Abstract
Background
The benefit of mechanical thrombectomy for an acute ischemic stroke involving M2 segment occlusion is not clear, especially when performed with second-generation thrombectomy devices.
Method
We reviewed the literature to investigate clinical outcomes and the rates of recanalization, symptomatic intracerebral hematoma, and mortality in mechanical thrombectomy performed using second-generation thrombectomy devices. We compared the outcomes between patients treated for M2 and M1 occlusions.
Results
Seven studies involving 805 patients with M2 thrombectomy were included in this meta-analysis. The functional independence rate 90 days after thrombectomy (modified Rankin Scale 0–2) was 59.3% (OR 1.81, 95% CI 1.74–1.88). The recanalization rate (thrombolysis in cerebral infarction 0–2) was 84.16% (OR 2.32, 95% CI 2.08–2.29). The symptomatic intracerebral hematoma rate was 4.9% (OR 1.05, 95% CI 1.03–1.09). The mortality was 7.7% (OR 1.08, 95% CI 1.03–1.13). The outcomes were better in patients with M2 occlusion than in those with M1 occlusion. In a subgroup analysis, we found that among patients with hypertension, mechanical thrombectomy achieved better functional outcomes and recanalization in M2 occlusion than M1 occlusion.
Conclusion
Mechanical thrombectomy performed with second-generation thrombectomy devices for M2 occlusion can provide a good functional outcome as well as satisfying recanalization. Moreover, there was no significant difference in the symptomatic intracerebral hematoma and mortality rates, suggesting this procedure is as safe in M2 occlusion as in M1 occlusion.
Keywords: Device, stroke, stent, thrombectomy
Introduction
Endovascular treatment, especially mechanical thrombectomy (MT), is considered a class IA treatment for acute ischemic stroke caused by occlusion of large vessels (the internal carotid artery and M1 segment) by current recommendations.1,2 Although the benefits of MT in patients with occlusion of the internal carotid artery and main middle cerebral artery (MCA) trunk have been demonstrated in several large clinical trials,3–7 it remains unclear whether satisfying outcomes can be achieved using MT in patients with occlusion in the first division of the MCA segment, which is considered for class IIB treatment in the current guidelines.2
M2 occlusions comprise approximately 20–41% of anterior circulation strokes and leaves patients with poor outcomes;8 intravenous thrombolysis remains the most widely used method of reperfusion therapy. However, only 1/3 of patients with M2 occlusion achieve recanalization when treated with intravenous tissue plasminogen activator (IV tPA),9 leaving patients with poor outcomes.8
A post hoc analysis of STAR, SWIFT, and SWIFT PRIME studies showed that there were no significant differences between M1 and M2 in the rates of successful reperfusion (85% versus 82%, P = 0.82), symptomatic intracerebral hemorrhages (sICHs) (2% versus 2%, P = 1.0), or device-related serious adverse events (6% versus 4%, P = 0.46) or modified Rankin Scale (mRS) scores of 0–2 at follow-up (60% versus 56%, P = 0.64), similar to results reported in other studies (MR CLEAN, ESCAPE, REVACAT, EXTEND-IA, STAR, and DEFUSE 2);4–7 however, the numbers and percentages of M2 cases were too low in these studies to come to a definitive conclusion. Later, two meta-analysis10,11 and one systematic review12 suggested that this approach was beneficial in M2 occlusion. However, the thrombectomy devices used in the trials included in the studies listed above were mainly first-generation devices, which have since been replaced by second-generation devices. To clarify the role of MT performed with second-generation thrombectomy devices in M2 occlusion, we conducted a systematic review and meta-analysis to evaluate its safety and efficacy.
Method
Literature search
This systematic review was conducted following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines.13 Ethical approval was not required to perform this study due to its nonexperimental design. The research strategies and literature searches were performed in March 2019 using the PubMed, Web of Science, and Cochrane databases (these cover the major databases, including EMBASE and MEDLINE). The searches were performed by two of the authors (GL and RH), who have a sufficient amount of experience in the field of neurology and extensive knowledge of evidence-based medicine to assess all of the articles for their suitability. The search terms included “M2” AND (“middle cerebral artery” OR “MCA”) AND (“mechanical” OR “thrombectomy” OR “endovascular”). Duplicates were removed from records identified in the database search. Articles were then screened based on their titles and abstracts, and the remaining papers underwent full-text review independently by the two reviewers. The Newcastle–Ottawa Scale was used to estimate the methodological quality of the studies included in the final analysis independently by each of the two reviewers. A consensus was achieved if there was a disagreement.
The inclusion criteria were as follows:
Articles published after 1 January 2015.
Studies including at least 10 patients treated with MT for acute ischemic stroke due to M2 occlusion.
