Abstract
Background and purpose
Cervical internal carotid artery (ICA) tortuosity is thought to impede distal catheterization during attempted mechanical thrombectomy in patients with acute ischemic stroke. This study sought to assess the morphologic characteristics of ICAs and the effects of tortuosity on thrombectomy attempts.
Methods
A retrospective review was completed of neck CTAs of patients with acute ischemic stroke due to a large vessel occlusion that underwent attempted endovascular recanalization. Significant tortuosity of ICAs was defined as the presence of kink(s) (acute (<90°) angulation), loop(s) (C- or S-shaped curvature with 2+ areas of acute (<90°) angulation), or coil(s) (full 360° turn arterial bend). Findings were statistically compared to procedure time, successful recanalization rate, patient demographics, and co-morbidities.
Results
Of 120 included patients, 47 (39.2%) had some form of tortuosity of one or both ICAs. Twenty-eight patients (23.3%) had a kink of one or both ICAs; this was followed in frequency by loops (n = 20; 16.7%) and coils (n = 8; 6.7%). Kinks were associated with lower rates of successful recanalization (p = 0.02). The presence of any tortuosity (kinks, loops, or coils) was not associated with number of passes during thrombectomy (p = 0.88), successful recanalization (p = 0.11), or total procedure time (p = 0.22). No association was noted between the presence of tortuosity and age (p = 0.96) or prior or current tobacco use (p = 0.75 and p = 0.69, respectively).
Conclusion
Among patients referred for urgent revascularization for large vessel occlusion, approximately 40% exhibit some tortuosity. Kinks may portend lower likelihood of recanalization success, although tortuosity as a whole seems to have little effect on endovascular thrombectomy.
Keywords: Carotid, coil, kink, loop, tortuosity
Introduction
The existence of ICA tortuosity among some patients has long been known; case reports detailing such arterial morphologies date back to the early 20th century.1 Many categories of tortuosity have been described, including arterial elongation, coils, kinks, and loops.2 Such findings are common among patients with acute ischemic stroke (AIS), affecting both the intra- and extra-cranial arterial vasculature.3
Tortuosity of the cervical arterial vasculature has been identified as an impedance to multiple types of endovascular procedures.4,5 In patients with AIS, carotid tortuosity may prevent ICA catheterization during recanalization attempts, and unfavorable vascular anatomy is associated with worse outcomes and increased revascularization time during thrombectomy.6,7 Nevertheless, the prevalence of tortuosity remains disputed; prior studies on the incidence of carotid artery kinks have cited frequencies ranging from 5 to 54% of patients.8–10 Furthermore, scant research has been performed on the prevalence of carotid tortuosity, specifically among patients with AIS, a glaring omission in the literature given the implications to those performing thrombectomies.3
The primary purpose of this study was to assess the prevalence of specific subsets of cervical carotid artery tortuosity in a thrombectomy cohort of patients. Secondarily, this study sought to assess the degree to which such arterial changes were associated with endovascular thrombectomy attempts.
Materials and methods
Patient selection
Institutional review board approval was obtained for the purposes of this study. A retrospective review was completed of consecutively imaged patients who presented to our institution between 8 February 2014 and 16 July 2018 who were diagnosed with AIS due to a large vessel occlusion (LVO) and were treated with endovascular mechanical thrombectomy or clot aspiration. Patients were included if pre-procedural imaging included CTA of the cervical arterial vasculature. Patients were excluded if imaging was inadequate for evaluation of ICA morphology (e.g. significantly degraded by artifact or with suboptimal timing of contrast bolus).
