Summary
Introduction
Children from minority groups are at increased risk of overweight. This study compared BMI growth patterns from birth onwards of boys and girls with overweight at 5‐6 years, according to socioeconomic status (SES) and country of origin, in order to gain more insight into the critical periods of growth to overweight.
Methods
A total of 3714 singletons of the multi‐ethnic ABCD study were included. Within children with overweight at age 5‐6 years (N = 487, prevalence boys: 11.6%, girls: 14.6%), BMI growth patterns from birth onwards (12.8 serial measurements; SD = 3.1) were compared between children from European (69.4%) and non‐European mothers (30.6%), and between children from low (20.8%), mid (37.0%) or high SES (42.2%), based on maternal educational level.
Results
BMI growth to overweight did not differ between children of European or non‐European mothers, but it did differ according to maternal SES. Children with overweight in the low and mid SES group had a lower BMI in the first 2 years of life, an earlier adiposity rebound and increased in BMI more rapidly after age 2, resulting in a higher BMI at age 7 years compared to children with overweight in the high SES group [∆BMI (kg/m2) between high and low SES: boys 1.43(95%CI:0.16;3.01) and girls 1.91(0.55;3.27)].
Conclusion
Children with overweight from low SES have an early adiposity rebound and accelerated growth to a higher BMI at age 5‐6 years compared to children with overweight from the high SES group. These results imply that timing of critical periods for overweight development is earlier in children with a low socioeconomic background as compared to other children.
Keywords: children, growth patterns, overweight, social inequalities
1. INTRODUCTION
Over the past decades there has been a worldwide increase in the prevalence of overweight and obesity among children. 1 Children with overweight or obesity are at increased risk of adult overweight and its associated comorbidities.2, 3, 4, 5 Early prevention of childhood overweight is therefore of absolute importance and identifying critical periods in the development of childhood overweight is an essential step towards effective prevention.
BMI growth patterns differ from early age onwards between children who will develop overweight in late childhood compared to those with normal weight.6, 7, 8 Children with overweight have higher birthweights, and faster rates of growth in the first years of life.6, 7, 8, 9, 10, 11 Moreover, their BMI peak tends to be higher and their adiposity rebound—a renewed rise in BMI after the decrease in BMI that followed the BMI peak—tends to be earlier with a steeper increase in BMI compared to those of normal weight.6, 7, 12, 13, 14
This general pattern to overweight is likely to reveal differences when comparing lower vs higher socioeconomic groups, or ethnic minority populations vs the host populations. Although this has not been studied directly, previous studies provide indications to suggest such differences in growth patterns. For instance, children of low socioeconomic background are born smaller, and are more likely to be overweight at age 5 years,15, 16 showing an increased growth in the first years compared to children of high socioeconomic background. In addition, children in ethnic minority populations are more often small at birth, but have more obesity in childhood compared to children from Dutch origin.17, 18, 19, 20 This shows that they grow faster after birth, compared to children of Dutch origin. There are indications that these differences in early postnatal growth are partly due to ethnic and socioeconomic differences in feeding practises.21, 22, 23, 24, 25, 26, 27
Therefore, this study will investigate BMI growth patterns to overweight at age 5‐6 years using longitudinal measurements of BMI from birth onwards stratified for maternal country of origin and maternal socioeconomic background. Country of origin will be indicated by country of birth (European origin vs non‐European origin) and socioeconomic background by maternal educational level. Growth curves will be described for boys and girls separately, as growth patterns of boys and girls have been shown to differ.28, 29 Disparities in timing of the critical periods in BMI growth to overweight could help to better identify children in minority groups at risk for childhood overweight at an early stage of development.
2. METHODS
2.1. Study population
This study was part of the Amsterdam Born Children and their Development (ABCD) study. The aim of the prospective cohort ABCD study was to examine the association between maternal lifestyle, medical, psychosocial and environmental conditions during pregnancy and children's health at birth as well as in later life. 30 All pregnant women in Amsterdam (January 2003‐March 2004) were approached at their first antenatal visit to an obstetric caregiver [median 13 weeks (IQR = 14‐16)] to participate. Of the 12 373 women approached, 8266 filled out the pregnancy questionnaire. Of the mothers who gave birth to a live‐born singleton, 6734 gave permission for follow‐up. In the following years, the follow‐up of growth of 5865 children was collected from files of the Youth Health Care registration of the Public Health Service in Amsterdam. Moreover, at age 5‐6 years, 3321 of the children participated in the ABCD health check, where weight and height were measured. Of the 4539 with known BMI at mean age 5.7 (SD = 0.4) years, children born with congenital anomalies (n = 105), celiac disease (n = 6), underweight (n = 511) or with missing growth data (n = 203) were excluded, leaving 3714 children in the final study sample (Figure 1). For this study, ethical approval was obtained according to the guidelines of the Declaration of Helsinki, and all procedures involving human subjects were approved by the review boards of all Amsterdam hospitals and the Registration Committee of Amsterdam. Written informed consent was obtained from all subjects.
FIGURE 1.
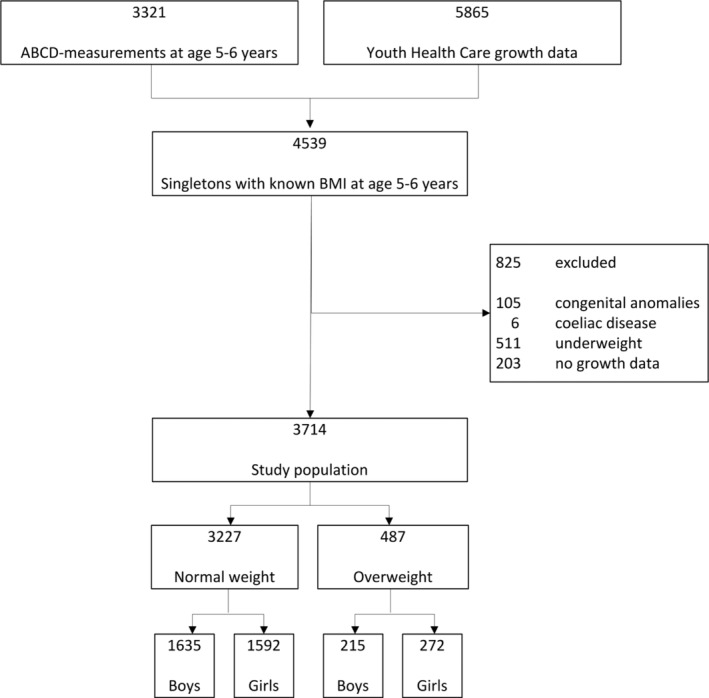
Flowchart of the study population
2.2. BMI growth pattern
Growth data were obtained from the Youth Health Care registration of the Public Health Service in Amsterdam. Following a standard procedure, trained nurses measured at regular follow‐up moments between birth and age 6 years weight and height and BMI was calculated (mean = 12.8; SD = 3.1). For each child an individual BMI growth curve was modelled. 31 Since the length of the child was first measured at 4 weeks of age, the BMI score at birth was extrapolated.
