Abstract
We used electronic medical record (EMR) data in the National Patient‐Centered Clinical Research Network (PCORnet) to characterize “real‐world” prescription patterns of Type 2 diabetes (T2D) medications. We identified a retrospective cohort of 613,203 adult patients with T2D from 33 datamarts (median patient number: 12,711) from 2012 through 2017 using a validated computable phenotype. We characterized outpatient T2D prescriptions for each patient in the 90 days before and after cohort entry, as well as demographics, comorbidities, non‐T2D prescriptions, and clinical and laboratory variables in the 730 days prior to cohort entry. Approximately half of the individuals in the cohort were females and 20% Black. Hypertension (60.3%) and hyperlipidemia (50.5%) were highly prevalent. Most patients were prescribed either a single T2D drug class (42.2%) or had no evidence of a T2D prescription in the EMR (42.4%). A smaller percentage was prescribed multiple T2D drug types (15.4%). Among patients prescribed a single T2D drug type, metformin was the most common (42.6%), followed by insulin (18.2%) and sulfonylureas (13.9%). Newer classes represented approximately 13% of single T2D drug type prescriptions (dipeptidyl peptidase‐4 inhibitors [6.6%], glucagon‐like peptide‐1 receptor agonists [2.5%], thiazolidinediones [2.0%], and sodium‐glucose cotransporter‐2 inhibitors [1.6%]). Among patients prescribed multiple T2D drug types, the most common combination was metformin and sulfonylureas (63.5%). Metformin‐based regimens were highly prevalent in PCORnet's T2D population, whereas newer agents were prescribed less frequently. PCORnet is a novel source for the potential conduct of observational studies among patients with T2D.
Keywords: distributed research network, electronic health records, PCORI, pharmacoepidemiology, Type 2 diabetes
1. INTRODUCTION
Electronic medical record (EMR) data sources are increasingly recognized for their potential to help answer important clinical questions and provide valuable information on a variety of patient outcomes. 1 Since EMR data have already been collected for clinical reasons, EMR data can be leveraged to provide large study populations 2 , 3 , 4 with longitudinal follow‐up. 2 Moreover, the sizeable and heterogeneous sample of patients in EMR databases can be used to detect rare events or common events among certain high‐risk groups. 5 Thus, EMR data may serve as valuable sources of long‐term outcomes data in large, “real‐world” populations. 2 , 3 , 4 , 6 , 7 EMR data sources can also be leveraged to evaluate the cardiovascular safety of drugs used to treat Type 2 diabetes (T2D), which has been a high‐priority research area since 2008 when concerns arose about the cardiovascular safety of the T2D drug rosiglitazone. 8 Some multi‐institutional clinical T2D cohorts have been established, including the Veterans Health Administration, 3 , 9 Northern California Kaiser Permanente healthcare system, 10 , 11 , 12 and healthcare registries in Nordic countries. 13
The National Patient‐Centered Clinical Research Network (PCORnet) is a novel source of EMR data. PCORnet is a national, distributed research network of interconnected healthcare data systems established by the Patient‐Centered Outcomes Research Institute (PCORI) in 2014 to facilitate research across multiple sites. 14 PCORnet's demographic diversity (in terms of gender, racial, and geographic diversity) offers advantages over some existing T2D datasets. In PCORnet, EMR data across multiple participating sites are organized into a common data model (CDM). The CDM facilitates the construction of standardized research datasets across multiple institutions, allowing for rapid responses to queries and for the potential to answer clinical questions in a large population across many healthcare systems. Our aim was to assemble and describe a retrospective cohort of patients with T2D according to the prescribing of specific T2D medications, the availability of clinical and laboratory variables, and the prevalence of comorbidities and non‐T2D medication prescriptions. We sought to clarify PCORnet's potential as a resource to inform future efforts to determine the cardiovascular outcomes associated with T2D drugs.
2. MATERIALS AND METHODS
2.1. Data source and study population
We used a previously validated computable phenotype (positive predictive value: 96.2% (CI 95.1%‐97.0%) to assemble a retrospective cohort of patients with T2D using data from PCORnet. 15 PCORnet is composed of multiple research networks encompassing one or multiple datamarts (a collection of data that can be queried and return output) across the United States. The EMR data from participating PCORnet networks are organized into the CDM and include clinical information, demographics, diagnosis and procedure codes, laboratory values, and prescription information. 14 , 16 To ensure datamart autonomy and maximize patient privacy, each datamart conducted secure data analysis locally behind its own firewall and maintained its own individual‐level data such that only summary statistics from each datamart were available.
We queried 44 datamarts from across the United States to create a cohort of adult patients (≥18 years of age) with T2D and a minimum of 1 healthcare encounter (inpatient, outpatient, or emergency department visits) in each of the 2 years prior to the date of cohort entry (t0). The t0 was the earliest date that a patient fulfilled one of three previously validated computable phenotypes (CP) for T2D between 1 January 2012 and 31 December 2017 15 : (CP1) a T2D diagnosis code (ICD9 or ICD10) as an inpatient or outpatient, and an outpatient prescription for a diabetes medication (Table S1) within 90 days after the first instance of a T2D diagnosis code, (CP2) T2D diagnosis code and Hemoglobin A1c (HbA1c) level >6.5% within 90 days before or after the diagnosis date, or (CP3) outpatient diabetes medication prescription within 90 days before or after a HbA1c level >6.5%. Patients with evidence of gestational diabetes, Type 1 diabetes, prediabetes, or a positive pregnancy test within 90 days of t0 were excluded.
2.2. T2D medications
The primary outcome was outpatient T2D medication prescriptions, organized by pharmacologic class (Table S1), in the 90 days before and 90 days after t0. We sought to capture a “snapshot” of the active outpatient prescriptions at the initial time a patient was identified by the computable phenotype as having T2D (t0), and therefore we designed the medication query in the following manner. First, we limited the time window to capture T2D prescriptions to a relatively narrow baseline period (t0 ± 90 days) to purposely identify active T2D medication prescriptions at the time the patient was identified in the cohort (t0). Second, a medication would only be captured and reported as an “outpatient T2D prescription” if an electronic prescription linked to an outpatient encounter was submitted during the timeframe of t0 ± 90 days. Medications that were simply listed in the medication list section in the progress note of the EMR were not captured as active prescriptions.
We generated a comprehensive list of FDA‐approved T2D medications, organized by T2D pharmacologic class (or “drug type”) (eg, sulfonylureas, insulin, glucagon‐like peptide‐1 receptor agonists, etc), using standardized nomenclature codes for individual drugs (RxNorm codes). The RxNorm code list was used to query the CDM for evidence of specific T2D medication prescriptions linked to outpatient encounters. The components of each drug were mapped to RxNorm codes for the individual drug such that the use of combination drugs was identified based on the presence of RxNorm codes for more than one pharmacologic class (Table S1). Each datamart then classified individual patients with T2D into mutually exclusive categories of T2D pharmacologic class.
2.3. Patient characteristics
For each patient, demographic and clinical characteristics were collected in the 730 days preceding t0, including age, sex, race (White, Black, Other), calendar year of cohort entry, smoking status, and specific comorbidities (Table S2). We also identified the most recently available information for specific clinical variables, including body mass index (BMI), blood pressure, HbA1c, low‐density lipoprotein (LDL) levels, and creatinine (which was used to calculate estimated glomerular filtration rate (eGFR) using the Chronic Kidney Disease Epidemiology Collaboration (CKD‐EPI) equation). 17 Evidence of at least one prescription for selected non‐T2D medications in 730 days prior to t0 were also characterized (Table S3). In addition, healthcare utilization (hospitalizations and outpatient visits) are reported in the 365 days prior to t0.
2.4. Statistical analysis
Each datamart reported the total number of patients with T2D within each mutually exclusive category of pharmacologic class, including those who met the computable phenotype T2D without evidence of a prescribed T2D medication. For each mutually exclusive group, the datamart characterized the patients by race and sex, the prevalence of specific comorbidities, and prescriptions of selected non‐T2D medications. Furthermore, for each pharmacologic class, each datamart characterized the availability, median, and interquartile range of the individual physiological and laboratory values for the population. As a result, only proportions and summary statistics for each pharmacologic class from each datamart were available to characterize the total PCORnet population. Therefore, we described continuous variables (age, BMI, blood pressure, and laboratory values) using weighted median values based on the denominator of the specific drug user population at each datamart such that more highly prevalent T2D drug user populations at datamarts with a greater number of patients received higher weights. Categorical variables (including prevalence of comorbidities) are reported as percentages.