Studies reporting at least one measured clinical outcome for patients treated with M2 thrombectomy.
Modern second-generation thrombectomy devices (Solitaire (Covidien/ev3 Inc., Irvine, CA) or Trevo (Concentric Medical, Mountain View, CA, USA) or stent retriever system) were used in >55% of the cases.
The abstracts of all selected studies were reviewed, and case series, case reports, reviewers, and animal experiments were excluded.
Data extraction and outcomes
Demographic and baseline information (the number of patients and their age, sex, initial National Institutes of Health Stroke Scale (NIHSS) scores, and Alberta Stroke Program Early CT (ASPECT) scores and the percentage of patients with other chronic diseases, including atrial fibrillation, hypertension, hyperlipidemia, and diabetes mellitus), treatment (MT device type, proportion of patients who received IV tPA before thrombectomy, MT attempts, onset to recanalization times), and clinical and safety outcomes were extracted from eligible studies. All studies were reviewed, and data were extracted independently by two separate reviewers (GL and RH). A consensus was reached based on discussion if there was a disagreement between the two reviewers.
Clinical outcomes of interest included successful recanalization (thrombolysis in cerebral infarction (TICI) 2 b/3 or modified TICI 2 b/3 recanalization rate) and 90-day functional independence (mRS 0–2 rate at 90 days). Clinical safety outcomes of interest included the 90-day mortality rate and the rate of sICH (defined as any type of hemorrhage with an increase of ≥4 in NIHSS score).
Statistical analysis
Both clinical outcomes for M2 thrombectomy and comparisons of outcomes for M1 versus M2 thrombectomy were performed using ReviewManager (RevMan) Version 5.3. A random effects model was used for meta-analysis if the heterogeneity was high, and a fixed effects model was used for the meta-analysis if the heterogeneity was low, with results presented as odd ratios (ORs) and 95% confidence intervals (CIs). The Cochran’s Q test and I2 test were used to detect heterogeneity. Significant heterogeneity was defined as either Q values greater than the χ2 critical value at the alpha = 0.1 level or an I2 value greater than 50%. A funnel plot for the primary efficacy outcome was not considered suggestive of publication bias based on visual inspection. A sensitivity analysis was performed only on studies of random control trials. Subgroup analyses were carried out to evaluate studies with different percentages of hypertension patients.
Results
Clinical outcomes of MCA-M2 thrombectomy
The flow of the study selection procedures is shown in online supplementary figure 1. Finally, seven studies including 805 patients treated with M2 thrombectomy were included in this analysis.14–20 Of the seven included studies, Goyal et al. studied patients with M2 occlusion included in five recent RCTs and established a post hoc analysis. The other six studies were retrospectively designed. The study characteristics are shown in Table 1, clinical and imaging characteristics are shown in Table 2, and vascular risk factors are shown in Table 3.
Table 1.
Study characteristics.
| Study | Study design | Number of centers | Region | Time window for EVT | Thrombectomy device type and percentage | Sample size |
|
|---|---|---|---|---|---|---|---|
| M1 | M2 | ||||||
| Gory et al.17 | Retrospective | 8 | France | 6 h | Stent | NA | 31 |
| Hisham Salahuddin 201720 | Retrospective | 2 | US | 6 h | Trevo/Solitaire (56.9%) | 153 | 59 |
| Bhogal14 | Retrospective | 1 | Germany | NR | Stent | 479 | 106 |
| Sarraj et al.19 | Retrospective | 10 | US | 8 h | Stent retrievers (88.9%) or aspiration techniques | NA | 522 |
| Protto18 | Perspective | 1 | Finland | NR | Stent | 46 | 22 |
| Dorn16 | Retrospective | 1 | Germany | NR | Solitaire | 104 | 15 |
| Coutinho et al.15 | Post hoc analysis | 96 | US and Europe | 6 h/8 h | Stent | 249 | 50 |
EVT: endovascular treatment; NA: not applicable; NR: not reported.
Table 2.
Clinical and imaging characteristics.