2.3. Overweight at age 5‐6 years
BMI was based on height and weight measures at 5‐6 years old, obtained from the ABCD health check (69.4%) complemented by growth measurements of the Youth Health Care registration (30.6%). Height was measured to the nearest millimetre using a Leicester portable height measure (Seca), and weight to the nearest 100 g using a Marsden weighing scale (model MS‐4102). 32 The agreement between the two registration for height and weight could be estimated in 1531 children who were measured during the ABCD health check as well as by YHC professionals within 1 year. The intra class correlation (ICC) of height was 0.83 and for weight 0.90 which indicate good to excellent agreement. Children were divided in normal weight and overweight/obese, by sex‐ and age specific BMI cut‐off points defined by the International Obesity Task Force. 33
2.4. Country of origin
Country of origin of the child was based on the country of birth of the mother and her mother, reported in the pregnancy questionnaire, to include first and second generation. 17 The children were divided in two groups: European origin (European countries, United States, Canada, Australia and New Zealand) and other.
2.5. Socioeconomic status
SES was based on maternal education in years after primary school, reported in the pregnancy questionnaire and divided in three categories: low (0‐5 years), middle (6‐10 years) and high (>10 years).
2.6. Characteristics of the study population
The following variables were used for demographic information: maternal age (years) and maternal smoking during pregnancy (yes/no) which were self‐reported in the pregnancy questionnaire, sex (boy/girl), gestational age (days), parity (nulliparous/multiparous), and birth weight of the child (gram) were retrieved from the Youth Health Care registration.
2.7. Analyses
Characteristics of the study sample were described according to weight status at age 5‐6 years for boys and girls separately. Demographic differences between children with normal weight and children with overweight as well as differences between the response and non‐response group (live‐born singletons with permission to follow‐up meeting the inclusion criteria, but without growth data and/or BMI status at 5 years of age) were tested with chi‐square tests for categorical variables and two‐sample t tests for continuous variables.
To model the overall longitudinal BMI growth patterns of normal weight and overweight, two separate sex‐specific linear mixed models were fitted to the BMI growth data. 34 To capture the non‐linearity of the BMI growth patterns, the fixed effect describing the relation between BMI and age were modelled with a natural spline function. The knot placement of the natural splines was based on quantiles of age. For both models, the best number of knots was chosen based on the Bayesian Information Criterion (BIC). To quantify the difference between normal weight and overweight, interaction terms were added to the model. Finally, we used a random intercept and slope to capture the correlation between BMI growth measurements from the same child.
Firstly (Part 1), differences in BMI growth patterns (BMI peak, BMI adiposity rebound) between children with normal weight and overweight were described by visual inspection. Differences between BMI at certain ages (0, 3, 6, 9 months, 1, 2, 3, 4, 5, 6, 7 years) were checked by investigating the amount of overlap of the 95% confidence intervals. If the 95% confidence intervals are not overlapping, there is some evidence that the BMI growth patterns are different.
Secondly (Part 2), the population was restricted to only children with overweight (N = 487). The same modelling procedure was followed as in Part 1. The BMI growth curves were compared for children who had overweight at age 5‐6 years of European origin and of other origin. Thirdly, to adjust for the interrelation of SES and country of origin, the population was further restricted to children with overweight from only European origin (N = 206). BMI growth curves were compared of children with overweight from high SES, middle SES and low SES groups. We did not correct for any covariates as potentially important variables as maternal smoking, birth weight and maternal weight status are strong determinants of postnatal growth, both influenced by ethnicity 17 and SES15, 16 and are therefore part of the causal pathway. A secondary analysis with subdivision of the non‐European group into children from Turkish, Moroccan and Surinamese decent was performed to have some indication whether BMI growth curves differed between these groups. Descriptive analyses were performed in SPSS version 23 and BMI growth patterns were analyzed with R version 3.3.3.
3. RESULTS
3.1. Study population
In our study population 13.1% of the children were overweight. Boys and girls with overweight had respectively a 3.4 and 3.6 kg/m2 higher BMI than children with normal weight at age 5‐6 years. Overweight was more prevalent in girls (14.6%) than in boys (11.6%) and in children with a non‐European origin (24.8%) and low SES (15.6%) background (Table 1). Children with overweight more often had mothers who were younger, more often overweight themselves, multiparous and smoked more often than the mothers of children with normal weight (Table 2).
TABLE 1.
Prevalence of overweight in our study population
| Total study population (N = 3714) (%) | Boys (N = 1850) (%) | Girls (1864) (%) | ||
|---|---|---|---|---|
| Total study population | 13.1 | 11.6 | 14.6 | |
| Country of origin | European origin | 8.0 | 7.0 | 8.9 |
| Other | 24.8 | 21.7 | 27.9 | |
| Socioeconomic status (only European origin) | High SES | 6.3 | 4.9 | 7.6 |
| Middle SES | 8.9 | 8.3 | 9.4 | |
| Low SES | 15.9 | 16.1 | 15.7 | |
Abbreviation: SES, socioeconomic status.
TABLE 2.
