of 2020.
Fig. 2.
Submission comparison by form type for the first six months of 2019 and 2020. DNR = do not resuscitate; MPOA = Medical Power of Attorney; POST = physician orders for scope of treatment; LW = living will; SS = surrogate selection.
Discussion
COVID-19 resulted in a new sense of urgency of patients receiving care in WV regarding advance care planning with increased attention to documenting their current wishes for medical care accurately and to ensuring that they were recorded in the registry. The center's toll-free phone line enabled callers to ask pandemic-related questions about advance care planning, advance directives, and medical orders and to confirm that their treatment wishes were documented in the registry. These calls may serve as a snapshot of the attitudes of patients in WV, and possibly in the U.S., with regard to advance care planning prompted by pandemic-related concerns.
Most significant is the increase in medical order and advance directive distribution by the center during the first six months of 2020 as compared with the preceding six years. Health care providers requested an additional 1600 more POST forms and 450 more DNR cards than were actually distributed during the study period because of pandemic-related distribution limits per request. They are not included in Fig. 1.
Although there was only a 9.05% increase in forms submitted to the registry (6471 vs. 5934), it is important to note there was a 77.18% increase in DNR cards submitted to the registry (1933 vs. 1091). This increase may reflect the concerns of patients who did not want heroic measures at the end of life if they were sick with COVID-19. Also portrayed in Fig. 2 is the increase in e-Directive Registry sign-up forms from 2019 to 2020. The registry uses an opt-in based system; this allows patients the option to choose whether their forms are included in the registry. For forms to be made available to treating health care providers through the registry, patients must either submit an e-Directive Registry sign-up form along with their form, which authorizes the registry to enter it into the database, or patients must submit forms that already include an initialed registry opt-in box on the form. During this study, there was a 45.95% increase in e-Directive Registry sign-up forms submitted to the registry (378 vs. 259). This increase resulted from patients who had previously completed forms without an opt-in box or chosen in the past not to opt in deciding that they wanted their forms in the registry.
The COVID-19 pandemic has resulted in dramatic changes in health care. An area in which it has had a major effect—advance care planning—is one in which patients frequently procrastinate or avoid altogether. Prompted by the pandemic and the heightened concerns about widespread illness, patients seeking health care in WV contacted the West Virginia Center for End-of-Life Care to ensure that their wishes were recorded in the registry and available to treating health care providers in an emergency. Even as the crisis of the pandemic appears to be subsiding, clinicians have noted a new openness of patients to engage in advance care planning to maintain control over their health care. The changes seen in WV may represent a glimpse into what may be a greater receptivity to advance care planning in this country in the future.
Disclosures and Acknowledgments
This research was funded by no outside source or agency. The authors declare no conflicts of interest.
References
- 1.Center to Advance Palliative Care “Fast five:” Legal issues in advance care planning during COVID-19. 2020. https://www.capc.org/covid-19/communication/advance-care-planning/ CAPC.org. Available from.
- 2.Curtis J.R., Kross E.K., Stapleton R.D. The importance of addressing advance care planning and decisions about do-not-resuscitate orders during novel Coronavirus 2019 (COVID-19) JAMA. 2020;323:1771–1772. doi: 10.1001/jama.2020.4894. [DOI] [PubMed] [Google Scholar]
- 3.deLima Thomas J. Pandemic as teacher – forcing clinicians to inhabit the experience of serious illness. NEJM. 2020;383:306–307. doi: 10.1056/NEJMp2015024. [DOI] [PubMed] [Google Scholar]
- 4.National POLST POLST and COVID-19. POLST.org. 2020. https://polst.org/covid/?pro=1 Available from.
- 5.Zitter J.N. Covid or no Covid, It's important to plan. NYTimes.com. 2020. https://www.nytimes.com/2020/04/16/well/live/coronavirus-planning-documents-advance-directives.html Available from.
- 6.Pedraza S.L., Culp S., Falkenstine E.C., Moss A.H. POST forms more than advance directives associated with out-of-hospital death: insights from a state registry. J Pain Symptom Manage. 2016;51:240–246. doi: 10.1016/j.jpainsymman.2015.10.003. [DOI] [PubMed] [Google Scholar]
- 7.Pedraza S.L., Culp S., Knestrick M., Falkenstine E., Moss A.H. Association of physician orders for life-sustaining treatment form use with end-of-life care quality metrics in patients with cancer. J Oncol Pract. 2017;13:e881–e888. doi: 10.1200/JOP.2017.022566. [DOI] [PubMed] [Google Scholar]
- 8.West Virginia legislature (2002; 2007; 2011; 2016; 2017) http://www.wvlegislature.gov/wvcode/code.cfm?chap=16&art=30 West Virginia code: [Chapter 16]. Public health. Article 30. West Virginia health care decisions act: §16-30. West Va Legislature. Available from.