Tortuosity definitions
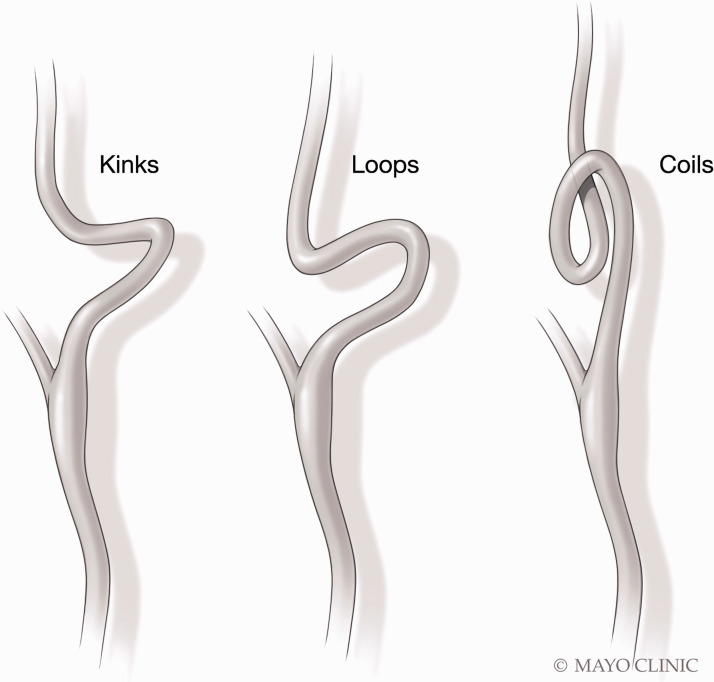
Patients were considered to have significant carotid artery tortuosity if one or more of the following were present: kink(s), loop(s), and/or coil(s). Each type of arterial tortuosity was defined based on a prior study by Barbour et al.11 Kinks represent solitary bends in the ICA with acute (<90°) angulation; loops are S- or C-shaped segments formed by two bends with acute angles (<90°); coils produce a full 360° turn in the artery (Figure 1). Retropharyngeal ICAs were defined by >50% of the ICA traveling medial to the lateral edge of the pharynx; retrojugular ICAs were defined by >50% of the ICA traveling posterior to the internal jugular vein.
Figure 1.
Illustration demonstrating the characteristic findings in cervical carotid artery kinks (a), loops (b), and coils (c).
Imaging and electronic medical record (EMR) review
A single neuroradiology fellow (JCB) completed a retrospective review of the imaging of all included patients. Images were evaluated for (1) the presence or absence of kinks, coils, or loops, and (2) variant ICA course(s) (i.e. retrojugular or retropharyngeal paths of either artery). Any arteries with markedly beaded appearance (indicative of possible fibromuscular dysplasia) were secondarily noted. A retrospective review of the EMR was completed to collect data on patients’ demographics and co-morbidities. Any history of diabetes, hypertension, hyperlipidemia, coronary artery disease, atrial fibrillation, congestive heart failure, prior stroke, prior TIA, or current or prior tobacco use was noted.
Thrombectomy procedure
In general, procedures were performed with local anesthesia only. General anesthesia was not administered for the purposes of mechanical thrombectomy. Arterial access was achieved using a 6Fr Asahi Fubuki guiding sheath placed in the right common femoral artery. Following placement of the guiding sheath in the proximal internal carotid artery, a 5Fr Sofia (125 cm) or 6Fr Sofia plus was advanced over an Avigo micro-guidewire to the occlusive lesion and aspiration thrombectomy was performed using a 60 cc manual aspiration syringe. In cases where more than three passes were necessary, the operators switched to combined aspiration and stent retriever thrombectomy using Solitaire stent retrievers placed through Rebar 18 or 27 microcatheters.
Thrombectomy review
Procedures were retrospectively reviewed for (1) number of passes during thrombectomy attempt, (2) whether the procedure resulted in successful arterial recanalization, (3) time to cross (TTC) of the occlusive thrombus (groin stick to crossing the thrombosis), and (4) total procedure time (TTP) (groin stick to revascularization). Successful recanalization was defined as thrombolysis in cerebral infarction score of 2b or 3.