Characteristics of the study population (N = 3714)
| Boys (N = 1850) | Girls (N = 1864) | |||||
|---|---|---|---|---|---|---|
| Normal weight N = 1635 (88.4%) | Overweight N = 215 (11.6%) | Normal weight N = 1592 (85.4%) | Overweight N = 272 (14.6%) | |||
| Maternal age | Mean (SD) | 31.4 (5.1) | 29.3 (5.7)* | 31.5 (4.9) | 29.5 (5.9)* | |
| Maternal country of origin | European origin | N (%) | 1181 (72.2) | 89 (41.4)* | 1192 (74.9) | 117 (43.0)* |
| Other | N (%) | 454 (27.8) | 126 (58.6) | 400 (25.1) | 155 (57.0) | |
| Maternal socioeconomic status | Low | N (%) | 320 (19.7) | 82 (38.7)* | 264 (16.7) | 99 (37.2)* |
| Middle | N (%) | 575 (35.4) | 87 (41.0) | 602 (38.1) | 101 (38.0) | |
| High | N (%) | 731 (45.0) | 43 (20.3) | 716 (45.3) | 66 (24.8) | |
| Maternal weight status | Not overweight | N (%) | 1177 (78.0) | 106 (54.6)* | 1182 (79.3) | 123 (51.3)* |
| Overweight | N (%) | 332 (22.0) | 88 (45.4) | 309 (20.7) | 117 (48.7) | |
| Maternal parity | Nulliparous | N (%) | 878 (53.7) | 106 (49.3) | 869 (54.6) | 138 (50.7) |
| Multiparous | N (%) | 757 (46.3) | 109 (50.7) | 723 (45.4) | 134 (49.3) | |
| Maternal smoking during pregnancy | Yes | N (%) | 158 (9.7) | 30 (14.0)* | 149 (9.4) | 46 (16.9)* |
| No | N (%) | 1476 (90.3) | 185 (86.0) | 1443 (90.6) | 226(83.1) | |
| Gestational age at birth (days) | Mean (SD) | 279 (12) | 278 (13) | 279 (11) | 279 (11) | |
| Birth weight (grams) | Mean (SD) | 3548 (556) | 3630 (581)* | 3412 (515) | 3443 (542) | |
| BMI at age 5‐6 years | Mean (SD) | 15.5 (0.8) | 18.9 (1.6)* | 15.4 (0.9) | 19.0 (1.7)* | |
| Duration of exclusive breastfeedinga | None | N (%) | 276 (17.7) | 41 (20.3)* | 250 (16.4) | 57 (21.5)* |
| <1 months | N (%) | 125 (8.0) | 26 (12.9) | 124 (8.1) | 32 (12.1) | |
| 1–3 months | N (%) | 459 (29.4) | 69 (34.2) | 434 (28.5) | 67 (25.3) | |
| >3 months | N (%) | 699 (44.8) | 66 (32.7) | 714 (46.9) | 109 (41.1) | |
| Sleep (h)a | Mean (SD) | 10.5 (0.9) | 10.3 (1.1)* | 10. 5 (0.9) | 10.3 (1.1)* | |
| Screentime (h)a | Mean (SD) | 1.5 (1.1) | 1.9 (1.2)* | 1.3 (0.9) | 1.8 (1.2)* | |
| Member of sports club a | N (%) | 646 (53.6) | 66 (56.9) | 506 (44.0) | 91 (58.3)* | |
P < 0.05.
Measured in a subset of N = 3548 (breastfeeding) and N = 1309 (sleep, screen time, membership of sports club).
3.2. Part 1: Total population
Based on the BIC, the optimal number of degrees of freedom for the natural spline function describing the relation between BMI and age was 7 for both boys and girls. Overweight boys at age 5‐6 years had a higher birth weight (Table 2) and higher BMI at birth (Table 3) compared to normal weight boys.). Figure 2 presents the average BMI growth curves of children with normal weight and overweight at age 5‐6 years. Visual inspection of this figure shows that in children with overweight, the BMI peak was higher (±1 kg/m2) than for children with normal weight. Although timing of the BMI peak was earlier in overweight boys than in normal weight boys, no differences were seen in girls. On the other hand, timing of the adiposity rebound was earlier in children with overweight (at age 3 years) than in children with normal weight (at age 5 years). The magnitude of the drop in BMI after the BMI peak differed between boys with overweight (ΔBMI = ±1 kg/m2) compared to boys with normal weight (ΔBMI = ±2 kg/m2), similar findings were found for girls (ΔBMI = ±0.5 kg/m2 for girls with overweight and ΔBMI = ±1.5 kg/m2 for girls with normal weight.
TABLE 3.
ΔBMI scores (95% confidence intervals) compared with reference group
| Overweight a | Country of origin b | Socioeconomic status c | ||||||
|---|---|---|---|---|---|---|---|---|
| Boys | Girls | Boys | Girls | Boys | Girls | |||
| Low | Mid | Low | Mid | |||||
| 0 months | 0.45 (0.11; 0.79) | 0.28 (0.01; 0.56) | 0.43 (−0.13;0.99) | 0.24 (−0.22;0.70) | −1.41 (−2.36;‐0.45) | −0.80 (−1.61;0.01) | −0.23 (−1.12;0.65) | −0.23 (−0.9;0.43) |
| 3 months | 1.02 (0.84; 1.20) | 0.83 (0.68; 0.98) | 0.34 (−0.03;0.72) | 0.32 (−0.01;0.65) | −1.15 (−1.87;‐0.43) | −0.58 (−1.18;0.02) | 0.29 (−0.41;1.00) | −0.21 (−0.73;0.32) |
| 6 months | 1.09 (0.92; 1.26) | 0.95 (0.80; 1.09) | 0.11 (−0.24;0.47) | 0.31 (−0.00;0.62) | −0.99 (−1.72;‐0.26) | −0.47 (−1.07;0.13) | 0.28 (−0.41;0.97) | −0.28 (−0.78;0.23) |
| 9 months | 1.03 (0.86; 1.20) | 1.08 (0.93; 1.23) | −0.11 (−0.47;0.25) | 0.25 (−0.07;0.56) | −0.93 (−1.62;‐0.23) | −0.47 (−1.04;0.10) | −0.13 (−0.78;0.52) | −0.40 (−0.88;0.08) |
| 1 year | 1.01 (0.85; 1.18) | 1.20 (1.06; 1.34) | −0.25 (−0.59;0.10) | 0.17 (−0.13;0.47) | −0.88 (−1.59;‐0.17) | −0.49 (−1.08;0.09) | −0.45 (−1.10;0.21) | −0.48 (−0.96;0.01) |
| 2 years | 1.29 (1.13; 1.45) | 1.47 (1.32; 1.61) | −0.41 (−0.77;‐0.05) | 0.08 (−0.23;0.40) | −0.69 (−1.40;0.01) | −0.59 (−1.18;‐0.01) | −0.31 (−0.92;0.30) | −0.28 (−0.73;0.17) |
| 3 years | 1.63 (1.48; 1.78) | 1.95 (1.81; 2.09) | −0.27 (−0.62;0.08) | 0.23 (−0.09;0.54) | −0.42 (−1.20;0.36) | −0.52 (−1.16;0.13) | 0.38 (−0.27;1.03) | 0.10 (−0.38;0.58) |
| 4 years | 2.06 (1.89; 2.22) | 2.53 (2.38; 2.68) | −0.06 (−0.47;0.35) | 0.34 (−0.03;0.71) | −0.05 (−0.91;0.81) | −0.22 (−0.93;0.50) | 0.91 (0.18;1.65) | 0.42 (−0.13;0.96) |
| 5 years | 2.66 (2.48; 2.83) | 3.04 (2.88; 3.20) | 0.14 (−0.31;0.60) | 0.35 (−0.07;0.76) | 0.40 (−0.56;1.36) | 0.25 (−0.56;1.06) | 1.32 (0.47;2.17) | 0.69 (0.06;1.32) |
| 6 years | 3.39 (3.18; 3.59) | 3.48 (3.29; 3.67) | 0.35 (−0.22;0.92) | 0.29 (−0.23;0.81) | 0.90 (−0.30;2.10) | 0.83 (−0.19;1.85) | 1.64 (0.59;2.70) | 0.92 (0.13;1.71) |
| 7 years | 4.19 (3.86; 4.52) | 3.89 (3.58; 4.19) | 0.55 (−0.25; 1.35) | 0.20 (−0.51; 0.91) | 1.43 (0.16; 3.01) | 1.48 (0.12; 2.84) | 1.91 (0.55; 3.27) | 1.13 (0.1; 2.16) |
Note: Bold numbers indicate no overlapping 95% confidence intervals.