3. RESULTS
3.1. Cohort assembly
We queried 44 datamarts, and 33 (75%) datamarts responded with the necessary results within the required timeframe. Across the 33 datamarts, we identified 613,203 individuals who met criteria for the T2D cohort (Figure 1 ). There was a median of 12,711 patients per datamart, and a range of 122‐79,519 patients among individual datamarts.
Figure 1.
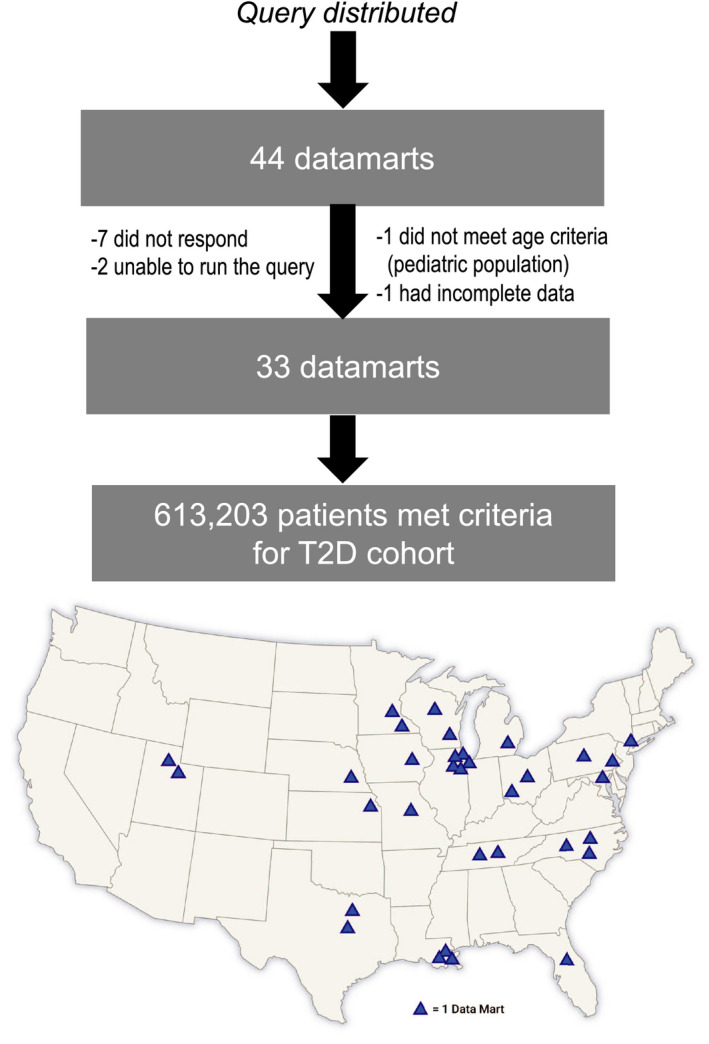
Schematic of creation of T2D cohort in PCORnet. The process of creating the T2D cohort in PCORnet is depicted. T2D, Type 2 diabetes; PCORnet, National Patient‐Centered Clinical Research Network
3.2. Patient characteristics
Patient demographics, comorbidities, and prescription of non‐T2D medications were characterized in the 730 days prior to cohort entry (Table 1 ). Approximately half of the individuals in the T2D cohort were females, and 20% were Black. Prevalence of hypertension was 60.3% and of hyperlipidemia was 50.5%. Atherosclerotic cardiovascular disease (ASCVD) was highly prevalent; 16.5% (N = 100 967) had coronary artery disease, 2.2% (N = 13 698) had stroke and transient ischemic attacks, 0.2% (N = 1426) had carotid artery disease, and 4.2% (N = 25 986) had peripheral artery disease. The prevalence of a prescription for angiotensin‐converting enzyme ACE inhibitors (ACEi) or angiotensin‐receptor blockers (ARB) was 27.4%.
Table 1.
Characteristics of patients identified with Type 2 Diabetes in PCORnet, 2012‐2017
| Total population | N = 613 203 | Any T2D Prescription | N = 353 331 | No T2D Prescription | N = 259 872 | |
|---|---|---|---|---|---|---|
| Age (y) – Median (25th percentile, 75th percentile) a | 64 | (47, 71) | 62 | (45, 69) | 64 | (47, 71) |
| Demographics | N | (%) | N | (%) | N | (%) |
| Female | 305 138 | (49.8) | 178 367 | (50.5) | 126 771 | (48.8) |
| Race | ||||||
| White | 397 614 | (64.8) | 231 105 | (65.4) | 166 509 | (64.1) |
| Black | 119 954 | (19.6) | 73 198 | (20.7) | 46 756 | (18.0) |
| Other | 64 993 | (10.6) | 32 387 | (9.2) | 32 606 | (12.5) |
| Missing | 31 159 | (5.1) | 17 166 | (4.9) | 13 993 | (5.4) |
| Hispanic/ Latino | 56 024 | (9.1) | 33 589 | (9.5) | 22 435 | (8.6) |
| Comorbidities | N | (%) | N | (%) | N | (%) |
| Atherosclerotic cardiovascular disease | ||||||
| Carotid artery disease | 1426 | (0.2) | 849 | (0.2) | 577 | (0.2) |
| Coronary artery disease | 100 967 | (16.5) | 49 297 | (14.0) | 51 670 | (19.9) |
| Peripheral Artery disease | 25 986 | (4.2) | 12 250 | (3.5) | 13 736 | (5.3) |
| Stroke/Transient ischemic attack | 13 698 | (2.2) | 7038 | (2.0) | 6660 | (2.6) |
| Cancer | 43 256 | (7.1) | 23 516 | (6.7) | 19 740 | (7.6) |
| Cardiac arrhythmia/ Atrial fibrillation | 65 603 | (10.7) | 30 128 | (8.5) | 35 475 | (13.7) |
| Cardiac valve disease | 20 962 | (3.4) | 9538 | (2.7) | 11 424 | (4.4) |
| Depression | 48 146 | (7.9) | 26 897 | (7.6) | 21 249 | (8.2) |
| Heart failure | 50 402 | (8.2) | 21 551 | (6.1) | 28 851 | (11.1) |
| Hyperlipidemia | 309 666 | (50.5) | 182 772 | (51.7) | 126 894 | (48.8) |
| Hypertension | 369 992 | (60.3) | 210 949 | (59.7) | 159 043 | (61.2) |
| Liver disease | 20 494 | (3.3) | 10 654 | (3.0) | 9840 | (3.8) |
| Parkinson's | 8971 | (1.5) | 5486 | (1.6) | 3485 | (1.3) |
| Pulmonary hypertension/ Embolism | 17 292 | (2.8) | 7548 | (2.1) | 9744 | (3.7) |
| Retinopathy | 15 622 | (2.5) | 8786 | (2.5) | 6836 | (2.6) |
| Serious mental illness | 29 044 | (4.7) | 15 599 | (4.4) | 13 445 | (5.2) |
| Smoking‐related illness/Chronic obstructive pulmonary disease/Oxygen use | 62 111 | (10.1) | 31 403 | (8.9) | 30 708 | (11.8) |
| Outpatient antihypertensive prescriptions | N | (%) | N | (%) | N | (%) |
| Angiotensin‐converting enzyme‐inhibitors/ Angiotensin‐receptor blockers | 167 728 | (27.4) | 134 869 | (38.2) | 32 589 | (12.6) |
| Beta‐blockers | 92 868 | (15.1) | 70 494 | (20.0) | 22 374 | (8.6) |
| Calcium channel Blockers | 72 472 | (11.8) | 56 463 | (16.0) | 16 009 | (6.2) |
| Loop diuretics | 41,636 | (6.8) | 29 557 | (8.4) | 12 079 | (4.6) |
| Nitrates | 10 202 | (1.7) | 7226 | (2.0) | 2976 | (1.1) |
| Non‐selective alpha blockers | 7129 | (1.2) | 5529 | (1.6) | 1600 | (0.6) |
| Peripheral vasodilators | 1976 | (0.3) | 1561 | (0.4) | 415 | (0.2) |
| Thiazide diuretics | 19 270 | (3.1) | 14 304 | (4.0) | 4966 | (1.9) |
| Antihypertensives ‐ other | 15 786 | (2.6) | 11 230 | (3.2) | 4556 | (1.8) |
| Other outpatient non‐T2D prescriptions | N | (%) | N | (%) | N | (%) |
| Antiarrhythmics/ digoxin and inotropes | 9523 | (1.6) | 6836 | (1.9) | 2687 | (1.0) |
| Anticoagulants and platelet inhibitors | 31 357 | (5.1) | 22 457 | (6.4) | 8900 | (3.4) |
| Antipsychotics | 6981 | (1.1) | 5516 | (1.6) | 1465 | (0.6) |
| Acetylsalicylic acid | 55 495 | (9.1) | 43 876 | (12.4) | 11 619 | (4.5) |
| Bone Resorption Inhibitors | 3153 | (0.5) | 2447 | (0.7) | 706 | (0.3) |
| Lipid lowering drugs | 111 993 | (18.3) | 89 854 | (25.4) | 22 139 | (8.5) |