| Study | Age (years) mean ± SD |
Male (%) |
Initial NIHSS score |
Initial ASPECT score |
IV tPA (%) |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Total | M1 | M2 | Total | M1 | M2 | Total | M1 | M2 | Total | M1 | M2 | Total | M1 | M2 | |
| Gory et al.17 | NA | NA | 70.2 ± 13. | NR | NR | 58.1 | NR | NR | 13.7 ± 6.5 | NR | NR | 7 | NA | NA | 74.2 |
| Hisham Salahuddin 201720 | 70 ± 14.7 | 70.2 ± 15.3 | 69.2 ± 13.2 | 49.5 | 43.8 | 64.4 | 16 | 17 | 14 | 9 | 9 | 9 | 42.5 | 37.9 | 54.2 |
| Bhogal14 | 71.3 ± 13 | 72 ± 12.8 | 68 ± 13.8 | 50.2 | 49.3 | 54.7 | 15 | 15.7 | 11.8 | 8.5 ± 1.8 | 8.5 ± 1.88 | 8.5 ± 1.7 | NR | NR | NR |
| Sarraj et al.19 | NA | NA | 68 ± 14.3 | 49 | NR | 49 | 13 | NR | 13 | 9 | NR | 9 | 66 | NA | 66 |
| Protto18 | 66.1 ± 11.2 | 65.3 ± 12.8 | 69.8 ± 9.3 | 43 | 35 | 68 | 14.5 ± 5 | 16 ± 6 | 14 ± 6 | 9 ± 3 | 9 ± 3 | 10 ± 1 | 63 | 65 | 41 |
| Dorn16 | 69.2 ± 14.1 | 69.4 ± 14.0 | 68.1 ± 14.8 | 50.4 | 51 | 46.7 | 15.8 ± 7.5 | 16.1 ± 7.3 | 13.7 ± 8.3 | NR | NR | NR | 50.5 | 51 | 46.7 |
| Coutinho et al.15 | 67.7 ± 12.7 | 67 ± 13 | 71 ± 11 | 45 | 43 | 52 | 30 | 17 | 13 | 8.3 ± 1.6 | 8.2 ± 1.7 | 9.0 ± 1.3 | 70 | 69 | 77 |
ASPECT: Alberta Stroke Program Early CT; IV tPA: intravenous tissue plasminogen activator; NA: not applicable; NIHSS: National Institutes of Health Stroke Scale; NR: not reported.
Table 3.
Vascular risk factors.
| Study | Atrial fibrillation (%) |
Hypertension (%) |
Hyperlipidemia (%) |
DM (%) |
Smoke (%) |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Total | M1 | M2 | Total | M1 | M2 | Total | M1 | M2 | Total | M1 | M2 | Total | M1 | M2 | |
| Gory et al.17 | NR | NR | NR | 58.1 | NA | 58.1 | 33.3 | NA | 33.3 | NR | NA | 25.8 | NR | NA | 16 |
| Hisham Salahuddin 201720 | 49.5 | 52.9 | 40.7 | 78.3 | 79.7 | 74.6 | 63.7 | 62.7 | 66.1 | 29.2 | 28.1 | 32.2 | 22.6 | 21.6 | 25.4 |
| Bhogal14 | NR | 56.9 | 50.9 | NR | 73.9 | 70.7 | NR | 28.8 | 27.3 | NR | 22.7 | 29.2 | NR | 13.6 | 19.8 |
| Sarraj et al.19 | 34.2 | NA | 34.2 | NR | NA | 76.1 | NR | NA | 41.7 | NR | NA | 28.2 | NR | NA | 21.8 |
| Protto18 | NR | 54 | 50 | NR | 46 | 41 | NR | NR | NR | NR | 20 | 12 | NR | NR | NR |
| Dorn16 | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR |
| Coutinho et al.15 | NR | 37 | 38 | NR | 61 | 70 | NR | 37 | 30 | NR | 15 | 18 | NR | 21 | 14 |
DM: diabetes mellitus; NA: not applicable; NR: not reported.
In the patients with M2 occlusion, the mean age ranged from 66.1 to 71.3 years old. The median NHISS score ranged from 11.8 to 14, and the median ASPECT score ranged from 7.5 to 10. IV tPA was administered to 63.64% (455 of 715) of patients with M2 occlusion.