ΔBMI score between children with normal weight [reference, boys (N = 1635), girls (N = 1592)] and children with overweight [boys (N = 215), girls (N = 272)] at age 5‐6 years.
ΔBMI score between children from European origin with overweight [reference, boys (N = 89), girls (N = 117)] and children from non‐European origin with overweight [(boys, N = 126), girls (N = 155)].
Only children from European origin included (N = 206). ΔBMI score between children from high socioeconomic status with overweight [reference, boys (N = 35), girls (N = 55)] and middle SES with overweight [(boys (N = 36), girls (N = 45)]/low SES with overweight [(boys (N = 18), girls (N = 17)].
FIGURE 2.
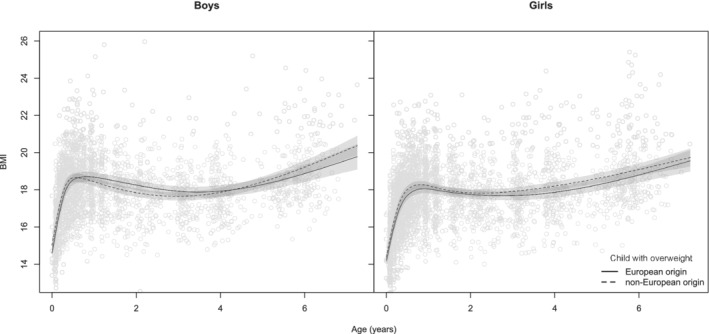
Growth patterns to normal weight and overweight at age 5‐6 years. Numbers in the different groups are: boys with normal weight (N = 1635), overweight (N = 215), girls with normal weight (N = 1592) and overweight (N = 272)
3.3. Part 2: Children with overweight at age 5‐6 years
3.3.1. BMI growth curves in children with overweight at age 5‐6 years: European vs non‐European origin children
Based on the BIC, the optimal number of degrees of freedom for the natural spline function describing the relation between BMI and age was 5 for both boys and girls. Figure 3 (lower panel) presents the BMI growth curves to overweight of boys and girls from European origin and non‐European origin. No differences were found in birth weight and subsequent growth patterns to overweight between both populations (Table 3 and Table S3). The secondary analysis indicated differences within the non‐European group, which were most pronounced for children from Turkish decent. Girls with overweight at age 5‐6 from Turkish decent showed the highest BMI peak, the earliest adiposity rebound and the highest BMI from age 2 onwards (Figure SS1).
FIGURE 3.
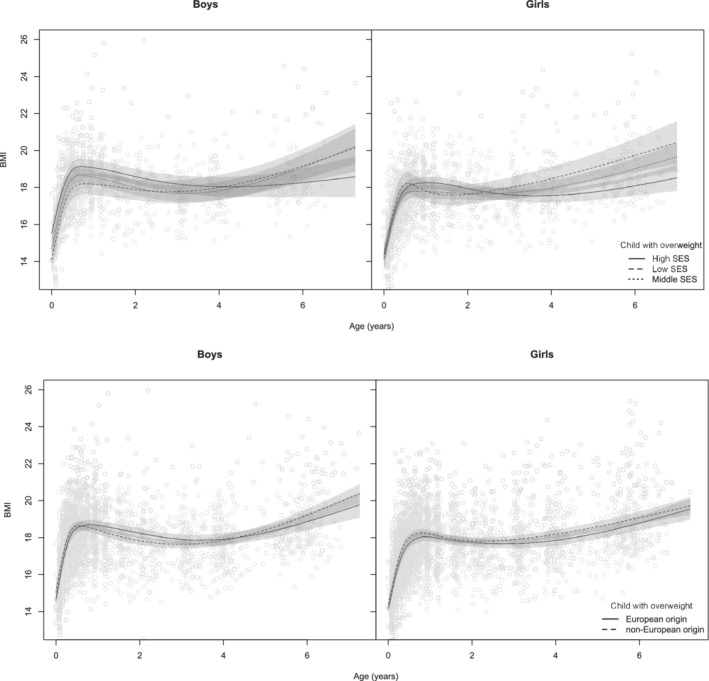
Growth patterns to overweight at age 5‐6 years by maternal country of origin (lower panel) and socioeconomic status (only women from European origin; upper panel). Numbers in the different groups are: boys from low SES (N = 82), mid SES (N = 87), high SES (N = 43), girls from low SES (N = 99), mid SES (N = 101), high SES (N = 66). Boys from European origin (N = 89), non‐European origin (N = 126), girls from European origin (N = 117) and non‐European origin (N = 155). SES, socioeconomic status
3.3.2. BMI growth curves in children with overweight at age 5‐6 years: children from lower vs higher SES background
Based on the BIC, the optimal number of degrees of freedom for the natural spline function describing the relation between BMI and age was 4 for both boys and girls. Figure 3 (upper panel) presents the growth to overweight for children from different SES groups, in children of European origin only. No differences in the growth patterns to overweight were found between children of low and middle SES, but both groups differed from the growth patterns observed in the higher SES group. Although timing and magnitude of the BMI peak was similar for all SES groups, the low/middle SES groups had a lower BMI during the first 2 years (only statistically significant for the low group; Table 3) and an earlier adiposity rebound (Figure 3) than children from the high SES group. After age 3 years BMI increased rapidly in the low/middle SES group and at age 7 years the children with overweight in low/middle SES groups had a higher mean BMI than those in the high SES group (Table 3).