Statistical analysis
Rates of carotid artery tortuosity are described using frequencies (n) and percent. Associations of tortuosity to successful recanalization, gender, and co-morbidities are examined using chi-square tests or Fisher’s exact tests. Associations of tortuosity to age, procedure time, and number of passes were tested with two sample t-tests. Analyses were conducted using SAS (version 9.4; Cary, NC). P-values are not corrected for multiple testing.
Results
Patient characteristics and carotid artery tortuosity
One hundred and twenty patients were included in the final cohort, of which 54 (44.2%) were female; mean age was 68.3 ± 13.8. Foty-seven (39.2%) patients had some form of tortuosity of an ICA (Figures 2 to 4). The most common types of ICA tortuosity were kinks (n = 28; 23.3%), followed by loops (n = 20; 16.7%) and coils (n = 8; 6.7%). Twelve kinks were on the right and 19 were on the left (three patients had bilateral kinks), 14 loops were on the right and eight were on the left (two patients had bilateral loops), and six coils were on the right and two were on the left.
Figure 3.
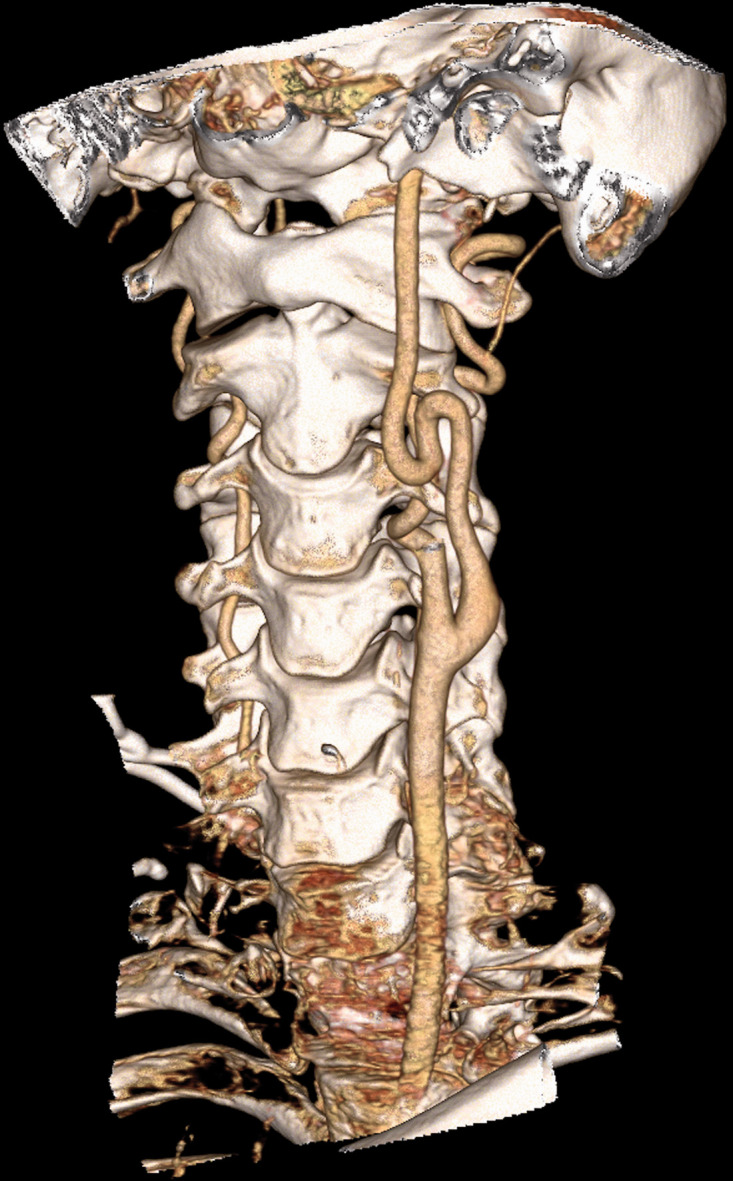
ICA loop in a patient with a history of hyperlipidemia. The 3D reformatted CTA images demonstrate two closely adjacent acute angulations of the left ICA.