| Oral glucocorticoids | 49 731 | (8.1) | 36 914 | (10.4) | 12 817 | (4.9) |
| Average values for selected clinical variables | Median a | (25th, 75th %) a | Median a | (25th, 75th %) a | Median a | (25th, 75th %) a |
| Body mass index (kg/m2) | 32.0 | (23, 41) | 32.5 | (23.5, 41.5) | 32.0 | (23.41) |
| Blood pressure – systolic (mmHg) | 130 | (108, 152) | 130 | (109, 151) | 130 | (107, 153) |
| Blood pressure – diastolic (mmHg) | 75 | (61, 89) | 76 | (62, 90) | 74 | (59,89) |
| Hemoglobin A1c (%) | 7.0 | (5.4, 8.6) | 7.2 | (5.7, 8.7) | 7.0 | (5.4, 8.6) |
| Low‐density lipoprotein cholesterol (mg/dl) | 87.5 | (42.5, 132.5) | 86.0 | (41.0, 131.0) | 89.0 | (43.0, 135.0) |
| Estimated glomerular filtration rate (eGFR) (ml/min/1.72 m2) | 75.0 | (38, 112) | 80.0 | (49.0, 121.0) | 72.0 | (34.0, 110.0) |
| Healthcare utilization in the past year | ||||||
| Hospitalization – N (%) | 87,147 | (14.2) | 39,602 | (11.2) | 47,545 | (18.3) |
| Outpatient visits – Median (25th %, 75th %) a | 5 | (0, 14) b | 6 | (0, 15) b | 5 | (0, 14) b |
Abbreviation: T2D, Type 2 diabetes.
Note: Demographics, comorbidities, non‐T2D prescriptions, and clinical variables are reported during the 730 days prior to t0, the earliest date that patient met criteria for the T2D cohort.
Median values were calculated as a weighted median of the median values reported from each drug‐type user population (ie metformin only, insulin only, etc) at each PCORnet site, while 25th and 75th percentile values calculated as estimated percentages based upon the weighted median and weighted IQR values reported from each drug‐type user population.
25th percentile values estimated to be less than 0 were recorded as 0 outpatient visits inTable 2.
3.3. Outpatient T2D drug prescriptions
Outpatient T2D prescriptions (based on submission of electronic prescriptions linked to an outpatient encounter) were captured for each patient during the 90 days before and 90 days after t0 (the earliest date that the patient fulfilled any of the 3 computable phenotypes for the T2D cohort). During this period, 42.4% of patients were prescribed no outpatient T2D medications, 42.2% were prescribed a single T2D drug type, and 15.4% were prescribed 2 or more T2D drug types (Figure 2 ).
Figure 2.
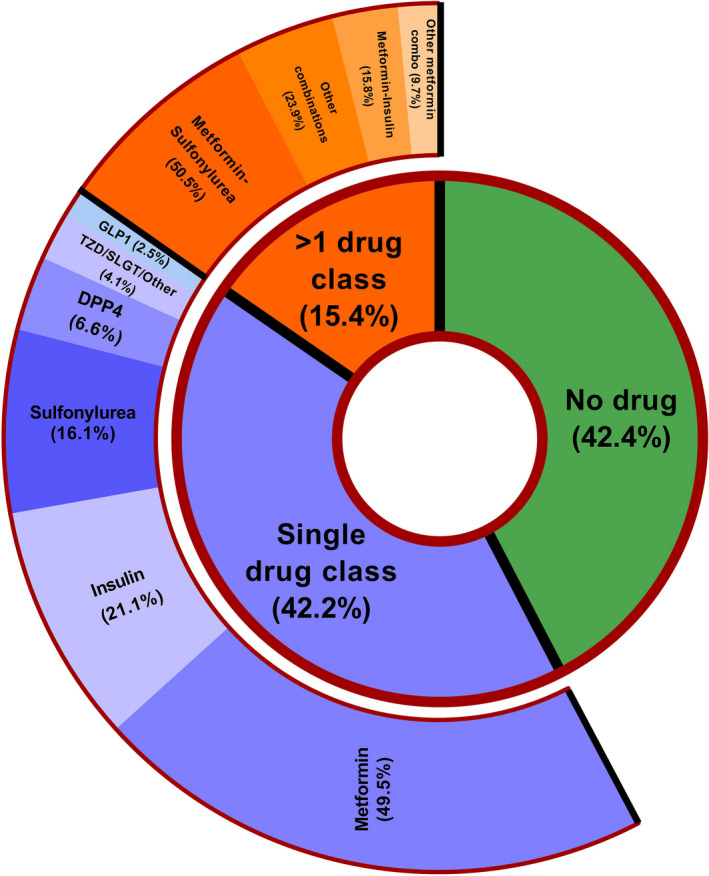
Outpatient Prescriptions of T2D medications in PCORnet (2012‐2017). The prevalence of outpatient prescriptions of T2D medications in the overall cohort of patients with T2D in PCORnet is presented. Data regarding outpatient T2D prescriptions were collected from the prescribing fields of the electronic medical record for each patient during the 90 days before and 90 days after t0 (the earliest date that the patient fulfilled any of the three computable phenotypes for the T2D cohort). T2D, Type 2 diabetes; PCORnet, National Patient‐Centered Clinical Research Network; DPP4, Dipeptidyl peptidase‐4 inhibitors; GLP‐1, glucagon‐like peptide‐1 receptor agonists (2.5%); TZD, thiazolidinediones; SGLT‐2, sodium‐glucose cotransporter‐2
Among patients prescribed a single outpatient T2D drug type, metformin was the most common (constituting nearly 50%), followed by insulin (21%) and sulfonylureas (16%). Newer drug classes (dipeptidyl peptidase‐4 inhibitors [DPP4], glucagon‐like peptide‐1 [GLP‐1] receptor agonists, thiazolidinediones, and sodium‐glucose cotransporter‐2 [SGLT‐2] inhibitors) represented approximately 13% of single drug type regimens in PCORnet. Among patients prescribed multiple classes of T2D agents, the most common combination regimen was metformin and sulfonylureas (approximately 50%), followed by metformin and insulin (16%).
The finding that 42% of the T2D cohort had no evidence of an active outpatient T2D prescription is due, in part, to the specified timeframe and the structure of the query which was designed to capture a “snapshot” of the active outpatient T2D prescriptions at the first instance that a patient met any of the criteria for the T2D cohort (t0). For instance, a patient may have qualified for the T2D cohort at t0 based on the criteria of a diagnosis code and laboratory value (CP3). If an outpatient prescription for a T2D medication was not written during the 90 days before or after this qualifying date, that patient would have been classified as having no outpatient T2D prescriptions even if a T2D medication was listed on EMR medication list or if a T2D prescription was written after 90 days. To address the latter issue, we conducted an exploratory analysis examining patients’ T2D drug regimens in the 12 months following t0. Over half of those individuals prescribed a particular T2D regimen at t0 had a prescription for the same regimen in the 12 months following t0 (Table 2 ). Moreover, all of the patients classified as having no outpatient T2D prescriptions at t0 were found to have a prescription for a T2D drug in the 12 months following t0.