4. DISCUSSION
This study investigated socioeconomic and country of origin inequalities in BMI growth patterns to overweight at age 5‐6 years, for boys and girls separately. No differences in BMI growth patterns to overweight were found when comparing European origin children with non‐European origin children. However, children with overweight in the low/middle SES group had a lower BMI during the first 2 years, an earlier adiposity rebound and a higher BMI at age 5‐6 years compared to children with overweight in the high SES group.
4.1. Strengths and Limitations
An important strength of this study was its longitudinal design with, on average, 13 standardized measurements at standard times performed by trained health care professionals in municipal Youth Health Care centers. However, this study had some limitations as well. First, we cannot rule out that there are no disparities in growth patterns to overweight in individual country of origin groups. Earlier research within the ABCD study showed that from 0 to3 years, Surinamese children have lower BMIs and Moroccan and Turkish children have higher BMIs compared to the Dutch children, 29 while all three groups have higher percentages of overweight at age 5‐6 years,35, 36 indicating that growth patterns to overweight might differ between specific non‐European origin groups. Our secondary analysis with more subdivisions of the non‐European group into Turkish, Moroccan and Surinamese children confirmed these differences in growth patterns in children with overweight, with children from Turkish decent (especially girls) showing the most detrimental BMI growth pattern to overweight. However, we should keep in mind that the individual groups were not large and therefore were combined into one non‐European origin group in our main analysis. More research is needed to confirm our preliminary findings with larger numbers. Second, we might have underestimated the inequalities in BMI growth patterns, due to the lower prevalence of overweight in this study (girls: 14.6%; boys: 11.6%) compared to the prevalence nationwide (girls: 18.5%; boys: 14.6%). 37 Fewer children with overweight, results in lower power to generate differences in growth patterns.
4.2. Comparison with the literature
This study confirms earlier reported growth patterns to overweight in the total population: children with overweight had higher birth weight, a higher BMI peak and an earlier adiposity rebound.6, 7, 12, 13, 14 Moreover, to our knowledge, this is the first study that compared longitudinal growth patterns to childhood overweight in separate groups with a higher risk for overweight and focusses on socioeconomic and country of origin inequalities in BMI growth patterns for boys and girls separately. This study found a higher prevalence of overweight in the non‐European origin children at age 5‐6 years, but a similar growth pattern to overweight for children of European origin and non‐European origin. Therefore, this study adds to the literature that ethnic inequalities in growth patterns, for instance, accelerated growth in the first year, might simply be a reflection of the higher prevalence of overweight in these groups,29, 38, 39, 40 rather than a specific ethnic growth pattern. Regarding SES, this study also found a higher prevalence of overweight in the low SES group compared to the high SES group. In contrast to the country of origin groups, however, also the growth patterns to overweight were different for the low and high SES group. The BMI of children with overweight at age 5‐6 was lower in the low SES group during the first two years, but higher at age 5‐6 years compared to the high SES group. Others did not distinguish between children with and without overweight, but did find similar patterns when socioeconomic inequalities in BMI growth were studied. In Generation R and ALSPAC, children in the low SES group had a lower BMI at age 2 years,41, 42 but a higher BMI at age 6 and 10 years.41, 43 This suggests that, socioeconomic inequalities in growth patterns do not simply result from socioeconomic inequalities in prevalence of overweight, but that children with a low socioeconomic background who end up being overweight, truly have a different growth pattern towards that overweight than children of a high socioeconomic background.
4.3. Underlying mechanisms
There are different mechanisms that could underlie the SES differences found in our cohort, but infant feeding patterns can probably be ruled out. Although children with low SES in our cohort had shorter breastfeeding duration and earlier introduction of solid foods, 44 which is associated with the development of childhood overweight,45, 46 they had lower BMIs in the first 2 years.
Moreover, within our cohort, differences in feeding style did not mediate the association of low SES with weight‐for‐length gain from 1‐5 years. 44 The lower BMI in the first 2 years might be explained by maternal smoking. Maternal smoking during pregnancy impairs foetal growth and causes low birth weight,47, 48, 49 which often leads to catch‐up growth and an increased risk of overweight in childhood. 50 In this study, 35% of the mothers with a low SES smoked during pregnancy, this was even higher (51%) if their children were overweight at age 5‐6 years (Table S5). A previous study within our cohort showed that maternal smoking during pregnancy largely attributed to the higher prevalence of infants born small‐for‐gestational age in the low SES group. 51 Therefore, the socioeconomic differences in growth patterns to overweight observed in infancy could be explained by maternal smoking during pregnancy. Furthermore, in the earlier mentioned study on the association between SES and weight‐for‐length gain from 1 to 5 years, the most important mediator was maternal pre‐pregnancy BMI. 44 The increased growth after two years might therefore be a consequence of maternal overweight, as prevalence of maternal overweight is higher in women of low SES.52, 53, 54, 55 related to an unhealthier lifestyle. Important childhood mediators in the inverse association between SES and childhood overweight at age 5 years are maternal TV watching, consuming breakfast and TV watching by the child. 56 More in general, not participating in organized sport was found to be associated with increased BMI z‐scores, 57 and children with overweight from a low socioeconomic background sleep shorter than their peers with normal weight.58, 59 In our study, children in the low SES group had more often mothers with overweight, they watched more TV and slept less, and were less often a member of a sports club (Table S5). Another explanation for the accelerated growth of children from the low SES group might be that mothers/parents perceive the child's overweight as normal and therefore take no action to change their lifestyle. Maternal underestimation of child's weight is more common in mother from low SES compared to mother from high SES. 60 The recognition of child's overweight is an important first step for the success of interventions aimed at prevention of further accelerated weight gain.