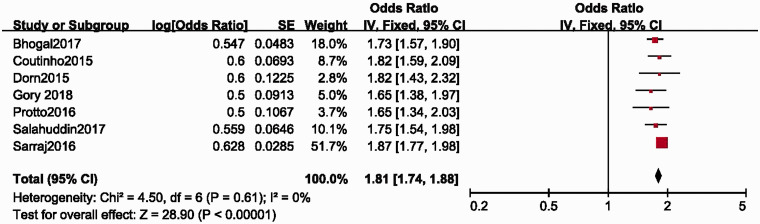
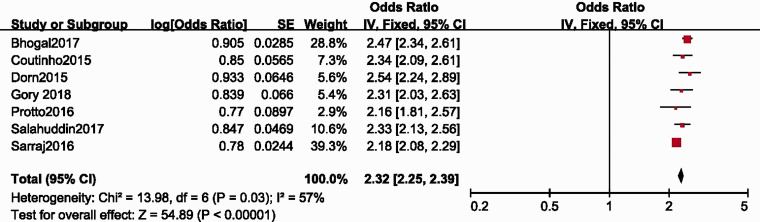
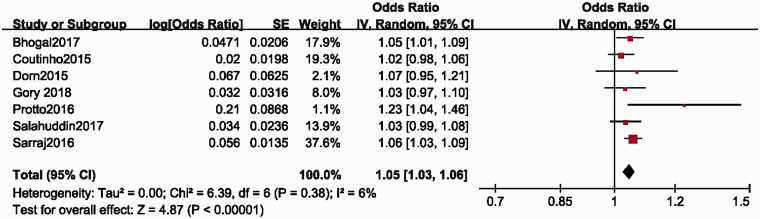
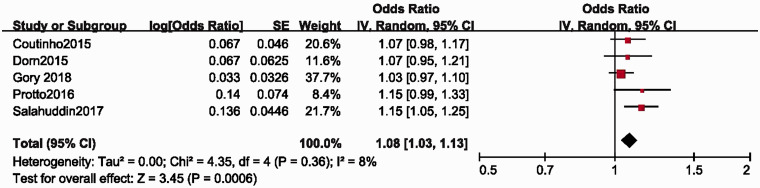
The functional independence rate (mRS at 90 days after thrombectomy) was 59.3% (OR 1.81, 95% CI 1.74–1.88) (Figure 1). The recanalization rate was 84.16% (OR 2.32, 95% CI 2.08–2.29) (Figure 2). The sICH rate was 4.9% (OR 1.05, 95% CI 1.03–1.09) (Figure 3). The mortality rate was 7.7% (OR 1.08, 95% CI 1.03–1.13) (Figure 4).
Figure 1.
The functional independence rate (mRS at 90 days after thrombectomy) was 59.3% (OR 1.81, 95% CI 1.74–1.88). CI: confidence interval; IV: intravenous; SE: standard error.
Figure 2.
The recanalization rate was 84.16% (OR 2.32, 95% CI 2.08–2.29). CI: confidence interval; IV: intravenous; SE: standard error.
Figure 3.
The sICH rate was 4.9% (OR 1.05, 95% CI 1.03–1.09). CI: confidence interval; IV: intravenous; SE: standard error.
Figure 4.
The mortality was 7.7% (OR 1.08, 95% CI 1.03–1.13). CI: confidence interval; IV: intravenous; SE: standard error.
A sensitivity analysis of 90-day mRS 0–2 outcomes and TICI 2b/3 recanalization, when restricted to studies including RCTs, did not significantly alter the estimates significantly (56.5 and 84.6%, respectively).
MCA-M1 versus MCA-M2 thrombectomy outcomes
A total of five studies were included in an analysis comparing M2 (n = 252; mean age, 69 years old, 57.1% male patients) versus M1 (n = 1031; mean age, 70 years old, 46.5% male patients) thrombectomy.
The functional independence rate was 55.7% in patients with M2 occlusion and 45.5% in patients with M1 occlusion. The proportion of patients with mRS 0–2 was significantly higher in the M2 intervention group than in the M1 intervention group (OR 1.48, 95% CI 1.12–1.95; P = 0.23; I2 = 28%). Heterogeneity was nonsignificant across the studies (online supplementary figure 2).
Recanalization was achieved in 87.2% of the patients with M2 occlusion and 85.7% of the patients with M2 occlusion. No significant difference in TICI 2 b/3 was observed between patients with M2 or M1 occlusion (OR 1.12, 95% CI 0.73–1.71; P = 0.22; I2 = 30%). Heterogeneity was not significant across the included studies (online supplementary figure 3).
The mortality rate was 12.8% in the M2 and 13.4% in the M1 intervention group and was not significantly different between the groups (OR 0.86, 95% CI 0.46–1.21; P = 0.35; I2 = 0%). Significant heterogeneity was observed among the studies (online supplementary figure 4).
sICH was significantly lower in patients with M2 occlusion (3.9%) than in those with M1 occlusion (OR 0.94, 95% CI 0.45–1.98; P = 1; I2 = 0%). No significant heterogeneity was observed across the studies (online supplementary figure 5).
Discussion
In our meta-analysis of patients with M2 occlusion who underwent MT, 87.2% achieved successful recanalization, a high percentage achieved functional independence at 90 days, and the rates of mortality and sICH were low. Additionally, we compared patients with M2 occlusion (n = 252) with those with M1 occlusion (n = 1031) and found no significant difference in recanalization rates, functional independence, or mortality. In the subgroup analysis, we investigated the association between hypertension and 90-day mRS or recanalization and found that among patients with hypertension, MT achieved a better functional outcome (online supplementary figure 6) and had a higher recanalization rate (online supplementary figure 7) in M2 occlusion than in M1 occlusion. A sensitivity analysis showed that retrospective studies did not contribute to the heterogeneity. Because five of the clinical trials demonstrating the benefits of MT in M2 occlusions were published in 2015,3–7 we searched the literature for studies published since 2015. Moreover, as first-generation thrombectomy devices have been abandoned in most stroke centers, we embraced only those studies in which modern second-generation thrombectomy devices were mainly used.