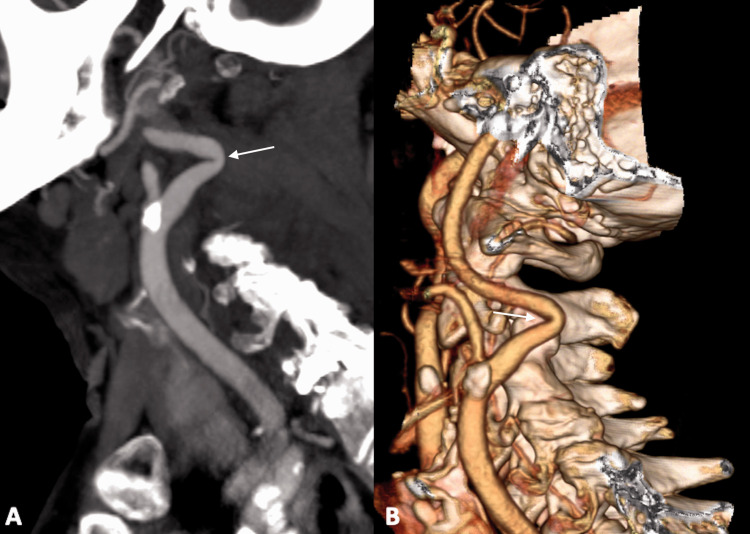
Figure 2.
Example of an ICA kink. Sagittal maximum intensity projection (a) and 3D reformatted (b) CTA images of a patient with a history of atrial fibrillation demonstrate a sharp angle in the mid left ICA (arrows).
Figure 4.
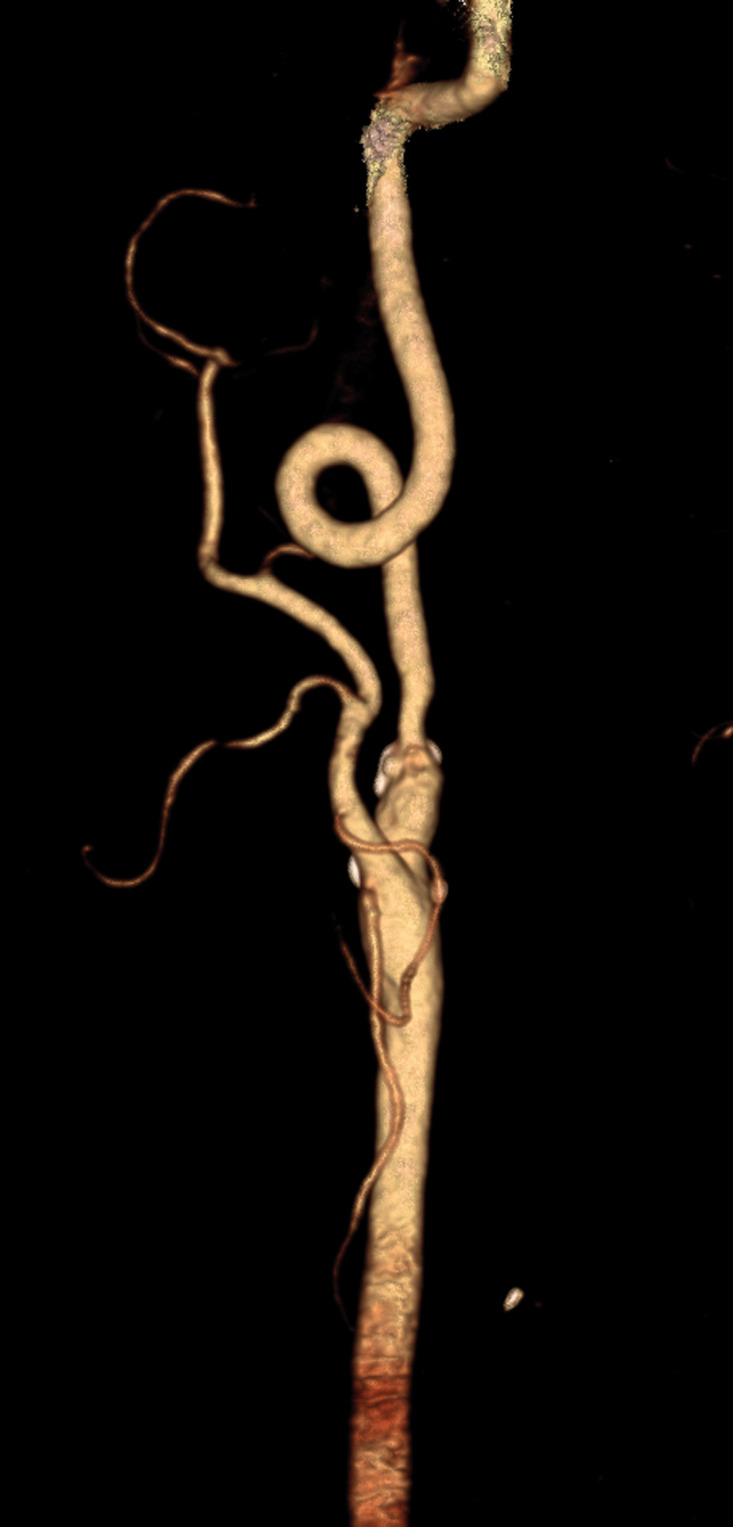
Example of a carotid coil in a patient with a history of diabetes. A 3D reformatted CTA image of the left carotid demonstrates a full 360° turn of the mid cervical ICA. Scattered atherosclerosis is noted, particularly at the ICA origin.
The average ages of patient without and with tortuosity were 68.2 ± 14.7 and 68.4 ± 12.5, respectively. There was no association with age and the presence of tortuosity (p = 0.96). No significant association was noted between gender and the presence or absence or any subtype of tortuosity (p = 0.9624). An association was noted between a retropharyngeal course of the right carotid artery and the presence of any type of carotid tortuosity (p = 0.03), although no such association was noted on the left side (p = 0.64); no association was found between a right or left retrojugular carotid course and the presence of carotid tortuosity (p = 0.31 and p = 0.10, respectively).
Thrombectomy procedures