4.4. Implications
This study showed that children with overweight from the low/middle SES group have lower BMIs in the first year compared to the high SES group, but after 2 years, these groups accelerated in growth and had a higher BMI at age 5‐6 years. Therefore, it is important to closely monitor children with a low SES background as their weight might be in the normal range before the age of 2, but this does not prevent them from being at risk of developing overweight later on. An early adiposity rebound should be an indicator for extra care, but to identify the adiposity rebound, it is necessary to measure anthropometrics frequently, for instance every 3‐4 months, in both infancy and early childhood. This is of foremost importance as BMI in childhood is a predictor of adult BMI3, 4, 5 and childhood SES has a greater influence on adult BMI and the prevalence of overweight/obesity than adult SES. 61 A combination of both a low SES and high BMI in early childhood might therefore be most detrimental for adult BMI.
5. CONCLUSION
To our knowledge, this is the first study that compares growth patterns to overweight between children from different socioeconomic and country of origin groups. Stratification by SES and country of origin background showed that the development of overweight is broadly similar for children from European origin and non‐European origin. However, children with overweight from a low SES background had a lower BMI during the first 2 years, but an earlier adiposity rebound and a more rapid BMI development after 2 years compared to children in the high SES group. Our results imply that within the Youth Health Care a distinction should be made according to children's SES in determining the critical periods in childhood growth.
CONFLICT OF INTEREST STATEMENT
No conflict of interest was declared.
AUTHOR CONTRIBUTIONS
A. J. J. M. O and M. H. P. H. conducted the analysis. A. J. J. M. O drafted the initial manuscript. All authors were involved in setting up the study, writing the paper and had final approval of the submitted and published version.
Supporting information
Figure S1.
Table S1. Non‐response analysis.
Table S2. BMI (kg/m2) of boys and girls with normal weight and overweight at age 5‐6 years.
Table S3. BMI (kg/m2) of overweight boys and girls at age 5‐6 years, split on maternal country of origin.
Table S4. BMI (kg/m2) of overweight boys and girls at age 5‐6 years, split on maternal socioeconomic status (only children from European origin Included).
Table S5. SES differences in obesogenic environment (only children from European origin included, N = 2579).
ACKNOWLEDGEMENTS
The authors thank the participating mothers and their children, and all other persons and institutions who contributed to the ABCD study: obstetric care providers, primary schools, students, and Youth Healthcare Centres in Amsterdam (the Netherlands). This study was supported by the Netherlands Organization for Health Research and Development (ZonMw) Grant (TOP, 40‐00812‐98‐11010).
Vrijkotte TGM, Oostvogels AJJM, Stronks K, Roseboom TJ, Hof MHP. Growth patterns from birth to overweight at age 5‐6 years of children with various backgrounds in socioeconomic status and country of origin: the ABCD study. Pediatric Obesity. 2020;15:e12635 10.1111/ijpo.12635
The copyright line for this article was changed on 20 April 2020 after original online publication.
REFERENCES
- 1. Wang Y, Lobstein T. Worldwide trends in childhood overweight and obesity. Int J Pediatr Obes. 2006;1(1):11‐25. [DOI] [PubMed] [Google Scholar]
- 2. Daniels SR. Cardiovascular disease risk factors and atherosclerosis in children and adolescents. Curr Atheroscler Rep. 2001;3(6):479‐485. [DOI] [PubMed] [Google Scholar]
- 3. Hardy LR, Harrell JS, Bell RA. Overweight in children: definitions, measurements, confounding factors, and health consequences. J Pediatr Nurs. 2004;19(6):376‐384. [DOI] [PubMed] [Google Scholar]
- 4. Field AE, Cook NR, Gillman MW. Weight status in childhood as a predictor of becoming overweight or hypertensive in early adulthood. Obes Res. 2005;13(1):163‐169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Baker JL, Olsen LW, Sorensen TI. Childhood body‐mass index and the risk of coronary heart disease in adulthood. N Engl J Med. 2007;357(23):2329‐2337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Glavin K, Roelants M, Strand BH, et al. Important periods of weight development in childhood: a population‐based longitudinal study. BMC Public Health. 2014;14:160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Willers SM, Brunekreef B, Smit HA, et al. BMI development of normal weight and overweight children in the PIAMA study. PloS One. 2012;7(6):e39517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Lagstrom H, Hakanen M, Niinikoski H, et al. Growth patterns and obesity development in overweight or normal‐weight 13‐year‐old adolescents: the STRIP study. Pediatrics. 2008;122(4):e876‐e883. [DOI] [PubMed] [Google Scholar]
- 9. Harrington JW, Nguyen VQ, Paulson JF, Garland R, Pasquinelli L, Lewis D. Identifying the “tipping point” age for overweight pediatric patients. Clin Pediatr (Phila). 2010;49(7):638‐643. [DOI] [PubMed] [Google Scholar]
- 10. Giles LC, Whitrow MJ, Rumbold AR, et al. Growth in early life and the development of obesity by age 9 years: are there critical periods and a role for an early life stressor? Int J Obes (Lond). 2013;37(4):513‐519. [DOI] [PubMed] [Google Scholar]
- 11. Min J, Li J, Li Z, Wang Y. Impacts of infancy rapid weight gain on 5‐year childhood overweight development vary by age and sex in China. Pediatr Obes. 2012;7(5):365‐373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Sovio U, Kaakinen M, Tzoulaki I, et al. How do changes in body mass index in infancy and childhood associate with cardiometabolic profile in adulthood? Findings from the Northern Finland Birth Cohort 1966 Study. Inter J Obes. 2014;38(1):53‐59. [DOI] [PubMed] [Google Scholar]