The duration of MT varied among these studies (6 or 8 h). The median ASPECT score was similar between M2 occlusion and M1 occlusion. All of the patients underwent MR or CT angiograms before MT to ensure the existence of an isolated M1 or M2 occlusion; hence, the imaging method did not have a significant effect on our results. The rates of tPA administration also varied among the studies.
Recent clinical trials have established that MT provides a benefit in patients with acute stroke resulting from large vessel occlusion of the anterior circulation. However, the safety and efficacy of MT in patients with M2 occlusion has not been fully explored as few such patients were involved in the trials listed above21 or in the two trials finished last year (DAWN and DEFUSE 3).22,23 Because so few M2 occlusion patients were included in these trials and most of the patients with M2 occlusion were misclassified as having M1 occlusion at enrollment, the power of our results is substantially reduced. The current guidelines recommend MT as a standard method in the management of acute ischemic stroke but provide limited evidence for the use of MT in M2 occlusions.2
Considering the distal location, smaller diameter, and thinner walls in the M2 segment, the safety of performing MT in M2 remains uncertain. Investigators have tended to compare M2 data to those obtained in M1 occlusion to evaluate the safety and effectiveness of thrombectomy in M2. Previous studies showed that the difference in the benefit of MT may result from a difference in the proportions of the ischemic core and penumbra between M1 occlusion and M2 occlusion.12 Less penumbra could result in less favorable outcomes after reperfusion therapy. However, patients with M2 occlusion may achieve worse outcomes and have higher mortality rates when not treated with reperfusion therapy.24 Shi et al.25 performed a pooled analysis of the Mechanical Embolus Removal in Cerebral Ischemia (MERCI) and Multi MERCI trials and found that although the recanalization rate was higher in M2 occlusion than in M1 occlusion (TIMI score 2/3, 82% versus 60%, p = 0.03), outcomes were similar between M1 and M2 occlusions (mRS ≤ 2 on the 90th day, 41% versus 33%, p = 0.51). Notably, MERCI devices are first-generation devices and were demonstrated in the SWIFT trial to achieve worse results than were obtained by Solitaire devices in thrombectomy.26 As their application in clinical practice is on the decline, any conclusions based on this pooled analysis should be regarded cautiously.
In a subgroup analysis of patients with M2 occlusion in the five trials involving endovascular therapy with stent retrieval, no significant improvement was achieved in 90-day mRS scores (MT VS medical therapy, OR 1.28, 95% CI 0.51–3.21) or the successful reperfusion, sICH, and serious adverse events rates.21 Compared with patients with M1 occlusion, patients with M2 occlusion were older (71 versus 67 years old, p = .04), and this may have resulted in poorer outcomes regardless of other factors. Moreover, fewer passes were required to achieve recanalization in M2 occlusion than in M1 occlusion (mean 1.4 versus 1.7, p = .07), similar to another study.25 Unfortunately, only 94 patients (7%) were included in the analysis, and 50 of the patients underwent MT. This small sample size may have led to an unconvincing result.
Few studies have provided adequate data on the natural history of M2 MCA occlusion. Lima et al. investigated 48 patients with untreated M2 occlusion (median NIHSS score, 7 (interquartile range, 4–15)) and found that the rate of favorable clinical outcomes (mRS ≤ 2 on the 90th day) was 54.2%, and the mortality rate was 20.8% at six months. Moreover, he compared these results to those obtained in 52 patients with M1 occlusion (median NIHSS score, 13 (interquartile range, 6–16)) and confirmed that there was no difference in the rate of functional independence (38% versus 54%) achieved by procedures performed at intracranial arterial occlusion levels. However, the author admitted that the patients with more proximal occlusions had lower ASPECT score on nonenhanced CT scans at admission (median scores of 7 and 8, respectively; P = .01) despite their similar presentation times.27
Therefore, a randomized trial to compare the results of MT performed in patients with M2 occlusion versus medical therapy is required to evaluate its safety and effectiveness. However, it may be not feasible to carry out such a study because of the lack of clinical equipoise. In addition, surgeons tend to choose patients with less operative difficulty, resulting in selection bias. Moreover, the lack of consensus regarding the definition of an M2 vessel may have affected the inclusion and exclusion criteria and caused heterogeneity among these trials. The definitions of the M2 branch varied among the studies included in our meta-analysis and are provided in Table 4.
Table 4.