Distal catheterization was achieved in all patients. No association noted between number of passes and the presence of a kink (p = 0.99), loop (p = 0.78), or coil (p = 0.85); nor was an association noted between the number of passes and the presence of any subtype of tortuosity (p = 0.88). The presence of a kink was associated with lower chance that a procedure would result in successful recanalization (p = 0.02). Neither the presence of a coil (p = 1.00) nor a loop (0.71) was associated with successful recanalization rates, nor was the presence of any subtype of tortuosity (p = 0.11). The median TTC for all patients was 13 min, and the median TTP for all patients was 27 min. There was no association between TTC or TTP and the presence of any subtype of tortuosity (p = 0.16 and p = 0.22, respectively).
Co-morbidities
Of the studied co-morbidities, the most common among the patient cohort was hypertension (n = 92; 76.7%), followed by hyperlipidemia (n = 69; 57.5%), diabetes (n = 31; 25.8%), coronary artery disease (n = 32; 26.7%), congestive heart failure (n = 15; 12.5%), prior stroke (n = 6; 5.0%), and prior TIA (n = 5; 4.2%). Sixty-six (55.0%) were prior smokers, and 16 (13.3%) were current smokers at the time of imaging. Sixty-three (52.5%) were on aspirin, 11 (9.2%) were on a different anti-platelet medication, and two (1.7%) were on an anti-coagulation medication. No significant association was found between the presence of any subtype of carotid tortuosity and any of the above co-morbidities, tobacco use, or medications (p values ranged from 0.13 to 1.00) (Table 1).