- 13. Hof MH, Vrijkotte TG, de Hoog ML, van Eijsden M, Zwinderman AH. Association between infancy BMI peak and body composition and blood pressure at age 5‐6 years. PloS One. 2013;8(12):e80517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Rolland‐Cachera MF, Deheeger M, Bellisle F, Sempe M, Guilloud‐Bataille M, Patois E. Adiposity rebound in children: a simple indicator for predicting obesity. Am J Clin Nutr. 1984;39(1):129‐135. [DOI] [PubMed] [Google Scholar]
- 15. Blumenshine P, Egerter S, Barclay CJ, Cubbin C, Braveman PA. Socioeconomic disparities in adverse birth outcomes: a systematic review. Am J Prev Med. 2010;39(3):263‐272. [DOI] [PubMed] [Google Scholar]
- 16. Raisanen S, Gissler M, Sankilampi U, Saari J, Kramer MR, Heinonen S. Contribution of socioeconomic status to the risk of small for gestational age infants—a population‐based study of 1,390,165 singleton live births in Finland. Int J Equity Health. 2013;12:28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. de Hoog ML, van Eijsden M, Stronks K, Gemke RJ, Vrijkotte TG. Overweight at age two years in a multi‐ethnic cohort (ABCD study): the role of prenatal factors, birth outcomes and postnatal factors. BMC Public Health. 2011;11:611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. van Rossem L, Hafkamp‐de Groen E, Jaddoe VW, Hofman A, Mackenbach JP, Raat H. The role of early life factors in the development of ethnic differences in growth and overweight in preschool children: a prospective birth cohort. BMC Public Health. 2014;14:722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Troe EJ, Raat H, Jaddoe VW, et al. Explaining differences in birthweight between ethnic populations. The Generation R Study. BJOG. 2007;114(12):1557‐1565. [DOI] [PubMed] [Google Scholar]
- 20. Goedhart G, van Eijsden M, van der Wal MF, Bonsel GJ. Ethnic differences in term birthweight: the role of constitutional and environmental factors. Paediatr Perinat Epidemiol. 2008;22(4):360‐368. [DOI] [PubMed] [Google Scholar]
- 21. Griffiths LJ, Tate AR, Dezateux C. Do early infant feeding practices vary by maternal ethnic group? Public Health Nutr. 2007;10(9):957‐964. [DOI] [PubMed] [Google Scholar]
- 22. Kramer MS, Matush L, Vanilovich I, et al. Effects of prolonged and exclusive breastfeeding on child height, weight, adiposity, and blood pressure at age 6.5 y: evidence from a large randomized trial. Am J Clin Nutr. 2007;86(6):1717‐1721. [DOI] [PubMed] [Google Scholar]
- 23. Gillman MW, Rifas‐Shiman SL, Berkey CS, et al. Breast‐feeding and overweight in adolescence. Epidemiology. 2006;17(1):112‐114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Colen CG, Ramey D.M. Is breast truly best? Estimating the effects of breastfeeding on long‐term child health and wellbeing in the United States using sibling comparisons. Soc Sci Med. 2014;109:55–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Rzehak P, Sausenthaler S, Koletzko S, et al. Period‐specific growth, overweight and modification by breastfeeding in the GINI and LISA birth cohorts up to age 6 years. Eur J Epidemiol. 2009;24(8):449‐467. [DOI] [PubMed] [Google Scholar]
- 26. de Hoog ML, van Eijsden M, Stronks K, Gemke RJ, Vrijkotte TG. The role of infant feeding practices in the explanation for ethnic differences in infant growth: the Amsterdam Born Children and their development study. Br J Nutr. 2011;106(10):1592‐1601. [DOI] [PubMed] [Google Scholar]
- 27. Bulk‐Bunschoten AM, Pasker‐de Jong PC, van Wouwe JP, de Groot CJ. Ethnic variation in infant‐feeding practices in the Netherlands and weight gain at 4 months. J Hum Lact. 2008;24(1):42‐49. [DOI] [PubMed] [Google Scholar]
- 28. de Zegher F, Devlieger H, Eeckels R. Fetal growth: boys before girls. Horm Res. 1999;51(5):258‐259. [DOI] [PubMed] [Google Scholar]
- 29. Hof MH, van Dijk AE, van Eijsden M, Vrijkotte TG, Zwinderman AH. Comparison of growth between native and immigrant infants between 0‐3 years from the Dutch ABCD cohort. Ann Hum Biol. 2011;38(5):544‐555. [DOI] [PubMed] [Google Scholar]
- 30. van Eijsden M, Vrijkotte TG, Gemke RJ, van der Wal MF. Cohort profile: the Amsterdam Born Children and their Development (ABCD) study. Int J Epidemiol. 2011;40(5):1176‐1186. [DOI] [PubMed] [Google Scholar]
- 31. Cole TJ. Fitting smoothed centile curves to reference data. J R Stat Soc Ser A Stat Soc. 1988;151(3):385‐418. [Google Scholar]
- 32. van Dijk AE, van Eijsden M, Stronks K, Gemke RJ, Vrijkotte TG. Cardio‐metabolic risk in 5‐year‐old children prenatally exposed to maternal psychosocial stress: the ABCD study. BMC Public Health. 2010;10:251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Cole TJ, Lobstein T. Extended international (IOTF) body mass index cut‐offs for thinness, overweight and obesity. Pediatr Obes. 2012;7(4):284‐294. [DOI] [PubMed] [Google Scholar]
- 34. West BT, Welch KB, Galecki AT. Linear Mixed Models: A Practical Guide Using Statistical Software. Boca Raton: Chapman and Hall/CRC; 2014. [Google Scholar]
- 35. de Hoog ML, van Eijsden M, Stronks K, Gemke RJ, Vrijkotte TG. Ethnic differences in cardiometabolic risk profile at age 5–6 years: the ABCD study. PLoS One. 2012;7(8):e43667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Gishti O, Kruithof CJ, Felix JF, et al. Ethnic disparities in general and abdominal adiposity at school age: a multiethnic population‐based cohort study in the Netherlands. Ann Nutr Metab. 2014;64(3–4):208‐217. [DOI] [PubMed] [Google Scholar]
- 37. Schonbeck Y, Talma H, van Dommelen P, et al. Increase in prevalence of overweight in Dutch children and adolescents: a comparison of nationwide growth studies in 1980, 1997 and 2009. PloS One. 2011;6(11):e27608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Fredriks AM, van Buuren S, Jeurissen SE, Dekker FW, Verloove‐Vanhorick SP, Wit JM. Height, weight, body mass index and pubertal development references for children of Moroccan origin in The Netherlands. Acta Paediatr. 2004;93(6):817‐824. [DOI] [PubMed] [Google Scholar]
- 39. Fredriks AM, van Buuren S, Jeurissen SE, Dekker FW, Verloove‐Vanhorick SP, Wit JM. Height, weight, body mass index and pubertal development reference values for children of Turkish origin in the Netherlands. Eur J Pediatr. 2003;162(11):788‐793. [DOI] [PubMed] [Google Scholar]