The definitions of M2 branch among the studies.
| Gory et al.17 | The M2 segment was defined as the vertical middle cerebral artery branches in the Sylvian fissure originating at the genu and extending to the next genu at the level of the operculum. If the anterior temporal artery arises from the horizontal M1 segment, it is not considered an M2 branch. |
| Hisham Salahuddin20 | The M2 MCA artery was defined as occlusion beyond the bifurcation of the M1 artery and extending to the apex of the circular sulcus. |
| Sarraj et al.19 | The start of the M2 segment of the MCA was defined as the vertical segment lying within the mesial margin of the Sylvian fissure. |
| Coutinho et al.15 | Vertical MCA branches in the Sylvian fissure originating at the genu and extending to the next genu at the level of the operculum; if the anterior temporal artery arises from the horizontal M1 segment, it will not be considered an M2 branch. |
MCA: middle cerebral artery.
A meta-analysis may be necessary as this type of study would provide more precise estimates of the effectiveness and safety of M2 thrombectomy than could be achieved by any single study and would have a better tolerance for heterogeneity among studies. A systematic review published in 2016 established that MT led to functional independence in most patients with M2 occlusion. However, that review also implied that M2 thrombectomy provided an unclear benefit when compared to the natural history of M2 occlusion. Moreover, it was acknowledged that using older-generation devices may lead to bad outcomes.12 Later, two meta-analyses suggested that MT was as safe and effective in M2 occlusion as it was in M1 occlusion, but first-generation thrombectomy devices played a significantly larger role in both studies than second-generation devices did. Therefore, we conducted this meta-analysis to determine the effectiveness and safety of thrombectomy in M2 occlusion and provide more details related to outcomes.
Our study has several limitations. First, a small number of studies were involved in our analysis, and most of them were retrospectively designed and without an adequate control group, indicating that selection bias cannot be ignored. However, the heterogeneity was acceptable in our meta-analysis, suggesting that the variation among studies was not significant. Second, no randomized design study was included as MT is not yet a routine method of treating patients with M2 occlusion in most hospitals; patients who underwent MT may be selected based on the severity of their stroke, while others may be treated with medical therapy, including IV tPA. In 2016, a large study showed that thrombectomy achieved a higher recanalization rate than was achieved by medical therapy alone (including IV rtPA), suggesting that better outcomes were achieved by thrombectomy in patients with M2 occlusion.19 In the future, more studies, especially randomized control trials, should focus on M2 occlusion and evaluate its benefit over IV tPA alone or standard medical management (antithrombotic drugs and statin drugs). Additionally, it should be noted that after CT/MR angiogram, operators may tend to select patients with less complex vascular anatomy and larger-caliber M2 vessels to perform MT. Therefore, the results of both our meta-analysis and the studies included in our meta-analysis may not reflect real-world outcomes.
Supplemental Material
Supplemental material, INE886405 Supplemetal Material1 for Mechanical thrombectomy with second-generation devices for acute cerebral middle artery M2 segment occlusion: A meta-analysis by Guangshuo Li, Rui Huang, Weishuai Li, Xiaotian Zhang and Guorong Bi in Interventional Neuroradiology
Supplemental material, INE886405 Supplemetal Material2 for Mechanical thrombectomy with second-generation devices for acute cerebral middle artery M2 segment occlusion: A meta-analysis by Guangshuo Li, Rui Huang, Weishuai Li, Xiaotian Zhang and Guorong Bi in Interventional Neuroradiology
Supplemental material, INE886405 Supplemetal Material3 for Mechanical thrombectomy with second-generation devices for acute cerebral middle artery M2 segment occlusion: A meta-analysis by Guangshuo Li, Rui Huang, Weishuai Li, Xiaotian Zhang and Guorong Bi in Interventional Neuroradiology
Supplemental material, INE886405 Supplemetal Material4 for Mechanical thrombectomy with second-generation devices for acute cerebral middle artery M2 segment occlusion: A meta-analysis by Guangshuo Li, Rui Huang, Weishuai Li, Xiaotian Zhang and Guorong Bi in Interventional Neuroradiology
Supplemental material, INE886405 Supplemetal Material5 for Mechanical thrombectomy with second-generation devices for acute cerebral middle artery M2 segment occlusion: A meta-analysis by Guangshuo Li, Rui Huang, Weishuai Li, Xiaotian Zhang and Guorong Bi in Interventional Neuroradiology
Supplemental material, INE886405 Supplemetal Material6 for Mechanical thrombectomy with second-generation devices for acute cerebral middle artery M2 segment occlusion: A meta-analysis by Guangshuo Li, Rui Huang, Weishuai Li, Xiaotian Zhang and Guorong Bi in Interventional Neuroradiology
Supplemental material, INE886405 Supplemetal Material7 for Mechanical thrombectomy with second-generation devices for acute cerebral middle artery M2 segment occlusion: A meta-analysis by Guangshuo Li, Rui Huang, Weishuai Li, Xiaotian Zhang and Guorong Bi in Interventional Neuroradiology
Declaration of conflicting interests
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
The authors received no financial support for the research, authorship, and/or publication of this article.