Table 1.
Co-morbidities and the presence or absence of any subtype of carotid tortuosity.
| No tortuosity (n = 73) | Kink, loop, or coil (n = 4) | P value | ||
|---|---|---|---|---|
| DM | No | 55 (75.3%) | 34 (72.3%) | p = 0.71 |
| Yes | 18 (24.7%) | 13 (27.7%) | ||
| HTN | No | 15 (20.5%) | 13 (27.7%) | p = 0.37 |
| Yes | 58 (79.5%) | 34 (72.3%) | ||
| HLD | No | 27 (37.0%) | 24 (51.1%) | p = 0.13 |
| Yes | 46 (63.0%) | 23 (48.9%) | ||
| CAD | No | 53 (72.6%) | 35 (74.5%) | p = 0.82 |
| Yes | 20 (27.4%) | 12 (25.5%) | ||
| AF | No | 41 (56.2%) | 23 (48.9%) | p = 0.44 |
| Yes | 32 (43.8%) | 24 (51.1%) | ||
| CHF | No | 64 (87.7%) | 41 (87.2%) | p = 0.94 |
| Yes | 9 (12.3%) | 6 (12.8%) | ||
| Prior stroke | No | 70 (95.9%) | 44 (93.6%) | p = 0.68 |
| Yes | 3 (4.1%) | 3 (6.4%) | ||
| Prior TIA | No | 69 (94.5%) | 46 (97.9%) | p = 0.65 |
| Yes | 4 (5.5%) | 1 (2.1%) | ||
| ASA | No | 32 (43.8%) | 25 (53.2%) | p = 0.32 |
| Yes | 41 (56.2%) | 22 (46.8%) | ||
| Other anti-platelet | No | 66 (90.4%) | 43 (91.5%) | p = 1.00 |
| Yes | 7 (9.6%) | 4 (8.5%) | ||
| Anti-coagulation | No | 72 (98.6%) | 46 (97.9%) | p = 1.00 |
| Yes | 1 (1.4%) | 1 (2.1%) | ||
| History smoking | No | 32 (43.8%) | 22 (46.8%) | p = 0.75 |
| Yes | 41 (56.2%) | 25 (53.2%) | ||
| Current smoker | No | 64 (87.7%) | 40 (85.1%) | p = 0.69 |
| Yes | 9 (12.3%) | 7 (14.9%) |
AF: atrial fibrillation; ASA: aspirin; CAD: coronary artery disease; CHF: congestive heart failure; DM: diabetes mellitus; HLD: hyperlipidemia; HTN: hypertension; TIA: transient ischemic attack.
Discussion
This current study sought to assess the prevalence of ICA tortuosity among patients that underwent endovascular mechanical thrombectomy or aspiration for LVO in AIS. The results indicate that tortuosity is present in approximately 40% of patients presenting for thrombectomy procedures, and that kinks are associated with lower rates of successful recanalization. However, extra-cranial tortuosity is otherwise not associated with any significant degradation of endovascular thrombectomy attempts.
A recent study by Jeong et al.6 assessed the importance of ICA tortuosity and catheter positioning in the setting of AIS treatment. Among patients with tortuous ICAs, successful recanalization was obtained in 90.9% of cases in which distal catheterization was achieved, compared to 70.6% in which the catheter tip was proximally located. However, distal catheterization was achieved in only 11/28 cases with ICA tortuosity. Hence the study by Jeong et al. suggests that ICA morphology may impact an interventionalist’s ability to successfully recanalize occluded vessels. The results of the current study indicate that carotid kinks specifically may impede recanalization attempts, even when distal catheterization is achieved. The reason for this, however, is uncertain; neither the number of pass attempts nor procedure time was affected by the presence of carotid tortuosity.