Table 2.
Characteristics among patients with Type 2 diabetes prescribed the most common antidiabetic drug classes in PCORnet, 2012‐2017
| Metformin only | Insulin only | Metformin‐Sulfonylurea | Sulfonylurea only | DPP4 only | Metformin‐Insulin | |
|---|---|---|---|---|---|---|
| Number of patients (N) | 128 248 | 54 608 | 47 645 | 41 787 | 17 060 | 14 950 |
| Age (y) – Median (25th percentile, 75th percentile) | 62 (45, 79) | 64 (47, 81) | 61 (45, 77) | 68 (50, 86) | 65 (48, 82) | 59 (43, 75) |
| % | % | % | % | % | % | |
| Drug regimen the same within 12 months after index date a | 63.4 | 71.9 | 58.7 | 66.8 | 61.9 | 57.4 |
| T2D prescription in the 90 to 720 days prior to index date | ||||||
| Metformin | 36.3 | 14.8 | 46.6 | 22.1 | 20.7 | 41.9 |
| Insulin | 3.2 | 34.1 | 7.1 | 3.8 | 5.4 | 41.8 |
| Sulfonylurea | 5.5 | 9.8 | 42.1 | 33.6 | 14.1 | 9.5 |
| DPP4 | 1.9 | 4.3 | 7.4 | 5.2 | 23.3 | 4.1 |
| GLP1 | 0.8 | 2.5 | 2.3 | 1.2 | 1.3 | 4.7 |
| Demographics | ||||||
| Female | 53.5 | 49.6 | 45.5 | 48.8 | 50.4 | 51 |
| Race | 64.1 | 66 | 65 | 68.6 | 63.6 | 62.8 |
| White | 21.5 | 22.9 | 19.3 | 18.9 | 20.1 | 23.8 |
| Black | 9.7 | 7.1 | 10.7 | 8.1 | 9.8 | 8.3 |
| Other | 4.7 | 3.9 | 5.0 | 4.4 | 6.8 | 5.3 |
| Missing | 9.3 | 8.7 | 10.2 | 8.8 | 11.7 | 10.6 |
| Hispanic/ Latino | 53.5 | 49.6 | 45.5 | 48.8 | 50.4 | 51.0 |
| Comorbidities | ||||||
| Atherosclerotic cardiovascular disease | ||||||
| Carotid artery disease | 0.1 | 0.3 | 0.2 | 0.3 | 0.2 | 0.4 |
| Coronary artery disease | 10.9 | 23.2 | 10 | 17.3 | 15.5 | 12.3 |
| Peripheral artery disease | 2.3 | 7.1 | 2.0 | 4.2 | 3.8 | 3.0 |
| Stroke/Transient ischemic attack | 1.6 | 3.1 | 1.3 | 2.4 | 2.0 | 2.0 |
| Cancer | 6.1 | 9.1 | 4.8 | 8.2 | 7.2 | 5.5 |
| Cardiac Arrhythmia/ Atrial fibrillation | 6.8 | 14.3 | 5.2 | 11.7 | 9.8 | 6.2 |
| Cardiac Valve Disease | 2.0 | 4.6 | 1.6 | 3.9 | 2.9 | 2.0 |
| Depression | 7.6 | 10.5 | 5.6 | 7.4 | 6.7 | 8.1 |
| Heart failure | 3.6 | 13.9 | 2.9 | 8.4 | 6.9 | 5.0 |
| Hyperlipidemia | 49.6 | 53 | 52.2 | 55.2 | 54 | 47.6 |
| Hypertension | 57.7 | 64.3 | 57.9 | 64.8 | 60.7 | 55.9 |
| Liver disease | 2.4 | 5.3 | 2.0 | 2.9 | 2.8 | 2.9 |
| Parkinson's | 1.3 | 2.1 | 1.0 | 1.5 | 1.4 | 1.8 |
| Pulmonary hypertension/ Embolism | 1.5 | 4.8 | 0.9 | 2.2 | 2.1 | 2.0 |
| Retinopathy | 1.2 | 6.1 | 1.6 | 2.2 | 2.1 | 3.6 |
| Serious mental illness | 4.2 | 6.2 | 2.9 | 4.7 | 4.3 | 4.7 |
| Smoking‐related illness/Chronic obstructive pulmonary disease/Oxygen use | 8.7 | 12.8 | 5.9 | 9.6 | 8.5 | 8.8 |
| Outpatient antihypertensive prescriptions | ||||||
| Angiotensin‐converting enzyme‐inhibitors/Angiotensin‐receptor blockers | 37.8 | 34.4 | 43.7 | 37.6 | 36 | 42.1 |
| Beta‐blockers | 18.5 | 23.9 | 18.9 | 22.8 | 18.6 | 20.3 |
| Calcium channel blockers | 15.3 | 17.3 | 15.3 | 17.7 | 16.6 | 15.5 |
| Loop diuretics | 5.7 | 15.5 | 5.5 | 11 | 8.4 | 8.2 |
| Nitrates | 1.3 | 3.8 | 1.3 | 2.7 | 2.0 | 2.0 |
| Non‐selective alpha blockers | 1.3 | 1.7 | 1.4 | 1.9 | 1.6 | 1.3 |
| Peripheral vasodilators | 0.2 | 0.6 | 0.3 | 0.4 | 0.5 | 0.6 |
| Thiazide diuretics | 3.3 | 6.3 | 3.0 | 4.6 | 3.8 | 3.9 |
| Antihypertensives ‐ other | 2.3 | 5.8 | 2.1 | 3.9 | 3.3 | 2.8 |
| Other outpatient non‐T2D prescriptions | ||||||
| Antiarrhythmics/ Digoxin and inotropes | 1.5 | 2.5 | 1.5 | 2.5 | 2.2 | 1.6 |
| Anticoagulants and platelet inhibitors | 5.2 | 9.7 | 5.0 | 7.8 | 6.3 | 6.6 |
| Antipsychotics | 1.7 | 1.7 | 1.1 | 1.1 | 1.4 | 2.2 |
| Acetylsalicylic acid | 11.7 | 13.7 | 12.8 | 11.9 | 11.6 | 15.1 |
| Bone resorption inhibitors | 0.5 | 0.6 | 0.5 | 0.8 | 0.9 | 0.5 |
| Lipid lowering drugs | 24.9 | 24.0 | 27.8 | 25.3 | 24.7 | 27.7 |
| Oral glucocorticoids | 11.3 | 11 | 8.1 | 11.2 | 10.4 | 9.0 |
| Healthcare utilization in the past year | ||||||
| Hospitalization‐ N(%) | 8.9 | 20.9 | 7.2 | 12.2 | 10.7 | 11.9 |
| Emergency department visits – Median (25th percentile, 75th percentile) b | 0 (0, 0) | 0 (0, 0) | 0 (0, 0) | 0 (0, 0) | 0 (0, 0) | 0 (0, 0) |
| Outpatient visits – Median (25th percentile, 75th percentile) b , c | 6 (0, 14) | 8 (0, 21) | 5 (0, 13) | 7 (0, 17) | 6 (0, 15) | 7 (0, 17) |
Abbreviation: T2D, Type 2 diabetes.
Note: Comobordities and non‐T2D prescriptions are reported during the 720 days prior to t0, the earliest date that patient met criteria for the T2D cohort.
Prescribing data was examined after t0 to determine if the patient remained on the same regimen in the 365 days following t0 (t0 + 365 days).
Median values calculated as a weighted median of the median values reported from each drug‐type user population (ie metformin only, insulin only, etc) at each PCORnet site, while 25th and 75th percentile values calculated as estimated percentages based upon the weighted median and weighted IQR values reported from each drug‐type user population.
25th percentile values estimated to be less than 0 were recorded as 0 outpatient visits inTable 2.