Supplemental material
Supplemental material for this article is available online.
References
- 1.Powers WJ, Derdeyn CP, Biller J, et al. 2015 American Heart Association/American Stroke Association focused update of the 2013 guidelines for the early management of patients with acute ischemic stroke regarding endovascular treatment: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 2015; 46: 3020–3035. [DOI] [PubMed] [Google Scholar]
- 2.Powers WJ, Rabinstein AA, Ackerson T, et al. 2018 Guidelines for the early management of patients with acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 2018; 49: e46–e99. [DOI] [PubMed] [Google Scholar]
- 3.Saver JL, Goyal M, Bonafe A, et al. Stent-retriever thrombectomy after intravenous t-PA vs. t-PA alone in stroke. N Engl J Med 2015; 372: 2285–2295. [DOI] [PubMed] [Google Scholar]
- 4.Berkhemer OA, Fransen PSS, Beumer D, et al. A randomized trial of intraarterial treatment for acute ischemic stroke. N Engl J Med 2015; 372: 11–20. [DOI] [PubMed] [Google Scholar]
- 5.Jovin TG, Chamorro A, Cobo E, et al. Thrombectomy within 8 hours after symptom onset in ischemic stroke. N Engl J Med 2015; 372: 2296–2306. [DOI] [PubMed] [Google Scholar]
- 6.Goyal M, Demchuk AM, Menon BK, et al. Randomized assessment of rapid endovascular treatment of ischemic stroke. N Engl J Med 2015; 372: 1019–1030. [DOI] [PubMed] [Google Scholar]
- 7.Campbell BC, Mitchell PJ, Kleinig TJ, et al. Endovascular therapy for ischemic stroke with perfusion-imaging selection. N Engl J Med 2015; 372: 1009–1018. [DOI] [PubMed] [Google Scholar]
- 8.Rahme R, Yeatts SD, Abruzzo TA, et al. Early reperfusion and clinical outcomes in patients with M2 occlusion: pooled analysis of the PROACT II, IMS, and IMS II studies. J Neurosurg 2014; 121: 1354–1358. [DOI] [PubMed] [Google Scholar]
- 9.Saqqur M, Uchino K, Demchuk AM, et al. Site of arterial occlusion identified by transcranial Doppler predicts the response to intravenous thrombolysis for stroke. Stroke 2007; 38: 948–954. [DOI] [PubMed] [Google Scholar]
- 10.Samuels OB, Joseph GJ, Lynn MJ, et al. A standardized method for measuring intracranial arterial stenosis. AJNR Am J Neuroradiol 2000; 21: 643–646. [PMC free article] [PubMed] [Google Scholar]
- 11.Saber H, Narayanan S, Palla M, et al. Mechanical thrombectomy for acute ischemic stroke with occlusion of the M2 segment of the middle cerebral artery: a meta-analysis. J Neurointerv Surg 2017; 10: 1–6. [DOI] [PubMed] [Google Scholar]
- 12.Chen CJ, Wang C, Buell TJ, et al. Endovascular mechanical thrombectomy for acute middle cerebral artery M2 segment occlusion: a systematic review. World Neurosurg 2017; 107: 684–691. [DOI] [PubMed] [Google Scholar]
- 13.Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 2009; 6: e1000097. [DOI] [PMC free article] [PubMed]
- 14.Bhogal P, Bucke P, AlMatter M, et al. A comparison of mechanical thrombectomy in the M1 and M2 segments of the middle cerebral artery: a review of 585 consecutive patients. Interv Neurol 2017; 6: 191–198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Coutinho JM, Liebeskind DS, Slater LA, et al. Mechanical thrombectomy for isolated M2 occlusions: a post hoc analysis of the STAR, SWIFT, and SWIFT PRIME studies. AJNR Am J Neuroradiol 2016; 37: 667–672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dorn F, Lockau H, Stetefeld H, et al. Mechanical thrombectomy of M2-occlusion. J Stroke Cerebrovasc Dis 2015; 24: 1465–1470. [DOI] [PubMed] [Google Scholar]
- 17.Gory B, Lapergue B, Blanc R, et al. Contact aspiration versus stent retriever in patients with acute ischemic stroke with M2 occlusion in the ASTER randomized trial (contact aspiration versus stent retriever for successful revascularization). Stroke 2018; 49: 461–464. [DOI] [PubMed] [Google Scholar]
- 18.Protto S, Sillanpaa N, Pienimaki JP, et al. Stent retriever thrombectomy in different thrombus locations of anterior cerebral circulation. Cardiovasc Intervent Radiol 2016; 39: 988–993. [DOI] [PubMed] [Google Scholar]