Regarding the prevalence of carotid tortuosity, the results of similar prior studies have varied, likely due to differences in methodology and/or patient selection. Barbour et al.11 found at least one type of “redundancy” (defined as a kink, loop, or coil) in 22 of 187 (11.8%) of non-dissected arteries, a lower prevalence than seen in the current study. Of the subtypes of redundancy identified by Barbour et al., coils (n = 10) were most common, followed by kinds (n = 9) and loops (n = 3). Pfeiffer et al.,12 in comparison, found kinks in 45.0% and coils in 12.1% of known aberrant ICAs. The current study focused on patients with AIS due to a LVO that underwent endovascular recanalization, thereby focusing on the subset of patients most likely to be encountered by interventionalists most likely to be interested in such a morphologic analysis.
The pathogenesis of ICA tortuosity is somewhat unclear. Leipzig et al.13 dichotomized ICA morphology into undulations (likely congenital and/or developmental) from sharp-angled “kinks” (likely acquired); all types of tortuosity in the current study would fall under the latter definition. Such kinks, opined Leipzig et al., may be secondary to age-related degenerative changes, atherosclerosis, or iatrogenic causes. Other authors have found associations between ICA tortuosity and increased body mass index and increased age.14–16 A histologic examination of kinked, coiled, and tortuous ICAs by La Barbera et al.17 found metaplastic changes of the tunica media of affected vessels, in which loose connective tissue was substituted for muscular and elastic tissue. Furthermore, Pellegrino et al.18 found that although single-sided dolichoarteriopathies of the carotid arteries were sometimes due to atherosclerosis, bilateral disease seemed to be independent of carotid plaques.
Regardless of the pathogenesis of tortuosity, the data from the current study indicate that co-morbidities do not seem to play a role in its prevalence. This includes an analysis of associated cardiovascular and neurovascular disease (e.g. prior stroke), medications, and current or prior tobacco use. In addition, no association was found between the incidence of tortuosity and age. However, it is possible that such an association was not noted because of the lack of pediatric subjects in this cohort; tortuosity is not routinely seen in pediatric patients.
Limitations are present in all studies, and the current study shares those of any retrospective analysis. Also, only specific subtypes of carotid tortuosity were noted; it is possible that other morphologic characteristics of cervical ICAs (such as generalized arterial redundancy) could also impede distal catheterization and may deserve the attention of future research. Common carotid artery tortuosity, likewise, was not assessed, which also could affect catheterization attempts. Finally, the degree to which carotid tortuosity impeded distal catheterization and/or successful recanalization was not explored, although such findings were outside of the scope of this study.
Conclusions
Among patients undergoing endovascular thrombectomy in the setting of AIS, significant tortuosity is present in approximately 40% of patients. Kinks are the most commonly encountered subtype of arterial redundancy, when present, followed by loops and coils. Kinks specifically may portend a lower likelihood of successfully recanalizing a vessel. Tortuosity in general otherwise seems to have little effect on thrombectomy procedures.
Declaration of conflicting interests
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
The authors received no financial support for the research, authorship, and/or publication of this article.