3.4. Availability of electronic medical record clinical variables
The availability of clinical and laboratory data varied by variable type, across datamarts, and between groups with different prescribed drug regimens (Table 3 ). The datapoint with the highest availability was blood pressure (84.5% of patients had at least one reported value), followed by BMI (78.9%), eGFR (51.5%), HbA1c (54.0%), and cholesterol (39.6%). The availability of clinical and laboratory information varied across the 33 datamarts. The maximum percentage of patients with HbA1c, cholesterol, and eGFR values at a single datamart were 80.3%, 68.1%, and 82.9%, respectively.
Table 3.
Values and availability of selected clinical and laboratory measurements of patients with Type 2 diabetes in PCORnet
| N | Systolic/Diastolic blood pressure (mmHg) | Body mass index (kg/m2) | Hemoglobin A1c (%) | LDL a Cholesterol (mg/dl) | eGFR b (ml/min/1.73 m2) | |
|---|---|---|---|---|---|---|
| Median values (25th, 75th %) c , d | ||||||
| No T2D prescription | 259,872 | 130 (107, 153)/ 74 (59, 89) | 32 (23, 41) | 7.0 (5.4, 8.6) | 89 (43, 135) | 72 (34, 110) |
| Metformin only | 128,248 | 129 (109, 149)/ 77 (64, 90) | 32 (23, 41) | 6.8 (5.6, 8.0) | 90 (44, 136) | 84 (55, 113) |
| Insulin only | 54,608 | 130 (106, 154)/ 73 (58, 88) | 33 (23, 43) | 7.9 (5.7, 10.1) | 83 (36, 130) | 67 (22, 112) |
| Sulfonylurea only | 41,787 | 130 (109, 151)/ 74 (60, 88) | 32 (23, 41) | 7.2 (5.7, 8.7) | 83 (40, 126) | 71 (32, 110) |
| DPP4 only | 17,060 | 129.5 (108.5, 150.5)/ 75 (62, 88) | 32 (23, 41) | 7.2 (5.7, 8.7) | 82 (39, 125) | 73 (35.5, 110.5) |
| Met‐Sulfonylurea | 47,645 | 130 (110, 150)/ 76 (63, 89) | 33 (24, 42) | 7.6 (5.7, 9.5) | 84 (41, 127) | 85 (55.5, 114.5) |
| Metformin‐insulin | 14,950 | 130 (108, 152)/ 76 (62, 90) | 34 (24, 44) | 8.4 (5.7, 11) | 87 (42, 132) | 86 (56, 116) |
| Data Site | N | (% available) e | (% available) | (% available) | (% available) | (% available) |
| Overall | 613,203 | 84.5 | 78.9 | 54.0 | 39.6 | 61.5 |
| 1 | 19,808 | 79.2 | 67.3 | 33.0 | 39.9 | 0.0 |
| 2 | 3,974 | 98.3 | 96.5 | 40.1 | 30.9 | 0.0 |
| 3 | 10,106 | 87.9 | 46.6 | 48.3 | 43.4 | 70.8 |
| 4 | 15,678 | 95.3 | 87.4 | 65.1 | 57.2 | 78.8 |
| 5 | 12,711 | 89.8 | 83.3 | 33.0 | 38.4 | 0.0 |
| 6 | 50,036 | 84.1 | 79.0 | 36.2 | 36.0 | 62.8 |
| 7 | 32,842 | 92.4 | 82.9 | 28.6 | 23.0 | 30.1 |
| 8 | 35,523 | 87.6 | 71.5 | 67.9 | 56.0 | 74.0 |
| 9 | 23,777 | 90.9 | 85.0 | 54.9 | 45.8 | 75.3 |
| 10 | 13,974 | 92.7 | 72.3 | 62.1 | 46.0 | 74.2 |
| 11 | 3,158 | 48.4 | 18.8 | 34.2 | 16.3 | 80.1 |
| 12 | 13,600 | 81.7 | 79.3 | 58.1 | 46.6 | 68.7 |
| 13 | 39,062 | 96.6 | 68.7 | 79.8 | 65.4 | 75.5 |
| 14 | 35,953 | 36.9 | 72.2 | 45.4 | 38.2 | 61.0 |
| 15 | 20,489 | 74.3 | 66.9 | 1.8 | 68.1 | 82.9 |
| 16 | 10,768 | 97.6 | 75.1 | 79.1 | 60.5 | 76.4 |
| 17 | 5,312 | 0.0 | 68.1 | 57.8 | 41.3 | 66.2 |
| 18 | 8,647 | 95.4 | 94.2 | 49.5 | 51.0 | 67.1 |
| 19 | 4,421 | 92.2 | 82.9 | 48.9 | 38.6 | 68.2 |
| 20 | 7,729 | 98.9 | 93.8 | 74.2 | 49.6 | 78.6 |
| 21 | 6,196 | 87.3 | 86.8 | 53.5 | 46.3 | 69.3 |
| 22 | 8,807 | 93.7 | 88.2 | 66.0 | 47.7 | 67.8 |
| 23 | 79,519 | 94.7 | 89.3 | 75.2 | 8.7 | 78.4 |
| 24 | 635 | 98.1 | 98.3 | 3.1 | 3.1 | 6.1 |
| 25 | 28,632 | 90.1 | 89.9 | 55.3 | 48.7 | 65.8 |
| 26 | 2,108 | 90.0 | 92.8 | 51.6 | 50.7 | 75.2 |
| 27 | 122 | 75.4 | 73.8 | 80.3 | 63.9 | 0.0 |
| 28 | 64,121 | 90.8 | 73.4 | 56.1 | 49.5 | 69.2 |
| 29 | 9,044 | 95.6 | 95.6 | 73.2 | 34.7 | 0.0 |
| 30 | 18,394 | 93.5 | 84.5 | 70.0 | 16.6 | 75.7 |
| 31 | 14,962 | 23.2 | 80.6 | 16.6 | 25.0 | 0.0 |
| 32 | 8,244 | 80.4 | 77.0 | 57.3 | 37.3 | 0.0 |
| 33 | 4,851 | 93.3 | 89.9 | 23.4 | 1.4 | 76.9 |
Abbreviation: T2D, Type 2 diabetes.
LDL: Low‐density lipoprotein.
eGFR: estimated glomerular filtration rate.
Calculated as a weighted median of the median values reported from each drug‐type user population (ie metformin only, insulin only, etc) at each PCORnet site.
The 25th and 75th percentiles were calculated using the interquartile range (IQR) calculated using the weighted median of reported IQRs from each drug‐type user population at each PCORnet site.
The percentage of patients at each participating PCORnet datamart with at least one baseline value for selected clinical and laboratory values (2012‐2017).
3.5. Clinical and laboratory variations between drug type regimen
Patient characteristics, stratified by subgroup of T2D medication drug regimen, are presented for some of the most common T2D drug type regimens (Table 2 ). Patient characteristics and median laboratory values varied substantially among datamarts, as well as between specific T2D drug regimen populations within and between datamarts (Figure 3 ). Median age was between 50 and 70 years of age for most drug regimen groups at most datamarts. Median BMI was between 30 and 35 kg/m2 for most datamarts, though individual drug regimen groups reported more extreme BMI values.
Figure 3.