- 19.Sarraj A, Sangha N, Hussain MS, et al. Endovascular therapy for acute ischemic stroke with occlusion of the middle cerebral artery M2 segment. JAMA Neurol 2016; 73: 1291–1296. [DOI] [PubMed] [Google Scholar]
- 20.Salahuddin H, Ramaiah G, Slawski DE, et al. Mechanical thrombectomy of M1 and M2 middle cerebral artery occlusions. J Neurointerv Surg 2017; 1–5. [DOI] [PubMed]
- 21.Goyal M, Menon BK, van Zwam WH, et al. Endovascular thrombectomy after large-vessel ischaemic stroke: a meta-analysis of individual patient data from five randomised trials. Lancet 2016; 387: 1723–1731. [DOI] [PubMed] [Google Scholar]
- 22.Albers GW, Marks MP, Kemp S, et al. Thrombectomy for stroke at 6 to 16 hours with selection by perfusion imaging. N Engl J Med 2018; 378: 708–718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Nogueira RG, Jadhav AP, Haussen DC, et al. Thrombectomy 6 to 24 hours after stroke with a mismatch between deficit and infarct. N Engl J Med 2018; 378: 11–21. [DOI] [PubMed] [Google Scholar]
- 24.Hernández-Pérez M, Pérez de la Ossa N, Aleu A, et al. Natural history of acute stroke due to occlusion of the middle cerebral artery and intracranial internal carotid artery. J Neuroimaging 2014; 24: 354–358. [DOI] [PubMed]
- 25.Shi ZS, Loh Y, Walker G, et al. Clinical outcomes in middle cerebral artery trunk occlusions versus secondary division occlusions after mechanical thrombectomy: pooled analysis of the mechanical embolus removal in cerebral ischemia (MERCI) and multi MERCI trials. Stroke 2010; 41: 953–960. [DOI] [PubMed] [Google Scholar]
- 26.Saver JL, Jahan R, Levy EI, et al. Solitaire flow restoration device versus the Merci Retriever in patients with acute ischaemic stroke (SWIFT): a randomised, parallel-group, non-inferiority trial. Lancet 2012; 380: 1241–1249. [DOI] [PubMed] [Google Scholar]
- 27.Lima FO, Furie KL, Silva GS, et al. Prognosis of untreated strokes due to anterior circulation proximal intracranial arterial occlusions detected by use of computed tomography angiography. JAMA Neurol 2014; 71:151–157. [DOI] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, INE886405 Supplemetal Material1 for Mechanical thrombectomy with second-generation devices for acute cerebral middle artery M2 segment occlusion: A meta-analysis by Guangshuo Li, Rui Huang, Weishuai Li, Xiaotian Zhang and Guorong Bi in Interventional Neuroradiology
Supplemental material, INE886405 Supplemetal Material2 for Mechanical thrombectomy with second-generation devices for acute cerebral middle artery M2 segment occlusion: A meta-analysis by Guangshuo Li, Rui Huang, Weishuai Li, Xiaotian Zhang and Guorong Bi in Interventional Neuroradiology
Supplemental material, INE886405 Supplemetal Material3 for Mechanical thrombectomy with second-generation devices for acute cerebral middle artery M2 segment occlusion: A meta-analysis by Guangshuo Li, Rui Huang, Weishuai Li, Xiaotian Zhang and Guorong Bi in Interventional Neuroradiology
Supplemental material, INE886405 Supplemetal Material4 for Mechanical thrombectomy with second-generation devices for acute cerebral middle artery M2 segment occlusion: A meta-analysis by Guangshuo Li, Rui Huang, Weishuai Li, Xiaotian Zhang and Guorong Bi in Interventional Neuroradiology
Supplemental material, INE886405 Supplemetal Material5 for Mechanical thrombectomy with second-generation devices for acute cerebral middle artery M2 segment occlusion: A meta-analysis by Guangshuo Li, Rui Huang, Weishuai Li, Xiaotian Zhang and Guorong Bi in Interventional Neuroradiology
Supplemental material, INE886405 Supplemetal Material6 for Mechanical thrombectomy with second-generation devices for acute cerebral middle artery M2 segment occlusion: A meta-analysis by Guangshuo Li, Rui Huang, Weishuai Li, Xiaotian Zhang and Guorong Bi in Interventional Neuroradiology
Supplemental material, INE886405 Supplemetal Material7 for Mechanical thrombectomy with second-generation devices for acute cerebral middle artery M2 segment occlusion: A meta-analysis by Guangshuo Li, Rui Huang, Weishuai Li, Xiaotian Zhang and Guorong Bi in Interventional Neuroradiology