ORCID iDs
John C Benson https://orcid.org/0000-0002-4038-5422
Waleed Brinjikji https://orcid.org/0000-0001-5271-5524
References
- 1.Cairney J. Tortuosity of the cervical segment of the internal carotid artery. J Anat 1924; 59: 87–96. [PMC free article] [PubMed] [Google Scholar]
- 2.Ballotta E, Abbruzzese E, Thiene G, et al. The elongation of the internal carotid artery: early and long-term results of patients having surgery compared with unoperated controls. Ann Vasc Surg 1997; 11: 120–128. [DOI] [PubMed] [Google Scholar]
- 3.Gocmen R, Arsava EM, Oguz KK, et al. Intravenous thrombolysis for acute ischemic stroke in patients with cervicocephalic dolichoarteriopathy. J Stroke Cerebrovasc Dis 2017; 26: 2579–2586. [DOI] [PubMed] [Google Scholar]
- 4.Faggioli G, Ferri M, Gargiulo M, et al. Measurement and impact of proximal and distal tortuosity in carotid stenting procedures. J Vasc Surg 2007; 46: 1119–1124. [DOI] [PubMed] [Google Scholar]
- 5.Chang CK, Huded CP, Nolan BW, et al. Prevalence and clinical significance of stent fracture and deformation following carotid artery stenting. J Vasc Surg 2011; 54: 685–690. [DOI] [PubMed] [Google Scholar]
- 6.Jeong DE, Kim JW, Kim BM, et al. Impact of balloon-guiding catheter location on recanalization in patients with acute stroke treated by mechanical thrombectomy. Am J Neuroradiol 2019; 30: 840–844. [DOI] [PMC free article] [PubMed]
- 7.Snelling BM, Sur S, Shah SS, et al. Unfavorable vascular anatomy is associated with increased revascularization time and worse outcome in anterior circulation thrombectomy. World Neurosurg 2018; 120: e976–e983. [DOI] [PubMed] [Google Scholar]
- 8.Oliviero U, Cocozza M, Picano T, et al. Prevalence of carotid kinking and coiling in a population at risk. Vasc Surg 1997; 31: 43–49. [Google Scholar]
- 9.Sacco S, Totaro R, Baldassarre M, et al. Morphological variations of the internal carotid artery: prevalence, characteristics and association with cerebrovascular disease. Int J Angiol 2007; 16: 59–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Illuminati G, Ricco J-B, Caliò FG, et al. Results in a consecutive series of 83 surgical corrections of symptomatic stenotic kinking of the internal carotid artery. Surgery 2008; 143: 134–139. [DOI] [PubMed] [Google Scholar]
- 11.Barbour PJ, Castaldo JE, Rae-Grant AD, et al. Internal carotid artery redundancy is significantly associated with dissection. Stroke 1994; 25: 1201–1206. [DOI] [PubMed] [Google Scholar]
- 12.Pfeiffer J, Becker C, Ridder GJ. Aberrant extracranial internal carotid arteries: new insights, implications, and demand for a clinical grading system. Head Neck 2016; 38: E687–E693. [DOI] [PubMed] [Google Scholar]
- 13.Leipzig TJ, Dohrmann GJ. The tortuous or kinked carotid artery: pathogenesis and clinical considerations. A historical review. Surg Neurol 1986; 25: 478–486. [DOI] [PubMed] [Google Scholar]
- 14.Wang H-F, Wang D-M, Wang J-J, et al. Extracranial internal carotid artery tortuosity and body mass index. Front Neurol 2017; 8: 508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Choudhry FA, Grantham JT, Rai AT, et al. Vascular geometry of the extracranial carotid arteries: an analysis of length, diameter, and tortuosity. J Neurointerv Surg 2016; 8: 536–540. [DOI] [PubMed] [Google Scholar]
- 16.Kamenskiy AV, Pipinos II, Carson JS, et al. Age and disease-related geometric and structural remodeling of the carotid artery. J Vasc Surg 2015; 62: 1521–1528. [DOI] [PubMed] [Google Scholar]
- 17.La Barbera G, La Marca G, Martino A, et al. Kinking, coiling, and tortuosity of extracranial internal carotid artery: is it the effect of a metaplasia? Surg Radiol Anat 2006; 28: 573–580. [DOI] [PubMed] [Google Scholar]
- 18.Pellegrino L, Prencipe G, Ferrara V, et al. [Bilateral and monolateral dolichoarteriopathies (kinking, coiling, tortuosity) of the carotid arteries and atherosclerotic disease. An ultrasonographic study]. Minerva Cardioangiol 2002; 50: 15–20. [PubMed] [Google Scholar]