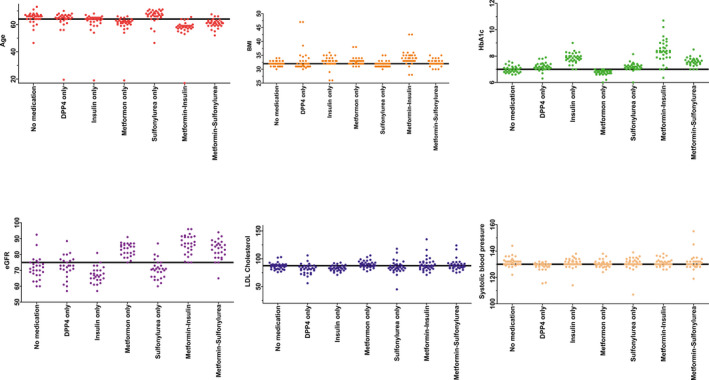
Overall median and distribution of datamart‐specific median values for selected variables for the common drug regimens, PCORnet, 2012‐2017 (n = 33 datamarts). The overall PCORnet population median value, as well as the datamart‐specific median values, for age, BMI, HbA1c, eGFR, LDL, and systolic blood pressure are presented for the most common drug regimens. The solid black horizontal line represents the overall PCORnet median value for each variable. Each dot represents the median value of one individual datamart for that specific drug regimen. Some variables have fewer than 33 dots for certain drug regimens, as some datamarts did not report values for certain variables for specific drug regimens. Data quality and population varied between datamarts. One datamart is a pediatric hospital yielding a low median age (included), and another datamart reported implausible HbA1c values < 1.0% for “No medication” and “metformin‐sulfonylurea” groups (excluded). PCORnet, National Patient‐Centered Clinical Research Network; BMI, body mass index; HbA1c; Hemoglobin A1c; eGFR, estimated glomerular filtration rate; LDL, low‐density lipoprotein
There were some differences in patient demographics, comorbidities, and non‐T2D medications among patients prescribed the most common T2D drug regimens (Tables 2 , 3 and 2 , 3 ). Patients prescribed metformin (whether alone or in combination regimens) had a lower median age in the PCORnet population (metformin only: 62 years; metformin‐sulfonylurea: 61 years; metformin‐insulin: 59 years) compared with those receiving insulin, DPP4, or sulfonylurea regimens only (64, 65, and 68 years, respectively). Median HbA1c values generally ranged from 6.8% to 8.4% in the most common drug regimens.
4. DISCUSSION
We characterized the prescription patterns, clinical characteristics, and medical comorbidities of a cohort of over 600 000 patients with T2D across a geographically diverse population in PCORnet, a novel source of EMR data. At cohort entry, approximately 42% of patients had no evidence of an outpatient T2D prescription, 42% had a single T2D drug class prescription, and 15% were prescribed multiple T2D drug classes. Conventional T2D medication regimens including metformin, sulfonylureas, and insulin were extremely prevalent; in contrast, a minority of regimens (approximately 13%) included newer T2D agents such as GLP1 agonists, DPP4 inhibitors, and SGLT2 inhibitors. Still, because of the large sample size of over 600 000 individuals, the 13% who were prescribed newer T2D agents corresponded to almost 80,000 individuals.
The T2D population in PCORnet has many strengths as a clinical data source including its large size and demographic diversity in terms of age, race, sex, and geographic spread. Other multi‐institutional clinical T2D cohorts exist within the United States, including the Veterans Health Administration (VHA) 3 , 9 (the largest single‐payer EMR system in the United States), 18 Northern California Kaiser Permanente healthcare system, 10 , 11 , 12 and institutions using Centricity EMR systems, 19 as well as internationally, including healthcare registries in the United Kingdom 20 , 21 and Nordic countries. 13 The PCORnet cohort offers certain advantages over existing T2D cohorts, such as greater gender diversity compared with the VHA, 3 , 9 greater geographic diversity compared with the Northern California Kaiser Permanente system, 10 , 11 , 12 and greater racial diversity compared with Nordic health registries. 13
Traditional T2D agents were the most commonly prescribed drug regimens in the PCORnet cohort. This finding is consistent with other studies, 9 , 19 including a recently published study of veterans in the VHA system evaluating an earlier time period. 9 In PCORnet during the years 2012‐2017, sulfonylureas were the most common second‐line antidiabetic drug class combined with metformin, which is concordant with studies evaluating earlier time periods. 3 , 19 , 22 Only a minority of regimens in the PCORnet cohort included newer T2D agents, which is consistent with the findings in the recently published VHA study. 9 The low prevalence of prescriptions for newer T2D agents in the PCORnet cohort is likely related to the study interval (2012‐2017). A recently published study in Nordic patients 13 found an increase in the use of newer agents toward the end of the study period (in 2015). Moreover, several clinical trials since 2015 have demonstrated that SGLT‐2 inhibitors and GLP‐1 receptor agonists decrease cardiovascular events in patients with T2D and known cardiovascular disease. 23 , 24 , 25 , 26 As a result, starting in 2018 the American Diabetes Association (ADA) and European Association for the Study of Diabetes (EASD) recommended augmenting metformin therapy with either SGLT2 or GLP1‐receptor agonists for those with prior cardiovascular disease. 27 , 28 , 29 Thus, we would expect that prescriptions for newer agents in PCORnet have increased since 2018 and will continue to increase.
The aim of the present study was to identify and characterize the T2D population in PCORnet for the first time. Future studies are necessary to establish PCORnet as a valid source for the conduct of pharmacoepidemiological studies, including examining the completeness of prescription data in PCORnet and validating the identification of specific outcomes. Thus, caution is needed when assessing outcomes using EMR data due to completeness of data and accuracy of outcomes. That said, the breadth and accessibility of data available in PCORnet could make it a valuable source of outcomes data for T2D medications in large, “real‐world” populations. Achieving similarly large and diverse sample sizes in clinical trials would be very costly. 30 , 31 Thus, pending additional validation studies, PCORnet could potentially serve as a valuable complement to long‐term trials for cardiovascular outcome assessment. For instance, whether newer agents (SGLT2 and GLP1) prevent cardiovascular outcomes in the broad group of T2D patients without pre‐existing ASCVD and compared to older more common medications is not fully established. Interestingly, a minority of the PCORnet T2D clinical cohort, as well as other clinical cohorts, 3 , 32 had established ASCVD at baseline, which has been an inclusion criteria for prior clinical trials. 23 , 27 , 28 , 29 Most prior observational studies evaluating the effects of newer agents in individuals without ASCVD have been methodologically limited, including a lack of tracking medication persistence, immortal time bias which can magnify the possible benefits, mixed comparison group including multiple drug classes as comparators, and a lack of accounting for clinical variables such as HbA1c, eGFR, and blood pressure. 33 , 34 , 35 , 36 , 37 These limitations can lead to artificial inflation of the effect size, as discussed in a prominent editorial. 38 , 39 The PCORnet datasource can potentially be leveraged to overcome some of these limitations of prior trials by adjusting for clinical variables, tracking medication persistence, and through rigorous study designs.
It is informative to consider the comorbidity and non‐T2D diabetes medication data in the PCORnet cohort with respect to other established T2D cohorts. Less than 30% of our PCORnet T2D cohort had evidence of ASCVD at baseline, which is similar to other clinical T2D populations. 3 , 32 Notably, the prevalence of prescriptions for lipid‐lowering therapies and for ACEi/ARBs are lower in PCORnet compared with T2D cohorts in the VHA 3 within the United States and in Nordic countries, 13 but consistent with a recently published retrospective cohort study analyzing US nationwide administrative claims data. 22 We would expect a majority of patients with T2D to be taking a lipid‐lowering medication given guidelines advocating a statin prescription in all patients with T2D between ages 40‐75 years of age. 40 Possible explanations for the low prevalence of ACEi, ARB, and lipid‐lowering therapies include a true underutilization of appropriate lipid and hypertension therapies for T2D in clinical practice, adverse effects or other contraindications not captured in the current query, receiving prescriptions outside the PCORnet system, and/or receiving prescriptions outside the timeframe specified in the query.
The present study has some important limitations. First, individual patient‐level data were not available. PCORnet data sharing agreements allow datamarts to maintain control of individual‐level data. Second, we classified patients according to prescribing information available only in PCORnet; actual use was not observed. Other studies have reported that approximately 10% of initial antidiabetic prescriptions are abandoned at the pharmacy, and approximately 15% of therapies are self‐discontinued by the patient within the first 6 months. 41 , 42 , 43 Additionally, prescriptions received from providers outside of the health systems in PCORnet would not have been captured in our dataset. Future work can address these limitations through the validation of prescribing data against prescription‐fill data in large‐scale observational studies, and through linkage of the EMR data to other data sources, including pharmacy claims databases. Moreover, over 40% of the T2D cohort had no evidence of an outpatient T2D prescription which is likely related to the timeframe of the query. We chose to capture a relatively narrow “snapshot” of active outpatient T2D prescriptions. For this reason, the prevalence of T2D medication prescriptions in the present study is lower than in other studies that characterized medication use over longer follow‐up periods. 19 Future studies could evaluate a broader timeframe. Next, the current study examined prescription patterns among patients at the time they were first identified in PCORnet, such that it included both patients with prevalent and incident T2D. Therefore, questions related to medication use and other important factors among only patients with incident T2D will need to be addressed in future studies. Another limitation is that the sensitivity and specificity of the computable phenotype for T2D were not available because the prior validation study did not evaluate records for patients who were not identified using the T2D computable phenotype. In addition, as with many clinical cohorts, laboratory values were missing in a substantial number of individuals; baseline HbA1c was only available in 54% of the patients. However, because of our large sample size, we still had HbA1c data in over 330,000 individuals. Finally, a limitation of the current study is the time period evaluated (2012‐2017). The present study had relatively low prevalence of SGLT2 and GLP1 prescriptions; we expect the number of these newer T2D prescriptions to increase in 2018 and beyond due to guideline changes.