- 40. Fredriks AM, Van Buuren S, Sing RA, Wit JM, Verloove‐Vanhorick SP. Alarming prevalences of overweight and obesity for children of Turkish, Moroccan and Dutch origin in The Netherlands according to international standards. Acta Paediatr. 2005;94(4):496‐498. [DOI] [PubMed] [Google Scholar]
- 41. Howe LD, Tilling K, Galobardes B, Smith GD, Ness AR, Lawlor DA. Socioeconomic disparities in trajectories of adiposity across childhood. Int J Pediatr Obes. 2011;6(2–2):e144‐e153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. van Rossem L, Silva LM, Hokken‐Koelega A, et al. Socioeconomic status is not inversely associated with overweight in preschool children. J Pediatr. 2010;157(6):929‐935. e1. [DOI] [PubMed] [Google Scholar]
- 43. Bouthoorn SH, Wijtzes AI, Jaddoe VW, Hofman A, Raat H, van Lenthe FJ. Development of socioeconomic inequalities in obesity among Dutch pre‐school and school‐aged children. Obesity. 2014;22(10):2230‐2237. [DOI] [PubMed] [Google Scholar]
- 44. Van Den Berg G, Van Eijsden M, Galindo‐Garre F, Vrijkotte T, Gemke R. Low maternal education is associated with increased growth velocity in the first year of life and in early childhood: the ABCD study. Eur J Pediatr. 2013;172(11):1451‐1457. [DOI] [PubMed] [Google Scholar]
- 45. Gillman MW, Rifas‐Shiman SL, Camargo CA, et al. Risk of overweight among adolescents who were breastfed as infants. JAMA. 2001;285(19):2461‐2467. [DOI] [PubMed] [Google Scholar]
- 46. Gunnarsdottir I, Schack‐Nielsen L, Michaelsen KF, Sorensen TI, Thorsdottir I, NordNet SG. Infant weight gain, duration of exclusive breast‐feeding and childhood BMI – two similar follow‐up cohorts. Public Health Nutr. 2010;13(2):201‐207. [DOI] [PubMed] [Google Scholar]
- 47. Bernstein IM, Mongeon JA, Badger GJ, Solomon L, Heil SH, Higgins ST. Maternal smoking and its association with birth weight. Obstet Gynecol. 2005;106(5 Pt 1):986‐991. [DOI] [PubMed] [Google Scholar]
- 48. Erickson AC, Arbour LT. Heavy smoking during pregnancy as a marker for other risk factors of adverse birth outcomes: a population‐based study in British Columbia, Canada. BMC Public Health. 2012;12:102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Mehaffey K, Higginson A, Cowan J, Osborne GM, Arbour LT. Maternal smoking at first prenatal visit as a marker of risk for adverse pregnancy outcomes in the Qikiqtaaluk (Baffin) Region. Rural Remote Health. 2010;10(3):1484. [PubMed] [Google Scholar]
- 50. Dubois L, Girard M. Early determinants of overweight at 4.5 years in a population‐based longitudinal study. Int J Obes (Lond). 2006;30(4):610‐617. [DOI] [PubMed] [Google Scholar]
- 51. van den Berg G, van Eijsden M, Galindo‐Garre F, Vrijkotte TG, Gemke RJ. Smoking overrules many other risk factors for small for gestational age birth in less educated mothers. Early Hum Dev. 2013;89(7):497‐501. [DOI] [PubMed] [Google Scholar]
- 52. Ng SK, Cameron CM, Hills AP, McClure RJ, Scuffham PA. Socioeconomic disparities in prepregnancy BMI and impact on maternal and neonatal outcomes and postpartum weight retention: the EFHL longitudinal birth cohort study. BMC Pregnancy Childbirth. 2014;14:314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Holowko N, Chaparro MP, Nilsson K, et al. Social inequality in pre‐pregnancy BMI and gestational weight gain in the first and second pregnancy among women in Sweden. JECH. 2015;69(12):1154‐1161. [DOI] [PubMed] [Google Scholar]
- 54. Knight B, Shields BM, Hill A, Powell RJ, Wright D, Hattersley AT. The impact of maternal glycemia and obesity on early postnatal growth in a nondiabetic Caucasian population. Diabetes Care. 2007;30(4):777‐783. [DOI] [PubMed] [Google Scholar]
- 55. Botton J, Heude B, Maccario J, et al. Parental body size and early weight and height growth velocities in their offspring. Early Hum Dev. 2010;86(7):445‐450. [DOI] [PubMed] [Google Scholar]
- 56. Veldhuis L, Vogel I, van Rossem L, et al. Influence of maternal and child lifestyle‐related characteristics on the socioeconomic inequality in overweight and obesity among 5‐year‐old children; the “Be Active, Eat Right” Study. Int J Environ Res Public Health. 2013;10(6):2336‐2347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Koning M, Hoekstra T, de Jong E, Visscher TL, Seidell JC, Renders CM. Identifying developmental trajectories of body mass index in childhood using latent class growth (mixture) modelling: associations with dietary, sedentary and physical activity behaviors: a longitudinal study. BMC Public Health. 2016;16(1):1128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Appelhans BM, Fitzpatrick SL, Li H, et al. The home environment and childhood obesity in low‐income households: indirect effects via sleep duration and screen time. BMC Public Health. 2014;14:1160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. O'Dea JA, Dibley MJ, Rankin NM. Low sleep and low socioeconomic status predict high body mass index: a 4‐year longitudinal study of Australian schoolchildren. Pediatr Obes. 2012;7(4):295‐303. [DOI] [PubMed] [Google Scholar]
- 60. de Hoog ML, Stronks K, van Eijsden M, Gemke RJ, Vrijkotte TG. Ethnic differences in maternal underestimation of offspring's weight: the ABCD study. Int J Obes (Lond). 2012;36(1):53‐60. [DOI] [PubMed] [Google Scholar]
- 61. Giskes K, van Lenthe FJ, Turrell G, Kamphuis CB, Brug J, Mackenbach JP. Socioeconomic position at different stages of the life course and its influence on body weight and weight gain in adulthood: a longitudinal study with 13‐year follow‐up. Obesity. 2008;16(6):1377‐1381. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Figure S1.
Table S1. Non‐response analysis.
Table S2. BMI (kg/m2) of boys and girls with normal weight and overweight at age 5‐6 years.
Table S3. BMI (kg/m2) of overweight boys and girls at age 5‐6 years, split on maternal country of origin.
Table S4. BMI (kg/m2) of overweight boys and girls at age 5‐6 years, split on maternal socioeconomic status (only children from European origin Included).
Table S5. SES differences in obesogenic environment (only children from European origin included, N = 2579).