In conclusion, among individuals with T2D in PCORnet, we found that conventional T2D therapies including metformin and insulin were very common; newer T2D agents were prescribed less frequently but represented a large absolute number of individuals given the large population size. The variation we observed in demographics and clinical measures between drug regimens and datamarts suggests geographic variation may exist in prescribing patterns and delivery of diabetes care. With its large sample size and geographic diversity, PCORnet represents a powerful resource for the study of many important questions among patients with T2D. Future studies could leverage PCORnet to investigate variation in prescriptions patterns and determine the potential of PCORnet as a valid source for investigating the long‐term safety of T2D medications in “real‐world” populations.
5. ETHICS STATEMENT
This work was performed with approval from Vanderbilt Internal Review Board #171986, approved under 45 CFR 46.110 (F)(5).
CONFLICT OF INTEREST
KNB owns stock in Medtronic (not related to the current project). CGG has served as consultant for Pfizer, Merck, and Sanofi, and received research support from Sanofi, Campbell Alliance, the Agency for Health Care Research and Quality, the Centers for Disease Control and Prevention, the Food and Drug Administration, and the National Institutes of Health; all listed activities are unrelated to the current project. VF receives research support from Bayer, Boehringer Ingelheim, and Gilead (not related to the current project). VF reports honoraria for Consulting and Lectures from Takeda, Novo Nordisk, Sanofi‐ Aventis, Eli, Abbott, Astra‐Zeneca, Intarcia, Asahi (not related to the current project). VF reports Stock Options in Microbiome Technologies, Insulin Algorithms, BRAVO4Health, and Stock in Amgen (not related to the current project). RLR is a consultant for Abbott and Edlogics (not related to the current project). JBB’s contracted consulting fees and travel support for contracted activities are paid to the University of North Carolina by Adocia, AstraZeneca, Dance Biopharm, Dexcom, Eli Lilly, Fractyl, GI Dynamics, Intarcia Therapeutics, Lexicon, MannKind, Metavention, NovaTarg, Novo Nordisk, Orexigen, PhaseBio, Sanofi, Senseonics, vTv Therapeutics, and Zafgen. JBB reports grant support from AstraZeneca, Eli Lilly, Intarcia Therapeutics, Johnson & Johnson, Lexicon, Medtronic, NovaTarg, Novo Nordisk, Sanofi, Theracos, Tolerion, and vTv Therapeutics. JBB is a consultant to Cirius Therapeutics Inc, CSL Behring, Mellitus Health, Neurimmune AG, Pendulum Therapeutics, and Stability Health. JBB holds stock/options in Mellitus Health, Pendulum Therapeutics, PhaseBio, and Stability Health. The remaining authors have no conflicts of interest to declare.
AUTHORS’ CONTRIBUTIONS
KNB contributed to data curation and data interpretation, wrote the original draft of manuscript, and reviewed and edited the manuscript. RJC conceptualized and designed the study, contributed to data curation and data interpretation, and reviewed and edited the manuscript. CLR conceptualized and designed the study, received funding for the research, contributed to data curation and interpretation, and reviewed and edited the manuscript. ADW curated and analyzed the data, contributed to data interpretation, drafted the figures and tables, and reviewed and edited the manuscript. All authors contributed to research implementation and data curation, and reviewed and edited the manuscript.
Supporting information
Table S1‐S3
ACKNOWLEDGMENTS
United States Department of Veterans Affairs Clinical Sciences Research and Development (CSRD) Service, Career Development Award Number: IK2 CX001678; Patient‐Centered Outcomes Research Institute, Grant/Award Number: CDRN‐1306‐04869; PhRMA Foundation; People Centered Research Foundation (PCRF) RFA 2017‐12‐05‐1252; Vanderbilt University Medical Center Faculty Research Scholars Award; National Institutes of Health, Grant/Award Number: UL1TR002489; U01DK098246, UC4DK108612, U54DK118612, and the National Institute of General Medical Sciences of the National Institutes of Health, which funds the Louisiana Clinical and Translational Science Center U54 GM104940.
Bachmann KN, Roumie CL, Wiese AD, et al. Diabetes medication regimens and patient clinical characteristics in the national patient-centered clinical research network, PCORnet. Pharmacol Res Perspect. 2020;8:e00637 10.1002/prp2.637
Primary Laboratory of Origin: Vanderbilt University Medical Center, Nashville, TN, USA.
Funding information
United States Department of Veterans Affairs Clinical Sciences Research and Development (CSRD) Service, Career Development Award Number: IK2 CX001678; Patient‐Centered Outcomes Research Institute, Grant/Award Number: CDRN‐1306‐04869; PhRMA Foundation; People Centered Research Foundation (PCRF) RFA 2017‐12‐05‐1252; Vanderbilt University Medical Center Faculty Research Scholars Award; National Institutes of Health, Grant/Award Number: UL1TR002489; U01DK098246, UC4DK108612, U54DK118612, and the National Institute of General Medical Sciences of the National Institutes of Health, which funds the Louisiana Clinical and Translational Science Center U54 GM104940.
DATA AVAILABILITY STATEMENT
A de‐identified and anonymized dataset is available with written request to the author.
REFERENCES
- 1. Dean BB, Lam J, Natoli JL, Butler Q, Aguilar D, Nordyke RJ. Review: use of electronic medical records for health outcomes research: a literature review. Med Care Res Rev. 2009;66:611‐638. [DOI] [PubMed] [Google Scholar]
- 2. Murff HJ, Roumie CL, Greevy RA, et al. Metformin use and incidence cancer risk: evidence for a selective protective effect against liver cancer. Cancer Causes Control. 2018;29:823‐832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Roumie CL, Greevy RA, Grijalva CG, et al. Association between intensification of metformin treatment with insulin vs sulfonylureas and cardiovascular events and all‐cause mortality among patients with diabetes. JAMA. 2014;311:2288‐2296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Min JY, Griffin MR, Hung AM, et al. Comparative Effectiveness of Insulin versus Combination Sulfonylurea and Insulin: a Cohort Study of Veterans with Type 2 Diabetes. J Gen Intern Med. 2016;31:638‐646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Brownstein JS, Murphy SN, Goldfine AB, et al. Rapid identification of myocardial infarction risk associated with diabetes medications using electronic medical records. Diabetes Care. 2010;33:526‐531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Paul SK, Klein K, Maggs D, Best JH. The association of the treatment with glucagon‐like peptide‐1 receptor agonist exenatide or insulin with cardiovascular outcomes in patients with type 2 diabetes: a retrospective observational study. Cardiovasc Diabetol. 2015;14:10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Roumie CL, Min JY, Greevy RA, et al. Risk of hypoglycemia following intensification of metformin treatment with insulin versus sulfonylurea. CMAJ. 2016;188:E104‐E112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Food and Drug Administration CfDEaR . Guidance for industry: diabetes mellitus—evaluating cardiovascular risk in new antidiabetic therapies to treat type 2 diabetes. 2008.
- 9. Alexopoulos AS, Jackson GL, Edelman D, et al. Clinical factors associated with persistently poor diabetes control in the Veterans Health Administration: A nationwide cohort study. PLoS One. 2019;14:e0214679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Whitmer RA, Karter AJ, Yaffe K, Quesenberry CP Jr, Selby JV. Hypoglycemic episodes and risk of dementia in older patients with type 2 diabetes mellitus. JAMA. 2009;301:1565‐1572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Karter AJ, Rowell SE, Ackerson LM, et al. Excess maternal transmission of type 2 diabetes. The Northern California Kaiser Permanente Diabetes Registry. Diabetes Care. 1999;22:938‐943. [DOI] [PubMed] [Google Scholar]
- 12. Laraia BA, Downing JM, Zhang YT, et al. Food Environment and Weight Change: Does Residential Mobility Matter?: The Diabetes Study of Northern California (DISTANCE). Am J Epidemiol. 2017;185:743‐750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Persson F, Bodegard J, Lahtela JT, et al. Different patterns of second‐line treatment in type 2 diabetes after metformin monotherapy in Denmark, Finland, Norway and Sweden (D360 Nordic): A multinational observational study. Endocrinol Diabetes Metab. 2018;1:e00036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Fleurence RL, Curtis LH, Califf RM, Platt R, Selby JV, Brown JS. Launching PCORnet, a national patient‐centered clinical research network. J Am Med Inform Assoc. 2014;21:578‐582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Wiese AD, Roumie CL, Buse JB, et al. Performance of a computable phenotype for identification of patients with diabetes within PCORnet: The Patient‐Centered Clinical Research Network. Pharmacoepidemiol Drug Saf. 2019;28(5):632‐639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Garza M, Del Fiol G, Tenenbaum J, Walden A, Zozus MN. Evaluating common data models for use with a longitudinal community registry. J Biomed Inform. 2016;64:333‐341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Coresh J, Turin TC, Matsushita K, et al. Decline in estimated glomerular filtration rate and subsequent risk of end‐stage renal disease and mortality. JAMA. 2014;311:2518‐2531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Kupersmith J, Francis J, Kerr E, et al. Advancing evidence‐based care for diabetes: lessons from the Veterans Health Administration. Health Aff (Millwood). 2007;26:w156‐w168. [DOI] [PubMed] [Google Scholar]
- 19. Montvida O, Shaw J, Atherton JJ, Stringer F, Paul SK. Long‐term Trends in Antidiabetes Drug Usage in the U.S.: Real‐world Evidence in Patients Newly Diagnosed With Type 2 Diabetes. Diabetes Care. 2018;41:69‐78. [DOI] [PubMed] [Google Scholar]
- 20. MacDonald MR, Eurich DT, Majumdar SR, et al. Treatment of type 2 diabetes and outcomes in patients with heart failure: a nested case‐control study from the U.K. General Practice Research Database. Diabetes Care. 2010;33:1213‐1218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. McGovern A, Hinton W, Correa A, Munro N, Whyte M, de Lusignan S. Real‐world evidence studies into treatment adherence, thresholds for intervention and disparities in treatment in people with type 2 diabetes in the UK. BMJ Open. 2016;6:e012801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. O'Brien MJ, Karam SL, Wallia A, et al. Association of Second‐line Antidiabetic Medications With Cardiovascular Events Among Insured Adults With Type 2 Diabetes. JAMA Netw Open. 2018;1:e186125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Zinman B, Wanner C, Lachin JM, et al. Cardiovascular Outcomes, and Mortality in Type 2 Diabetes. N Engl J Med. 2015;373:2117‐2128. [DOI] [PubMed] [Google Scholar]
- 24. Neal B, Perkovic V, Mahaffey KW. Canagliflozin and Cardiovascular and Renal Events in Type 2 Diabetes. N Engl J Med. 2017;377:644‐657. [DOI] [PubMed] [Google Scholar]
- 25. Marso SP, Daniels GH, Brown‐Frandsen K, et al. Liraglutide and Cardiovascular Outcomes in Type 2 Diabetes. N Engl J Med. 2016;375:311‐322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Gerstein HC, Colhoun HM, Dagenais GR, et al. Dulaglutide and cardiovascular outcomes in type 2 diabetes (REWIND): a double‐blind, randomised placebo‐controlled trial. Lancet. 2019. [DOI] [PubMed] [Google Scholar]
- 27. Summary of Revisions . Standards of Medical Care in Diabetes‐2019. Diabetes Care. 201942:S4‐S6. [DOI] [PubMed] [Google Scholar]
- 28. Pharmacologic Approaches to Glycemic Treatment . Standards of Medical Care in Diabetes‐2019. Diabetes Care. 2019;42:S90‐S102. [DOI] [PubMed] [Google Scholar]
- 29. Disease C, Management R. Standards of Medical Care in Diabetes‐2019. Diabetes Care. 2019;42:S103‐S123. [DOI] [PubMed] [Google Scholar]
- 30. Bachmann KN, Wang TJ. Biomarkers of cardiovascular disease: contributions to risk prediction in individuals with diabetes. Diabetologia. 2018;61:987‐995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Singh AK, Singh R. SAVOR‐TIMI to SUSTAIN‐6: a critical comparison of cardiovascular outcome trials of antidiabetic drugs. Expert Rev Clin Pharmacol. 2017;10:429‐442. [DOI] [PubMed] [Google Scholar]
- 32. Holden SE, Jenkins‐Jones S, Morgan CL, Peters JR, Schernthaner G, Currie CJ. Prevalence, glucose control and relative survival of people with Type 2 diabetes in the UK from 1991 to 2013. Diabet Med. 2017;34:770‐780. [DOI] [PubMed] [Google Scholar]
- 33. Ryan PB, Buse JB, Schuemie MJ, et al. Comparative effectiveness of canagliflozin, SGLT2 inhibitors and non‐SGLT2 inhibitors on the risk of hospitalization for heart failure and amputation in patients with type 2 diabetes mellitus: A real‐world meta‐analysis of 4 observational databases (OBSERVE‐4D). Diabetes Obes Metab. 2018;20:2585‐2597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Patorno E, Goldfine AB, Schneeweiss S, et al. Cardiovascular outcomes associated with canagliflozin versus other non‐gliflozin antidiabetic drugs: population based cohort study. BMJ. 2018;360:k119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Kosiborod M, Lam CSP, Kohsaka S, et al. Cardiovascular Events Associated With SGLT‐2 Inhibitors Versus Other Glucose‐Lowering Drugs: The CVD‐REAL 2 Study. J Am Coll Cardiol. 2018;71:2628‐2639. [DOI] [PubMed] [Google Scholar]
- 36. Kosiborod M, Birkeland KI, Cavender MA, et al. Rates of myocardial infarction and stroke in patients initiating treatment with SGLT2‐inhibitors versus other glucose‐lowering agents in real‐world clinical practice: Results from the CVD‐REAL study. Diabetes Obes Metab. 2018;20:1983‐1987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Cavender MA, Norhammar A, Birkeland KI, et al. SGLT‐2 Inhibitors and Cardiovascular Risk: An Analysis of CVD‐REAL. J Am Coll Cardiol. 2018;71:2497‐2506. [DOI] [PubMed] [Google Scholar]
- 38. Suissa S. Lower Risk of Death With SGLT2 Inhibitors in Observational Studies: Real or Bias? Diabetes Care. 2018;41:6‐10. [DOI] [PubMed] [Google Scholar]
- 39. Suissa S. Response to Comment on Suissa. Lower Risk of Death With SGLT2 Inhibitors in Observational Studies: Real or Bias? Diabetes Care 2018;41:6–10. Diabetes Care. 2018;41:e109‐e110. [DOI] [PubMed] [Google Scholar]
- 40. Stone NJ, Robinson JG, Lichtenstein AH, et al. ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2013;2014(129):S1‐45. [DOI] [PubMed] [Google Scholar]
- 41. Capoccia K, Odegard PS, Letassy N. Medication Adherence With Diabetes Medication: A Systematic Review of the Literature. Diabetes Educ. 2016;42:34‐71. [DOI] [PubMed] [Google Scholar]
- 42. Raebel MA, Carroll NM, Ellis JL, Schroeder EB, Bayliss EA. Importance of including early nonadherence in estimations of medication adherence. Ann Pharmacother. 2011;45:1053‐1060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Shah NR, Hirsch AG, Zacker C, Taylor S, Wood GC, Stewart WF. Factors associated with first‐fill adherence rates for diabetic medications: a cohort study. J Gen Intern Med. 2009;24:233‐237. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1‐S3
Data Availability Statement
A de‐identified and anonymized dataset is available with written request to the author.


